Maternal and neonatal mortality are important public health issues in low-income countries. This study evaluated spatial and temporal maternal and neonatal mortality trends in Brazil between 1997 and 2012.
MethodsThis study employed spatial analysis techniques using death records from the mortality information system. Maternal mortality rates per 100,000 and neonatal mortality rates (early and late) per 1000 live births were calculated by state, region, and period (1997–2000, 2001–2004, 2005–2008, and 2009–2012). Multivariate negative binomial models were used to explain the risk of death.
ResultsThe mean Brazilian maternal mortality rate was 55.63/100,000 for the entire 1997–2012 period. The rate fell 10% from 1997–2000 (58.92/100,000) to 2001–2004 (52.77/100,000), but later increased 11% during 2009–2012 (58.69/100,000). Early and late neonatal mortality rates fell 33% (to 7.36/1000) and 21% (to 2.29/1000), respectively, during the 1997–2012 period. Every Brazilian region witnessed a drop in neonatal mortality rates. However, maternal mortality increased in the Northeast, North, and Southeast regions.
ConclusionBrazil's neonatal mortality rate has improved in recent times, but maternal mortality rates have stagnated, failing to meet the Millennium Development Goals. Public policies and intersectoral efforts may contribute to improvements in these health indicators.
A mortalidade materna e neonatal é um importante problema de saúde pública em países de baixa renda. Este estudo avaliou as tendências de mortalidade materna e neonatal espacial e temporal no Brasil entre 1997 e 2012.
MétodosEste estudo utilizou técnicas de análise espacial utilizando registros de óbito do Sistema de Informações sobre Mortalidade. As taxas de mortalidade materna a cada 100.000 e as taxas de mortalidade neonatal (precoce e tardia) a cada 1.000 nascidos vivos foram calculadas por estado, região e período (1997-2000, 2001-2004, 2005-2008 e 2009-2012). Os modelos binomiais negativos multivariados foram utilizados para explicar o risco de morte.
ResultadosA taxa de mortalidade materna no Brasil foi 55,63/100.000 em todo o período entre 1997 e 2012. A taxa caiu 10% de 1997-2000 (58,92/100.000) a 2001-2004 (52,77/100.000), porém, mais tarde, aumentou 11% até 2009-2012 (58,69/100.000). As taxas de mortalidade neonatal precoce e tardia caíram 33% (para 7,36/1.000) e 21% (para 2.29/1.000), respectivamente, durante o período de 1997-2012. Toda região brasileira testemunhou uma queda nas taxas de mortalidade neonatal. Contudo, a mortalidade materna aumentou nas regiões Nordeste, Norte e Sudeste.
ConclusãoA taxa de mortalidade neonatal do Brasil melhorou nos últimos anos, porém as taxas de mortalidade materna estagnaram, deixando de atingir os Objetivos de Desenvolvimento do Milênio. As políticas públicas e os esforços intersetoriais poderão contribuir para as melhorias nesses indicadores de saúde.
Maternal and neonatal mortality are important health issues in low-income countries: 99% of the worldwide maternal deaths occur in developing countries,1 and 44% of global neonatal deaths occur in only five countries of the world: India (27.8%), Nigeria (7.2%), Pakistan (6.9%), China (6.4%), and the Democratic Republic of Congo (4.6%).2 Factors like poor access to education, low income, poor obstetrics assistance, and high pregnancy rates contribute to the persistence of these high indicators of mortality.3
While the maternal mortality rate in developed countries was about 16/100,000 in 2010, in developing countries it was about 240/100,000 (fifteen times higher) for the same year. In Brazil, previous studies showed that the maternal mortality rate in 2000 was 54.3/100,000 live births (73.2/100,000 in the North region and 42/100,000 in the South region),4,5 but in 2009 it rose to 65.1/100,000.6
The worldwide percentage of neonatal deaths in 2009 (regarding all under-five child deaths) was 41%, which corresponds to 3.3 million of deaths in children younger than 28 days. Between 1990 and 2009, global neonatal mortality rates fell 28%, or from 33.2/1000 to 23.9/1000 over the period. In Brazil, the neonatal mortality rate was 11.1/1000 in 2011–2012, and 38.3% and 30.5% of the these deaths occurred in the Northeast and Southeast regions, respectively.7
Brazil is the largest country of South America and has several regional socioeconomic differences. The Human Development Index in the Southeast, South, and Midwest regions of the country varies around 0.75–0.76, while in the North and Northeast, it ranges from 0.66 to 0.67.8 These contrasts make mortality indicators quite heterogeneous across the country.
World leaders have set goals to reduce mortality rates both for children and for pregnant women (Millennium Development Goal 4 and Millennium Development Goal 5, respectively). For child mortality, the goal was to reduce 1990 benchmark rates to one-third of their values by 2015.2 As the neonatal period is the most vulnerable phase of a child's life and the neonatal component of infant mortality is the most difficult to reduce, decreased neonatal deaths have played an important part in reaching this goal.3,9 However, even though the overall rates show a reasonable situation regarding this indicator, it is necessary to consider the heterogeneity of the rates across the country. The North and Northeast regions witness rates almost 100% higher than those in the South and Southeast.7
For maternal mortality, the goal was to reduce rates by 75% between 1990 and 2015.3,9 The Brazilian Ministry of Health estimated that the maternal mortality rate in 1990 was 141/100,000.10 Thus, Brazil's goal was to reduce maternal deaths to 36 per 100,000 by 2015. In 2001, the maternal rate had decreased 44%, reaching 80/100,00010; however, after that, the rate of decline slowed,11 reaching only 70/100,000 in 2011.10 In light of this situation, the reduction of maternal mortality in Brazil remains an important public health issue and a continuing challenge for obstetric care.
Maternal and neonatal indicators reflect both the social contrasts and the poor capacity of Brazilian health system to provide suitable health care for its entire population. Given Brazil's difficulties in meeting its Millennium Development Goals,6,12 despite some improvement in these indicators, this study evaluated spatial and temporal trends in maternal and neonatal mortality from 1997 to 2012 in order to help health managers implement actions and resources to improve this situation.
MethodsThis is an ecological study using spatial analysis techniques. The spatial analysis unit used to prepare thematic maps was the state.
Data about maternal and neonatal deaths were collected from the Mortality Information System (Sistema de Informações sobre Mortalidade [SIM]). This study considered maternal deaths as those classified in the tenth revision of the International Classification of Disease (ICD-10): (1) pregnancy, childbirth, and puerperium (codes O00-O99) excluding deaths outside of puerperium's period of 42 days (codes O96 and O97); (2) human immunodeficiency virus (HIV) disease (B20-B24), hydatidiform mole, invasive or malignant (D39.2), or hypopituitarism (E23.0), since it occurs in pregnant women or during the puerperium period (from 1997 to 1999, it was only considered in the deaths of pregnant women); (3) puerperal osteomalacia (M83.0), obstetrical tetanus (A34), or mental and behavioral disorders associated with the puerperium, not elsewhere classified (F53), for deaths occurring up to 42 days after birth or in deaths without information of the time between birth and death.12
Early neonatal deaths were considered as those occurring in live births aged 0–6 days and late neonatal deaths were classified as those in live births aged 7–27 days.
Maternal mortality rates per 100,000 live births were calculated, as well as early and late neonatal mortality rates per 1000 live births by area (state and region) and by four-year period (1997–2000, 2001–2004, 2005–2008, and 2009–2012). In the numerator of the rates, this study used maternal, early neonatal, and late neonatal deaths to construct maternal, early-neonatal, and late-neonatal mortality indexes, respectively. The number of live births was used in the denominator for all rates.13
Statistical methodsSpatial analysis techniques were applied to prepare thematic maps and the georeferenced mesh of Brazilian states was used (shapefile file), available at the website of the Brazilian Institute of Geography and Statistics.
Although Poisson regression is the most common strategy for modeling count data, this technique does not produce reliable estimates for models presenting overdispersion.14 In this study, the Poisson model showed significant dispersion, so it was not used in the analysis. To avoid this problem, multivariate binomial negative models were used to explain the risk of maternal deaths and neonatal (early and late) deaths. Response variables of the three models were the counts of maternal deaths, early neonatal deaths, and late neonatal deaths. The independent variables included in both models were: period (four-year), prenatal care (average of the number of prenatal visits), place of birth (homebirth or hospital birth), and the residence area (North, Northeast, South, Southeast, and Midwest). The number of live births was included in the models as an offset variable.
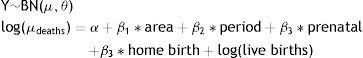
Specifications of the models:
where μ is the average number of expected deaths, α is the model intercept, and β corresponds to regression coefficients. Period and area were included as dummy variables; the following were used as reference category: 1997–2000 period and Midwest area. In both models, a logarithmic link function (logarithm of the live births) was added as an offset variable.Tables, graphical models, and maps were used to present the results. All analyses were performed with TerraView (TerraView 4.1.0. São José dos Campos, SP: INPE, 2010) and R-Project software version 3.1.3 (R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria, 2014).12
This study follows the ethical principles of Brazilian legislation (Ethics Committee document No. 02/2016 – Ethics Committee of Escola Nacional de Saúde Pública Sérgio Arouca).
ResultsThe average Brazilian maternal mortality rate during the 1997–2012 period was 55.63/100,000, reaching a minimum of 52.77 and a maximum of 58.92/100,000. The rate showed a preliminary decrease of 10% in the 2001–2004 period compared to 1997–2000. After that, the rate increased 11%, reaching 58.69/100,000 in 2009–2012. The results by region show increasing mortality rates in the period 2009–2012 compared to 1997–2000, except for the Southeast and South regions (Table 1).
Maternal and neonatal mortality trends by Brazilian region, 1997–2012.
| Maternal mortality ratio/100,000 live births | Neonatal mortality rate (0–6 days)/1000 live births | Neonatal mortality rate (7–28 days)/1000 live births | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1997–2000 | 2001–2004 | 2005–2008 | 2009–2012 | 1997–2000 | 2001–2004 | 2005–2008 | 2009–2012 | 1997–2000 | 2001–2004 | 2005–2008 | 2009–2012 | |
| North | 58.86 | 53.24 | 59.95 | 63.88 | 12.66 | 11.06 | 9.69 | 8.87 | 3.17 | 2.94 | 2.57 | 2.48 |
| Northeast | 56.27 | 61.36 | 65.93 | 69.63 | 11.50 | 11.51 | 10.14 | 8.85 | 2.98 | 2.87 | 2.53 | 2.27 |
| Southeast | 59.59 | 44.24 | 45.5 | 52.22 | 11.09 | 8.53 | 7.16 | 6.38 | 3.06 | 2.80 | 2.54 | 2.28 |
| South | 65.79 | 55.17 | 54.78 | 49.86 | 8.69 | 7.80 | 6.73 | 5.85 | 2.32 | 2.52 | 2.29 | 2.12 |
| Midwest | 51.06 | 57.46 | 55.45 | 57.83 | 9.79 | 8.95 | 7.66 | 7.14 | 2.78 | 2.93 | 2.59 | 2.44 |
| Total | 58.92 | 52.77 | 55.19 | 58.69 | 10.89 | 9.62 | 8.32 | 7.36 | 2.92 | 2.81 | 2.51 | 2.29 |
Early neonatal mortality rates declined 33% from 1997 to 2012, falling from 10.89/1000 (1997–2000) to 7.36/1000 (2008–2012). Overall, early neonatal mortality rates fell in every Brazilian region. In the Southeast, the largest decrease was detected (42%), and in the Northeast, the smallest (23%; Table 1).
Late neonatal mortality rates decreased 21%, from 2.92/1000 to 2.29/1000 between 1997 and 2012, with the Southeast showing the highest decrease of 26% (Table 1).
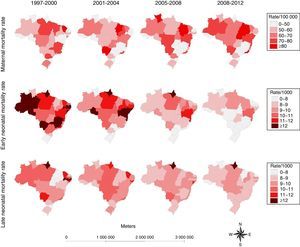
In Fig. 1, it can be seen that in some North and Northeast states, like Amazonas and Bahia, there was a significant increase in maternal mortality rates during this period. In contrast, in the Southeast, there was a decrease in states like Minas Gerais and São Paulo.
Distribution of maternal and neonatal1 mortality in Brazilian states by period, 1997–2012. Neonatal mortality: early neonatal mortality, deaths among live births in the first 6 days of life; late neonatal mortality, deaths among live births between the seventh and the 28th day of life.
Regarding early neonatal mortality rates, the states with the highest rates in the first study period experienced significant declines during the period under study (e.g. Minas Gerais, in the Southeast; Mato Grosso do Sul, in the Midwest; and Amazonas, Acre, and Rondônia, in the North). The state of Bahia, in the Northeast, showed the highest early neonatal mortality rate at the end of the study period (10–11/1000) (Fig. 1).
Regarding late neonatal mortality rates, Rio de Janeiro (Southeast), Ceará and Pernambuco (Northeast), Amazonas (North), and Mato Grosso do Sul (Midwest) were some of states that showed the highest rates in the first periods. Amapá, in the North, had the highest rates in all the study periods (over 12/1000) (Fig. 1).
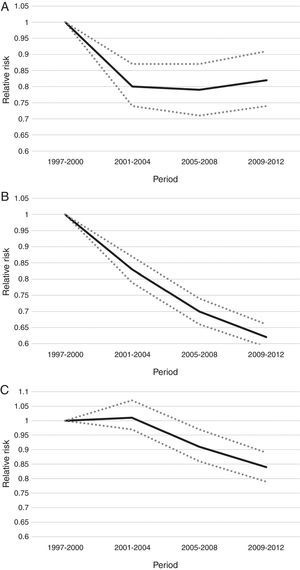
The findings in Table 2 and Fig. 2 reveal a significant reduction of 20% in maternal mortality from 1997–2000 to 2001–2004 (adjusted by region, homebirth and prenatal care). After this time, maternal mortality rates remained nearly steady. A 31% increase in maternal mortality risk was found in the Northeast compared to the Midwest region (results adjusted by period, homebirth, and prenatal care) (Table 2).
Factors associated with maternal, early, and late neonatal mortality in Brazil.
| Maternal mortality rate | Early neonatal mortality rate | Late neonatal mortality rate | ||||
|---|---|---|---|---|---|---|
| RR | p-v | RR | p-v | RR | p-v | |
| Period | ||||||
| 1997-2000a | 1.00 | 1.00 | 1.00 | |||
| 2001–2004 | 0.80 | 0.0001 | 0.83 | 0.0001 | 1.01 | 0.56 |
| 2005–2008 | 0.79 | 0.0001 | 0.70 | 0.0001 | 0.91 | 0.002 |
| 2009–2012 | 0.82 | 0.0002 | 0.62 | 0.0001 | 0.84 | 0.0001 |
| Area | ||||||
| Midwesta | 1.00 | 1.00 | 1.00 | |||
| North | 1.25 | 0.13 | 1.45 | 0.0001 | 1.10 | 0.27 |
| Northeast | 1.31 | 0.0002 | 1.38 | 0.0001 | 0.99 | 0.86 |
| South | 0.88 | 0.001 | 0.96 | 0.07 | 1.00 | 0.94 |
| Southeast | 1.00 | 0.98 | 0.86 | 0.0001 | 0.86 | 0.0001 |
RR, adjusted relative risk (binomial negative regression models); p-v, p-value.
The factors included in the models were: period, region, prenatal care, and homebirth. The number of live births was included in the models as an offset.
Trends in mortality rates from 1997 to 2012. A, maternal mortality; B, early neonatal mortality; C, late neonatal mortality. Each figure corresponds to one binomial negative model. Dependent variables of each model: maternal deaths (A), early neonatal deaths (B), and late neonatal deaths (C). The factors included in the models were: period, region, prenatal care, and homebirth. The number of live births was included in the models as an offset.
Regarding early neonatal mortality rates, the results of Table 2 and Fig. 2 showed a decrease in early neonatal mortality risk in all periods (adjusted by region, homebirth, and prenatal care). This reduction was 17%, 30%, and 38% in 2001–2004, 2005–2008, and 2009–2012, respectively, compared to the 1997–2000 reference period.
Early neonatal mortality risk in the North and Northeast regions was 45% and 38% higher than the Midwest region, respectively (adjusted by period, homebirth, and prenatal care) (Table 2).
Table 2 and Fig. 2 also reveal a decrease in late neonatal mortality risk in 2005–2008 and 2009–2012 as compared to 1997–2000 (adjusted by region, homebirth, and prenatal care). This reduction was 9% and 16%, respectively in 2005–2008 and 2009–2012, compared to 1997–2000 (adjusted by region, homebirth, and prenatal care). Both early and late neonatal mortality risks were 14% lower in the Southeast than in the Midwest region (adjusted by period, homebirth, and prenatal care) (Table 2).
DiscussionFrom 1997 to 2012, the average maternal mortality rate in Brazil was 56/100,000. Stratifying this data in terms of period and place helps to clarify some inconsistencies in previous findings. From 1990 to 2010, Brazil's Ministry of Health reported a decrease of 62% (ranging from 141/100,000 to 54/100,000).10 Ferraz and Bordignon, however, saw a 20% jump in Brazilian maternal mortality rates from 54/100,000 in 2000 to 65/100,000 in 2009.6 In contrast, the present study detected a 20% decrease in maternal mortality risk from the 1997–2000 period to the 2001–2004 period. After this time, maternal mortality risk remained roughly constant.
This study confirms previous findings showing regional discrepancies in maternal mortality risk. In 2009–2012, the South and Southeast showed the lowest maternal mortality rates, while the North and Northeast showed the highest. Previous studies have highlighted that the North region has the highest maternal mortality rates of the country, while the South retains the lowest.4,5,15 In the Northeast, this study shows that maternal mortality rates increased throughout the period, while in the South, the opposite happened.
The greater availability of public health services in the South and Southeast compared to the North and Northeast may explain regional differences. In 1999, there were 5709 health services in Brazil providing childbirth care (73% of all Brazilian hospitals); however, only 5% of these health services specialized in obstetrics. In the same year, the North, Northeast, Southeast, South, and Midwest had 65%, 53%, 78%, 71%, and 91% of the Brazilian health services providing obstetrics care, respectively.16,17
Brazil's neonatal mortality rates fell by more than half from 1990 to 2012 (from 22.05/1000 to 9.33/1000).12 The present study disaggregates early vs. late neonatal mortality rates. The findings show that average early neonatal mortality rates decreased from 10.89/1000 (1997–2000) to 7.86/1000 (2009–2012), while late neonatal mortality decreased from 2.92/1000 (1997–2000) to 2.29/1000 (2009–2012). Similarly, in the state of São Paulo (Southeast region), the average early neonatal mortality rate fell from 8.67/1000, in 2000, to 5.74/1000 in 2010,18 while the late neonatal mortality remained around 2.5/1000 (2006–2010).19
Brazil's reductions in neonatal mortality risk compare favorably to international standards. In 2004, the neonatal mortality rate in developing countries was 31/1000, and 76% of the neonatal deaths occurred in the first week of life.20 In developed countries, there are few neonatal deaths, with rates around 4/1000 in 2004.20 In underdeveloped and developing countries (2010–2012), 34% of neonatal deaths occur on the same day as childbirth, and 14% in the day after.21 In low-income countries, the late neonatal mortality rate in 2004 was approximately 7/1000, while in developed countries, this rate was nearly 1/1000.20
Neonatal mortality is gradually decreasing in several parts of the world. From 1990 to 2010, there was a decrease in neonatal mortality rates of approximately 50% in European regions, and 19% in African regions.22 In the present study, from 1997–2000 to 2009–2012, a decrease of 38% was detected in early neonatal mortality risk, and 16% drop in late neonatal mortality risk.
The availability of hospital beds for newborns – as well as the supply of specialized equipment for neonatal assistance – is not uniform throughout Brazil.16 This situation may explain the differences in neonatal mortality rates across Brazilian regions. While in the South, in 1999, 40% of health institutions had at least, ten neonatal intensive care unit (ICU) beds, in the North and Northeast, only 10% of health institutions had at least ten neonatal ICU beds.16 The prevention of neonatal deaths contributes significantly to reduce infant mortality.23 The neonatal component is associated with access to health services providing assistance with childbirth, support for newborns, and care for pregnant women.23 For example, Brazil's Family Health Program has played a significant role in reducing perinatal mortality.24
Below, the main limitations of this study are highlighted. The quality of health data from Brazil's information systems is gradually improving. As the quality of mortality information has improved only recently in the North and Northeast regions, compared to the other regions, the apparent increase in maternal mortality risk in the North and Northeast regions observed in this study must be interpreted with caution. The results thus may reflect recent improvements in Brazil's health data collection systems in these regions.25,26 In addition, the spread of maternal mortality committees across the country has improved the quantity and quality of information regarding the causes of maternal deaths. In 2005, there were 748 and 206 of these committees at the municipal and hospital level, respectively.27 Although the present findings represent official data, the Brazilian national health information system still experiences underreporting, slow data processing, and a high number of ill-defined causes of death.28
Brazil appears to have met the international targets for reducing infant mortality, but not maternal mortality. Infant mortality fell from 48/100,000 in 1990 to 13.46/100,000 in 2012.10,23 If this trend has not changed until 2015, the World Health Organization (WHO) targets should be achieved. Technological advances, including better use of resources at neonatal ICUs that save or prolong lives of newborns, probably contributed to the reduction in neonatal rates during this period.
Maternal mortality rates have fallen, but this figure still remains high and above the 75% reduction target for the 1990–2015 period,2,3,9i.e., reaching a level near 36/100,000. Since 2001, Brazil's current maternal rate has stagnated at around 54/100,000. As maternal death is a sentinel event indicating deficient quality of health assistance, Brazil needs to improve health care during pregnancies and childbirth. In fact, childbirth and obstetrics problems were the main causes of hospitalization in 2001 in public health hospitals of Brazil.29
Public health policies can contribute to minimize health risks in pregnant women and newborns, as well as improve access to health assistance. The Ministry of Health has made efforts to reduce these indicators by establishing national pacts in 2006, and by starting new programs like the Stork Network in 2011. Health officials set up this network in order to guarantee the right to a safe birth. Additional intersectoral actions could also contribute to health promotion and favor positive results in the health of children and women.1
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Rodrigues NC, Monteiro DL, Almeida AS, Barros MB, Pereira Neto A, O’Dwyer G, et al. Temporal and spatial evolution of maternal and neonatal mortality rates in Brazil, 1997–2012. J Pediatr (Rio J). 2016;92:567–73.