Brazil is a large, heterogeneous, and diverse country, marked by social, economic, and regional inequalities. Stillbirth is a global concern, especially in low- and middle-income countries. This study investigated the prevalence and possible determinants of stillbirth in different regions of Brazil.
MethodsThis is a cross-sectional study including all women of reproductive age who had had a pregnancy in the last five years, enrolled in the most recent Brazilian Demographic and Health Survey (DHS/PNDS-2006/07). Logistic regression was used to assess the association between region and other maternal characteristics and stillbirth risk.
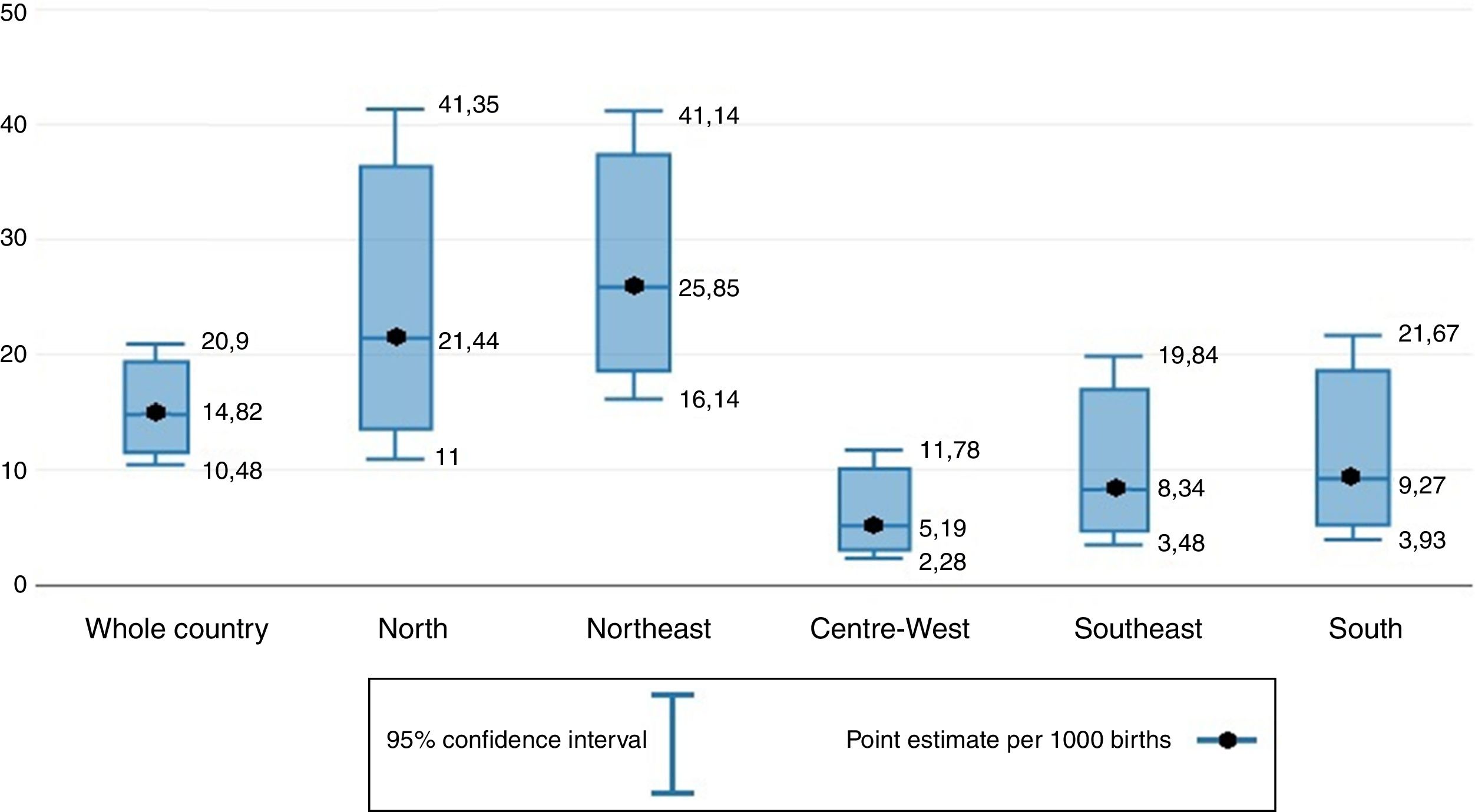
ResultsThe prevalence of stillbirth in Brazil was 14.82 per 1000 births, with great variation by region of the country, and a higher prevalence among the most deprived. The North and Northeast regions had the highest odds of stillbirth compared to the Center-West, which persisted after adjustment for multiple confounders – including deprivation level and ethnicity. Low maternal age and maternal obesity were also related to higher odds of stillbirth.
ConclusionIn Brazil, the region influences stillbirth risk, with much higher risk in the North and Northeast. Variation in socioeconomic level does not explain this finding. Further research on the subject should explore other possible explanations, such as antenatal care and type of delivery, as well as the role of the private and public health systems in determining stillbirth. Preventive strategies should be directed to these historically disadvantaged regions, such as guaranteeing access and quality of care during pregnancy and around the time of birth.
O Brasil é um país extenso, heterogêneo e diverso, marcado por desigualdades sociais, econômicas e regionais. A natimortalidade é uma preocupação global, principalmente em países de reida média e baixa. Este estudo investigou a prevalência e possíveis determinantes da natimortalidade nas diferentes regiões do Brasil.
MétodosEste é um estudo transversal incluindo todas as mulheres em idade reprodutiva que estiveram grávidas nos últimos cinco anos registradas na Pesquisa Nacional sobre Demografia e Saúde (PNDS-2006/07). Regressão logística foi utilizada para avaliar a relação entre região e outras características maternas e risco de natimortalidade.
ResultadosA prevalência de natimortos no Brasil foi de 14,82 a cada 1.000 nascimentos, com grande variação de acordo com a região do país e uma prevalência mais alta entre as mais desfavorecidas. As regiões Norte e Nordeste tiveram as taxas de natimortalidade mais altas em comparação à região Centro-Oeste, que perdurou após o ajuste das diversas variáveis de confusão – incluindo nível de pobreza e etnia. A baixa idade e a obesidade maternas também estavam relacionadas a taxas de natimortalidade mais elevadas.
ConclusãoNo Brasil, a região influencia o risco de natimortalidade, com riscos muito mais altos no Norte e no Nordeste. A variação no nível socioeconômico não explica esse achado. Futuras pesquisas sobre o assunto devem explorar outras possíveis explicações como cuidado pré-natal e tipo de parto, bem como o papel dos sistemas de saúde público e privado com relação à natimortalidade. Estratégias de prevenção devem ser direcionadas a essas regiões historicamente desfavorecidas, como garantir acesso e qualidade da assistência durante a gravidez e perto do momento do nascimento.
Brazil is the largest country in South America, the fifth most populous in the world, and markedly heterogeneous in density and socioeconomic level.1,2 The country is divided into five geographic regions – North, Northeast, Center-West, Southeast, and South. There has been great improvement in health indicators and coverage of health services in Brazil in the recent past. For instance, 98% of births were overseen by skilled attendants in 2011 compared to 70% in 1991, and antenatal care (ANC) coverage was 98% in 2012. However, structural and social inequalities continue to be a major issue within the country, and there are still great differences in health outcomes among the five regions.3,4
New evidence from 2016, from the “Ending preventable stillbirths” series in the Lancet, shows stillbirth continues to be a problem worldwide. Comparing data from 2000 to 2015, there was progress, but the reduction was slower than that seen for maternal, neonatal, and post-neonatal deaths.5 The great majority of stillbirths occur in low-income countries, in the places with more socioeconomically disadvantaged residents. In many of these, data on stillbirths are scarce or even inexistent.6–10 Unfortunately, the Sustainable Development Goals – the United Nations agenda for addressing extreme poverty and its dimensions – did not implement a target for stillbirth.11 Thus, stillbirth remains an important topic for research and discussion.5
Although there have been studies investigating determinants of stillbirth in Brazil, most did not use data representative of the whole country or did not focus specifically in differences by region.12–18
Thus, this study aimed to measure the prevalence of stillbirth in different regions of Brazil and to investigate possible determinants of stillbirth in this population.
MethodsDatasetThis is a cross-sectional analysis using data from the National Survey on Demography and Health of Women and Children (Pesquisa Nacional de Demografia e Saúde da Criança e da Mulher [PNDS]) from Brazil in 2006. The PNDS represented the fifth phase of the Demographic and Health Surveys (DHS) Program. DHS surveys are nationally representative household surveys that provide data for monitoring and impact evaluation indicators.
The study population included women of reproductive age (15–49 years old) who had had a pregnancy in the past five years. The response rate was almost 90%. The sample was representative of the five regions of the country, including urban and rural areas.
The PNDS was approved for data collection in 2005 by the Research Ethics Committee of São Paulo. More details on sampling and ethical aspects regarding the data collection can be found elsewhere.19 For the purpose of the analysis presented here, the dataset was obtained from the public domain.20
The PNDS data were collected through a household survey using standardized questionnaires, applied by trained female interviewers according to DHS regulation on face-to-face interview.19
The outcome under investigation was stillbirth. According to the World Health Organization's (WHO) international comparison definition, stillbirths are babies delivered dead weighting 1000g or more, or at 28 weeks of gestation or more, or with body length of 35cm or more. They are classified into antepartum (death before onset of labor) and intrapartum (death after onset of labor and before birth) stillbirths.5,9,10
Information on pregnancies ending in the past five years was collected. Stillbirths were defined as a fetal death between 6 to 9 months of gestation. The weeks of gestation were not specified in the dataset.
Deprivation was measured according to The Brazilian Economic Classification Criteria, designed to estimate the purchasing power of families by separating the population into economic classes. Each household earns a number of points proportional to the number of goods it owns – such as color television, radio, bathroom, etc., the number of house cleaners, and the head of household educational level. The sum of these points puts the household into an economic class – A1, A2, B1, B2, C1, C2, D, and E, from least to most deprived. This classification is considered representative in economic terms, and was used in this study as an estimation of deprivation, following its previous use in the official DHS report. Economic classes A, B, and C were classified as “least deprived,” whereas D and E were classified as “most deprived.”21
For this analysis, women who reported miscarriages, ectopic pregnancies, or twins, and those who did not respond to questions about the outcome of pregnancy, were excluded.
Statistical analysisThe prevalence of stillbirth was calculated as the proportion of all births (live and still) ending in a stillbirth, presented per thousand with 95% confidence intervals (CI).
Maternal factors included region, deprivation, place of residence (urban or rural), age, education, parity, and ethnicity. Cross tabulations of maternal factors with the outcome of stillbirth used the chi-squared test. Logistic regression was used to assess the crude and adjusted associations between each maternal factor and stillbirth risk. Odds ratios (OR) were calculated alongside their 95% CI. Variables showing evidence of an association with stillbirth were considered as potential confounders – and included in the adjusted analysis, which used a stepwise model. A sensitivity analysis was conducted to determine if the variables not included in the adjusted model would change the association between exposures and outcome. This was done by adding the factors to the adjusted model one by one and observing the effect.
Analyses were performed using the Stata software package (StataCorp. 2013. Version 13. TX, USA). The survey (svy) group of commands was used to take into account the survey design.
ResultsThe initial dataset included 6833 pregnancies, reported by 5025 women. After excluding miscarriages, ectopic pregnancies, twins, and non-response regarding result of pregnancy and type of pregnancy, 6134 pregnancies reported by 4751 women were included in the final analysis. Of these, 6060 were live births and 74 were stillbirths.
The overall prevalence of stillbirth in the population was 14.82 stillbirths per 1000 births (Fig. 1).
The prevalence of stillbirth varied greatly among regions of the country (Fig. 1). The North region had a prevalence of 21.44/1000, the Northeast 25.85/1000, while the Center-West had a figure of 5.19/1000, the Southeast 8.24/1000, and the South 9.27/1000.
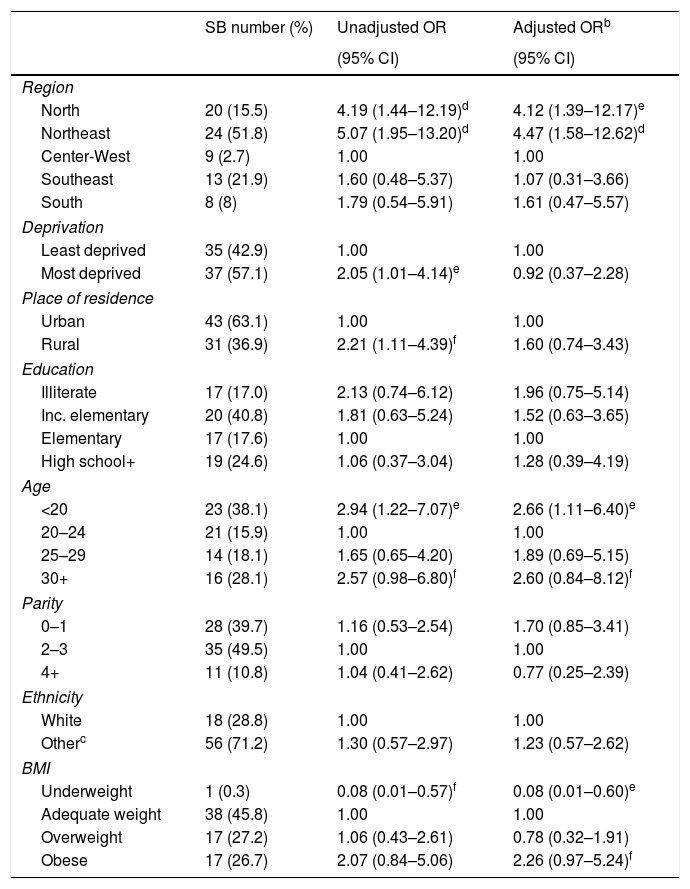
From the logistic regression analysis, the North region had more than four times the odds of stillbirth when compared to the Center-West region (OR [95% CI]: 4.19 [1.44–12.19]), while the Northeast region had more than five times the odds (OR [95% CI]: 5.07 [1.95–13.20]). After adjustment for the maternal factors deprivation, place of residence, education, age, parity, ethnicity, and body mass index (BMI), the association remained statistically significant for both the North (AOR [95% CI]: 4.12 [1.39–12.17]) and Northeast (AOR [95% CI]: 4.47 [1.58–12.62]) compared to the Center-West region (Table 1). Adjustment did not change the magnitude of the associations to any great extent.
Association of region and other maternal factors with stillbirth risk: crude and adjusted.a
| SB number (%) | Unadjusted OR | Adjusted ORb | |
|---|---|---|---|
| (95% CI) | (95% CI) | ||
| Region | |||
| North | 20 (15.5) | 4.19 (1.44–12.19)d | 4.12 (1.39–12.17)e |
| Northeast | 24 (51.8) | 5.07 (1.95–13.20)d | 4.47 (1.58–12.62)d |
| Center-West | 9 (2.7) | 1.00 | 1.00 |
| Southeast | 13 (21.9) | 1.60 (0.48–5.37) | 1.07 (0.31–3.66) |
| South | 8 (8) | 1.79 (0.54–5.91) | 1.61 (0.47–5.57) |
| Deprivation | |||
| Least deprived | 35 (42.9) | 1.00 | 1.00 |
| Most deprived | 37 (57.1) | 2.05 (1.01–4.14)e | 0.92 (0.37–2.28) |
| Place of residence | |||
| Urban | 43 (63.1) | 1.00 | 1.00 |
| Rural | 31 (36.9) | 2.21 (1.11–4.39)f | 1.60 (0.74–3.43) |
| Education | |||
| Illiterate | 17 (17.0) | 2.13 (0.74–6.12) | 1.96 (0.75–5.14) |
| Inc. elementary | 20 (40.8) | 1.81 (0.63–5.24) | 1.52 (0.63–3.65) |
| Elementary | 17 (17.6) | 1.00 | 1.00 |
| High school+ | 19 (24.6) | 1.06 (0.37–3.04) | 1.28 (0.39–4.19) |
| Age | |||
| <20 | 23 (38.1) | 2.94 (1.22–7.07)e | 2.66 (1.11–6.40)e |
| 20–24 | 21 (15.9) | 1.00 | 1.00 |
| 25–29 | 14 (18.1) | 1.65 (0.65–4.20) | 1.89 (0.69–5.15) |
| 30+ | 16 (28.1) | 2.57 (0.98–6.80)f | 2.60 (0.84–8.12)f |
| Parity | |||
| 0–1 | 28 (39.7) | 1.16 (0.53–2.54) | 1.70 (0.85–3.41) |
| 2–3 | 35 (49.5) | 1.00 | 1.00 |
| 4+ | 11 (10.8) | 1.04 (0.41–2.62) | 0.77 (0.25–2.39) |
| Ethnicity | |||
| White | 18 (28.8) | 1.00 | 1.00 |
| Otherc | 56 (71.2) | 1.30 (0.57–2.97) | 1.23 (0.57–2.62) |
| BMI | |||
| Underweight | 1 (0.3) | 0.08 (0.01–0.57)f | 0.08 (0.01–0.60)e |
| Adequate weight | 38 (45.8) | 1.00 | 1.00 |
| Overweight | 17 (27.2) | 1.06 (0.43–2.61) | 0.78 (0.32–1.91) |
| Obese | 17 (26.7) | 2.07 (0.84–5.06) | 2.26 (0.97–5.24)f |
The association between socioeconomic level and stillbirth found in the unadjusted analysis was not confirmed following adjustment for confounding factors, including the region. The same pattern was found for place of residence, with a crude association between rural residence and risk of stillbirth that was not confirmed following adjustment for confounding factors.
Younger mothers less than 20 years old had higher odds of stillbirth (SB) when compared to those aged 20–24, which remained after adjustment. (AOR [95% CI]: 2.66 [1.11–6.40]) (Table 1) There was some evidence that mothers over 30 years old had higher odds of stillbirth compared to mothers aged 20–24 (AOR [95% CI]: 2.60 [0.84–8.12]). Underweight women had lower odds of stillbirth compared to normal weight women (AOR [95% CI]: 0.08 [0.01–0.60]), and there was some evidence that obese women had higher odds of stillbirth compared to normal weight women (AOR [95% CI] 2.26 [0.97–5.24]).
DiscussionThe prevalence of stillbirth in the present cross-sectional study was 14.82 per 1000 births, which is slightly higher than that found for Latin American countries (13.2 per 1000 births),22 and lower than that found in studies conducted in maternity hospitals in the Northeast (24.4 per 1000 births)13 and Southeast (19.6 per 1000 births)17 regions of Brazil, around the same time period. One systematic review of studies on fetal death in Brazil, which included stillbirths, published between 2003 and 2013, found an overall reduction of fetal mortality rates in the period.14 Another study analyzing stillbirth rates in Brazil from 1996 to 2012 found a decrease from 13.4 to 10.0 per 1000 births.15
The present study found that stillbirth prevalence varied according to region of Brazil, with markedly higher figures in the North and Northeast compared to Southern regions. Region was the most important determinant of stillbirth, even after adjustment for deprivation level and other confounders. By November 2016, only one other study has showed the difference of stillbirth risk across regions in Brazil. In that study, the DATASUS, a database on health information in Brazil, was analyzed from 1996 to 2012, finding that the Northeast had the lowest decrease in stillbirth rate across time, while Northeast and North maintained the highest rates, which agrees with the findings presented here.15
Differences by region are an important topic in a continental country such as Brazil. The Southeast and South regions of Brazil have the highest population density, and the North and Northeast regions have the worse economic and social indices.23
The Brazilian health system is constituted by the Brazilian Unified Health System (Sistema Único de Saúde [SUS], in place since 1986) and the private system. The Family Health Program (Estratégia de Saúde da Família [ESF]) is a special arm of the public health system that aims to increase health coverage among disadvantaged groups.2 The social determinants of health, originating from the colonial legacies and impacting the current health, social, and economic inequities, play an important role in Brazil. The conditional cash transfer program (Bolsa Família), implemented in 2003, and later broadened as the Brazil without Misery Plan (Plano Brasil sem Miséria) in 2011, aimed to tackle these inequalities, and in general had a positive impact by facilitating access to health services by groups of the population who were traditionally excluded.24,25 Besides improvements in access to health care and in tackling social inequalities, Brazil remains a country of contrasts, in which many health-related issues can be associated to regional differences.
Access to internal household water and sanitation is much lower in the North compared to other regions, and there is a much lower ratio of physicians to population in both the North and Northeast. These figures show how the disparities affect the access to basic needs in Brazil.23 Moreover, a high turnover of professionals and lack of structure in careers can be associated with poor quality of care in the most disadvantaged settings.26
Stillbirth reflects maternal health status, accessibility to health care, and quality of care delivered, including antenatal and intrapartum care. The WHO has been working to include antepartum stillbirths and intrapartum stillbirths as indicators for quality of ANC and quality of care at birth, respectively.11 The higher risk of stillbirth in the North and Northeast presented here could be related to poor quality of health care delivered during pregnancy and around the time of birth.
As pointed by Lansky et al., despite Brazil having increasingly medicalized deliveries, the high rates of maternal and perinatal mortality (which includes stillbirth and early neonatal deaths) persist, possibly related to poor quality of care around time of birth and inadequate procedures. In their study of neonatal mortality in Brazil between 2011 and 2012, rates were high in the North and Northeast, with findings indicating unsatisfactory quality of health care.27
According to previous research, indicators of access to ANC and the presence of a skilled attendant at delivery has improved in Brazil recently.3,4 However, even if women are followed throughout pregnancy, at-risk pregnancies are identified, and there is professional care for childbirth, if quality of care delivered is not standard, stillbirths which could be prevented can occur. The previously studied misplaced use of cesarean-sections, the under-use of recommended practices such as the partograph, for labor monitoring, and the use of practices that diminish the mother's role and autonomy are examples of problems that persist.27 High-quality prenatal care, with early identification of at-risk pregnancies, and adequate care around time of birth are necessary to reduce stillbirths. This should involve multidisciplinary teams, following protocols and recommended practices during labor and delivery. Moreover, the promotion and evaluation of interventions, and monitoring of service indicators, is imperative.
The stillbirth burden worldwide is also higher in rural areas, traditionally associated to socioeconomically disadvantaged, hard-to-reach populations.5 According to Viellas et al., who studied women delivering at hospitals in Brazil, barriers to attending prenatal care included being indigenous and black, having less education, having a higher number of pregnancies, and living in the North and Northeast.4 In Brazil, women living in resource poor settings such as the rural North and Northeast regions possibly have less access to antenatal and intrapartum care, with delayed or even inexistent hospital care. This can lead to unassisted home deliveries, possibly contributing to an even higher stillbirth risk in these areas. The WHO recommendations on ANC for a positive pregnancy experience, from 2016, highlight context-specific recommendations to improve the utilization and quality of ANC, some of which could serve as base to interventions for rural, hard-to-reach Brazilian areas. The use of ANC home visits organized through community mobilization can impact on ensuring continuity of care for pregnant women, but should not replace ANC visits. Also, recruitment and retention of health staff in remote areas is crucial to improve ANC. Recommendations for action include implementation of students’ clinical rotations in these areas, and providing better conditions for health workers, such as safe living and working environments, as well as cooperation with better-served areas through tele-health services.28
Other findingsOther determinants of stillbirth found to be relevant were high and low maternal age, with a higher risk of stillbirth for mothers younger than 20 and a tendency to increased risk of stillbirth in those older than 40. These findings agree with the classical determinants of stillbirth reported in many previous studies, which include high and low maternal age, as well as low gestational age at birth, high parity, lack of or inadequate ANC, lack of a skilled attendant at delivery, low socioeconomic status, and poor nutrition, among others.6,8,29 Maternal obesity showed a tendency to be associated with increased risk of stillbirth, a finding which has been reported in previous studies.16,30
Deprivation was previously proposed as a determinant of stillbirth.6 In this analysis, the crude association between deprivation and stillbirth did not remain after adjustment for region of the country, suggesting that region determines stillbirth more strongly than deprivation, through other pathways, possibly unmeasured factors such as use and access to ANC, type and place of delivery, and presence of a skilled attendant at birth. Further analysis of this association stratified by region could not be performed due to low numbers in the sample.
Similarly, ethnicity was not found to be a determinant of stillbirth in this study. This could be due to the fact that despite the persistence of ethnic inequalities, gaps are being narrowed progressively in Brazil. However, the possibility of underreporting has to be considered. As self-reported questionnaires were used, with skin color as a proxy for ethnicity, there could be misclassification, potentially underestimating the role of ethnicity as a determinant of stillbirth.
LimitationsThere were some limitations in this study that deserve mention. The relatively small numbers in the sample reduced statistical power. Also, because some maternal and clinical information was not collected, it could not be included in the analysis. It would have been useful to have information on the timing of stillbirth, use of ANC, presence of a skilled attendant at delivery, type and place of delivery, HIV status, and other maternal infections. As these factors could not be accounted for, conclusions are limited regarding explanations for the regional differences in prevalence observed in this study.
The different criteria used to define stillbirth remain an issue globally.11 Also, the correct measurement of stillbirth is key to the development of interventions and monitoring of strategies already in place. In this study, stillbirth was measured by a questionnaire based on self-report. As stillbirth is known to be subject of underreporting, the possibility of misclassification between antepartum stillbirth and miscarriages, and between intrapartum stillbirths and early neonatal deaths, has to be considered. Furthermore, time of delivery for the stillbirths was not specified in weeks, but in months, therefore not standardized according to the WHO comparison definition.
However, the major strength of this study is that the data are representative of the whole country, providing a general view of stillbirth risk across Brazil. The questionnaires were collected by trained female interviewers according to DHS regulation regarding face-to-face interviews, which contributed to reliability.
Stillbirth risk varies by region in Brazil, with higher risks in the North and Northeast. This variation is not explained by socio-demographic factors, including deprivation level.
Important unmeasured factors such as use of ANC, timing of stillbirth, presence of a skilled attendant at birth, and place of delivery could be possible explanations for such higher risk in the North and Northeast.
This finding suggests that health professionals and policy makers should look at these historically disadvantaged regions more carefully, and direct preventive strategies at them. When aiming to reduce stillbirths in these regions, there are two measures that should be addressed:
- •
Guarantee delivery of standard quality of care, throughout pregnancy until the moment of delivery, following practices that meet scientific evidence-based recommendations, and performing evaluation of interventions and monitoring of service indicators.
- •
Target the most in-need populations in the most affected regions, aiming for continuity of care for pregnant women in hard-to-reach areas, and improving conditions for health workers to stay in the rural and remote areas.
Much has been done in Brazil to tackle social and regional inequalities. However, it is still notable that the health care delivered is not the same for all and there is still much room for improvement.
Further research on the association between region and stillbirth in Brazil should explore the use and quality of antenatal and intrapartum care, as well as other possible explanatory factors. Furthermore, examining how health care is delivered by region, and how private and public health systems interact in determining stillbirth, is recommended.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Carvalho TS, Pellanda LC, Doyle P. Stillbirth prevalence in Brazil: an exploration of regional differences. J Pediatr (Rio J). 2018;94:200–206.