To investigate the determinants of dyslipidemia in preschoolers.
MethodsA total of 227 preschoolers residing in an urban area of the city of Diamantina, Minas Gerais, Brazil were evaluated at age 5 years, using a cross-sectional design. Dietary intake from a food frequency questionnaire, anthropometric/biochemical parameters, and socioeconomic/behavioral information from a questionnaire were evaluated. ‘Mixed diet’, ‘snack’, and ‘unhealthy’ dietary patterns were identified using principal component analysis. The determinants of dyslipidemia were examined using Poisson regression analysis.
ResultsThe prevalence of dyslipidemia in this study was 65.19%. Preschoolers who less frequently consumed foods in the ‘mixed diet’ dietary pattern had a higher risk of high concentrations of low-density lipoprotein cholesterol (PR=2.30; p=0.004) when compared with those with more frequent consumption of the ‘mixed diet’ dietary pattern. Preschoolers whose mothers had lower levels of education presented a lower risk of high concentrations of low-density lipoprotein cholesterol (PR=0.43; p=0.003), and preschoolers who were overweight/obese presented with greater risk of high concentrations of low-density lipoprotein cholesterol (PR=2.23; p=0.003).
ConclusionThe determinants of dyslipidemia identified in this study were less frequent consumption of foods in the ‘mixed diet’ dietary pattern, higher body mass index, and lower level of maternal education. This study shows that despite the young age of the group under study, they already present a high prevalence of dyslipidemia, which is an important risk factor for cardiovascular disease.
O objetivo deste estudo foi investigar os determinantes de dislipidemia em pré-escolares.
MétodosA partir de um desenho transversal, foi avaliado um total de 227 pré-escolares com 5 anos de idade residentes em uma área urbana da cidade de Diamantina, Minas Gerais, Brasil. Foram avaliados: variáveis bioquímicas, antropométricas, condição socioeconômica e comportamental, a partir de um questinário; e ingestão alimentar, a partir de um questionário de fequência de consumo de alimentos. Os padrões alimentares denominados “dieta mista”, “fast food” e “não saudável” foram identificados por meio de análise de componentes principais. Os determinantes de dislipidemia foram examinados através da análise de regressão de Poisson.
ResultadosA prevalência de dislipidemia, neste estudo, foi de 65,19%. Os pré-escolares que consumiam com menos frequência alimentos do padrão “dieta mista” tiveram um risco maior de concentrações mais altas de lipoproteína de baixa densidade (PR=2,30; p=0,004), em comparação com aqueles com um consumo mais frequente do padrão “dieta mista”. Os pré-escolares cujas mães apresentaram uma escolaridade mais baixa tiveram um menor risco de concentrações mais altas com lipoproteína de baixa densidade (PR=0,43; p=0,003), e os pré-escolares que estavam com sobrepeso/obesos apresentaram maior risco de concentrações mais altas de lipoproteína de baixa densidade (PR=2,23; p=0,003).
ConclusãoOs determinantes de dislipidemia identificados neste estudo foram o consumo menos frequente de alimentos do padrão “dieta mista”, índice de massa corporal mais alto e um maior nível de escolaridade materna. Este estudo mostra que, apesar da baixa idade do grupo em estudo, já estão apresentando alta prevalência de dislipidemia, que é um fator de risco importante para doença cardiovascular.
Dyslipidemia is a disorder of lipoprotein metabolism that results in elevation of plasma lipid levels, such as high total cholesterol (TC), high low-density lipoprotein cholesterol (LDL-c), low high-density lipoprotein cholesterol (HDL-c), and high triacylglycerol (TAG).1 In children and adolescents, dyslipidemia is also defined as having a TC, LDL-c, and/or TAG level higher than the 95th percentile or an HDL-c level lower than the 10th percentile for age and gender.2
The prevalence of dyslipidemia in children and adolescents has been high in most countries. According to Al-Shehri,3 dyslipidemia's prevalence varies worldwide from 2.9% to 33% when defining the disease as having a TC level above 200mg/dL. Studies conducted with children and adolescents in Brazil between 2000 and 2010 observed prevalence rates from 10% to 60.6%.4-10
Abnormal levels of lipids and lipoproteins are associated with indirect markers of atherosclerosis, including endothelial dysfunction assessed by flow-mediated dilation in the brachial artery and increased carotid intima-media thickness (cIMT).11 Pediatric elevations of TC, LDL-c, TAG, and the ratio of TC/HDL-c are correlated with increased cIMT and coronary artery calcium during adulthood.12
The majority of the cases of dyslipidemia in children and adolescents are related to obesity,13–17 high waist-to-hip ratio, family history of dyslipidemia,17 and lifestyle factors such as high consumption of unhealthy dietary patterns,18–20 meals rich in cholesterol and energy21 and low intake of unsaturated fatty acids.22
Research into determinants of dyslipidemia in Brazilian preschoolers that includes dietary patterns as an explanatory variable has not been conducted yet. Thus, the aim of the present study was to investigate the determinants of dyslipidemia in preschoolers by including dietary patterns, since they can predict disease risk better than single foods or nutrients. The use of dietary patterns makes it possible to identify the cumulative effect of various nutrients on health.
MethodsType of study and locationThis study used a cross-sectional design nested in a cohort of children who were born in the urban area of the city of Diamantina, Minas Gerais, Brazil, and resided there between September of 2004 and July of 2005.23 This study23 aimed to follow the growth and development of this cohort in their first year of life. The newborns’ parents were contacted in their homes during the first weeks of life. The recruitment was conducted using the Statement of Live Birth recorded by one of the two hospitals in the city of Diamantina.
Diamantina is a municipality located in the Vale do Jequitinhonha in Minas Gerais, Brazil, that has a mortality rate of 32.8 deaths per 1,000 births among children under one year old, a literacy rate of 83.4%, a human development index (HDI) of 0.748, and an income HDI of 0.752.24
Subjects and study protocolAt the beginning of the present study, all children were aged 5 years±5 months. They were recruited after an informed consent was obtained from their parents/guardians. This research was conducted from July of 2009 to July of 2010, and data collection was conducted by four nutritionists and one student. Each preschooler was visited in his/her home.
Previous work recommended having five individual per food group listed on the food frequency questionnaire (FFQ), in order to identify dietary patterns.25 In the present study, 24 food groups were identified, thus 120 individuals (5 x 24 groups) were needed for this study. Data from 227 preschoolers were obtained, which was considered a satisfactory sample for the present study.
This study aimed to analyze the determinants of dyslipidemia in addition to identifying dietary patterns, so power for the sample was calculated. Power was calculated post-hoc by using a Poisson regression to estimate the parameter risk difference from being overweight/obese, which was 2.11. The power obtained was 99%, using the statistical software G*Power.26
This study was conducted according to the guidelines presented in the Declaration of Helsinki, and all procedures involving human subjects were approved by the Ethics Committee of the Universidade Federal de Minas Gerais (ref. No. ETIC 545/08). An informed consent was obtained from the preschoolers’ parents or guardians.
Anthropometric indicatorEach child's anthropometric status was evaluated by measuring weight and height to obtain the body mass index (BMI). Weight was measured utilizing a portable electronic digital scale with a 150kg capacity that measured increments of 50g. Height was measured using a portable stadiometer with a degree of precision of 0.1cm. The procedures adopted for these measurements followed the protocols recommended by Jelliffe.27
These measurements were taken in a laboratory of the Department of Nursing of the Universidade Federal dos Vales do Jequitinhonha e Mucuri (UFVJM) in the morning with fasting children, and all measurements were performed on a single occasion.
The cut-off point of ≥+1 z-score identified preschoolers with elevated body mass index (overweight or obese) for their age using BMI/age.28 To identify z-scores for each child, the World Health Organization(WHO) Anthro and Anthro plus softwares, versions 3.0.1 and 1.0.3, respectively, were used (WHO - Geneva).
Dietary patternsDietary patterns (DP) were identified using dietary information collected from a food frequency questionnaire (FFQ) created by Sales et al.29 Before its use, a pilot test was conducted to assess the adequacy of the FFQ for the research. Any foods not mentioned by the preschoolers’ families were excluded, and others were added to the FFQ after the pilot. Details of the food groupings and factor analysis used to generate the dietary patterns are described elsewhere.30
The dietary patterns are presented as a discrete variable. First, the sum of the frequency of consumption of foods contained in each group was calculated. Then, participants were categorized by a dichotomous variable (0 or 1) according to whether they had a value above (1) or below (0) the first quartile frequency of consumption for each food group.
Biochemical indicatorVenous blood samples for quantification of serum TC, LDL-c, HDL-c, and TAG were collected by a trained professional in the morning, between 7:00 and 9:00 a.m., following a fasting period of 10 to 12hours. Biosafety principles were observed for this collection.
The values for TC, HDL-c, and TAG were obtained utilizing a Cobas Mira Plus device, and were analyzed via absorption photometry using the enzymatic method. LDL-c was determined through calculation using the Friedwald formula while observing the limitations of this methodology.
The cut-offs used to assess the serum levels of TC, TAG, LDL-c, and HDL-c were based on national recommendations.31 Elevated levels of TC and LDL-c were defined as ≥170mg/dL and ≥130mg/dL, respectively. TAG levels ≥130mg/dL were considered elevated, and HDL-c levels <45mg/dL were considered low. Dyslipidemia was defined as the preschooler presenting abnormal levels of any of these parameters.
Other evaluationsInformation regarding factors possibly associated with alterations in the lipid profile was obtained from a questionnaire completed by the child's mother or caregiver at home. This questionnaire provided information about the family's monthly income, maternal education, and behavioral characteristics of the child, such as time spent watching TV.
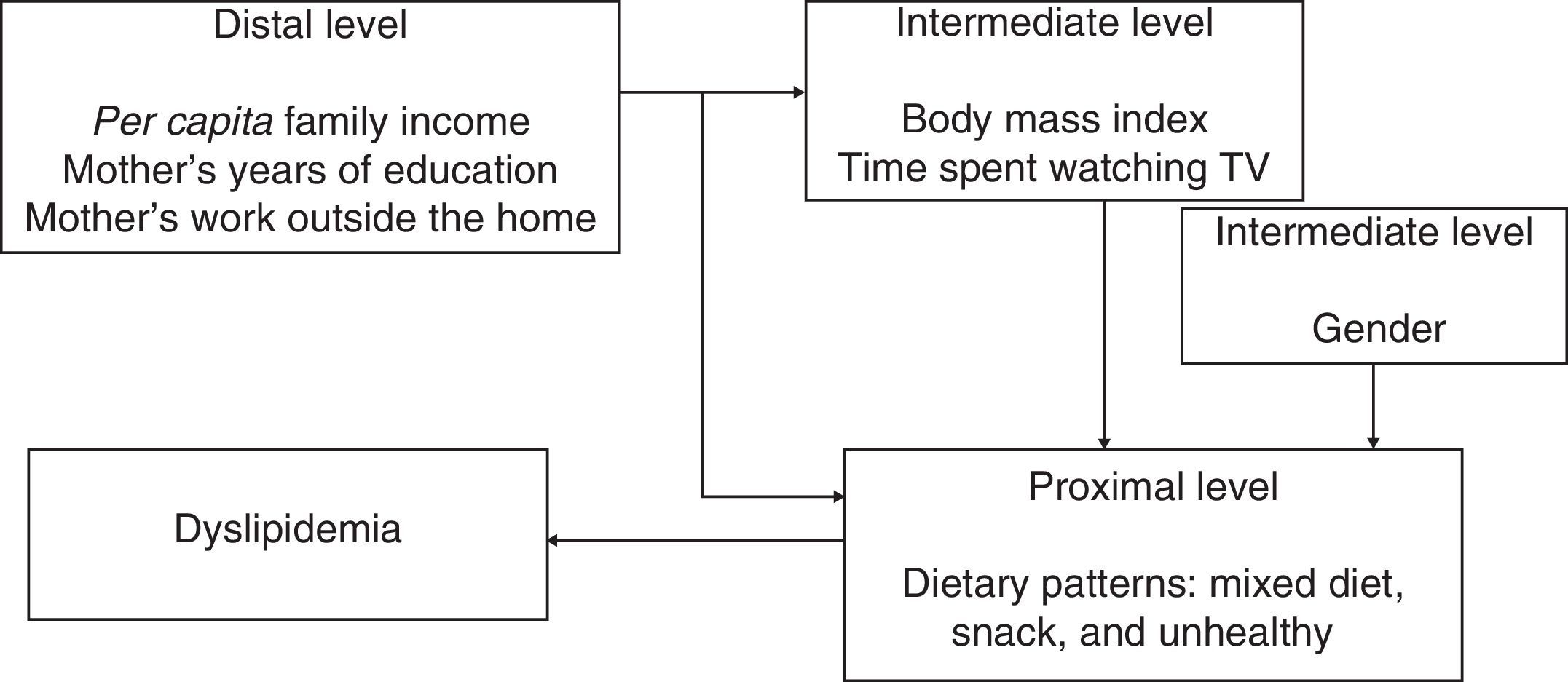
Statistical analysisPoisson regression was used to evaluate determinants of dyslipidemia. The variables that presented a p-value < 0.2 in the bivariate analysis were included in a multivariate analysis, and a p-value < 0.05 was considered to be associated with dyslipidemia in the multivariate analysis. This analysis followed a hierarchical approach for the determination of significant factors32 (Fig. 1). The database was constructed in Excel. Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) (SPSS Inc. - Chicago, IL, USA) for Windows, version 19.0.
ResultsOf the 227 preschoolers evaluated, 147 (64.7%) presented with dyslipidemia. Among those, 121 (81.7%) had low levels of HDL-c. High levels of TC, LDL-c, and TG were present in 73 (49.3%), 45 (30.4%), and six (2.6%) preschoolers, respectively.
Three dietary patterns were identified: ‘mixed diet’ consisted of food groups typical of a Brazilian diet; ‘snack’ consisted of baked food groups that usually do not require preparation for consumption; and ‘unhealthy’ consisted of sweets and foods rich in lipids and carbohydrates. The ‘mixed diet’ pattern explained a higher percentage of variance, and was the pattern that best represented the food intake of the sample analyzed.
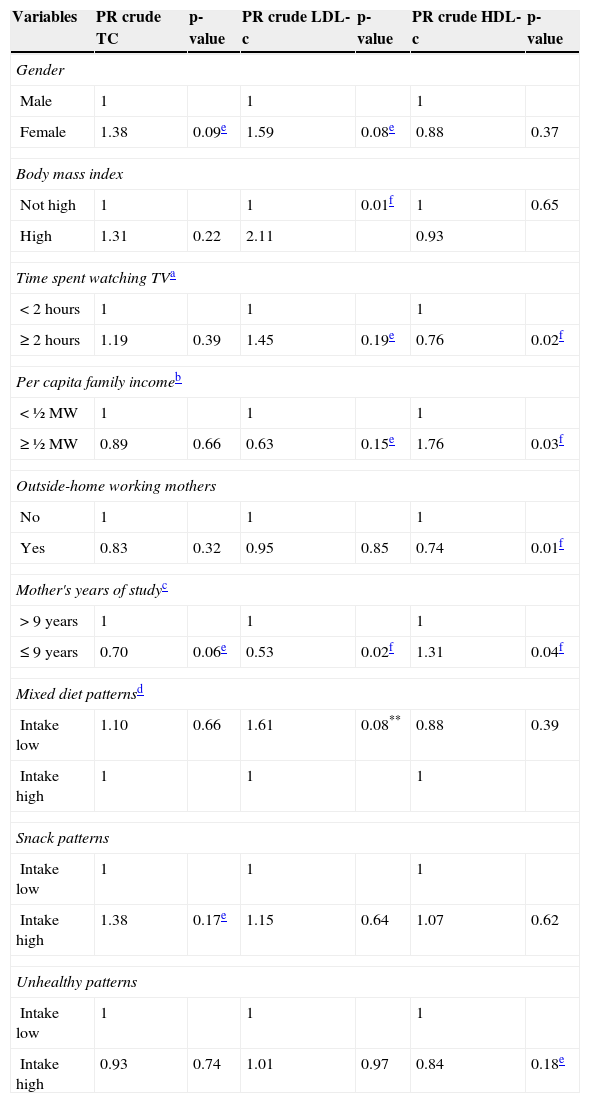
Table 1 shows the crude prevalence ratios for dyslipidemia according to the socioeconomic, anthropometric, and behavioral characteristics and dietary patterns. This table demonstrates that LDL-c was the lipid associated with the greatest number of variables, followed by HDL-c and TC. Isolated hypertriglyceridemia was not associated with any variable studied, and the results were not presented.
Crude prevalence ratios (PR) and respective p-values of variables associated with altered lipid profiles of preschoolers from Diamantina, Minas Gerais, Brazil.
| Variables | PR crude TC | p-value | PR crude LDL-c | p-value | PR crude HDL-c | p-value |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Male | 1 | 1 | 1 | |||
| Female | 1.38 | 0.09e | 1.59 | 0.08e | 0.88 | 0.37 |
| Body mass index | ||||||
| Not high | 1 | 1 | 0.01f | 1 | 0.65 | |
| High | 1.31 | 0.22 | 2.11 | 0.93 | ||
| Time spent watching TVa | ||||||
| <2hours | 1 | 1 | 1 | |||
| ≥2 hours | 1.19 | 0.39 | 1.45 | 0.19e | 0.76 | 0.02f |
| Per capita family incomeb | ||||||
| <½ MW | 1 | 1 | 1 | |||
| ≥½ MW | 0.89 | 0.66 | 0.63 | 0.15e | 1.76 | 0.03f |
| Outside-home working mothers | ||||||
| No | 1 | 1 | 1 | |||
| Yes | 0.83 | 0.32 | 0.95 | 0.85 | 0.74 | 0.01f |
| Mother's years of studyc | ||||||
| >9 years | 1 | 1 | 1 | |||
| ≤9 years | 0.70 | 0.06e | 0.53 | 0.02f | 1.31 | 0.04f |
| Mixed diet patternsd | ||||||
| Intake low | 1.10 | 0.66 | 1.61 | 0.08** | 0.88 | 0.39 |
| Intake high | 1 | 1 | 1 | |||
| Snack patterns | ||||||
| Intake low | 1 | 1 | 1 | |||
| Intake high | 1.38 | 0.17e | 1.15 | 0.64 | 1.07 | 0.62 |
| Unhealthy patterns | ||||||
| Intake low | 1 | 1 | 1 | |||
| Intake high | 0.93 | 0.74 | 1.01 | 0.97 | 0.84 | 0.18e |
HDL-c, low high-density lipoprotein cholesterol; LDL-c, high low-density lipoprotein cholesterol; MW, Brazilian minimum wage; TC, total cholesterol.
It is worth mentioning that in the ‘mixed diet’ pattern, which can be considered protective against alteration of the lipid profile, ‘low intake’ was categorized as a 1. For the other patterns, which can be considered higher risk for alterations of the lipid profile, ‘high intake’ was categorized as 1.
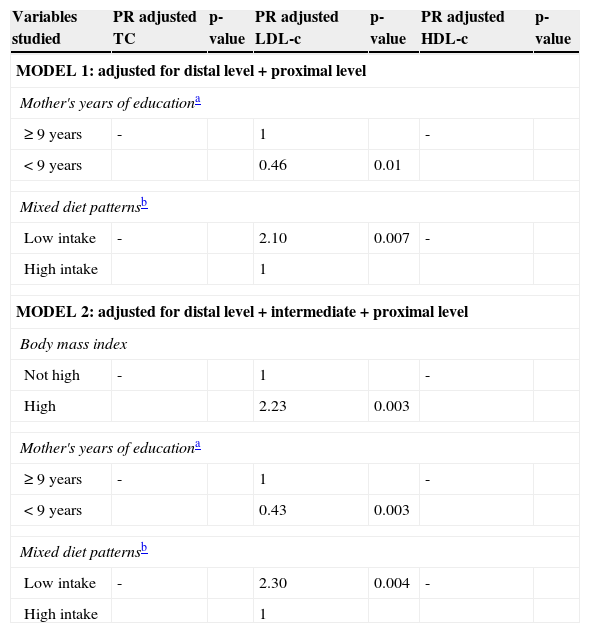
The regression analysis, adjusted for factors associated with dyslipidemia, is presented in Table 2. Considering the hierarchical framework proposed, which examines the determinants of dyslipidemia among the studied preschoolers, two models were extracted. In model 1, a significant association was found for higher levels of LDL-c, lower maternal education, and low frequency of intake of the ‘mixed diet’ dietary pattern.
Adjusted prevalence ratios (PR) and respective p-values of variables associated to the alteration in lipid profile of preschoolers. Diamantina, Minas Gerais, Brazil.
| Variables studied | PR adjusted TC | p-value | PR adjusted LDL-c | p-value | PR adjusted HDL-c | p-value |
|---|---|---|---|---|---|---|
| MODEL 1: adjusted for distal level + proximal level | ||||||
| Mother's years of educationa | ||||||
| ≥9 years | - | 1 | - | |||
| <9 years | 0.46 | 0.01 | ||||
| Mixed diet patternsb | ||||||
| Low intake | - | 2.10 | 0.007 | - | ||
| High intake | 1 | |||||
| MODEL 2: adjusted for distal level + intermediate + proximal level | ||||||
| Body mass index | ||||||
| Not high | - | 1 | - | |||
| High | 2.23 | 0.003 | ||||
| Mother's years of educationa | ||||||
| ≥9 years | - | 1 | - | |||
| <9 years | 0.43 | 0.003 | ||||
| Mixed diet patternsb | ||||||
| Low intake | - | 2.30 | 0.004 | - | ||
| High intake | 1 | |||||
HDL-c, low high-density lipoprotein cholesterol; LDL-c, high low-density lipoprotein cholesterol; PR, prevalence ratios; TC, total cholesterol; Trace, variable not associated with lipid abnormality in question.
In model 2, high levels of LDL-c were associated with lower maternal education (PR=0.43; p=0.003), higher BMI (PR=2.23; p=0.003), and low frequency of intake of the ‘mixed diet’ dietary pattern (PR=2.30; p=0.004). In this analysis, high levels of TC and low HDL-c were not associated with any variable.
Of the 281 children in the original cohort, 232 (82.56%) were included in the study. The loss of 17.33% during follow-up was due to families moving away from the area (n=37; 75.51%), incorrect addresses (n=8, 16.33%); and family refusal to participate (n=4; 8.16%). Five parents did not allow their children to provide blood samples, so this study presents results for the remaining 227 preschoolers.
DiscussionThe findings of the present study are important warnings that dyslipidemia is part of a worrying reality that needs to be investigated at an early age, such as during preschool. Furthermore, these findings corroborate studies that have shown an increase in the number of cases of this disorder in Brazilian children and adolescents.4–10 Is important to mention that the some publications4–6 about alterations in lipid profiles in Brazilian children and adolescents used cutoff points proposed by the NCEP21 and recommendations by the III Brazilian guidelines on dyslipidemia,1 and others7–10 used the 1st Brazilian guideline for prevention of atherosclerosis in childhood and adolescence (IDPAIA)31
Some international publications on this topic have described how alterations in the lipid profiles of children are also a reality in other countries,13–15,17,33–36 but at much lower prevalence than in research reported in Brazil and in the present study.
In this study, the higher prevalence of alterations in lipid profiles was found to be associated with low levels of HDL-c and high levels of LDL-c. These lipoproteins are involved, respectively, in the protection against and formation of atherosclerosis. Individuals with low levels of HDL-c have a higher risk of developing atherosclerosis because this lipoprotein is responsible for various actions that contribute to protection against atherosclerosis.1 LDL-c is the main atherogenic lipoprotein; its oxidation is the key mechanism in the pathophysiology of an atheroma. Individuals with high levels of LDL-c may present with early clinical manifestations of atherosclerosis.
It is worth mentioning that the lipid profile of children in this study was classified according to the category “increased” on the IDPAIA,31 which favored a higher prevalence of low HDL-c. The IDPAIA uses a raised cutoff point for this lipoprotein. This cutoff point may be inappropriate for this age group, since high levels of HDL-c occur in the presence of increased consumption of fruits and vegetables and physical activity, which are characteristics that are difficult to achieve in this age group.
Among the variables evaluated, three were associated with dyslipidemia (elevated levels of LDL-c) in preschoolers: less frequent consumption of the ‘mixed diet’ dietary pattern, overweight/obesity, and having a mother with lower levels of education. The ‘mixed diet’ pattern represents a balanced diet because it consists of foods from all food groups and follows the principles of a healthy diet. Therefore, less frequent consumption may represent a risk factor for elevated levels of LDL-c. Some foods contained in this dietary pattern admittedly provide greater protection against altered lipid profile,31 such as leafy vegetables and fruits. Leafy vegetables (r=0.656) and fruits (r=0.618) showed higher correlations with this AP, which probably explains why less frequent consumption of this dietary pattern was significantly associated with increased levels of LDL-c.
It is interesting to note that some studies18,20,37–39 that evaluated the relation between AP and dyslipidemia found that this problem was associated with more frequent consumption of a ‘Western’ dietary pattern. This pattern is usually composed of foods like red meat, eggs, refined grains, cafeteria foods, hamburgers, mayonnaise, biscuits, cakes, pies, chocolates, and soft drinks. In this study, while unhealthy patterns were also identified, they not were associated with dyslipidemia.
The association between overweight/obesity and dyslipidemia has been identified in several studies.4,9,10,14–16 The Bogalusa Heart Study,15 conducted in the United States with children and adolescents, found that obese children had 2.4 times and 7.1 times greater chances of having higher levels of total cholesterol and triglycerides, respectively, than children who were not obese. In a study conducted in Brazil, Coronelli et al.16 observed that obese children had a 2.17 times greater risk of hypercholesterolemia than non-obese children. Alcântara Neto et al.9 observed a significant positive association between dyslipidemia and overweight (OR =3.40) in children and adolescents in the city of Salvador, Bahia.
However, in a study with schoolchildren also residing in the city of Diamantina, MG, Barbosa et al.10 observed that the correlation between lipid profile (TC, TG, and HDL-c) and anthropometric and body composition parameters was weak. This finding was despite the fact that TC was positively correlated with body fat percentage, whereas HDL-c was negatively correlated with waist-hip ratio in both boys and girls.
According to Asayama et al.,14 the association between body mass and dyslipidemia has multiple metabolic causes: insulin resistance, hyperinsulinemia, hyperglycemia, and increased protein for transferring cholesterol esters secreted by adipocytes, among other factors.
Another variable associated with dyslipidemia in this study was low maternal education, which exerted a protective effect. This result can be contradictory if it is considered that mothers with lower education may have lower income and less access to information about a balanced diet, which may result in leaving their children more exposed to an unhealthy diet. However, it was observed that the preschoolers with mothers with lower education more often consumed the ‘mixed diet’ dietary pattern, and this pattern was considered protective against dyslipidemia.
In addition, when a more detailed analysis was performed to understand this relationship, it was observed that the factor that is really influencing this analysis was the lower per capita income, and whether the child attended school. That is, low maternal education only remained associated with more frequent consumption of the ‘mixed diet’ dietary pattern for preschool children attending schools (OR=4.27) and those with lower per capita income (OR=3.56).30 This means that the children of mothers with lower education who also had lower incomes and were attending school had less access to processed foods high in fats and sugars and less access to fast food, which put children at the highest risk for dyslipidemia. Moreover, children attending schools eat more balanced meals and likely to be exercising more.
There are some limitations to this study. The most important limitation concerns the assessment of the usual food intake of preschoolers and time spent watching television. Obtaining accurate information on these topics was difficult because most mothers worked outside the home (62.5%), and their children attended school (88.79%). It was difficult for mothers to accurately report what their children eat during the day, and their time spent on each activity. However, it is likely that studies with young children should take these factors into consideration.
The determinants of dyslipidemia identified in this study were less frequent consumption of foods in the ‘mixed diet’ dietary pattern, higher BMI, and lower levels of maternal education. This study shows that, despite the young age of the group under study, they are already presenting a high prevalence of dyslipidemia, which is an important risk factor for cardiovascular disease. This finding indicates the need to stimulate behavioral change, which can include public policies to fight against inappropriate dietary patterns and prevent diseases that accompany these practices. Children should be the target group of these policies because eating habits are formed in childhood. Inadequate habits that are incorporated in this phase of life and that increase in adolescence may augment the appearance of diseases in adulthood.
FundingFundação de Amparo à Pesquisa do Estado de Minas Gerais – FAPEMIG (Process number: APQ-00428-08).
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Nobre LN, Lamounier JA, Franceschini SC. Sociodemographic, anthropometric and dietary determinants of dyslipidemia in preschoolers. J Pediatr (Rio J). 2013;89:462–9.