This study aimed to evaluate the first episode of unprovoked epileptic seizure in children and assess recurrence risk factors.
MethodsThis was a retrospective observational study, based on the analysis of medical records of patients admitted between 2003 and 2014, with first epileptic seizure, at the pediatric service of a secondary hospital. The data were analyzed using the SPSS 20.0 program.
ResultsOf the 103 patients, 52.4% were boys. The median age at the first seizure was 59 (1–211) months. About 93% of children were submitted to an electroencephalogram at the first episode and 47% underwent neuroimaging assessment. Treatment with an antiepileptic drug was started in 46% of patients. The recurrence rate was 38% and of these, 80% had the second seizure within six months after the first event. Of the assessed risk factors, there was a statistically significant association between seizure during sleep and recurrence (p=0.004), and between remote symptomatic etiology seizure and occurrence of new seizure (p=0.02). The presence of electroencephalogram abnormalities was also associated with the occurrence of new seizures (p=0.021). No association was found between age, duration of the seizure, and family history of epilepsy with increased risk of recurrence.
ConclusionsMost children with a first unprovoked epileptic seizure had no recurrences. The risk of recurrence was higher in patients with seizure occurring during sleep or remote symptomatic ones and those with abnormal electroencephalogram results.
Este trabalho teve como objetivos estudar o primeiro episódio de crise epilética não provocada em idade pediátrica e avaliar os fatores de risco de recorrência.
MétodosEstudo observacional retrospectivo, baseado na análise dos processos clínicos dos pacientes internados entre 2003 e 2014, num serviço de pediatria de um hospital de nível 2, com primeira crise epilética. Os dados foram trabalhados com o programa SPSS Statistics 20.0.
ResultadosDos 103 pacientes, 52,4% eram meninos. A mediana da idade da primeira crise foi 59 (1-211) meses. Cerca de 93% das crianças realizaram eletroencefalograma no primeiro episódio e 47% realizaram neuroimagem. O tratamento com fármaco antiepilético foi instituído em 46% dos pacientes. A taxa de recorrência foi 38% e, destes, 80% tiveram a segunda crise nos 6 meses seguintes após o primeiro evento. Dos fatores de risco estudados verificou-se uma relação estatisticamente significativa entre a crise durante o sono e a recorrência (p=0,004), assim como entre as crises de etiologia sintomática remota e a ocorrência de novas crises (p=0,02). A presença de anormalidades no eletroencefalograma também esteve associada à ocorrência de novas crises (p=0,021). Não se encontrou relação entre idade, duração da crise e história familiar de epilepsia com risco aumentado de recorrência.
ConclusõesA maioria das crianças com uma primeira crise epilética não provocada não teve recorrências. O risco de recorrência foi superior nos pacientes com crise durante o sono ou crise sintomática remota e naqueles com eletroencefalograma alterado.
Epileptic seizures are one of the most common neurological problems in children. It is estimated that approximately 50% of children and adolescents who have a first epileptic seizure will have one recurrence.1 Knowledge of the natural history after a first unprovoked epileptic seizure and risk factors for recurrence are essential to establish treatment and follow-up criteria. Over the years, several authors have suggested recurrence predictors,2–4 such as age at the first seizure, gender, family and perinatal history, seizure characteristics, and electroencephalogram (EEG) results, among others. However, the studies are not always consensual and those found in Portugal on this topic are still scarce. Pereira et al.5 evaluated 200 children with a first episode of unprovoked epileptic seizure during a 15-year period. According to their study, which was carried out in Portugal, 30% of the children developed epilepsy, with focal seizures and EEG alterations being associated with increased risk of recurrence. These authors found no association between history of febrile seizures, neonatal complications, and family history of epilepsy with increased risk of recurrence.
The present study aimed to assess the first episode of unprovoked epileptic seizure in pediatric patients, as well as the recurrence risk factors.
MethodsStudy design and population sampleThis was a retrospective observational study, based on the assessment of medical records of patients admitted to a secondary hospital in Portugal between October 2003 and June 2014. This study included patients at the pediatric age range (<18 years) with a suspected first episode of epileptic seizure. Patients younger than 28 days of life and those in whom an acute causative factor for the seizure was identified were excluded. Children with seizures with symptomatic etiology in whom an acute causative factor was not identified were included.
Study protocolThe definitions used were based on the criteria and classifications published by the International League Against Epilepsy (ILAE),6 after some adjustments. The diagnosis of first unprovoked epileptic seizure was established by the physician who treated the child, considering the described and/or displayed signs and symptoms. The seizure was classified as unprovoked when an acute causative factor was not identified for the seizure (e.g., head trauma, fever, hyponatremia, hypocalcemia, and toxin exposure, among others). A seizure was considered as remote symptomatic when there was no immediate cause, but the child had a prior history of neurological injury, such as chronic non-progressive encephalopathy or stroke, leading to a static lesion. It was not possible to retrospectively distinguish between an idiopathic and a cryptogenic seizure in all children.
Regarding the type of seizure, they were classified as focal (which were differentiated into focal without consciousness alterations, focal with consciousness alterations, and focal with secondary generalization) or generalized seizures (differentiated into absence seizures, myoclonic, clonic, tonic, tonic–clonic, and atonic seizures). A seizure was considered to be undetermined when, considering the medical records, it was not possible to establish the classification between focal and generalized seizure. Recurrence was defined as an unprovoked seizure occurring over 24h after the first event.
The study was approved by the ethics committee of the institution where it was conducted (Centro Hospitalar do Médio Ave). As this was a retrospective study, it was not necessary to obtain a signed informed consent form from the patients’ legal guardians.
Analyzed clinical, demographic and analytical variablesGender, age at the first epileptic seizure, personal history (including information on prenatal and perinatal history, psychomotor development and history of febrile seizures), family history (mainly related to history of epilepsy, febrile seizures and cognitive delay), type of seizure, objective examination, complementary diagnostic tests, treatment, and follow-up were analyzed.
Statistical analysisThe chi-squared test for independence was used for comparisons between groups, based on categorical variables. Where it was not possible to use the chi-squared test, the exact test results were used. The t-test for independent samples was used to compare two groups based on continuous variables. Statistical analysis was performed using the SPSS (IBM SPSS Statistics for Windows, version 20.0, USA). A type I error probability (α) of 0.05 was considered in all inferential analyses.
ResultsPopulation sample descriptionDuring the study period, a total of 103 patients were admitted, aged 1 month to 18 years, diagnosed with a first episode of unprovoked epileptic seizure. Of the 103 assessed patients, 52.4% were males. The median age at the first seizure episode was 59 (1–211) months and the mean was 74 months; 35% were younger than 2 years and 25.2% older than 10 years. Of these children, 12 (11.7%) had a history of prematurity, five (4.9%) were resuscitated after birth, and 15 (14.6%) had delayed psychomotor development or cognitive impairment. Seven patients (6.8%) had a prior brain alteration and nine (8.7%) had a history of febrile seizures. A family history of epilepsy was positive in 44% of cases. Approximately 3.4% of the patients had a family history of febrile seizures and 7% had family members with cognitive delay.
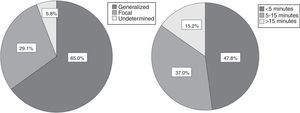
Characteristics of the first seizureThe seizure was classified as remote symptomatic in seven cases (one case of brain calcifications and chorioretinitis due to congenital infection by cytomegalovirus, two cases of polymalformation syndromes, two cases of hypoxic-ischemic encephalopathy, one case of stroke after cardiac surgery in the perinatal period, and one case of meningitis). Regarding symptomatology, the seizure was generalized in 65% of cases (mainly tonic-clonic), focal in 29.1% (mainly focal with consciousness alteration), and undetermined in 5.8% of the children and adolescents. Duration was less than 5min in 48% of patients and longer than 15min in 15% (Fig. 1). Approximately 25% of the children had their first seizure during sleep. In 5% of children, the initial presentation was status epilepticus and 30% had more than one seizure within the first 24h.
Study and treatmentApproximately 93% of children underwent an EEG at the first episode of epileptic seizure, which indicated epileptiform activity in 45% of cases. Of the altered EEGs, 72.1% had focal paroxysmal activity (with or without secondary generalization) and 27.9% had generalized paroxysmal activity. Approximately 47% of children underwent neuroimaging assessment (brain magnetic resonance imaging [MRI], computed tomography [CT] or transfontanellar ultrasound) at the first episode of epileptic seizure; alterations were observed in three cases (presence of ischemic foci). The treatment with antiepileptic drug was established in 46% of patients; in most cases, the drug used was sodium valproate (87% of those who received treatment).
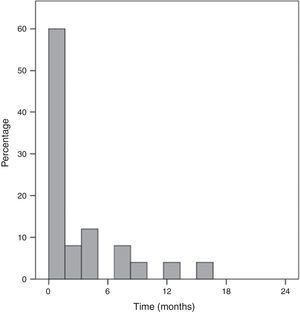
Recurrence rate and respective risk factorsOf the 103 assessed patients, 17 (three with remote symptomatic etiology) were lost to follow-up and thus, it was not possible to evaluate their recurrence rate. Of the remaining 86 cases, 26 were followed for over five years, 35 were followed between two and five years, and 25 had a follow-up period <2 years at the time of the study. The recurrence rate was 38% and, of these, 80% had the second seizure within six months after the first event. Only one child had the second seizure more than one year after the first event (Fig. 2).
Of the assessed recurrence risk factors, there was a statistically significant association between seizure occurring during sleep and the occurrence of new seizures (p=0.004), as well as between remote symptomatic etiology seizures and recurrence (p=0.020). The presence of electroencephalogram abnormalities was also associated with the occurrence of new seizures (p=0.021). No association was found between gender, age, pre- and perinatal complications, duration, and type of seizure (generalized vs. focal), personal history of febrile seizures, or family history of epilepsy and increased risk of recurrence (Table 1).
Analysis of recurrence risk factors.
| Risk factors | Recurrence n=33 | No recurrence n=53 | p |
|---|---|---|---|
| Female gender | 17 (51.5%) | 36 (67.9%) | NS |
| Age<2 years | 12 (36.3%) | 30 (56.6%) | NS |
| Prematurity | 2 (6%) | 7 (13%) | NS |
| Remote symptomatic etiology | 4 (12.1%) | 0 | 0.02 |
| Delayed psychomotor development | 6 (18.1%) | 7 (13.2%) | NS |
| Partial seizure | 10 (30%) | 9 (17%) | NS |
| Status epilepticus | 0 | 4 (7.5%) | NS |
| Duration of seizure>15min | 3 (9.1%) | 11 (20.8%) | NS |
| Seizures during sleep | 14 (42.4%) | 8 (15.1%) | 0.004 |
| Paroxysmal activity in the EEG | 18 (54.5%) | 19 (35.8%) | 0.021 |
| Personal history of febrile seizures | 3 (9.1%) | 6 (11.3%) | NS |
| Family history of epilepsy | 13 (39.4%) | 34 (67.9%) | NS |
NS, non-significant; EEG, electroencephalogram.
Seizures are one of the most common neurological disorders in children. The first episode of epileptic seizure is always an anxiety-causing event for parents and it is the health professional's duty to know the best approach and recommendations to use in each case.
Studies of recurrence after a first unprovoked seizure have shown percentages between 33% and 61% over a median follow-up of 2 years.2,3,7–9 In the present study, the recurrence rate was 38%, with a higher probability of recurrence within the first months after the first seizure and very low after the first year, which is consistent with the literature and with another study conducted in Portugal.5 Although follow-up duration was not the same for all children, most were followed-up for over 2 years, which appears to indicate that the time interval without seizures after the first epileptic seizure influences the risk of recurrence.
Shinnar et al.9 and Winckler et al.10 investigated the risk factors associated with unprovoked seizure recurrence in children. According to these authors, the mean age at first seizure was 6 years, which is in agreement with the results of the present study. The age at the first seizure was not associated with increased risk of recurrence in the present study, which is consistent with the results by Winckler et al.10
Regarding the influence of family history of epilepsy on the recurrence risk, some studies in the literature have found a positive association.3,10,11 That was not observed in the present study nor in that by Pereira et al.5
The studies developed in the 1980s on seizures occurring in children reported a predominance of generalized seizures,12,13 which is in accordance with the recent study by Winckler et al.10 and the present study. However, most articles and the recent literature describe a higher number of focal seizures.14,15 This discrepancy can be explained by differences in study samples or the fact that the present is a retrospective study, where the cases were assessed and recorded by several physicians, which cannot exclude a bias in the semiological classification (it is known that focal motor seizures are often classified as generalized seizures).
Regarding the influence of the seizure type on the recurrence risk, Winckler and Rotta2 found a six-fold higher risk of new seizures if the first one was focal. Similar results were reported by other authors.16 In contrast, similarly to the present study, other studies3,10 found no association. However, as previously explained, the possibility of a semiological classification bias cannot be discarded; therefore, these results have to be confirmed by prospective studies.
As previously reported, there was a predominance of short-duration seizures and of those that occurred when the child was wake. The recurrence risk in the present study was higher in seizures that occurred during sleep, as described in other studies.9,17 According to the literature, this association appears to be independent from the association of certain epileptic syndromes with seizures during sleep.18 Some authors suggest that seizures that occur during sleep cannot be identified early and, thus, the existence of other seizures prior to the one that was detected would explain the higher risk of recurrence in these children.4 Nonetheless, the explanation for this association is still controversial.
Over the years, several authors have mentioned the importance of an EEG with epileptiform activity for the risk of recurrence.5,10,19,20 The present study confirmed the increased risk of recurrence when the first EEG showed paroxysmal activity. As the EEG is a noninvasive and low-cost test, with an important role in the assessment of seizure recurrence, the authors suggest that it be requested after the first unprovoked seizure.
As expected, the group of children with remote symptomatic etiology (which included the three cases with abnormal brain MRI) showed a greater risk of recurrence.
It is known that antiepileptic treatment after the first seizure reduces recurrence in the first two years.21 However, the long-term evolution of children treated after the second episode is similar to that of children treated after the first seizure,1,21 and treatment with antiepileptic (AE) drugs does not reduce the risk of epilepsy. Therefore, and taking into account that the treatment with AE drugs is not harmless, the latter is generally recommended only after a second event or, in special cases, after the first seizure. In the present study, in accordance with the recommendations in the literature,22 antiepileptic therapy was implemented after the first seizure, after discussion with parents, only in children with neurological deficits, when the EEG showed unequivocal epileptic activity or when neuroimaging disclosed the presence of a structural abnormality.
This study has some limitations. One is related to the loss of follow-up of some children after the first seizure. Furthermore, as this was a retrospective study, in some cases it was not possible to verify some demographic and clinical data that could have influenced the prediction of recurrence risk. As previously mentioned, semiological classification bias cannot be ruled out. Finally, the fact that antiepileptic treatment was instituted in a significant proportion of children does not allow for inferring what would have occurred if these children had not been treated. However, it allows for the assessment of the natural history and risk factors for recurrence after a first epileptic seizure in the pediatric population, including specific cases with treatment indication after the first seizure.
In conclusion, most children with a first unprovoked epileptic seizure did not present recurrence; therefore, it is important to reassure the child/adolescent and their parents and try to minimize, as much as possible, the anxiety that these events generate in the family. The risk of recurrence was significantly higher in patients with a seizure occurring during sleep or remote symptomatic etiology seizure and in individuals with an abnormal EEG.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Maia C, Moreira AR, Lopes T, Martins C. Risk of recurrence after a first unprovoked seizure in children. J Pediatr (Rio J). 2017;93:281–6.