To assess the quality of neonatal transport performed by the Mobile Emergency Medical Services (Serviço de Atendimento Móvel de Urgência [SAMU]).
MethodsThis was a cross-sectional before-and-after observational study. The study was carried out from March to August of 2013 using a validated instrument, the Transport Risk Index of Physiologic Stability (TRIPS), to assess the characteristics of the newborn, medical and mechanical complications (equipment and ambulance), and stability of newborns before and after transport. Tests were conducted with 95% confidence level. Numerical variables are represented by measures of central tendency and dispersion. Categorical variables were compared by Fisher's exact test. In the comparison of variables between the groups, the Student's t-test was used for variables with normal distribution, Fisher exact test, when appropriate, and the Mann-Whitney test, for non-normal distribution.
Results33 newborns were transported from low-risk units to neonatal intensive care units. Male gender (57.6%) and full-term gestational age (63.6%) were more prevalent. Birth weight<2,500g was found in 39.4% of newborns. Respiratory failure accounted for 42.4% of the requests. The mean transport time was 58minutes without medical or mechanical complications. The TRIPS score worsened in 15% of neonates; in this group of infants, the mean initial temperature of 36.46±0.19 decreased significantly to 36.08±0.22 (p=0.041).
ConclusionThe transport performed by the SAMU was adequate for most newborns. The oscillation in body temperature was the only significant variable for the alteration in the TRIPS score.
Verificar a qualidade do transporte neonatal realizado por serviço de atendimento móvel de urgência (SAMU).
MétodosEstudo observacional transversal de antes e depois, de março a agosto de 2013. Utilizou-se instrumento validado de avaliação do transporte, o Transport Risk Index of Phisiologic Stabilit (TRIPS). Foram analisadas características dos recém-nascidos, intercorrências de aspecto médico e mecânico (das máquinas e ambulância) e a estabilidade, antes e depois do transporte. Os testes foram aplicados com 95% de confiança. As variáveis numéricas estão representadas pelas medidas de tendência central e de dispersão. As variáveis categóricas foram avaliadas pelo Teste Exato de Fisher. Na comparação das variáveis entre os grupos utilizou-se o Teste T-Student para as distribuições normais, teste exato de Fisher, quando indicado, e de Mann-Whitney para as não-normais.
Resultados33 recém-nascidos foram transportados de unidades de baixo risco para unidade de terapia intensiva neonatal. Prevaleceram o gênero masculino (57,6%) e a idade gestacional a termo (63,6%). Peso de nascimento abaixo de 2500g foi encontrado em 39,4% dos recém-nascidos. Insuficiência respiratória foi responsável por 42,4% das solicitações. A duração média do transporte foi de 58 minutos, sem intercorrências médicas ou mecânicas. O escore Trips piorou em 15% dos pacientes e nesse grupo de RN, a média da temperatura inicial de 36,46 ±0,19 diminuiu de forma significativa para 36,08±0,22 (p=0,041).
ConclusãoO transporte realizado pelo SAMU foi adequado para a maioria dos recém-nascidos. A oscilação da temperatura corporal foi a única variável importante para alteração do escore no transporte.
Since the late 1990s, studies have stated that an adequately performed neonatal transfer reduces morbidity and perinatal mortality.1,2
New technologies associated with the development of Medicine and longer life expectancy for newborn preterm infants have increased the demand for progressively specialized services. The regionalization of the latest technology is challenging, and inter-hospital transport is part of the treatment strategy of these patients.3
Studies on the subject are scarce. Only in 2011 the Brazilian Society of Pediatrics (Sociedade Brasileira de Pediatria [SBP]) created a manual and organized a training course for healthcare professionals in neonatal transport, in a partnership with the Brazilian Ministry of Health (MOH).4
The stability of vital signs in these children before the transport is a prerequisite for safe transfer. The aim of the transport is that the newborns reach their destination unit with equal or better status than that prior to the transport.1,5
There are many factors leading to clinical deterioration in newborns submitted to inter-hospital transport that do not depend on transport conditions. There is a consensus that the severity status before transport, gestational age, weight, and use of vasoactive drugs influence the stability during transport. A recent study showed that birth in the absence of a trained professional in the delivery room has a direct influence on the chance that the infant will survive with good quality of life.6
Conditions associated with transport can contribute to patient instability: vibration, excess noise, temperature difference, distance, duration of transport time, and highway conditions. However, the transport team should be prepared to learn to recognize and minimize them.7
In Brazil, the Mobile Emergency Medical Services (Serviço de Atendimento Móvel de Urgência [SAMU]) is responsible for pediatric and neonatal inter-hospital transport, whose conducts must follow the guidelines established by the MOH Edict 2048, which regulates their activities.8 The Stork Network established the Stork SAMU program, aimed at improving the quality and safety of transport for pregnant women and newborns.9
To assess the quality of transport, ensuring patient safety without worsening his/her health status, it is necessary to use a tool to predict its effects. For this purpose, the Transport Risk Index of Physiologic Stability (TRIPS) was validated. The MOH considers TRIPS to be a good assessment tool and recommends its use.10
There are other scores validated for the study of neonatal severity that were proposed to assess the impact of inter-hospital transport on the newborn's stability, but some difficulties have prevented their use. The use of the Score for Neonatal Acute Physiology, Version II (SNAP-II) or the Clinical Risk Index for Babies (CRIB) score requires observation and data collection for 12hours. The Neonatal Status Score and the Alberta Neonatal Transport Stabilization Score (ANTSS) have not been validated for this population, and the Hermansen's transport score only takes into account very-low birth weight newborns, in addition to requiring laboratory exams, which also makes it unpractical.11
The aim of this study was to assess the quality of newborn transport conducted by the Metropolitan SAMU of the city of Recife, state of Pernambuco, Brazil.
MethodsThis was a cross-sectional observational study, performed at two different times: immediately before and after neonatal inter-hospital transport conducted by the Metropolitan SAMU of the city of Recife, which provides full-time services, from March to August of 2013.
The TRIPS score was applied according to the guidelines of the SBP.4
The Metropolitan SAMU of Recife, at the time of research data collection, was responsible for 22 municipalities, with 32 basic ambulances and eight mobile intensive care units (ICUs).
Events that met the following inclusion criteria were selected for the study: a) neonatal inter-hospital transport request, b) mobile ICU type, sent at the discretion of the physician, with a destination hospital pre-defined by the hospital bed coordinator, and c) signed informed consent by a parent or guardian.
The study exclusion criteria included newborns that were hemodynamically unstable before transport and refractory to stabilization measures, or those transported as a result of pre-hospital care (rescue service).
Maintenance of body temperature using a transport double-wall incubator; maintenance of patent airways by endotracheal intubation, when necessary; two patent venous accesses; and hypoglycemia and metabolic acidosis correction, as well as hemodynamic stabilization measures were essential for the beginning of the transport.
Neonatal transport was performed by a team consisting of an interventional physician, nurse, nursing technician, and ambulance driver, as well as a neonatologist, as recommended by the SBP.4
The mobile ICU, when configured for neonatal transport, includes a double-wall heated incubator, neonatal mechanical ventilator, continuous infusion pumps, and monitors.
The study variables were: data related to the newborn (gender, gestational age, type of delivery, age at transportation, birth weight, weight during transportation, primary diagnosis, and reason for transfer), data related to the pre- and post-transport (hemodynamic stability of the newborn, ventilatory support, and TRIPS score), and data related to the analysis of medical and mechanical complications (of the equipment and ambulance) during transport.
Data collection was performed by one of the authors, using the electronic database of SAMU, the patient referral file, and the form completed by the team during transport. The SAMU transport team was trained to standardize the collection of the TRIPS score, which was incorporated into the service routine. The TRIPS score provides body temperature measurement (which was measured with a digital thermometer in the right axilla), systolic blood pressure measurement, breathing pattern, and neurological status before and after the transport, and was applied in all cases.
A database was created by the researchers and double data entry was performed, using the software program StataCorp 2011 (Stata Statistical Software: Release 12. College Station, TX: StataCorp LP) for the analysis.
Good-quality transport was considered when the TRIPS score at the second measurement was equal to or smaller than the score at the first measurement.
The result of the TRIPS score was grouped according to the before and after score variation, as “increased” and “maintained/decreased”, reflecting the transport quality. An increase in the TRIPS score reflects the transport-related clinical worsening of the newborn.
All tests were applied with 95% confidence. Numerical variables were represented by measures of central tendency and dispersion. Categorical variables were assessed for the presence of associations, using Fisher's exact test. When comparing the variables between groups, Student's t-test was used for normal distributions, in addition to Fisher's exact test, when indicated, and Mann-Whitney test for non-normal distributions.
The project was approved by the Research Ethics Committee (REC), opinion No. 200,364. The TRIPS score was applied noninvasively, without pain or harm to the patient. The study was conducted according to existing protocols with no change in conduct, regardless of the patient participation in the study. In cases of patient instability or safety threat, the transport was contraindicated, in accordance with the SAMU criteria.
ResultsNo equipment or ambulances problems of the Metropolitan SAMU of Recife were recorded. The devices were stable and functioning adequately in all transported cases.
A total of 42 ambulance transports of newborns were requested at the Recife Metropolitan SAMU. After exclusion criteria were applied, 33 newborns remained in the analysis, of whom 57% (19/33) were males and 78.8% (26/33) were born by vaginal delivery.
There were 14 services (maternities) of origin, including emergency units (EUs); there were five destination hospitals, all of which had high-complexity neonatal ICU. All but one of the destination hospitals (transport of one newborn) were in the Brazilian Unified Health System (Sistema Único de Saúde [SUS]).
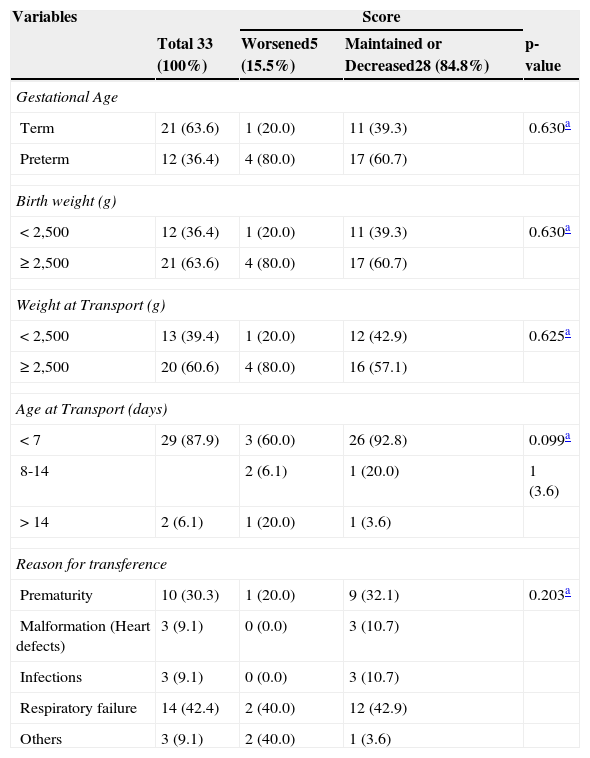
Table 1 shows that the TRIPS score was “maintained or decreased” in 84.80% (28/33) of cases. Most cases had gestational age between 37 and 42 weeks, age less than seven days old at the time of transport and weight during transport<2,500g (mean weight was 2,438±946.1g). When comparing these data between newborns whose score “increased” and those whose score was “maintained/decreased” after transport, variable distribution was similar between both groups.
Comparison of the study newborns regarding the population characteristics.
| Variables | Score | |||
|---|---|---|---|---|
| Total 33 (100%) | Worsened5 (15.5%) | Maintained or Decreased28 (84.8%) | p-value | |
| Gestational Age | ||||
| Term | 21 (63.6) | 1 (20.0) | 11 (39.3) | 0.630a |
| Preterm | 12 (36.4) | 4 (80.0) | 17 (60.7) | |
| Birth weight (g) | ||||
| < 2,500 | 12 (36.4) | 1 (20.0) | 11 (39.3) | 0.630a |
| ≥ 2,500 | 21 (63.6) | 4 (80.0) | 17 (60.7) | |
| Weight at Transport (g) | ||||
| < 2,500 | 13 (39.4) | 1 (20.0) | 12 (42.9) | 0.625a |
| ≥ 2,500 | 20 (60.6) | 4 (80.0) | 16 (57.1) | |
| Age at Transport (days) | ||||
| < 7 | 29 (87.9) | 3 (60.0) | 26 (92.8) | 0.099a |
| 8-14 | 2 (6.1) | 1 (20.0) | 1 (3.6) | |
| > 14 | 2 (6.1) | 1 (20.0) | 1 (3.6) | |
| Reason for transference | ||||
| Prematurity | 10 (30.3) | 1 (20.0) | 9 (32.1) | 0.203a |
| Malformation (Heart defects) | 3 (9.1) | 0 (0.0) | 3 (10.7) | |
| Infections | 3 (9.1) | 0 (0.0) | 3 (10.7) | |
| Respiratory failure | 14 (42.4) | 2 (40.0) | 12 (42.9) | |
| Others | 3 (9.1) | 2 (40.0) | 1 (3.6) | |
Respiratory failure was the main reason for newborn transfer; prematurity was the second cause. The mean time of transport duration was 58±16.26minutes. Regarding the need for ventilatory support, the invasive type was the most often used, and it was higher than the number of children who did not require support.
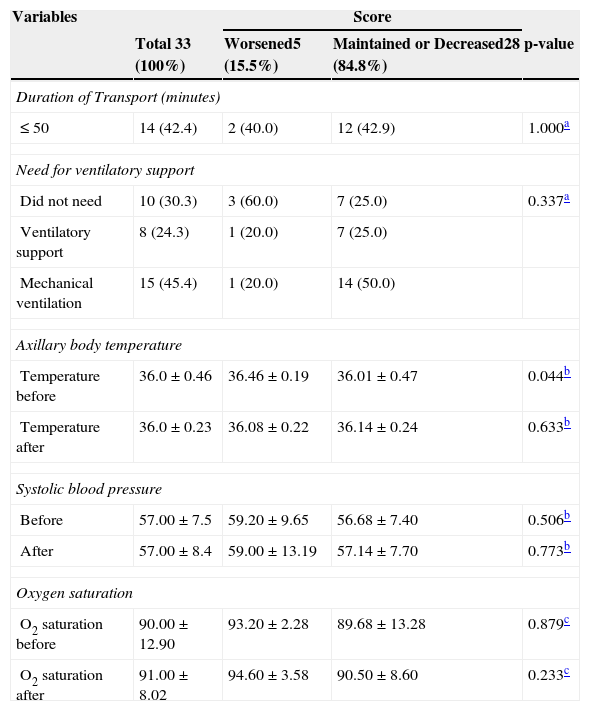
Vital signs (body temperature, oxygen saturation, and systolic blood pressure) are described in Table 2. These data were also compared between the groups of newborns whose score “increased” or “maintained/decreased”. It was observed that, in the group of newborns whose score “increased” after transport, the mean initial temperature of 36.46±0.19 decreased significantly to 36.08±0.22 (p=0.041), suggesting this variable is the most affected by inter-hospital transport. This temperature alteration was observed in all five infants who showed worsening of the score.
Comparison of the study newborns according to the physiological status result during transport.
| Variables | Score | |||
|---|---|---|---|---|
| Total 33 (100%) | Worsened5 (15.5%) | Maintained or Decreased28 (84.8%) | p-value | |
| Duration of Transport (minutes) | ||||
| ≤ 50 | 14 (42.4) | 2 (40.0) | 12 (42.9) | 1.000a |
| Need for ventilatory support | ||||
| Did not need | 10 (30.3) | 3 (60.0) | 7 (25.0) | 0.337a |
| Ventilatory support | 8 (24.3) | 1 (20.0) | 7 (25.0) | |
| Mechanical ventilation | 15 (45.4) | 1 (20.0) | 14 (50.0) | |
| Axillary body temperature | ||||
| Temperature before | 36.0±0.46 | 36.46±0.19 | 36.01±0.47 | 0.044b |
| Temperature after | 36.0±0.23 | 36.08±0.22 | 36.14±0.24 | 0.633b |
| Systolic blood pressure | ||||
| Before | 57.00±7.5 | 59.20±9.65 | 56.68±7.40 | 0.506b |
| After | 57.00±8.4 | 59.00±13.19 | 57.14±7.70 | 0.773b |
| Oxygen saturation | ||||
| O2 saturation before | 90.00±12.90 | 93.20±2.28 | 89.68±13.28 | 0.879c |
| O2 saturation after | 91.00±8.02 | 94.60±3.58 | 90.50±8.60 | 0.233c |
Values expressed as mean±standard deviation or median, quartiles for continuous variables, and as absolute numbers (percentages) for categorical variables.
Among the newborns, 46.4% (13/28) of those whose score was “maintained/decreased” and 80% (4/5) of those whose score “worsened” had scores<10 before transport, indicating low pre-transport severity. After transport, the scores for the groups “maintained/decreased” and “worsened” were 50% (14/28) and 80% (4/5), respectively. However, when comparing the groups regarding severity according to the TRIPS score before (p=0.34) and after (p=0.35) transport, there was no statistically significant difference.
The other variables (oxygen saturation and systolic blood pressure) showed similar behavior before and after transport, both in newborns whose score “increased”, and in those whose score was “maintained/decreased”.
When comparing regarding the clinical deterioration variables, it was observed that only the initial temperature was significantly different; it was lower in the group of newborns whose score was “maintained/decreased” (p=0.044).
There were two deaths on the seven days immediately after transport among the study children: one newborn with increased TRIPS score due to congenital malformation, and another in the group whose score was “maintained/decreased”, during surgery for tetralogy of Fallot correction.
DiscussionOnly five of the transported infants showed evidence of clinical deterioration, suggesting that the adequate transport prevailed. In spite of the small number of study subjects, the present data diverged from some studies in the literature that showed transport as the cause of instabilities.2,12–14 In this study, change in temperature was the variable that was altered in the score.
Among the newborns’ previous conditions mentioned in the literature as likely to influence the quality of inter-hospital neonatal transport, the following are the most frequently mentioned: prematurity, low birth weight, age at the time of transport and hemodynamic instability.15–17 In the present study, the fact that most infants had birth weight>2,500g and gestational age>37 weeks in both groups may have contributed to a higher percentage of patients with stable vital signs during transport. This is in contrast to the study with a predominance of preterm newborns with low birth weight.18
Regarding the main reasons for inter-hospital transfer, the results were similar to those reported in the literature: respiratory failure as the main cause of transport request. In other words, situations requiring transfer to tertiary units are the respiratory distress syndromes (meconium aspiration, respiratory distress syndrome, pneumonia, and pneumothorax), preterm newborn requiring special care (gestational age<32 weeks and/or birth weight<1,500g), severe hypoxia, suspected heart disease, seizures, perinatal infections (sepsis), and surgical situations/congenital malformations.19
The transport occurred within distances of less than 50km, which was reflected in the transport time. It is of utmost importance to understand that patient stabilization is an essential requirement for adequate transport, regardless of transport time or distance.20 The transport team must confirm patient stability before starting the transport, so that its benefits outweigh the inherent risks.1
For the transport to be successful, with minimal risks, the patient must be well-monitored patient, undergoing assisted mechanical ventilation, if necessary, after receiving medications at the local hospital before transpor.4 The transport of critically-ill newborns is a process with a high degree of risk and complexity, as these patients tend to be unstable.5 The internal environment of the ambulance hinders invasive procedures: orotracheal intubation should be performed before the transport, whenever necessary.4
SBP has created a course to train healthcare professionals in neonatal transport, as part of the Neonatal Resuscitation Program, identifying the ten steps for successful transport; seven of them refer to the pre-transport. The sixth step recommends the calculation of the risk of patient mortality, using the TRIPS score. Although there are other scores to assess physiological stability, which take into account other parameters of vital signs, such as heart rate, mean arterial pressure, Apgar score at birth, use of vasoactive drugs, respiratory rate, blood glucose, white blood cell count before and after transport, among other factors,11,15,21 SBP uses the TRIPS score to support their recommendations. This was the basis for the score selection for the present study, used to assess the reality of the transport performed by SAMU.
The measurement of vital signs before and after transport, regardless of the score calculation, is a routine practice in transport services, which measures heart rate, oxygen saturation, axillary temperature, and systolic blood pressure. The latter two not only contribute to the calculation of the TRIPS score, but are also included in the transport medical file and informed at the destination hospital. Axillary temperature is one of the variables that change the most during transport, as shown in studies that used it as a transport assessment parameter.12,20,22
If the teams were trained specifically in neonatal transport, the results would probably be even better. The authors suggest an integration between SAMU, MOH, and SBP in order to systematically train healthcare staff in neonatal transport, reassessing neonatal transport service teams and exchanging previous experience on patient transport and care of the transported newborn.
Conflicts of interestThe authors declare no conflicts of interest.
To the Mobile Emergency Medical Services of the city of Recife, and to Dr. José Henrique Moura and Dr. Sônia Bechara, for their support and assistance on the project.
Please cite this article as: Romanzeira JC, Sarinho SW. Quality Assessment of Neonatal Transport performed by the Mobile Emergency Medical Services (SAMU). J Pediatr (Rio J). 2015;91:380–5.