To evaluate the association between oxidative and inflammatory stress markers with peri-intraventricular hemorrhage (PIVH) in very-low birth weight newborns.
MethodsThis was a prospective study conducted in a level III neonatal unit. Basal and stimulated reactive oxygen intermediates (ROIs), reduced glutathione (GSH), and interleukin-6 (IL-6) levels were measured in umbilical cord blood. Newborns underwent serial ultrasound at the bedside, at 6, 12, 24, and 72hours of life and at seven days for the diagnosis of PIVH, classified as grades I to IV. Two groups were assessed, those with and without PIVH; maternal and neonatal control variables were used for comparison. Univariate and multiple regression analyses were applied.
ResultsA total of 125 newborns were assessed. PIVH incidence rate was 12.0%. In the univariate analysis, basal ROI, the use of two or more doses of corticosteroids, birth weight<1,000g, ventilatory support use, and SNAPPE II value ≥ 22 were significantly associated with PIVH. However, in the multivariate analysis, only antenatal steroid use was independently associated with the disease (OR 0,194; 95% CI: 0,048 to 0,773; p=0,02).
ConclusionROI, GSH, and IL-6 levels were not associated with the occurrence of PIVH in very-low birth weight infants
avaliar a associação entre marcadores de estresse oxidativo e inflamatório com a hemorragia peri- e intraventricular (HPIV) em recém-nascidos (RN) de muito baixo peso ao nascer.
Métodosestudo prospectivo em unidade neonatal nível III. Foi feita dosagem em sangue de cordão umbilical de intermediários reativos de oxigênio (ROI) basal e estimulado, glutationa reduzida (GR) e interleucina-6 (IL-6). Recém-nascidos foram submetidos à ultrassonografia seriada, à beira do leito, com 6, 12, 24 e 72 horas de vida e 7 dias para o diagnóstico de HPIV, classificada em graus de I a IV. Foram avaliados dois grupos: com e sem HPIV e variáveis de controle maternas e neonatais foram usadas para comparação. Análise univariada e de regressão múltipla foram aplicados.
Resultadosforam avaliados 125 recém-nascidos. A taxa de incidência de HPIV foi de 12,0%. Na análise univariada o valor basal de ROI, o uso de duas ou mais doses de corticosteroide, peso ao nascer menor que 1.000g, o uso de assistência respiratória e valor de SNAPPE II maior ou igual a 22 foram significativamente associados à HPIV. Porém, na análise multivariada, apenas o uso antenatal de esteroides se mostrou independentemente associado à doença (OR 0,194 IC95% 0,048-0,773 p=0,02).
ConclusãoROI, GR e Il-6 não foram associados à ocorrência de HPIV em RN de muito baixo peso ao nascer
Peri-intraventricular hemorrhage (PIVH) remains a high-prevalence disease in preterm newborns, especially those with birth weight<1,500g and gestational age<34 weeks. The disease is associated with the development of posthemorrhagic hydrocephalus, neurodevelopmental disorders, need for specialized rehabilitation therapies, and high social costs.1,2
The most common site of PIVH is the germinal matrix, which is located in the periventricular subependymal region and is irrigated by fragile and immature vasculature. It is an important proliferation site of neuronal precursors before their migration to their final location in the cerebral cortex. Several factors, especially those related to cerebral hypoperfusion and reperfusion phenomena, can result in bleeding at this site.2,3
In addition to the mechanism of vascular rupture associated with cerebral blood flow impairment, PIVH can occur due to other mechanisms, which may be of vascular origin or not.2
Experimental studies and those with humans have showed an association between PIVH and oxidative stress. In experimental studies in preterm newborn dogs, Ment et al. demonstrated that blocking the production of free radicals with etamsylate and indomethacin, or the use of superoxide-dismutase, had a protective effect on PIVH occurrence after reperfusion injury due to hypovolemic hypotension.3–5
More recently, there has been evidence of an association between PIVH with intrauterine inflammatory-infectious processes,6–8 as well as an association between serum interleukin-6 (IL-6) levels and vascular endothelium matrix lesions by cytokines.9–11
However, the specific evaluation of oxidative stress markers such as reactive oxygen species and glutathione antioxidant enzyme has not been assessed regarding the development of PIVH.
This study aimed to evaluate the association of oxidative stress markers, specifically the production of reactive oxygen intermediates (ROIs) and reduced glutathione (GSH) levels, with inflammation markers, namely serum IL-6 levels measured in umbilical cord blood, as risk factors for the development of PIVH.
MethodsThis was a prospective cohort study that included all preterm newborns (< 37 weeks of gestation) with a birth weight<1,500g who were hospitalized at a level 3 university neonatal unit, from May 10, 2009 to October 31, 2010. Exclusion criteria were: failure to collect umbilical cord blood; maternal or guardian refusal to allow the newborn to participate in the study; severe malformation of the central nervous system; and neonatal death within six hours of life, preventing the performance of the first cerebral ultrasound.
Sample size was calculated according to the umbilical cord serum levels of IL-6 as a marker of PIVH onset in very-low birth weight newborns, based on the study by Heep et al.,9 in which IL-6 was categorized into values>100pg/mL or ≤ 100pg/mL, with PIVH rates of 63% and 38% in these groups, respectively. Considering a 5% significance level, a test power of 80%, and a local PIVH incidence rate of 20%, the calculated minimum sample size was n=125.9
The assessed outcome was the presence of peri-intraventricular hemorrhage (PIVH), dividing patients into two groups: with and without PIVH, classified according to Papile et al. 12
For the diagnosis of PIVH, newborns underwent cerebral ultrasound at the bedside, after six, 12, 24, and 72hours of life and at seven days of age, using the anterior fontanel as acoustic window and a Xario® (Toshiba®, CA, United States) echograph with a 5-mHz transducer. The exams were recorded and stored on CD-ROMs and reviewed by two experienced evaluators. In case of doubt, a third expert was called to give his/her opinion.
Umbilical cord blood was collected at birth for the measurement of biochemical markers, after the infant's birth with the placenta still attached, through puncture of the umbilical vessels, thus yielding a mixed sample, both arterial and venous. Then, the material was distributed into three vials, two with an anticoagulant and one containing silicon oxalate and the samples were processed immediately.
The measurement of ROI production from polymorphonuclear leukocytes was determined using flow cytometry in two different moments: spontaneous (or basal) production, with leukocytes incubated only in Hanks solution; and the stimulated sample, with leukocytes incubated in Phorbol-myristate acetate.13 Values were expressed in nMol ×106 cells.
The measurement of erythrocyte GSH levels was performed by spectrophotometry: the assays performed in duplicate and results were expressed in mg% in relation to hematocrit.14
IL-6 was measured in samples frozen at -80°C by enzyme linked immunosorbent assay (ELISA), according to the manufacturer's instructions (R&D Systems®, MN, United States).15
For comparison between groups, the following maternal and neonatal control variables that could interfere with the PIVH outcome were further analyzed: primiparity, hypertensive disease, use of antenatal corticosteroids and number of doses ≥ 2, vaginal delivery, cephalic presentation, chorioamnionitis, twin pregnancy, birth weight<1,000g, gestational age<30 weeks, male gender, Apgar score<7 at the first and fifth minutes, need for resuscitation, small for gestational age, ventilatory support, use of surfactant, and Score for Neonatal Acute Physiology and Perinatal Extension (SNAPPE) II value.
Maternal hypertensive disease was defined as the presence of systolic blood pressure (SBP) ≥ 140mmHg or higher and diastolic blood pressure (DBP) ≥ 90mmHg, in two measurements, with an interval of at least four hours between them, or the presence of SBP ≥ 160mmHg and DBP ≥ 110mmHg in a single measurement.16 Chorioamnionitis was defined as the presence of maternal fever (maternal temperature ≥ 37.8° C) combined with two or more of the following signs: pain on uterine palpation, fetid/purulent amniotic fluid, fetal tachycardia (> 160 bpm), maternal tachycardia (> 100 bpm) and leukocytosis (total leukocyte count>15,000/mL).17 Small for gestational age was defined as the newborn with birth weight<10th percentile, according to the fetal growth curve of Alexander et al.18
For SNAPPE II, ROI, GSH, and IL-6 values, the cutoff for categorization was obtained through the maximization of the area under the curve (AUC).
Clinical variables were only considered present or absent at the time of detection of PIVH by serial ultrasound. In case of absence of PIVH development, variables were assessed until the seventh day of life.
For statistical analysis, birth weight, gestational age, maternal age, and ROI production values, as well as blood levels of GHS and IL-6, were expressed as medians and 25th and 75th percentiles, and were assessed by Mann-Whitney test. The chi-squared test or Fisher's test were used to compare categorical variables. Step-by-step multiple logistic regression analysis was applied to verify the independent variables with the occurrence of PIVH outcome, adapted for the calculation of incidence ratio using the variables that showed significance level ≥ 0.2 in the univariate analysis. The significance level was set at p<0.05.
The SPSS, release 15.0 for Windows (SPSS Inc. Statistics for Windows, Chicago, United States) was used in all statistical analyses. Parents signed an informed consent. The study was approved by the local Research Ethics Committee under No. 971/2008.
ResultsDuring the study period, 138 children with birth weight<1,500g were eligible for inclusion. Of these, 13 were not included in the present study, as umbilical cord blood collection was not possible in 12 children; two of these had PIVH (16.66%), one with grade I and another, grade III. One newborn was excluded because, although cord blood had been collected, he died within less than six hours of life, which prevented the ultrasound assessment.
A total of 125 children were included in the study. The number of mothers was 111, as there were 14 multiple pregnancies, 11 twin and three triplet pregnancies. There was no maternal refusal to participate.
Of the 125 children studied, 15 had PIVH (12.0%), six of them with grade I, two with grade II, four with grade III, and three with grade IV. The mild form of the disease (grades I and II) occurred on eight cases (53.33%), and the severe form (grades III and IV) in seven newborns (46.66%). The PIVH rate in the group that was not included was similar to that of the study group (16.6% vs. 12.0%; p=0.342).
In four cases (26.67%), PIVH was diagnosed within six hours of life, including the severe form of the disease, and nearly half (46.6%) was observed at up to 24hours of life.
There were 14 deaths among the study population and four of these newborns (28.57%) had the severe forms of the disease (three newborns were grade III and one was grade IV). All but three deaths occurred after 72hours of life. Of the three patients who died between six and 72hours of life, one of them already had a diagnosis of parenchymal hemorrhage at the cerebral ultrasound (grade IV of Papille et al.)12 and was classified as “presence of PIVH”. The other two cases died after 31 and 43hours of life, without hemorrhagic lesion at the ultrasound at 6/12/24hours of life, with no PIVH at necropsy, and were therefore classified as “absence of PIVH”.
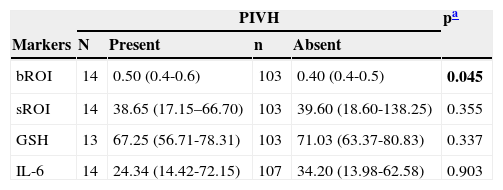
When assessing the markers, it was observed that the basal ROI production showed a statistically higher median in the group with PIVH (p=0.045). However, the stimulated production showed no statistical difference. The median glutathione and IL-6 values also showed no statistically significant difference between the groups (Table 1).
Basal and stimulated ROI values, glutathione, and IL-6 levels in umbilical cord blood of very low birth weight preterm newborn, according to the occurrence of PIVH.
| PIVH | pa | ||||
|---|---|---|---|---|---|
| Markers | N | Present | n | Absent | |
| bROI | 14 | 0.50 (0.4-0.6) | 103 | 0.40 (0.4-0.5) | 0.045 |
| sROI | 14 | 38.65 (17.15–66.70) | 103 | 39.60 (18.60-138.25) | 0.355 |
| GSH | 13 | 67.25 (56.71-78.31) | 103 | 71.03 (63.37-80.83) | 0.337 |
| IL-6 | 14 | 24.34 (14.42-72.15) | 107 | 34.20 (13.98-62.58) | 0.903 |
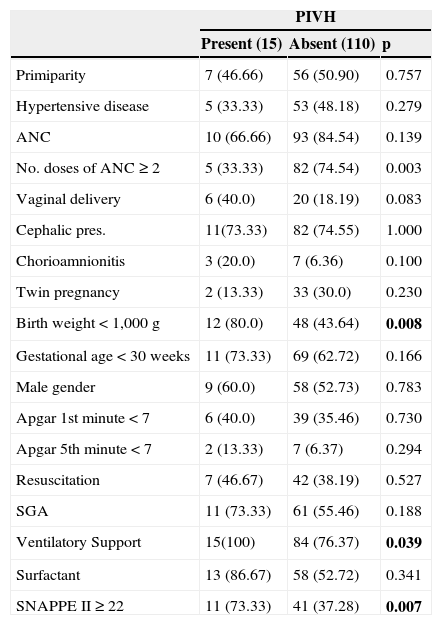
Regarding control clinical variables, the group with significantly PIVH had the lowest median birth weight (870 versus 1,042g; p=0.017), gestational age (27 versus 29 weeks; p=0.014) and higher values of SNAPPE II (26 versus 17; p=0.016).
Regarding the use of antenatal betamethasone, it was observed that 82.4% (103/125) of the newborns received the medication, and 87 of them received the complete cycle, but no significant difference was observed in the incidence of PIVH (10/15 versus 93/110; p=0.1395). However, when the use of corticosteroids was assessed according to the number of doses used, it was observed that the use of two or more doses of betamethasone was more statistically frequent (p=0.003) in the group without PIVH (Table 2).
Distribution of PIVH occurrence according to the categorical control variables.
| PIVH | |||
|---|---|---|---|
| Present (15) | Absent (110) | p | |
| Primiparity | 7 (46.66) | 56 (50.90) | 0.757 |
| Hypertensive disease | 5 (33.33) | 53 (48.18) | 0.279 |
| ANC | 10 (66.66) | 93 (84.54) | 0.139 |
| No. doses of ANC ≥ 2 | 5 (33.33) | 82 (74.54) | 0.003 |
| Vaginal delivery | 6 (40.0) | 20 (18.19) | 0.083 |
| Cephalic pres. | 11(73.33) | 82 (74.55) | 1.000 |
| Chorioamnionitis | 3 (20.0) | 7 (6.36) | 0.100 |
| Twin pregnancy | 2 (13.33) | 33 (30.0) | 0.230 |
| Birth weight<1,000g | 12 (80.0) | 48 (43.64) | 0.008 |
| Gestational age<30 weeks | 11 (73.33) | 69 (62.72) | 0.166 |
| Male gender | 9 (60.0) | 58 (52.73) | 0.783 |
| Apgar 1st minute<7 | 6 (40.0) | 39 (35.46) | 0.730 |
| Apgar 5th minute<7 | 2 (13.33) | 7 (6.37) | 0.294 |
| Resuscitation | 7 (46.67) | 42 (38.19) | 0.527 |
| SGA | 11 (73.33) | 61 (55.46) | 0.188 |
| Ventilatory Support | 15(100) | 84 (76.37) | 0.039 |
| Surfactant | 13 (86.67) | 58 (52.72) | 0.341 |
| SNAPPE II ≥ 22 | 11 (73.33) | 41 (37.28) | 0.007 |
Categorical variables expressed as a percentage.
ANC, antenatal corticosteroid; SGA, small for gestational age; SNAPPE II, Score for Neonatal Acute Physiology and Perinatal Extension
Regarding the other control variables, in the univariate analysis, PIVH was significantly associated with birth weight<1,000g, use of two or more doses of antenatal corticosteroids, respiratory assistance, and SNAPPE-II values ≥ 22. The other variables were not significantly different between the two groups (Table 2).
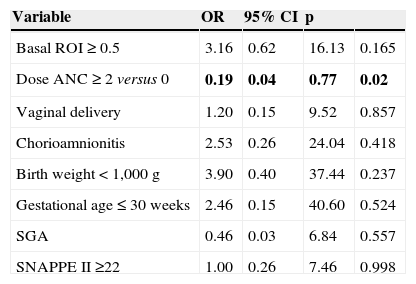
The following variables remained in the multivariate analysis: basal ROI (> 0.5 nMol×106 cells), two or more doses of corticosteroids, vaginal delivery, birth weight<1,000g, gestational age ≤ 30 weeks, nutritional status, and SNAPPE ≥ 22. At the final result of the multiple analysis, ROI production was not independently associated with the occurrence of the disease. It was observed that only the antenatal use of two or more doses of corticosteroids was independently associated with PIVH, as a protective factor (OR 0.194; 95%CI: 0.048 to 0.773; p=0.02; Table 3). Glutathione and IL-6 levels were not included in the final multivariate regression model, as they did not show statistical difference in the univariate model.
Multiple regression analysis to assess variables associated with PIVH in very-low birth weight newborns.
| Variable | OR | 95% CI | p | |
|---|---|---|---|---|
| Basal ROI ≥ 0.5 | 3.16 | 0.62 | 16.13 | 0.165 |
| Dose ANC ≥ 2 versus 0 | 0.19 | 0.04 | 0.77 | 0.02 |
| Vaginal delivery | 1.20 | 0.15 | 9.52 | 0.857 |
| Chorioamnionitis | 2.53 | 0.26 | 24.04 | 0.418 |
| Birth weight<1,000g | 3.90 | 0.40 | 37.44 | 0.237 |
| Gestational age ≤ 30 weeks | 2.46 | 0.15 | 40.60 | 0.524 |
| SGA | 0.46 | 0.03 | 6.84 | 0.557 |
| SNAPPE II ≥22 | 1.00 | 0.26 | 7.46 | 0.998 |
OR, odds ratio; 95% CI, 95% confidence interval, ROI, reactive oxygen intermediates; ANC, antenatal corticosteroid; SGA, small for gestational age; SNAPPE II, Score for Neonatal Acute Physiology and Perinatal Extension.
The study comprised a population of newborns at risk for PIVH. Birth weight was used as the inclusion criterion, since although prematurity itself is the main risk factor for the disease, the definition of gestational age may not be exact due to the inaccuracy of measurement methods. National and international research networks have also used birth weight as an inclusion criterion, facilitating data comparison between the units.19–21
Cerebral ultrasound was performed within the first hours of life, as the early perinatal and neonatal risk factors are very important for the onset of PIVH; therefore, the analysis of blood markers for PIVH could be timely conducted. In the present study, the disease was detected within the first hours of life, as almost 50% of hemorrhage cases occurred up to 24hours of life, which is in agreement with other studies.22 In addition to the diagnostic aspect, performing an early serial ultrasound assessment allowed for a more appropriate selection of neonatal risk factors present at a certain moment, as well as for establishing their association with the disease diagnosis. Many of the studies that assessed the risk factors for PIVH considered the occurrence of the disease within seven days of life and, therefore, it was not possible to accurately identify the decisive factor in the disease genesis.23
Basal ROI production was significantly higher in newborns who later developed PIVH. This fact implies that leukocytes had a significant activation potential at birth and could participate in events related to oxidative damage.
Studies have shown that in normal full-term newborns, the production of superoxide anions by polymorphonuclear leukocytes from blood of the umbilical cord was significantly higher when the delivery was vaginal, when compared with blood samples from newborns whose mothers had undergone cesarean delivery, without labor. This suggests that leukocyte activation is part of the mechanisms of parturition and normal birth processes. However, in preterm labor, that leukocyte activation in the fetus could cause tissue cell damage, either due to intensity of the reaction or the functional immaturity.24,25
Perrone et al. evaluated the basal and stimulated production of superoxide anions in 168 preterm newborns with 24-32 weeks gestation. When assessing several neonatal oxidative diseases related to oxidative stress, the authors found no difference in superoxide anion production by cord blood leukocytes. However, the authors did not comment on the data regarding PIVH alone, due to the small number of cases.26
Stimulated ROI production was not different in both groups. This fact could be explained either because the production in the group with PIVH was already at its maximum, or, as this is an artificial in vitro stimulation, it may not reflect the complex conditions in vivo biological stimuli. In a study of polymorphonuclear leukocytes in full-term newborns, it was demonstrated that the generation of superoxide radicals increased significantly after stimulation with its N-formyl-methionyl-leucyl-phenylalanine, but there was no additional increase when IL-10 or dexamethasone was added to the culture medium.27
As for glutathione, there was no difference in the values observed in both groups. Studies have shown that, as the pregnancy reaches term, the antioxidant system blood levels, both enzymatic or not, increase gradually and act as a protective factor for the relative hyperoxia that follows birth. Therefore, the low reserve of a non-enzymatic antioxidant system at a preterm birth exposes the newborn to a greater risk of oxidative damage.28,29 However, the low sample power of the test for glutathione found in the present study (11.5%), prevents generalizations regarding the existence of a protective effect or not.
The IL-6 serum levels were not different in patients with and without PIVH. This result could be justified by the low incidence of clinical chorioamnionitis in the population (8%). Furthermore, the prior effective antimicrobial treatment of the mothers, which is routine practice in our service, could have reduced fetal levels of cytokines, as they have short half-lives.30–32
The high incidence of hypertension in the sample (46.4%), may also explain the lack of association between inflammation markers and PIVH. Experimentally, Kauma et al. demonstrated that hypertensive women's placentas produced lower amounts of IL-6 when compared with normotensive pregnant women.33 Antenatal corticosteroid use could also alter placental IL-6 production, as shown in placental cell cultures34 and in a study with humans.32
Studies that have shown an association of PIVH with increased levels of IL-6 have some aspects that justify such difference, such as more premature newborns and, therefore, more susceptible to PIVH, selected population (pregnant women with clinical suspicion of chorioamnionitis), higher incidence of histological chorioamnionitis in the sample and IL-6 measurement in the newborn's blood and not umbilical cord blood.9–11 In the study by Bhandari et al., IL-6 levels in cord blood were significantly higher in the group that developed PIVH, but in the regression analysis using clinical variables with correction for gestational age, IL-6 levels were not independently associated with PIVH.35
The clinical variables may have interfered with the biochemical results as previously mentioned. Of the variables studied, only the antenatal use of two or more doses of corticosteroids was associated (as a protective factor), with the development of PIVH, which is consistent with the literature. A systematic review showed that antenatal steroid use promoted a significant reduction in the incidence of PIVH, considering all forms of the disease (RR 0.54; 95% CI: 0.43 to 0.69) and in the prevention of severe forms (RR 0.28; 95% CI: 0.16 to 0.50). However, protection was not observed when the birth occurred before 24hours of the administration of the first dose (RR 0.54; 95%CI: 0.21 to 1.36), but was observed when birth occurred before 48hours after the administration of the first dose (RR 0.26; 95%CI: 0.09 to 0.75).36
Steroid use alone is capable of altering the response of the assessed biomarkers, with decreased production of ROI and IL-6,27,32,34,37 and may therefore prevent such markers from expressing themselves and being factors independently associated with PIVH. However, studies with controlled exposure to antenatal steroid use, in case of premature birth danger, would not be ethical.
ConclusionIn conclusion, the basal production of ROI from umbilical cord blood was statistically higher in newborns that developed PIVH; however, in the multivariate analysis, the baseline ROI levels were not statistically an independent risk factor for HPIV. IL-6 or glutathione levels were also not associated with the PIVH.
FundingFundo de Amparo à Pesquisa do Estado de São Paulo (FAPESP) projeto 08/57405-4.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Caldas JP, Braghini CA, Mazzola TN, Vilela MM, Marba ST. Peri-intraventricular hemorrhage and oxidative and inflammatory stress markers in very-low birth weight newborns. J Pediatr (Rio J). 2015;91:373–9.
Study conducted at the School of Medical Sciences, Universidade Estadual de Campinas, Centro de Investigação em Pediatria (CIPED), Universidade Estadual de Campinas, and Hospital da Mulher Prof. Dr. José Aristodemo Pinotti, Centro de Atenção Integral à Saúde da Mulher (CAISM), Universidade Estadual de Campinas (UNICAMP), Campinas, SP, Brazil