The aim of this study was to assess clinical features and colonic transit patterns in Brazilian children with refractory constipation.
MethodsFrom 2010 to 2013, 79 constipated patients received follow-up care in a tertiary hospital. Of these patients, 28 (aged 8–14 years) were refractory to conventional therapy and underwent a simplified visual method of nuclear colonic transit study, by ingestion of a liquid meal containing 9.25MBq/kg of 99mTc-phytate. Abdominal static images were taken immediately and at two, six, 24, 30, and 48h after ingestion for qualitative analysis of the radio marker progression through the colon.
ResultsTwo patterns of colonic transit were found: slow colonic transit (SCT, n=14), when images at 48h showed a larger part of the tracer remained in proximal and transverse colon, and distal retention (DR, n=14), when after 30h, the radio isotope passed the transverse colon and was retained in the rectosigmoid up to 48h. The SCT and DR group included, respectively, nine and ten males; median ages in the nuclear study of 11 and 10 years, p=0.207; median duration of constipation of seven and six years, p=0.599. Constipation appearing during first year age (p=0.04) and report of soft stools (p=0.02) were more common in SCT patients. Palpable abdominal fecal impaction was found only in DR group. Appendicostomy for antegrade continence enema was successful in 4/12 (30%) of SCT patients (median follow-up: 2.4 years).
ConclusionNuclear transit study distinguished two colonic dysmotility patterns and was useful for guiding refractory patients to specific therapies.
O objetivo deste estudo foi avaliar as características clínicas e os padrões de trânsito colônico em crianças brasileiras com constipação refratária.
MétodosDe 2010 a 2013, 79 pacientes constipados receberam acompanhamento em um hospital terciário. Desses pacientes, 28 (com idade entre 8–14 anos) foram identificados como e realizaram estudo neclear do trânsito colônico por método visual simplificado, com ingestão de uma refeição líquida contendo 9.25MBq/Kg de fitato −99mTc. Imagens estáticas abdominais foram tomadas imediatamente e em 2, 6, 24, 30 e 48horas após a ingestão para uma análise qualitativa da progressão do marcador radioativo pelo cólon.
ResultadosForam encontrados dois padrões de trânsito intestinal: trânsito intestinal lento (STC, N=14), quando as imagens de 48 horas mostraram que grande parte do marcador permaneceu no cólon proximal e transverso, e retenção distal (DR, N=14), quando, após 30 horas, o radioisótopo havia passado o cólon transverso e permaneceu retido no retossigmoide até 48horas. O grupo STC e o grupo DR incluíram, respectivamente, 9 e 10 meninos; idade média no momento do: 11 e 10 anos, p=0.207; duração média de constipação: 7 e 6 anos, p=0.599. Sintomas de constipação durante o primeiro ano de i (p=0.04) e relatos de fezes (p=0.02) foram mais comuns em pacientes com STC. Observou-se impactação fecal palpável no abdomen apenas no grupo DR. A apendicostomia para enema anterógrado foi bem-sucedida em 4/12 (30%) pacientes com STC (acompanhamento médio: 2.4 anos).
ConclusãoO estudo nuclear do trânsito colônico diferenciou dois padrões de dismotilidade e foi útil para orientar terapias específicas para pacientes refratários.
Constipation is a common complaint in children and improvement is seen in the majority of patients who adhere to treatment recommended by consensus guidelines, including osmotic laxatives and intake of a fiber-rich diet.1 However, in approximately one-third of children, symptoms are more intense and there is refractoriness to regular enemas and maximum doses of laxatives.2 The constipation may be severe enough to result in complete cessation of spontaneous bowel motions.3 To explain such a clinical course, the main hypothesis is colonic transit dysfunction. Studies of colonic motor function in pediatric patients with refractory constipation have recorded dysfunctional patterns of colonic transit.4 Recent studies suggest that severe chronic constipation in children may be due to slowed colonic transit; different patterns of delayed transit have been described4–6 and specific therapies have been successfully proposed.7
There is a lack of data on role of colonic transit studies in clinical practice, mainly concerning its reproducibility in different populations, standardization of technical procedures, and purpose for investigating refractory constipation. The aim of the current study was to group refractory constipated patients according colonic transit pattern, using a simplified method of nuclear transit study (NTS).
Case study and methodsFrom September 2010 to December 2013, 79 patients diagnosed with functional constipation according to Roma III criteria8 received tertiary outpatient follow-up care in a pediatric gastroenterology unit at the University of Campinas Medical School Hospital in São Paulo, Brazil. Of these, 28 patients (aged 8–14 years; ages at the time of NTS) were identified as refractory to conventional therapy, after a prospective follow-up of 2.8±1.7 years (mean±SD). This group participated in a colonic transit study, after written informed consent term was obtained from the parents/legal guardians and patients. The main demographic characteristics of 28 children with clinical refractoriness included male gender (n=19) and median duration of symptoms longer than five years (ranging from 2 to 12 years).
Refractory constipation was considered when patient had presented severe chronic constipation resistant to therapy for at least two years, maintained fecal retention, and require regular cleansing enemas, despite adherence to maximum laxative dosage (when osmotic effects are intolerable). Subjects in the study were prescribed to doses of magnesium hydroxide or lactulose equal to or higher than 2mL/kg/day, or macrogol 3350 with electrolytes 1.4g/kg/day; exhibited symptoms of excessive laxatives, such as colicky abdominal pain, flatulence, vomiting, and cramps; expressed signs of osmotic intolerance; and consumed 18g of fibers/day (one-half cup of FibraMais®, Nestlé, Brazil). Adherence to therapy and clinical features on constipation symptoms were systematically evaluated during last 6 months before colonic transit study, by weekly telephone contact and clinical consultation every 15 days. If the pediatric gastroenterologist was uncertain regarding the presence of retentive soiling, a plain abdominal radiography was taken to confirm or exclude fecal impaction and Barr score9 was defined. Adherence to treatment was an inclusion criterion.
After medical history and physical examination, anorectal manometry and barium enema were performed for excluding Hirschsprung disease and other organic causes of constipation. Anorectal manometry was performed with a continuous perfusion system, and a low-complacency pneumatic hydraulic system of continuous capillary perfusion (Arndorfer, Inc., WI, USA), interfaced with a computerized system using commercially available software (Gastrosoft, Polygram Lower GI, version 6.4 and, Windows, Synetics Medical Inc., TX, USA and Dynapack MPX 816, Dynamed, SP, Brazil) and an 8-channel axial manometry probe (Dynamed Pro-life technology, Prolife technology, São Paulo, SP, Brazil).
NTS was performed during a four-day admission period scheduled exclusively for this purpose. Laxatives were discontinued five days before hospital admission. Rectal disimpaction was performed by rectal infusion of 20mL/kg of 12% glycerin solution, at a maximum dose of 500mL. Anorectal manometry was performed after rectal disimpaction. Normal manometry values were considered those reported by Kumar et al.10 Then, patients remained 12h with no medication, maintaining a normal diet and activities. On the morning of the first day, a liquid meal containing 9.25 MBq/kg (a maximum of 370MBq) of 99mTc-phytate diluted in 20mL of milk was ingested. Static images of the anterior abdominal view were taken immediately after radioactive drug ingestion and after two, six, 24, 30 and 48h. Images acquired immediately and at two and 6h after drug ingestion were used to assess gastric emptying and small bowel transit. Images acquired between six and 48h allowed assessment of colonic transit.
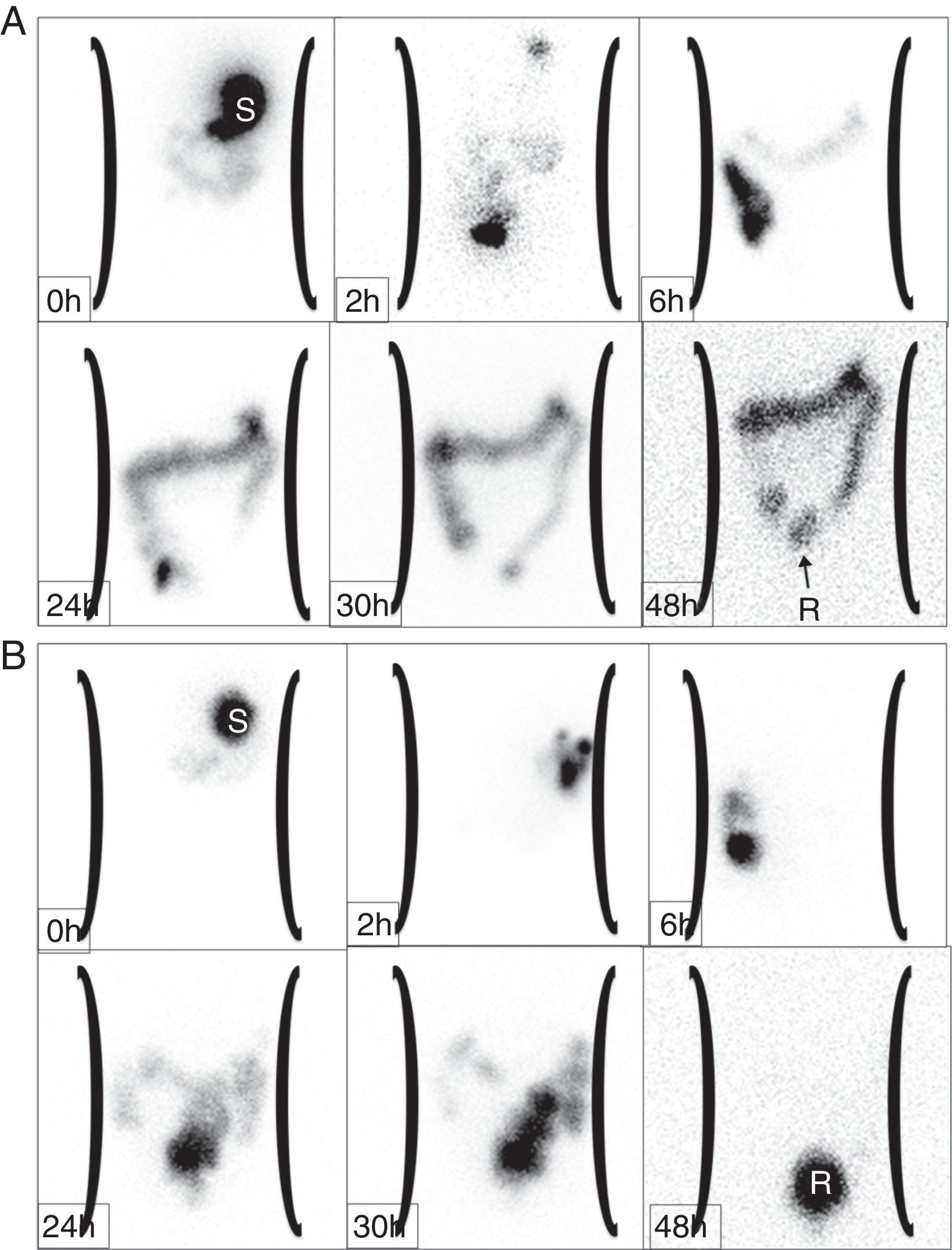
Colonic transit analysis was based on qualitative visual assessment of the images acquired at each time interval and considering progression of the radioisotope through the colon. Two nuclear medicine physicians reviewed the NTS images while blinded to clinical details. Images were grouped by visual analysis; classification was according to appearance of the activity pattern within the colon at six, 24, 30 and 48h. Two types of colonic motor patterns were found: the first was termed slow colonic transit (SCT) when the tracer in the main remained in the proximal and transverse colon, at 48-hour scans. The second pattern was classified as distal retention (DR) when the radioisotope had passed the transverse colon at 30h after the study, but persisted in the rectosigmoid region up to 48h.
Age, duration of constipation, follow-up time before NTS, and clinical features in the groups were compared by the Mann–Whitney test, and Pearson's chi-squared test was used to compare clinical features test. p-values <0.05 were considered significant.
This research project was presented to the Research Ethics Committee of the UNICAMP School of Medicine, on 4/16/2010 and approved by process 322/2010, CAAE number 02450146000-10, on 4/27/2010. A signed informed consent from patients and legal guardians was required to fulfill inclusion criteria in the study.
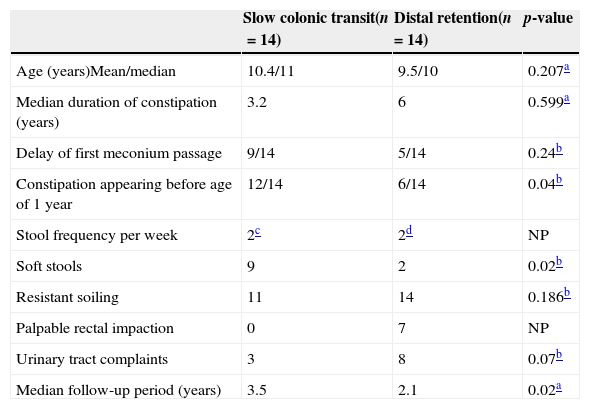
ResultsNTS showed two motor dysfunction patterns: isotope retention in the proximal colon (SCT group, n=14) or in the rectosigmoid region (DR group, n=14). Clinical data are shown at Table 1. The SCT and DR groups showed following characteristics, respectively: nine and ten males; median age at the time of NTS of 11 and 10 years, p=0.207, Mann–Whitney; median duration of constipation according data recorded in medical history, seven and six years, p=0.599, Mann–Whitney; and median duration of follow-up at the specialized service until the performance of NTS, 3.5 and 2.2 years, p=0.02, Mann–Whitney. Constipation symptoms appearing during first year age and report of soft stools were more common in SCT patients (p=0.04 and p=0.02, respectively). Abdominal palpable fecal impaction was found only in the DR group.
Comparison of the clinical features in 28 patients managed in a specialized outpatient facility with refractory constipation and presenting with two patterns of colonic transit scintigraphy: slow colonic transit (SCT) and distal retention (DR).
| Slow colonic transit(n=14) | Distal retention(n=14) | p-value | |
|---|---|---|---|
| Age (years)Mean/median | 10.4/11 | 9.5/10 | 0.207a |
| Median duration of constipation (years) | 3.2 | 6 | 0.599a |
| Delay of first meconium passage | 9/14 | 5/14 | 0.24b |
| Constipation appearing before age of 1 year | 12/14 | 6/14 | 0.04b |
| Stool frequency per week | 2c | 2d | NP |
| Soft stools | 9 | 2 | 0.02b |
| Resistant soiling | 11 | 14 | 0.186b |
| Palpable rectal impaction | 0 | 7 | NP |
| Urinary tract complaints | 3 | 8 | 0.07b |
| Median follow-up period (years) | 3.5 | 2.1 | 0.02a |
NP, not performed.
NTS was well tolerated and no adverse events were observed. Two specialists in nuclear medicine reviewed the images, separately. Inter-observer reliability with kappa coefficient was 0.727, p<0.001. Photographs of the two colonic transit patterns (SCT and DR) are shown in Fig. 1.
Scintigraphic images of bowel transit in a patient exhibiting motor pattern defined as slow colonic transit (A) and distal retention (B). (A) The progress of the radioisotope is observed for a period of 48h: stomach (S, 0h), small bowel (2h), cecum and ascending colon (6h). The image at 24h shows that almost all the radioactive material is distributed throughout the entire colon. The slow transit pattern is confirmed in the following images (30h and 48h), with minimum progress of the material to the rectum (R). (B) Nuclear colonic transit with retention pattern in the rectosigmoid region. After administration of the material, the stomach (S), small bowel, and ascending colon are sequentially imaged at zero, two, and 6h, respectively. Progress of the radioisotope throughout the colon is clearly seen in scans at 24 and 30h. At 48h, the material is retained in the rectum (R), with almost no radioactivity remaining in the colon.
Before NTS, all subjects underwent anorectal manometry. Rectoanal inhibitory reflex was identified in all patients; other parameters were unable to differentiate groups. Patients in both groups referred hyposensitivity during balloon insufflation with volumes from 20mL to 60mL in-rectum, and most children referred balloon insufflation as imperceptible. There are no differences between groups considering anal sphincter length, maximum resting pressure, and maximum squeeze pressure.
Barium enema of patients showed no stricture or malformation.
During the study, 64 plain abdominal radiographs were taken to investigate fecal impaction. Barr scores were calculated to assess severity of stool retention. Radiographs were retrospectively reviewed by two pediatric radiologists and correlated to NTS reports. The agreement between pairs of observers was assessed by the kappa coefficient and was good for the Barr score: 0.59. There was no association between stool retention severity and NTS images, p=0.08, test.
Twelve patients with SCT underwent to appendicostomy. Soiling was prevented in all cases and four patients recovered spontaneous bowel passage without using laxatives, after a median follow-up period of 2.4 years (min: 1.9 years; max: 2.6 years), the others continued to require stoma for antegrade cleansing enemas, median follow-up period: 1.5 years (min: 1.3 years; max: 4.9 years). During the same follow-up period, no DR patients recovered spontaneous bowel movements without lavage.
DiscussionTo allow for comparisons and reproducibility of clinical trials, research studies of new therapies or diagnostic tests in pediatric patients with constipation must be careful to specify the type of patient tested, since constipation is not a disease, but rather a symptom with different determinative factors. The pediatric population of constipated patients consists of a heterogeneous group, ranging in age, severity, and duration of symptoms. Until now, a consensus definition of refractory constipation has not been defined in international guidelines; this represents one of the most widely found clinical presentations of constipation in pediatric tertiary centers.
Considering that colonic transit dysfunction is present in 60% of children with refractory constipation4 and that specific therapies have been proposed for dysfunctional colonic patterns,11 it would be useful to distinguish them on a clinical basis. A retrospective study correlated constipation symptoms with transit times to determine clinical differences between SCT and DR, authors concluded that this was not possible on a symptomatic basis.12 However, despite the fact that the frequency of each symptom is not enough to define the transit pattern, some complaints are found more commonly in SCT patients: soft stools despite infrequent bowel movements; delayed passage of meconium; very early onset of constipation, generally during first year of life; and absence of a hard palpable stool mass on distal colon and rectum sigmoid.11–13 The clinical picture of the currently examined groups did not allow distinction of colonic patterns, despite the fact that reports of soft stools and early onset constipation were more frequent in SCT. Reports on stool frequency in the current groups were considered a weak symptom for differentiation purposes, since most of patients were prescribed cleansing enemas on a regular basis.
This study was also are unable to show association between fecal retention evaluated by Barr score and differentiated patterns in NTS. A recent study investigated a relation between Barr score and total colonic transit time with radiopaque markers in children; no relation was found.14
Colonic motility NTS performed in healthy individuals15 demonstrated that the proximal and distal portions of the colon have different motor functions. The radioisotope persists in the ascending colon for up to 12h. At 24h, radioactivity is equally distributed among the ascending colon, transverse colon, and distal portion of the bowel. At 48h, most of the tracer has already been evacuated. The transverse colon appears to function as a reservoir, while the left colon performs as a conduit. Camilleri & Zinsmeister concluded that evaluation of colonic segment transit time within 24h after the test has a high sensitivity for detection of colonic motor disorders, since the emptying rate of the proximal colon is significantly different between healthy and constipated individuals.16
Studies on colonic motor function in pediatric patients with refractory constipation have recorded normal or dysfunctional patterns of colonic transit. Yik et al.4 identified patients with normal colonic transit (no evidence of colonic dysmotility), anorectal retention, rapid proximal colonic transit (rapid transit through proximal colon at 6 and 24h), and slow proximal colonic transit. One study observed a predominance of slow transit patients.17 Another demonstrated a higher percentage of children with DR.18 This variability may be related to differences in criteria to send patients for test (initial reports only sent patients without fecal retention)19; technique for the performance of NTS, involving preparation of the patient, and type and mode of meal ingestion; and finally, differences in phases of image acquisition. The current study prescribed a cleansing enema for fecal impaction before the NTS; this decision was based on the understanding that a hard fecal mass could interfere with gastrointestinal transit studies, since children with hard fecal mass usually avoid stool passage due to pain or discomfort.20,21 Other researchers have not performed rectal disimpaction before the test. Studies on constipated adults did not confirm a relation between rectal evacuation and colonic transit time.22
To the best of the authors’ knowledge, NTS is not performed in Brazilian health centers, so these results cannot represent a general pattern in Brazilian children, and certainly the choice of children sent to scintigraphy may interfere with the patterns found in this study. The authors only considered such an evaluation on a research basis because only the most severe cases in follow-up were studied. A clinical consensus guideline is required.
The colonic transit patterns found herein were visually identified. Reproducibility of visual evaluation of patterns of colonic transit was previously demonstrated, as well as high rates of inter-observer agreement. Visual evaluation of nuclear images was compared to analysis of the geometric center.23 Visual inspection was considered adequate for general appreciation of transit pattern, while analysis of the geometric center indicates the site of greatest intensity of the radioisotope, but does not permit a clear view of transit, failures, and retropulsive movements that can be assessed by the visual technique.23 In clinical practice, visual assessment may be adequate for grouping patients. As users of such nuclear methodology, the authors tried to propose a more practical and low cost technique for daily use in most of centers with a nuclear medicine service. Camilleri & Zinsmeister16 described that slow colonic transit may be diagnosed 24h after radioisotope ingestion. In practice, images assessed between 24 and 48h were also considered the best index for diagnosis in clinical trials.24
Different therapies have been recommended to SCT and DR patients. While patients with DR are counseled to maintain the use of oral laxatives and supplemental intake of dietary fiber, therapeutic proposals for slow transit patients include mainly surgical treatment, more usually by appendicostomy for the performance of anterograde enemas and a new technique with transcutaneous electrical stimulation.3,7,25,26 The authors treated a small number of patients surgically and their evolution might be considered relatively better than those with DR on drug therapy, in terms of achieving spontaneous stool passage. In a study on resistant pediatric constipation, 80 patients underwent the Malone procedure and the authors found 12 children were able cease use of appendicostomy because of resolution of their symptoms; the probability of the child to stop colonic lavage was 20% 6.2 years after construction of the stoma; however, colonic transit patterns were not considered before surgical treatment in most patients.27 King et al., however, found that antegrade continence enemas were successful in 34 (81%) of 42 children with radiologically proven SCT.28
In conclusion, this study showed similar results to those conducted in other pediatric populations, a relevant fact for its eventual application in Brazilian children.29 These results corroborate the potentially relevant role of the NTS as a guide in clinical practice for management of constipated patients refractory to conventional therapy.
FundingThis study obtained financing support from the FAEPEX (Fundo de Apoio ao Ensino, à Pesquisa e Extensão) da UNICAMP, Solicitation number: 149/09.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Carmo RL, Oliveira RP, Ribeiro AE, Lima MC, Amorim BJ, Ribeiro AF, et al. Colonic transit in children and adolescents with chronic constipation. J Pediatr (Rio J). 2015;91:386–91.
Study conducted at Hospital de Clínicas, Faculdade de Ciências Médicas, Universidade Estadual de Campinas (UNICAMP), Campinas, SP, Brazil.