To verify the effect of psychological preparation on the relief of preoperative anxiety in children and to correlate parents’ and children's levels of anxiety.
MethodAfter the approval of the institutional Research Ethics Committee and written consent of the children's parents or guardians, 118 children of both genders were prospectively selected, aged between 2 and 8 years, physical condition classification ASA I, who were treated in the pre-anesthetic evaluation ambulatory of the University Hospital and who underwent ambulatory surgeries at the same hospital. Two controlled groups of 59 children were randomized: control group basic preparation and psychological preparation group. On the day of surgery, all selected children were evaluated regarding their level of anxiety using the modified Yale Preoperative Anxiety Scale and their parents were evaluated regarding their level of anxiety through the Visual Analog Scale. The evaluator was blinded to which study group the child and family member belonged to.
ResultsNine children and their family members were excluded per group when the results were analyzed. Children from the prepared group showed significant reductions in their level of anxiety in relation to the control group (p=0.04). There was no correlation between the level of anxiety of children and their parents’ levels (p=0.78).
ConclusionThe psychological preparation was effective in reducing the level of anxiety of children. However, there was no relation between the level of anxiety of children and their parents’ level.
Verificar o efeito da preparação psicológica no alívio da ansiedade pré-operatória de crianças e avaliar se há correlação com a ansiedade dos pais.
MétodoApós a aprovação do Comitê de Ética e Pesquisa da Faculdade de Medicina e obtenção do consentimento pelos responsáveis dos pacientes, foram selecionadas prospectivamente 118 crianças, de ambos os sexos, entre dois e oito anos, classificação de estado físico ASA I, atendidas no ambulatório de avaliação pré-anestésica do Hospital Universitário e submetidas a cirurgias ambulatoriais. Foram randomizados dois grupos controlados de 59 crianças: grupo de preparação básica e grupo preparação psicológica. No dia da cirurgia, todas as crianças foram avaliadas em relação ao seu grau de ansiedade através da Escala de Ansiedade Pré-operatória de Yale Modificada e seus pais, avaliados quanto ao seu nível de ansiedade pela Escala Visual Analógica. O avaliador era cego sobre qual grupo do estudo a criança e seu familiar pertenciam.
ResultadosNa análise dos resultados, foram excluídas nove crianças e familiares de cada grupo. As crianças do grupo preparado tiveram reduções significativas no grau de ansiedade em relação ao grupo controle, (p = 0,04). Não houve correlação entre os graus de ansiedade das crianças e seus pais (p = 0,78).
ConclusãoA preparação psicológica foi eficaz na redução do grau de ansiedade das crianças no momento da cirurgia. Não houve, entretanto, relação entre os graus de ansiedade dos pais e seus filhos.
Anxiety is present in approximately 50% of patients who undergo an anesthetic-surgical procedure.1 The prospect of postoperative pain, separation from family members, exposure to strangers, fear of the surgery and anesthesia, and the possibility of becoming incapacitated are factors that may increase the degree of anxiety in pediatric patients.2 In the preoperative period, anxiety tends to manifest as feelings of tension, nervousness, worry, apprehensiveness, or psychological stress.3 Some children verbalize their dreads, while others demonstrate anxiety through behavioral changes, such as becoming restless, trembling, breathing deeply, ceasing to speak, crying, or becoming, in some cases, difficult to control.4 In relation to anesthesia, high levels of anxiety can have negative effects, such as difficulty in achieving anesthetic induction, reduction in defenses against infections, and increase in intraoperative anesthetic consumption and postoperative analgesics.5
Diverse ways to alleviate preoperative anxiety have been widely studied, such as preanesthetic medications, distraction techniques, presence of parents during anesthesia induction, and preoperative psychological and educational interventions.6 The non-pharmacological management of anxiety has advantages when compared to anxiolytics, as they do not have adverse events; however, further studies are required to demonstrate the efficacy of distraction techniques such as the use of medical clowns, videogames, and cartoons, among others.7,8 Psychological preparation is seen as expensive due to the need for several sessions;9 however, it has good results in reducing preoperative anxiety, as well as in the psychological recovery of the children and their family members after the surgery.10,11
Thus, the authors propose a single-session model of psychological preparation for parents and children, with the main objective of verifying the effect of anxiety reduction in children at the time of the surgery. Moreover, the authors proposed to investigate whether there would be a correlation between parents’ and children's anxiety.
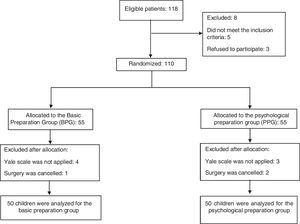
MethodsClinical study description and participantsAfter approval by the Research Ethics Committee of Faculdade de Medicina de Jundiaí (CAEE: 16288513.2.0000.5412) and after the informed consent form was signed by the patients’ parents or guardians, 118 children of both genders, aged between 2 and 8 years, with physical status classification according to the American Association of Anesthesiologists (ASA) I, treated at the pre-anesthetic outpatient clinic of the University Hospital of Faculdade de Medicina de Jundiaí, and who underwent outpatient surgeries at that hospital were selected. A randomized, parallel-controlled, prospective, and double-blinded trial was carried out to evaluate the effect of psychological preparation on the preoperative anxiety levels of children and their parents. The methodology was not changed after the study was started.
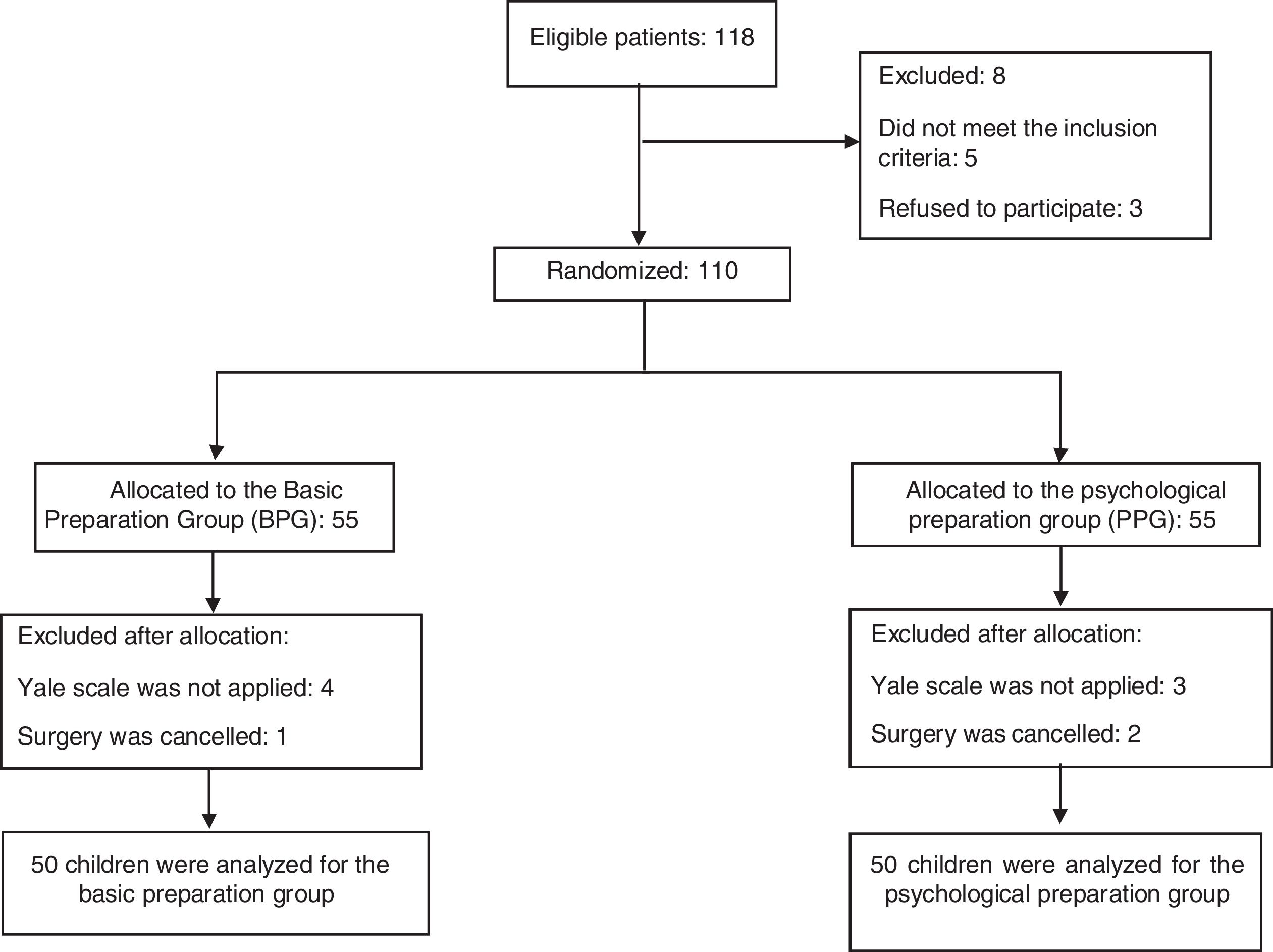
AllocationParticipants were randomly allocated using the List randomizer program (Randomness and Integrity Services Ltd, School of Computer Science and Statistics at Trinity College, Dublin, Ireland). This allocation was implemented by two anesthesiologists responsible for the pre-anesthetic consultation: they enrolled the participants, applied the exclusion criteria and directed the participants to intervention when necessary. The exclusion criteria were children with proven behavioral and cognitive alterations; history of previous surgeries and general anesthesia; users of psychoactive medications; and history of seizures, mental illness, or chronic pain. Five children were excluded for these reasons and three patients were excluded because their parents did not agree to their participation in the study (Fig. 1).
InterventionsFrom November 6, 2014 to October 5, 2015, two groups of children and their parents or guardians were randomly assigned, as described below:
Basic preparation group (BPG): a group that received the standard preparation at the pre-anesthetic consultation, where parents could have their questions answered and receive explanations from the anesthesiologist; as for the children, on the day of surgery, they waited for the moment of surgery in the toy library, a place with toys and books reserved for them and their family members.
Psychological preparation group (PPG): a group that, in addition to the basic preparation, underwent a psychological interview always performed by the same psychologist, after the pre-anesthetic consultation, with the presence of the family member and the child. Parents were briefed on the aspects of the surgery and the separation that would occur when the child entered the operating room, aiming to help them cope with these situations. A story was told to the child, with the support of a children's book entitled “Gaspar in the hospital” by Anne Gutman and Georg Hallensleben, published by Cosacnaif. Gaspar is a child character who suffers an accident and needs to undergo an emergency surgery.12 He was at school and is taken to the hospital by ambulance alone. He needs to be operated on and during anesthesia he sleeps and has a good dream. The book highlights Gaspar's courage and independence, how happy he is with his dream and when he wakes up, how happy he is to see his mother. The approach used with the child is that of coping with a new situation without the presence of the parents.
Psychological preparationFour main questions were addressed with the parents or family members present in the psychological session using a semi-open interview model, i.e., the questions were necessarily the same, but the interview varied according to the family responses and demands. The first question addressed the feelings about the surgery by the parent and the child; specifically asking for the verbalization of feelings such as fear, anxiety, concern and others as an initial approach. In the second question, adult aspects were questioned regarding the mother-child, or father-child separation, from simple separations such as leaving the child with a relative for a few hours, adaptation to school, and other separation experiences. The third question addressed how the mother or father perceived and dealt with the child's health and illness situations, and the last question addressed the child's attachment to objects. This session with the parents was used to guide and to calm them down regarding the anesthesia and surgery aspects, as well as to support the children's separation from their parents, so they would feel confident going into the operating room.
MeasuresAt the pre-anesthetic evaluation outpatient clinic, on the day of the consultation, the following tools were applied to the parents: a questionnaire to assess the sociodemographic profile, a questionnaire about the role of the anesthesiologist, the parents’ apprehensions and fears related to anesthesia and assessment of their degree of anxiety through the visual analogue scale (VAS). Such scale, used as a secondary outcome measure, was also applied to parents or guardians at the time of the surgery. The scale measured 100mm, where 0 (zero) was equivalent to “calm” and 100mm meant “very anxious.”13 Mild anxiety was expressed by the scores 0, 1, and 2; moderate anxiety, 3, 4, 5, 6, and 7; and intense anxiety, 8, 9, and 10.
On the day of the surgery, all children selected from both groups were referred to the toy library attached to the surgical center, where their anxiety levels were assessed through the modified Yale Preoperative Anxiety Scale (m-YPAS). This observational scale consists of 27 items divided into five categories: activity, vocalization, emotional expression, apparent awakening state, and family interaction. The score ranges from 23.5 to 100; when above 30, the higher the score, the greater the anxiety.14 The m-YPAS Scale was applied continuously, from the pre-anesthetic preparation room at the time of the child's separation from the parents to the moment of anesthetic induction, and was performed by a single and the same resident physician in anesthesiology, under the supervision of the anesthesiologist in charge for the division, after previous training. The evaluator was blinded to the child's group.
The basic protocol of anesthetic induction was performed in a closed-loop anesthesia delivery system with 33% O2 and 66% N2O, with a total flow of 5 L.min-1 for one minute, followed by administration of sevoflurane at 8%. After the child lost consciousness, the gas flow was reduced to 2Lmin−1 and the anesthetic concentration, to 2–3%.
Sample size determination and statistical analysisAfter the 110 children were allocated in both groups, five children from each group were lost to follow-up due to surgery cancellation or non-application of the anxiety scale on the day of the surgery. The final analysis was restricted to 50 children from each studied group.
Considering that the prevalence of anxiety in the operating room in children is 50%1 and that the proposed intervention was able to reduce children's anxiety by 20% after a pilot study with 20 children, and using an α-error of 5%, β-error of 20%, and 95% confidence interval (95% CI), the number of patients was determined at 42 in each group, totaling a number of 84 participants in the proposed study.
The statistical analysis was performed using the software Stata/SE version 9.0 for Windows (Stata Corporation – College Station, Texas, USA). In the analysis of groups, medians and the 25–75% percentiles were used as a measure of central tendency and variability due to the non-normal distribution trend of the sample separated in groups. Categorical variables were shown as absolute values and percentages. Histograms and the Shapiro–Wilk test were used to verify the symmetry of data distribution.
The chi-squared test and Fisher's exact test were used for categorical variables, and the chi-squared partition was performed if p-value was less than 0.05 (significance level used). The comparisons between two groups for continuous or ordinal variables were performed using the Mann-Whitney test.
Spearman's correlation was used to evaluate the association intensity of ordinal variables in the same individual.
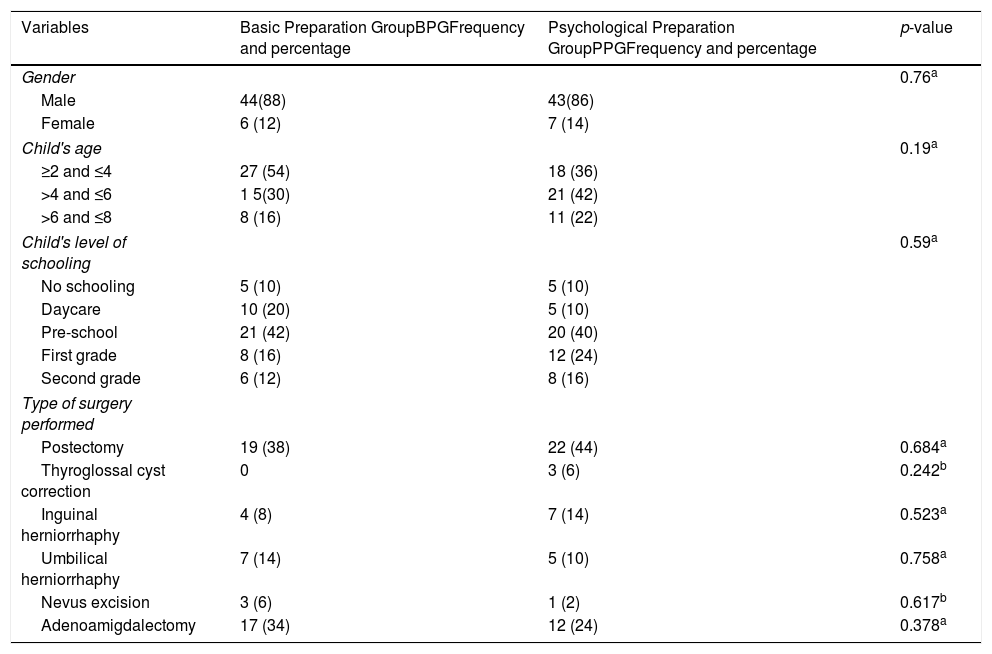
ResultsThe groups were homogeneous regarding gender, age, level of schooling, and type of surgery. In both groups, a prevalence of boys for both groups and children attending preschool was observed (Table 1).
Characteristics of the study children: comparison by group.
| Variables | Basic Preparation GroupBPGFrequency and percentage | Psychological Preparation GroupPPGFrequency and percentage | p-value |
|---|---|---|---|
| Gender | 0.76a | ||
| Male | 44(88) | 43(86) | |
| Female | 6 (12) | 7 (14) | |
| Child's age | 0.19a | ||
| ≥2 and ≤4 | 27 (54) | 18 (36) | |
| >4 and ≤6 | 1 5(30) | 21 (42) | |
| >6 and ≤8 | 8 (16) | 11 (22) | |
| Child's level of schooling | 0.59a | ||
| No schooling | 5 (10) | 5 (10) | |
| Daycare | 10 (20) | 5 (10) | |
| Pre-school | 21 (42) | 20 (40) | |
| First grade | 8 (16) | 12 (24) | |
| Second grade | 6 (12) | 8 (16) | |
| Type of surgery performed | |||
| Postectomy | 19 (38) | 22 (44) | 0.684a |
| Thyroglossal cyst correction | 0 | 3 (6) | 0.242b |
| Inguinal herniorrhaphy | 4 (8) | 7 (14) | 0.523a |
| Umbilical herniorrhaphy | 7 (14) | 5 (10) | 0.758a |
| Nevus excision | 3 (6) | 1 (2) | 0.617b |
| Adenoamigdalectomy | 17 (34) | 12 (24) | 0.378a |
No significant differences were found regarding the parents’ characteristics (chi-squared test) when the two groups were compared regarding gender (p=0.76), schooling (p=0.39), income (p=0.32), occupation (p=0.20), and marital status (p=0.36). Most interviewees were women (87%), who were generally the mothers, had finished high school (39%), belonged to the middle class (57%), and were employed (58%) and married (77%).
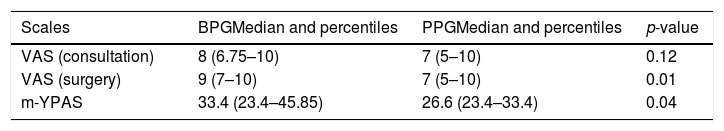
When comparing the groups, both parents and children from the PPG group had significantly lower anxiety levels at the time of surgery when compared with parents and children from the BPG. There was no difference between the parents’ level of anxiety assessed by the VAS at the time of the preanesthetic consultation (Table 2).
Parents’ and children's anxiety: comparison by group.
| Scales | BPGMedian and percentiles | PPGMedian and percentiles | p-value |
|---|---|---|---|
| VAS (consultation) | 8 (6.75–10) | 7 (5–10) | 0.12 |
| VAS (surgery) | 9 (7–10) | 7 (5–10) | 0.01 |
| m-YPAS | 33.4 (23.4–45.85) | 26.6 (23.4–33.4) | 0.04 |
Mann–Whitney test.
Values expressed as medians and percentiles (25–75%).
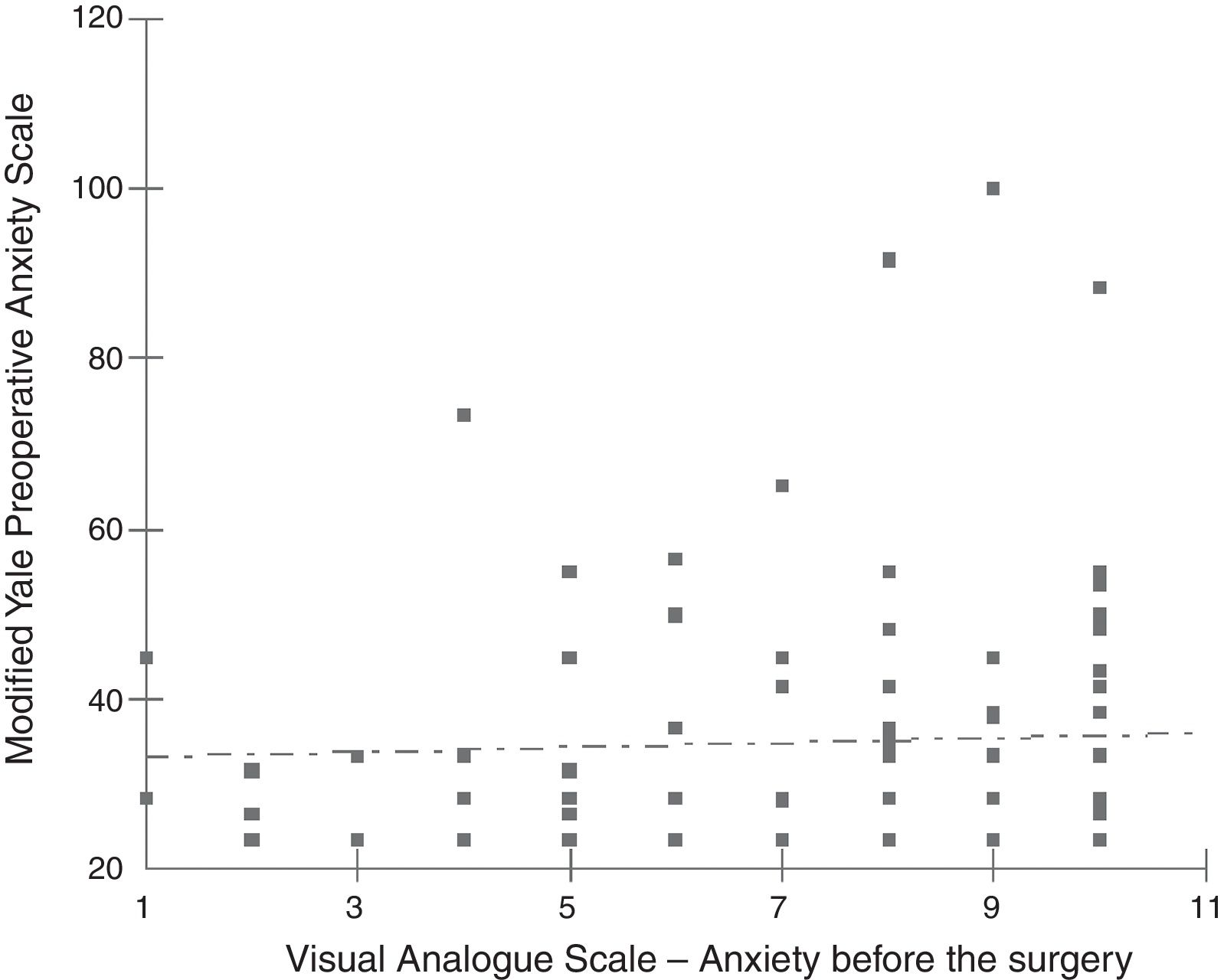
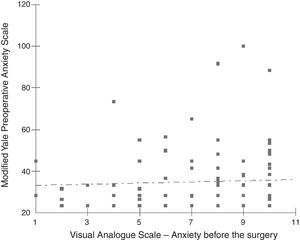
There was no correlation between parental anxiety at the time of surgery and the children's anxiety the two studied groups (r=0.0276, p=0.78; Fig. 2).
None of the children's demographic data, such as gender (p=0.20), age (p=0.88), and level of schooling (p=0.52; chi-squared test) presented a significant association with anxiety.
DiscussionThis clinical trial demonstrated that the children and their parents who received psychological preparation care in a single session had their preoperative degree of anxiety significantly reduced when compared with the group that did not receive this care (p=0.04 for the children and=0.01 for parents at the time of surgery).
The preparation was focused on alleviating separation anxiety in young children. According to the care protocol used at the University Hospital where this study was performed, the parents did not accompany their children during anesthetic induction, and the separation took place at the toy library attached to the surgical ward. The authors consider the age limit of 8 years as a predisposing factor to this anxiety,15 due to the peculiar fact that children between 6 months and 4 years of age manifest a greater intensity of seizures and the fear of separation from parents still remain in some children between the ages of 4–8 years.15
In his review article, Moro16 discusses the question of age related to preoperative anxiety and concludes that there is still no consensus on the subject. The literature contains some assertions that younger children, up to 6 years of age, are more likely to suffer from preoperative anxiety related to separation. Older children, however, would be more concerned with the surgery itself. Some studies have reported that older children are more anxious, and other authors did not find any evidence related to age.16 In the present study, no differences regarding an age-related degree of anxiety were observed; younger children between 2 and 4 years, or those aged 5 and 6 years, were no more anxious than those aged 7 and 8 years (p=0.08). Similarly to the present results, Wollin et al.17 found no significance in the association between anxiety and the children's age between 5 and 12 years – they divided the children into age groups: 5–6 years, 7–10 years, and 11–12 years. The present authors therefore believe that maintaining the focus on the separation anxiety approach for the age group of 2–8 years reduced the number of consultations to a single session.
Kain et al. performed a family-centered preparation.9 In this intervention, parents received counseling through videos, booklets, or by telephone, and the children received a surprise box at the time of anesthetic induction; their parents were monitored by a researcher who asked them to use planned distraction strategies for children, if necessary. This advanced preparation group presented superior results in reducing the children's anxiety in comparison with the other study groups that were not submitted to this preparation.
Although the trial concluded that the psychological preparation significantly contributed to the reduction of preoperative anxiety in children, the program was expensive and feasible only in large hospitals. Moreover, because of the complexity involved, it was not clear which component would be essential in this preparation.
Another study, comparing children who underwent a preoperative psychological preparation to a group of children who did not receive this type of care showed that the group of children trained by the psychologist had lower anxiety levels than those who underwent only distraction techniques.18 Another trial19 evaluated the psychologist's presence at the time of anesthetic induction and concluded this method was more effective in reducing anxiety in children when compared with distraction techniques. In that study, it was necessary to have the presence of a professional psychologist, who is part of the surgical team, only for this in-person support during anesthetic induction. In the present study, the preparation aimed to enable the child to face the moment of surgery alone, but with the support of the existing team.
Regarding the aspect of an association between the degree of anxiety of the parents and their children in the preoperative period, the present* study did not show such correlation. Another clinical trial20 also failed to observe such association, but its result was attributed to the restricted number of participants. Cui et al.21 demonstrated a correlation between the anxiety of parents and their children younger than 4 years during anesthetic induction. It could be suggested that this difference in results was due to the fact that the mean age of the children in the present study was higher. According to Nascimento,22 there may be differences in the correlations between parents’ and children's anxiety levels regarding their age group.
The present study had some limitations. In the postoperative period, the children's behaviors and need for pain medication were not assessed and, therefore, it was not possible to verify the extent of the benefits in this psychological preparation model. It was also not possible to match the genders in the studied groups, which predominantly consisted of boys, due to the high frequency of postectomies in the service. The psychological preparation for preanesthetic medication use was not compared, and ethical reasons prevented the creation of a control group without any preanesthetic preparation. Children who received psychological preparation were compared with children awaiting surgery in a toy library, since it has already been shown that toys help reduce anxiety.3,23,24
Finally, the study could have selected parents and children with a high risk of anxiety based on the information collected during the psychological consultation and compare them to the anxiety assessed by VAS and YALE scale at the time of surgery. This prognosis would have been useful in estimating which parents and children would need a more comprehensive approach with more than one session. The authors suggest this approach for future studies.
Children in the PPG and their parents benefited from the anxiety reduction when compared to the group that did not receive this preparation. Therefore, the authors conclude that a single psychological session was effective in preparing parents and children for separation anxiety and coping with the surgical procedure in most cases. This result has practical and clinical importance and thus, this approach was shown to be as effective as programs that rely on multiple sessions.
FundingThe study was registered in the Registro de Ensaios Clínicos Brasileiros. Primary Identifier: RBR-5jh9sf.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Meletti DP, Meletti JF, Camargo RP, Silva LM, Módolo NS. Psychological preparation reduces preoperative anxiety in children. Randomized and double-blind trial. J Pediatr (Rio J). 2019;95:545–51.
Study conducted at the Master's Degree Program of Faculdade de Medicina de Jundiaí, São Paulo, SP, Brazil