To assess the prevalence, mortality and risk factors associated with the birth of very low birth weight preterm infants over a period of 33 years.
MethodsFour cross-sectional studies were analyzed, using data from perinatal interviews of birth cohorts in the city of Pelotas collected in 1982, 1993, 2004, and 2015. Based on perinatal questionnaires, anthropometric measurements of newborns and death certificates were analyzed to obtain the prevalence rate, neonatal mortality, and risk factors (maternal age, income and type of delivery) for very low birth weight.
ResultsA total of 19,625 newborns were included in the study. In the years 1982, 1993, 2004, and 2015, there were, respectively, 5909, 5232, 4226, and 4258 births. The prevalence of very low birth weight was, respectively, 1.1% (n=64), 0.9% (n=46), 1.4% (n=61), and 1.3% (n=54). There was no statistical evidence of an increasing trend over time (p=0.11). Among the risk factors, family income in the three poorest quintiles was associated with prevalence rates that were approximately twice as high as in the richest quintile (p=0.003). Mortality per 1000 live births for neonates weighing <1500g decreased from 688 to 259 per thousand from 1982 to 2015 (p<0.001), but still represented 61% of neonatal deaths in the latter year.
ConclusionAlthough mortality in very low birth weight decreased by more than 60% in recent years, this group still contributes with more than half of neonatal deaths. Low family income remains an important risk factor in this scenario.
Verificar a prevalência, mortalidade e fatores de risco associados aos nascimentos de prematuros de muito baixo peso ao nascer (MBPN) ao longo de 33 anos.
MétodosSérie de quatro estudos transversais utilizando dados das entrevistas perinatais das coortes de nascimento da cidade de Pelotas coletados em 1982, 1993, 2004 e 2015. A partir de questionários perinatais, medidas antropométricas dos recém-nascidos e certidões de óbito, foram analisadas a prevalência, mortalidade neonatal e fatores de risco (idade materna, renda e tipo de parto) para prematuros de muito baixo peso ao nascer.
ResultadosForam incluídos no estudo 19.625 recém-nascidos. Em 1982, 1993, 2004 e 2015 ocorreram, respectivamente, 5.909, 5.232, 4.226 e 4.258 nascimentos. A prevalência de prematuros de muito baixo peso ao nascer naqueles anos foi, respectivamente, de 1,1% (n=64), 0,9% (n=46), 1,4% (n=61) e 1,3% (n=54). A tendência de aumento durante o período não alcançou significância estatística (p=0,11). Entre os fatores de risco, a renda familiar nos três quintis mais pobres esteve associada a prevalências cerca de duas vezes mais altas do que no quintil mais rico (p=0,003). A mortalidade por 1.000 nascidos vivos para os neonatos com peso < 1500g caiu de 688 para 259 por mil ao longo dos anos (p<0,001), mas ainda representa 61% dos óbitos neonatais em 2015.
ConclusãoEmbora a mortalidade nos prematuros de muito baixo peso ao nascer tenha diminuído em mais de 60% nos últimos anos, esse grupo ainda contribui com mais da metade dos óbitos neonatais. A baixa renda familiar continua a ser fator de risco importante nesse cenário.
In Brazil, since the end of the 1980s, neonatal mortality has been considered the main component of childhood mortality.1 Preterm birth, with a gestational age of less than 37 weeks, plays an important role in this context, being a potentially preventable cause.2–4 It is estimated that approximately 12% of the total births of the Brazilian population are preterm, a higher rate than that observe in developed countries.5,6
The causes for preterm birth include factors associated to the mother's age, such as pregnancy in adolescence or above 35 years of age; to the pregnancy, such as a short interval between conceptions, multiple gestations, elective cesarean sections, labor induction, chronic gestational diseases, and infections, as well as socioeconomic and nutritional conditions; and those associated to the fetus, such as genetic diseases.5,7
Neonates with very low birth weight (VLBW) are those whose birth weight is below 1500g. They constitute a group with high morbidity and mortality, scarcely studied in the literature, and can account for 60% of neonatal deaths.8 There is a high correlation between extreme prematurity and VLBW. Based on the Intergrowth-21st study, the 50th percentile of birth weight for a 32-week-old fetus is equal to 1500g,9 so that, in the absence of accurate gestational age data, temporal trends of VLBW may indicate evolution in extreme prematurity.
In the city of Pelotas, state of Rio Grande do Sul, Brazil, a cohort is started every 11 years, which includes all births that occurred in the city during the year.10 These cohorts have allowed researchers to assess the evolution of health indicators in the city starting in 1982, 1993, 2004 and, finally, 2015. Based on the data from these studies, the authors attempted to understand the previous and current birth scenario in this group of neonates, in the three decades comprised by the cohorts. Therefore, this study aimed to verify the prevalence, mortality, and risk factors associated with the birth of VLBW neonates throughout this 33-year period.
MethodsFour cross-sectional studies were analyzed using data from the perinatal interviews of the birth cohorts of the city of Pelotas. Data were collected in the years 1982, 1993, 2004 and 2015, and included all live births in the municipality, from the first to the last day of these years. The strategies used for data collection were similar in all cohorts: structured questionnaires (perinatal in all cohorts and prenatal in 2015, available at http://www.epidemio-ufpel.org.br/site/content/estudos/index.php) applied by previously trained interviewers. The mothers were interviewed soon after the delivery and the newborns were measured, weighed, and examined by a team trained and supervised by a pediatrician.10,11 Data on the few infants born outside the hospital environment were obtained as soon as the mothers sought care after childbirth. Neonatal mortality (between birth and the 27th day of life, including it) was evaluated through visits to hospitals, cemeteries, notaries, and registries, and were obtained through the SIM (Mortality Information System) from 2004 onwards.10–12 The detailed methodological descriptions of each cohort study can be found in the publications by Victora and Barros,13 Victora et al.,14 Santos et al.,15 and Hallal et al.11
In the present study, the newborns were subdivided according to their birth weight into four subgroups: <1500g, 1500–1999g, 2000–2499g and ≥2500g. The cutoff points of 1500 and 2500g are recommended by the World Health Organization (http://www.who.int/reproductivehealth/publications/monitoring/9280638327/en/), and it was decided to subdivide the group between 1500 and 2500g into two subgroups. The distribution of birth weights was described in absolute numbers and percentages. Neonatal mortality was assessed in these groups. For the calculation of gestational age in the 1982 and 1993 cohorts, the date of the last menstrual period reported by the mother was used in the perinatal interview, whereas for the 2004 and 2015 cohorts, the information on gestational age according to the obstetric ultrasound examination was prioritized, and in the absence of this information, the date of the last menstrual period was used. It should also be noted that, in the four cohorts, the gestational age was unknown in approximately 10% of births.
The risk factors studied for VLBW were: monthly family income in minimum wages, maternal age, and type of delivery. The monthly family income was calculated by the sum of the individual incomes and expressed in quintiles of income; maternal age was subdivided into 3 groups: <20 years, 20–34 years, and ≥35 years; and the type of delivery as vaginal or cesarean section. The analyses are shown as tables and charts. The chi-squared test for proportions was used for the contingency tables.16 Poisson regression with robust variance was used for raw and adjusted risk factor analyses (expressed in raw and adjusted prevalence for each cohort). Poisson regression was chosen because, in addition to providing correct estimates, it is the most appropriate method for analysis in cross-sectional studies with binary results,17 making it possible for prevalence ratios to be more easily interpreted and reported when compared with odds ratios calculated by logistic regression.17 The chi-squared test for linear tendency was used for the analysis of deaths in VLBW over the years. The data were analyzed using the statistical software SPSS (IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY, USA).
This study and all procedures related to the cohorts were approved by the Ethics Committees of the institutions involved in the study. In 1982, the mothers gave verbal consent to participate in the research, whereas from 1993 onwards, their consent was obtained in writing. As of 1996, it has been mandatory to submit projects to the Ethics Committee. In 2004, the study was approved under number 40601116 and, in 2015, under CAAE registration 26746414.5.0000.5313.
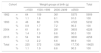
ResultsA total of 19,625 newborns (NBs) were included in the study. The percentages of newborns with VLBW ranged from 0.9% to 1.4%, with no evidence of changes over time (chi-squared test for linear trend, p-value=0.11) and are expressed in Table 1. The total number of newborns that were studied in the VLBW group was 225, being assessed as a single group for the analysis of risk factors. The majority of births (89.9%–91.0%) occurred in the group with birth weight ≥2500g in all the years studied. Only nine (5.3%) of the 169 children with VLBW and with known gestational age had 37 or more weeks. In turn, the weight of 99.9% of the full-term children was >1500g.
Birth weight distribution in the birth cohorts of Pelotas, Brazil, in 1982, 1993, 2004, and 2015.
| Cohort | Weight groups at birth (g) | Total | ||||
|---|---|---|---|---|---|---|
| <1500 | 1500–1999 | 2000–2499 | ≥2500 | |||
| 1982 | n | 64 | 109 | 361 | 5375 | 5909 |
| % | 1.1 | 1.8 | 6.1 | 91.0 | 100 | |
| 1993 | n | 46 | 88 | 376 | 4722 | 5232 |
| % | 0.9 | 1.7 | 7.2 | 90.3 | 100 | |
| 2004 | n | 61 | 81 | 281 | 3803 | 4226 |
| % | 1.4 | 1.9 | 6.6 | 90.0 | 100 | |
| 2015 | n | 54 | 94 | 280 | 3830 | 4258 |
| % | 1.3 | 2.2 | 6.6 | 89.9 | 100 | |
| Total | n | 225 | 372 | 1298 | 17,730 | 19625 |
| % | 1.1 | 1.9 | 6.6 | 90.3 | 100 | |
Chi-squared test for heterogeneity (p<0.001); chi-squared test for linear trend in VLBW prevalence (p=0.11).
Table 2 shows that the prevalence rate of VLBW is close to 2.0 in the poorest 60% of cases (corresponding to quintiles 1, 2, and 3 of family income). The main difference is related to the comparison between this group, which includes 60% of the children, and the wealthiest 40% (quintiles 4 and 5), among which the prevalence was below 1%.
Risk factors for very low birth weight in the birth cohorts of Pelotas, Brazil, in 1982, 1993, 2004, and 2015.
| Prevalence of very low birth weight according to family income, maternal age, and type of delivery. Pelotas, Brazil, 1982–2015. | |||||||
|---|---|---|---|---|---|---|---|
| Income | % VLBW | Prevalence ratio | |||||
| Raw | Adjusted for the cohort | ||||||
| PR (95% CI) | Lower limit | Upper limit | PR (95% CI) | Lower limit | Upper limit | ||
| 1stQuintile | 1.3 | 1.68 | 1.06 | 2.65 | 1.67 | 1.06 | 2.64 |
| 2ndQuintile | 1.6 | 2.14 | 1.38 | 3.31 | 2.16 | 1.40 | 3.33 |
| 3rdQuintile | 1.3 | 1.69 | 1.07 | 2.68 | 1.68 | 1.06 | 2.66 |
| 4thQuintile | 0.9 | 1.17 | 0.72 | 1.92 | 1.17 | 0.71 | 1.91 |
| 5thQuintile | 0.7 | 1.00 | 1.00 | ||||
| p-value | 0.004 | 0.003 | |||||
| Maternal age | |||||||
| <20 years | 1.4 | 1.10 | 0.70 | 1.72 | 1.12 | 0.71 | 1.76 |
| 20–34 years | 1.0 | 0.79 | 0.54 | 1.17 | 0.81 | 0.55 | 1.20 |
| ≥35 years | 1.3 | 1.00 | 1.00 | ||||
| p-value | 0.11 | 0.13 | |||||
| Type of delivery | |||||||
| Vaginal | 1.1 | 1.00 | 1.00 | ||||
| C-section | 1.2 | 1.14 | 0.88 | 1.48 | 1.07 | 0.82 | 1.39 |
| p-value | 0.32 | 0.61 | |||||
VLBW, very low birth weight; PR, prevalence ratio.
Statistics used: Poisson regression.
The adjustment for the cohort years did not change the observed pattern and the differences between the income groups remained (p=0.003). Regarding maternal age, the prevalence of VLBW was slightly lower among mothers aged 20–34, but the difference was not significant (p=0.13). No differences were observed between the prevalence of VLBW according to type of delivery (p=0.61).
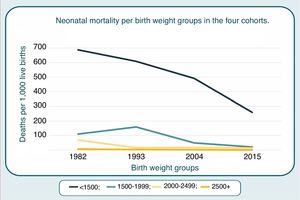
Over the period of 33 years encompassed by the four cohorts, mortality per 1000 live births for neonates weighing <1500g decreased from 688 in 1982 to 259 in 2015 (p<0.001). Among the neonatal deaths, as shown in Fig. 1, the proportion with VLBW increased during the period: 37.9% in 1982, 43.1% in 1993, 60.0% in 2004, and 60.9% in 2015 (p<0.001).
Table 3 shows the results of the multivariate analyses including all factors studied. Only family income showed a significant association (p=0.003) with VLBW after adjustment. The prevalence of VLBW was approximately three-fold higher in the poorest 60%, when compared with the wealthiest quintile.
Multivariate analysis for very low birth weight in the birth cohorts of Pelotas, Brazil, in 1982, 1993, 2004 and 2015.
| Variable | Category | Prevalence ratio | 95% CI | p-value% | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Cohort | 1982 | 0.92 | 0.64 | 1.32 | 0.107 |
| 1993 | 0.73 | 0.49 | 1.09 | ||
| 2004 | 1.17 | 0.81 | 1.69 | ||
| 2015 | 1.00 | ||||
| Gender | Male | 0.87 | 0.67 | 1.14 | 0.314 |
| Female | 1.00 | ||||
| Family income | 1st Quintile | 1.73 | 1.08 | 2.79 | 0.003 |
| 2nd Quintile | 2.24 | 1.43 | 3.50 | ||
| 3rd Quintile | 1.74 | 1.08 | 2.79 | ||
| 4th Quintile | 1.20 | 0.73 | 1.98 | ||
| 5th Quintile | 1.00 | ||||
| Type of delivery | Vaginal | 1.00 | 0.173 | ||
| C-section | 1.21 | 0.92 | 1.58 | ||
| Maternal age | <20 years | 0.98 | 0.62 | 1.55 | 0.270 |
| 20–34 years | 0.79 | 0.54 | 1.16 | ||
| ≥35 years | 1.00 | ||||
The birth cohorts of Pelotas show great potential for the analysis of the temporal evolution of perinatal variables and their risk factors, since they are characterized as population-based studies, covering a broad period of 33 years. The results described herein complement the analyses of the birth weight evolution in Pelotas until 2004, published by Barros et al.18
The present analyses show a significant decrease in mortality among VLBW newborns throughout the years, whereas the prevalence of births with VLBW has been stable, ranging from 0.9% to 1.4%. A study carried out in the state capital (Porto Alegre) by Da Silva et al., with secondary data, found a VLBW prevalence between 1.1% and 1.3% between 1994 and 2005, with a very slight increase trend (p=0.049).
The prevalence rates reported for Porto Alegre are similar to those observed in the present study; it is possible that the borderline level of statistical significance is influenced by the large sample size (more than 20,000 births per year), without indicating a substantial increase in prevalence. The authors report that the increased risk was associated with primiparity.19
Regarding the risk factors, income was the only studied factor that was associated with VLBW, as observed in the study by Sadovsky et al. for overall prematurity.12 In the Porto Alegre study, the authors found that the prevalence of VLBW in public hospitals was 67% higher than in private hospitals, which is in agreement with the association observed for socioeconomic status.19 The same study19 described an 87% increase in the risk of VLBW for cesarean sections in relation to vaginal deliveries, which was not confirmed in the present study. The association between type of delivery and VLBW is difficult to interpret, since early pregnancy interruptions certainly occur due to medical indication in the case of severe maternal conditions.
Regarding maternal age, a large North American study identified an increased risk for preterm birth (<37 weeks) at the extremes of age, <24 years, and >40 years. Those authors found no association for VLBW preterm births or for gestational age <32 weeks, which is consistent with the present results.20
The significant reduction in neonatal mortality of VLBW newborns over the years can be attributed to improved medical care for this part of the population. The 2015 data showed that this reduction was even more pronounced than in the previous cohorts (Fig. 1).21 It should be recalled that, in 1982, there were no neonatal intensive care units in the city, and that the number of beds offered in these units increased from 16 in 1993 to 19 in 2004 and to 29 in 2015. VLBW newborns, however, still account for a large portion of the mortality observed in the neonatal period. In the study “Born in Brazil” of 2011–2012, it was observed that 60% of the neonatal deaths are contained in this VLBW group, which is in agreement with the present findings.8
The present study has some limitations. First, only a few risk factors were selected for analysis, based on the literature on VLBW and neonatal mortality determinants. These included family income, type of delivery, maternal age, sex of the newborn, and year of the cohort, with the latter being used to investigate temporal trends. It was not possible to study public and private hospitals separately, since the analyzed hospitals treat equally patients from the private sector and from the Brazilian Unified Health System.
In conclusion, the prevalence of VLBW remained stable, but there was an evident decrease in mortality among these newborns in recent years. Nonetheless, children with VLBW continue to represent a relevant share of neonatal mortality. The prevention of the birth of very low birth weight children depends not only on the health system improvement but also on policies that can reduce social inequalities.
FundingCoordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
Conflicts of interestThe authors declare no conflicts of interest.
Alicia Matijasevich, Aluísio J.D. Barros, Andréa Damaso Bertoldi, Fernando C. Wehrmeister, Helen Gonçalves, Joseph Murray, Luciana Tovo Rodrigues, Maria Cecília Assumpção, Marlos Rodrigues Domingues, Pedro Rodrigues Curi Hallal
Appendix A lists all the authors of the article..
Please cite this article as: Victora JD, Silveira MF, Tonial CT, Victora CG, Barros FC, Horta BL, et al. Prevalence, mortality and risk factors associated with very low birth weight preterm infants: an analysis of 33 years. J Pediatr (Rio J). 2020;96:327–32.
Study conducted at Universidade Federal de Pelotas (UFPEL), Programa de Pós-Graduação em Epidemiologia, Pelotas, RS, Brazil.