Enuresis may have a negative impact on the self-image in childhood and adolescence. The objective of this study was to evaluate the association between enuresis and psychiatric disorders at 6 and 11 years of age.
Method3,356 children of a birth cohort were evaluated. A standard questionnaire on urinary habits and mental health (Development and Well-Being Assessment [DAWBA]), was used. The prevalence of psychiatric disorders pursuant to the existence of enuresis and its subtypes (monosymptomatic and non-monosymptomatic), stratified by sex, was described. A logistic regression was used for adjusted analysis.
ResultsThe prevalence of enuresis at age 6 years was of 10.2% (9% non-monosymptomatic) and, at 11 years old, of 5.4% (4.5% non-monosymptomatic). At age 6 years, boys with non-monosymptomatic enuresis showed more hyperactivity disorders than those without enuresis (6.2% vs. 2.7%, p=0.017). At 11 years old, after adjustment, among the boys with non-monosymptomatic enuresis, the prevalence of any psychiatric disorder, hyperactivity disorders, and oppositional disorders was, respectively, 3.2, 3.4, and 2.6 times higher than in boys without enuresis; and, among the girls with non-monosymptomatic enuresis, the prevalence of any psychiatric disorder and oppositional disorders was, respectively, 4 and 5.5 times higher than among girls without enuresis.
ConclusionThere is a strong association between non-monosymptomatic enuresis and psychiatric disorders at 6 and 11 years old.
A enurese pode ter grande impacto negativo na autoimagem na infância e adolescência. O objetivo deste estudo foi avaliar a associação entre enurese e transtornos psiquiátricos aos 6 e 11 anos de idade.
MétodosForam avaliadas 3356 crianças de uma coorte de nascimentos. Foi utilizado questionário padronizado sobre hábitos urinários e saúde mental (Development and Well-Being Assesment - DAWBA)). Foi descrita a prevalência de transtornos psiquiátricos conforme a presença de enurese e seus subtipos (monossintomática e não-monossintomática), estratificando por sexo. Para análise ajustada usou-se regressão logística.
ResultadosA prevalência de enurese aos 6 anos foi 10,2% (9% não-monossintomática) e aos 11 anos, 5,4% (4,5% não-monossintomática). Aos 6 anos, meninos com enurese não-monossintomática apresentaram mais transtornos de hiperatividade, em comparação aos não enuréticos (6,2% x 2,7%, p=0,017). Aos 11 anos, após ajuste, entre os meninos com enurese não-monossintomática, a prevalência de qualquer transtorno psiquiátrico, transtornos de hiperatividade e transtornos de oposição foi, respectivamente, 3,2, 3,4 e 2,6 vezes maior do que nos meninos não enuréticos; e entre as meninas com enurese não-monossintomática, a prevalência de qualquer transtorno psiquiátrico e transtornos de oposição foi, respectivamente, 4 e 5,5 vezes maior do que entre meninas não enuréticas.
ConclusõesHá uma forte associação entre enurese não-monossintomática e transtornos psiquiátricos aos 6 e 11 anos de idade.
Enuresis is a chronic, multifactorial condition characterized by genetic, biological, and psychological factors and has a vast impact on the social life of children, adolescents, and their families, limiting opportunities and causing a negative impact on their self-image.1–3
The knowledge of enuresis has been changed throughout the years. In 1815, Guersant associated genetics, male sex, and lower social class with higher prevalence of enuresis; highlighted the influence on the child's mind, describing an “aspect of sadness and shame, affecting even their intelligence.” Formerly, it was seen as an isolated psychiatric disorder. The advances on the researches showed somatic factors as the main factors causing enuresis: nocturnal polyuria, overactive bladder, and parasomnias.4–6 Nowadays, sleep and psychiatric disorders were added to the pathophysiology of enuresis, turning it into a multifactorial pathology.7,8 The concomitance of physiological and behavioral findings and the approach to these two etiologies could make the understanding and treatment easier.9
Regarding the association between enuresis and behavioral disorders, four possible basic combinations have been raised: the behavioral disorder may be consequence of voiding disorders; the behavioral disorder may precede and induce urinary leaks when there is a genetic predisposition to enuresis; enuresis and behavioral disorders may share the same neurobiological disorder; and enuresis and behavioral disorders may randomly coexist, without causal relationship between them.8
Several studies identified that most children with enuresis show psychological disorders, which jeopardize their self-esteem,10–13 and that enuresis is associated with emotional, relationship, and behavioral problems,14 notably attention-deficit/hyperactivity disorder (ADHD), both in clinical trials and epidemiologic studies.15,16
Most studies available were carried out in selected samples of children, usually in specialty outpatient clinics. Birth cohorts, particularly population-based cohorts, may provide more accurate information on the prevalence and association of enuresis with emotional problems. Thus, this study aimed to evaluate the presence of psychiatric disorders in children from the 2014 Pelotas Birth Cohort at ages 6 and 11 years, with or without a history of enuresis.
MethodsThis study is the result of the follow-up of a birth cohort beginning at 2004 in the city of Pelotas, RS, Brazil. The mothers resident in the city were interviewed during their hospitalization for the delivery and their babies were measured (length and weight) and examined. The children were examined again at ages 3, 12, 24, and 47 months, and at 6 and 11 years old, time when the mothers were interviewed and the children went through a series of examinations. At each visit, the mothers answered a questionnaire on the child's health situation, morbidities, diet, sleep patterns, vaccination, and urinary and intestinal habits, as well as data related to maternal health. Sphincter control, urinary and intestinal habits, enuresis, and urinary symptoms have already been described in previous publications.17–19 Information on the methods of the 2014 Pelotas Birth Cohort is available in other publications.20,21 children with malformations on the neurological system, cerebral palsy, mental retardation, and twins were excluded from this article.
EnuresisThe International Classification of Diseases (ICD), version 10, defines enuresis as bedwetting at least once a month, for three months, in children aged 5 years or more. The American Psychiatric Association defines enuresis as bedwetting at least twice a month, for three months. In this analysis, enuresis was defined as bedwetting at night at least once a month for the last three months, according to the mother's report.8 Monosymptomatic enuresis was defined as enuresis without other related urinary or intestinal symptoms; enuresis was considered non-monosymptomatic when there was at least one urinary or intestinal symptom related to enuresis (urinary urgency, holding maneuvers, urinary incontinence, or encopresis).
Urinary and intestinal symptomsThe criteria defined by the International Continence Society were used to assess the urinary symptoms.8 Urinary incontinence was defined as the involuntary leak of small amounts of urine during the day, at least one time at every two weeks, in children aged 3 years or older; holding maneuvers were considered the child's efforts at suppressing the urgency associated with urination, such as crossing the legs, sitting over the heels, squeezing the penis; and urinary urgency, as a urge to urinate. Encopresis was defined as passage of stool for the last three months. Urinary and intestinal symptoms were categorized by frequency, as: never, sometimes (one to 14 days per month), often (15 to 29 days per month), and always (seven days per week), based on Farhat's voiding score described in the assessment at 7 years old.18 This analysis assessed the psychiatric disorders associated with enuresis and its subtypes (monosymptomatic and non-monosymptomatic).
Psychiatric disordersThe Development and Well-Being Assessment (DAWBA) is a diagnosis instrument created by Goodman, et al.22 and translated and validated for Brazilian children by Bacy Fleitlich-Bilyk & Goodmana R23; it used in several epidemiological studies worldwide. The instrument is composed of an initial part with structured questions based on the diagnostic criteria of the DSM-IV and ICD-10, and another part with open questions about the disorders to which there was a minimum number of positive structured questions.22 In the open questions, there is room for a subjective and detailed description of the children's symptoms. The DAWBA must be answered by the legal guardian alone up to 10 years old and, after 11 years old, by the legal guardian and the adolescent itself. DAWBA takes into account the level of loss and suffering caused by the symptoms to the children's and their families’ lives. DAWBA has a final section to assess the child's positive qualities (abilities). For this analysis, the ICD-10 diagnoses were used, to allow comparisons with other studies. Children with mental retardation (score in the IQ test<70 at 6 and 11 years old) were excluded in the analysis of the behavioral and psychiatric symptoms.
For this study, six groups of psychiatric disorders were considered: any problem, emotional changes, anxiety disorders (including separation anxiety, generalized anxiety, obsessive compulsive disorder, social phobia, and specific phobias), depression, hyperactive disorders (hyperactivity and other hyperactivities), and oppositional disorders (defiant, oppositional, unsociability, sociability, and other conduct disorders).
Co-variablesOther variables included in the analysis were: sex of the child, low birth weight (< 2,500g); prematurity (gestational age<37 weeks); number of children in the house other than the child (information obtained at the 48-month consultation); maternal characteristics: education and age (in complete years) at 48 months of the child, and skin color (white, black, or mixed-race); and the family's socioeconomic status, according to the Brazilian National Economic Indicator (Indicador Econômico Nacional [IEN]) in quintiles of reference to Pelotas, based on information provided in the visit at 48 months.
The interviewers were trained to conduct the interviews. All mental health assessments were carried out by trained psychologists, supervised by a psychologist with extensive experience in population-base researches and by a child psychiatrist with major clinic experience. Both were supervised by the author who validated the DAWBA for Brazilian children. Aiming to avoid and identify frauds during the interviews, quality control included the repetition of 10% of the interviews in the house (using a reduced questionnaire), as well as phone calls with the mothers to confirm the interview and assess their satisfaction.
The analysis was performed by using the Stata 12 software (Stata Corp–College Station, TX, United States). First, the distribution of the sample was analyzed and the presence of enuresis at 6 and 11 years old was calculated, pursuant to the characteristics of the mother and the child. Then, the presence of psychiatric disorders at 6 and 11 years old was calculated for the entire cohort and, after stratification per sex, pursuant to the existence of monosymptomatic or non-monosymptomatic enuresis. The analysis by sex was stratified based on the theoretical basis arising from the literature review and a previous article in the same cohort.18 Later, gross and adjusted prevalence ratios and confidence intervals of 95% (95% CI) were calculated by logistic regression for boys and girls separately. For the adjusted analysis, a theoretical conceptual model was created pursuant to the hierarchical relationship between the variables,in order to identify potential confounding factors. The first level included the socio-demographic and birth variables (prematurity, low birth weight, maternal age and education, number of children in the house, maternal skin color, and socioeconomic status); the second level included monosymptomatic or non-monosymptomatic enuresis (for each type of enuresis there was a different logistic regression).
The protocol of all visits was approved by the Research Ethics Committee of the Federal University of Pelotas’ Medical School. A written consent was requested to participate in the study, after the mother was informed about the goals and the confidentiality was ensured. At 11 years old, the adolescents signed an informed consent to participate in the study.
ResultsAmong the 3,356 children assessed, the prevalence of enuresis at age 6 years was of 10.6% (95% CI 9.6-11.7), and of 5.7% (95% CI 4.9–6.5) at 11 years old, both with predominance in boys (decrease in 54% in the prevalence between 6 and 11 years old). In 97.4% of the enuresis cases at 11 years of age, the children already presented symptoms at the age of 6 years. The prevalence of monosymptomatic enuresis in the overall sample at 6 years of age was of 1.2%, with a male predominance (1.4% among boys and 0.8% among girls); and, at 11 years old, of 1% (1.5% among boys and 0.6% among girls).
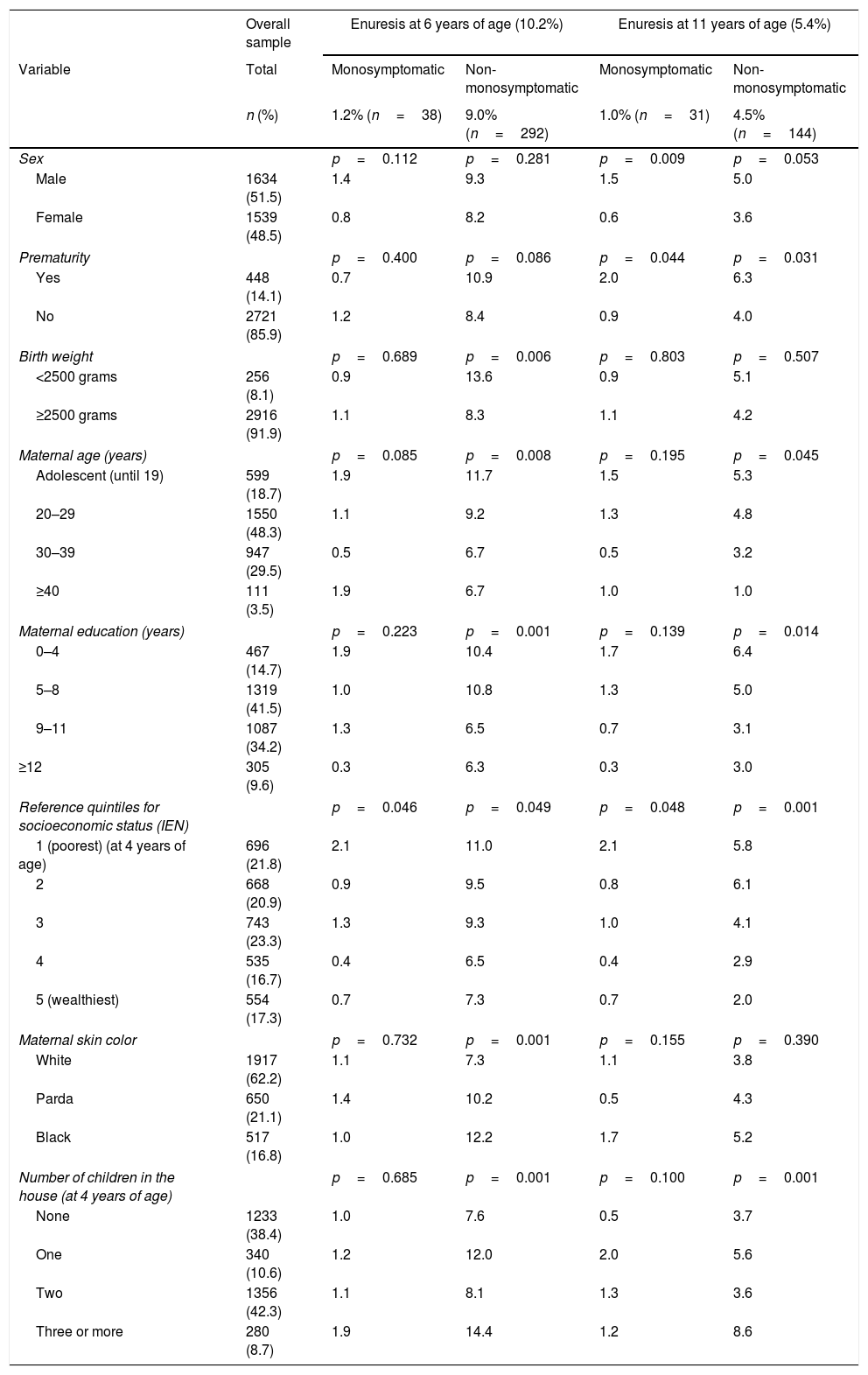
Table 1 describes the prevalence of enuresis and its subtypes at 6 and 11 years old, pursuant to the characteristics of the mother and the child. Boys, children of lower socioeconomic status, children of younger, less educated, and black mothers, and children with higher number of siblings in the house showed higher prevalence of enuresis both at 6 and 11 years old.
Description of the overall sample and presence of mono and non-monosymptomatic enuresis at 6 and 11 years of age. 2004 Pelotas Birth Cohort.
| Overall sample | Enuresis at 6 years of age (10.2%) | Enuresis at 11 years of age (5.4%) | |||
|---|---|---|---|---|---|
| Variable | Total | Monosymptomatic | Non-monosymptomatic | Monosymptomatic | Non-monosymptomatic |
| n (%) | 1.2% (n=38) | 9.0% (n=292) | 1.0% (n=31) | 4.5% (n=144) | |
| Sex | p=0.112 | p=0.281 | p=0.009 | p=0.053 | |
| Male | 1634 (51.5) | 1.4 | 9.3 | 1.5 | 5.0 |
| Female | 1539 (48.5) | 0.8 | 8.2 | 0.6 | 3.6 |
| Prematurity | p=0.400 | p=0.086 | p=0.044 | p=0.031 | |
| Yes | 448 (14.1) | 0.7 | 10.9 | 2.0 | 6.3 |
| No | 2721 (85.9) | 1.2 | 8.4 | 0.9 | 4.0 |
| Birth weight | p=0.689 | p=0.006 | p=0.803 | p=0.507 | |
| <2500 grams | 256 (8.1) | 0.9 | 13.6 | 0.9 | 5.1 |
| ≥2500 grams | 2916 (91.9) | 1.1 | 8.3 | 1.1 | 4.2 |
| Maternal age (years) | p=0.085 | p=0.008 | p=0.195 | p=0.045 | |
| Adolescent (until 19) | 599 (18.7) | 1.9 | 11.7 | 1.5 | 5.3 |
| 20–29 | 1550 (48.3) | 1.1 | 9.2 | 1.3 | 4.8 |
| 30–39 | 947 (29.5) | 0.5 | 6.7 | 0.5 | 3.2 |
| ≥40 | 111 (3.5) | 1.9 | 6.7 | 1.0 | 1.0 |
| Maternal education (years) | p=0.223 | p=0.001 | p=0.139 | p=0.014 | |
| 0–4 | 467 (14.7) | 1.9 | 10.4 | 1.7 | 6.4 |
| 5–8 | 1319 (41.5) | 1.0 | 10.8 | 1.3 | 5.0 |
| 9–11 | 1087 (34.2) | 1.3 | 6.5 | 0.7 | 3.1 |
| ≥12 | 305 (9.6) | 0.3 | 6.3 | 0.3 | 3.0 |
| Reference quintiles for socioeconomic status (IEN) | p=0.046 | p=0.049 | p=0.048 | p=0.001 | |
| 1 (poorest) (at 4 years of age) | 696 (21.8) | 2.1 | 11.0 | 2.1 | 5.8 |
| 2 | 668 (20.9) | 0.9 | 9.5 | 0.8 | 6.1 |
| 3 | 743 (23.3) | 1.3 | 9.3 | 1.0 | 4.1 |
| 4 | 535 (16.7) | 0.4 | 6.5 | 0.4 | 2.9 |
| 5 (wealthiest) | 554 (17.3) | 0.7 | 7.3 | 0.7 | 2.0 |
| Maternal skin color | p=0.732 | p=0.001 | p=0.155 | p=0.390 | |
| White | 1917 (62.2) | 1.1 | 7.3 | 1.1 | 3.8 |
| Parda | 650 (21.1) | 1.4 | 10.2 | 0.5 | 4.3 |
| Black | 517 (16.8) | 1.0 | 12.2 | 1.7 | 5.2 |
| Number of children in the house (at 4 years of age) | p=0.685 | p=0.001 | p=0.100 | p=0.001 | |
| None | 1233 (38.4) | 1.0 | 7.6 | 0.5 | 3.7 |
| One | 340 (10.6) | 1.2 | 12.0 | 2.0 | 5.6 |
| Two | 1356 (42.3) | 1.1 | 8.1 | 1.3 | 3.6 |
| Three or more | 280 (8.7) | 1.9 | 14.4 | 1.2 | 8.6 |
Chi-squared test was used to calculate p-value.
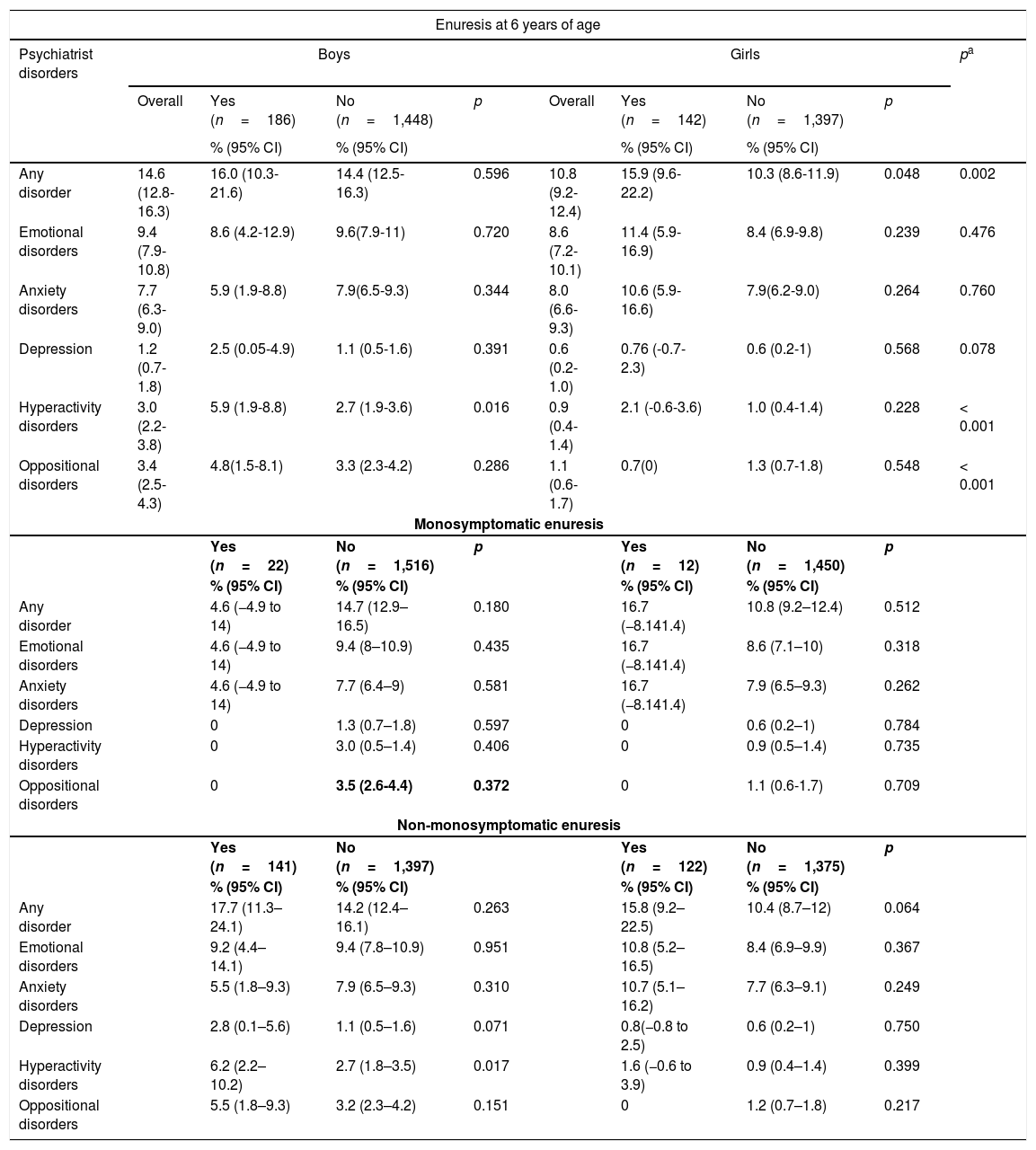
Table 2 describes the prevalence of psychiatric disorders divided by sex, at 6 years of age, in children with and without enuresis. Psychiatric, hyperactivity, and oppositional disorders were more prevalent among boys: 14.6% vs. 10.8%, 3% vs. 0.9%, and 3.4% vs. 1.1%, respectively.
Presence of psychiatric disorders at 6 years of age according to the classification of enuresis, stratified by sex. 2004 Pelotas Birth Cohort.
| Enuresis at 6 years of age | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Psychiatrist disorders | Boys | Girls | pa | ||||||
| Overall | Yes (n=186) | No (n=1,448) | p | Overall | Yes (n=142) | No (n=1,397) | p | ||
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | ||||||
| Any disorder | 14.6 (12.8-16.3) | 16.0 (10.3-21.6) | 14.4 (12.5-16.3) | 0.596 | 10.8 (9.2-12.4) | 15.9 (9.6-22.2) | 10.3 (8.6-11.9) | 0.048 | 0.002 |
| Emotional disorders | 9.4 (7.9-10.8) | 8.6 (4.2-12.9) | 9.6(7.9-11) | 0.720 | 8.6 (7.2-10.1) | 11.4 (5.9-16.9) | 8.4 (6.9-9.8) | 0.239 | 0.476 |
| Anxiety disorders | 7.7 (6.3-9.0) | 5.9 (1.9-8.8) | 7.9(6.5-9.3) | 0.344 | 8.0 (6.6-9.3) | 10.6 (5.9-16.6) | 7.9(6.2-9.0) | 0.264 | 0.760 |
| Depression | 1.2 (0.7-1.8) | 2.5 (0.05-4.9) | 1.1 (0.5-1.6) | 0.391 | 0.6 (0.2-1.0) | 0.76 (-0.7-2.3) | 0.6 (0.2-1) | 0.568 | 0.078 |
| Hyperactivity disorders | 3.0 (2.2-3.8) | 5.9 (1.9-8.8) | 2.7 (1.9-3.6) | 0.016 | 0.9 (0.4-1.4) | 2.1 (-0.6-3.6) | 1.0 (0.4-1.4) | 0.228 | < 0.001 |
| Oppositional disorders | 3.4 (2.5-4.3) | 4.8(1.5-8.1) | 3.3 (2.3-4.2) | 0.286 | 1.1 (0.6-1.7) | 0.7(0) | 1.3 (0.7-1.8) | 0.548 | < 0.001 |
| Monosymptomatic enuresis | |||||||||
| Yes (n=22) | No (n=1,516) | p | Yes (n=12) | No (n=1,450) | p | ||||
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | ||||||
| Any disorder | 4.6 (−4.9 to 14) | 14.7 (12.9–16.5) | 0.180 | 16.7 (−8.141.4) | 10.8 (9.2–12.4) | 0.512 | |||
| Emotional disorders | 4.6 (−4.9 to 14) | 9.4 (8–10.9) | 0.435 | 16.7 (−8.141.4) | 8.6 (7.1–10) | 0.318 | |||
| Anxiety disorders | 4.6 (−4.9 to 14) | 7.7 (6.4–9) | 0.581 | 16.7 (−8.141.4) | 7.9 (6.5–9.3) | 0.262 | |||
| Depression | 0 | 1.3 (0.7–1.8) | 0.597 | 0 | 0.6 (0.2–1) | 0.784 | |||
| Hyperactivity disorders | 0 | 3.0 (0.5–1.4) | 0.406 | 0 | 0.9 (0.5–1.4) | 0.735 | |||
| Oppositional disorders | 0 | 3.5 (2.6-4.4) | 0.372 | 0 | 1.1 (0.6-1.7) | 0.709 | |||
| Non-monosymptomatic enuresis | |||||||||
| Yes (n=141) | No (n=1,397) | Yes (n=122) | No (n=1,375) | p | |||||
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | ||||||
| Any disorder | 17.7 (11.3–24.1) | 14.2 (12.4–16.1) | 0.263 | 15.8 (9.2–22.5) | 10.4 (8.7–12) | 0.064 | |||
| Emotional disorders | 9.2 (4.4–14.1) | 9.4 (7.8–10.9) | 0.951 | 10.8 (5.2–16.5) | 8.4 (6.9–9.9) | 0.367 | |||
| Anxiety disorders | 5.5 (1.8–9.3) | 7.9 (6.5–9.3) | 0.310 | 10.7 (5.1–16.2) | 7.7 (6.3–9.1) | 0.249 | |||
| Depression | 2.8 (0.1–5.6) | 1.1 (0.5–1.6) | 0.071 | 0.8(−0.8 to 2.5) | 0.6 (0.2–1) | 0.750 | |||
| Hyperactivity disorders | 6.2 (2.2–10.2) | 2.7 (1.8–3.5) | 0.017 | 1.6 (−0.6 to 3.9) | 0.9 (0.4–1.4) | 0.399 | |||
| Oppositional disorders | 5.5 (1.8–9.3) | 3.2 (2.3–4.2) | 0.151 | 0 | 1.2 (0.7–1.8) | 0.217 | |||
At 6 years of age, boys with enuresis showed higher prevalence of hyperactivity disorders when compared with those without enuresis (5.9% vs. 2.7%, respectively). Among the girls with enuresis, the prevalence of any psychiatric disorder was about 50% higher compared to girls without enuresis (15.9% vs. 10.3%). When enuresis was classified as monosymptomatic and non-monosymptomatic, only hyperactivity disorder in boys with non-monosymptomatic enuresis was shown to be more prevalent.
Regarding the presence or absence of urinary incontinence at 6 years of age, boys had higher rates of any type of psychiatrist disorders (22% vs. 13.8%, respectively) and oppositional disorders (7.6% vs. 3%); among girls, the rates were 16.9% vs. 10% for psychiatric disorders, and 3.5% vs. 0.6% for hyperactivity disorders. Children with encopresis were more likely to have any psychiatrist disorder when compared with those without encopresis: 23.6% vs. 14.2% among boys and 28.6% vs. 10.6% among girls; such as the hyperactivity disorders among girls (7.1% vs. 1.1%; data not shown in the tables).
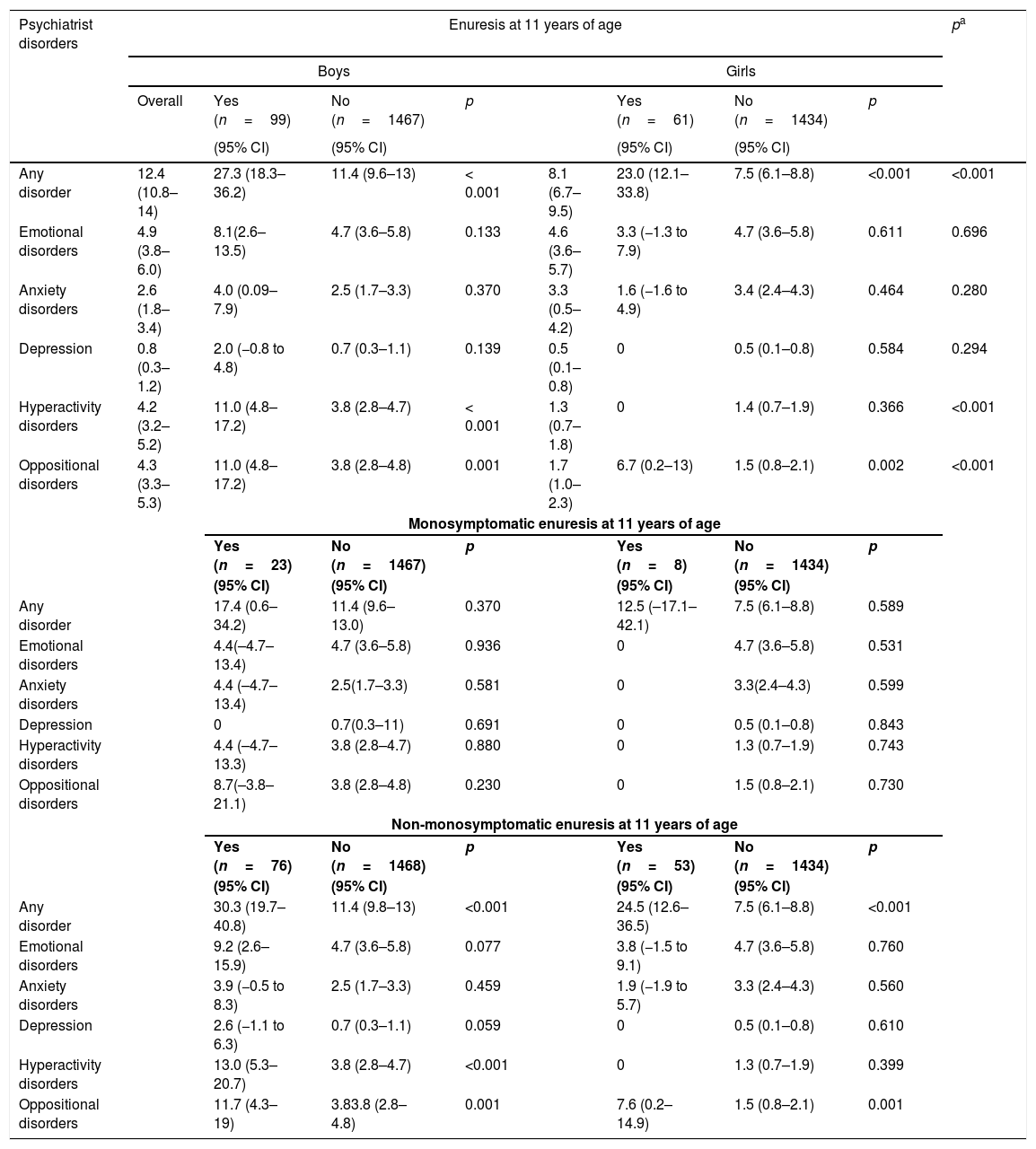
At 11 years of age (Table 3), the prevalence of any psychiatrist, hyperactivity, and oppositional disorders was higher among boys than among girls, and among boys with monosymptomatic enuresis. Among girls, the presence of any disorder was three times higher; the presence of oppositional disorder was five times higher among girls with non-monosymptomatic enuresis.
Presence of psychiatric disorders at 11 years of age according to the classification of enuresis, stratified by sex. 2004 Pelotas Birth Cohort.
| Psychiatrist disorders | Enuresis at 11 years of age | pa | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Boys | Girls | ||||||||
| Overall | Yes (n=99) | No (n=1467) | p | Yes (n=61) | No (n=1434) | p | |||
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | ||||||
| Any disorder | 12.4 (10.8–14) | 27.3 (18.3–36.2) | 11.4 (9.6–13) | < 0.001 | 8.1 (6.7–9.5) | 23.0 (12.1–33.8) | 7.5 (6.1–8.8) | <0.001 | <0.001 |
| Emotional disorders | 4.9 (3.8–6.0) | 8.1(2.6–13.5) | 4.7 (3.6–5.8) | 0.133 | 4.6 (3.6–5.7) | 3.3 (−1.3 to 7.9) | 4.7 (3.6–5.8) | 0.611 | 0.696 |
| Anxiety disorders | 2.6 (1.8–3.4) | 4.0 (0.09–7.9) | 2.5 (1.7–3.3) | 0.370 | 3.3 (0.5–4.2) | 1.6 (−1.6 to 4.9) | 3.4 (2.4–4.3) | 0.464 | 0.280 |
| Depression | 0.8 (0.3–1.2) | 2.0 (−0.8 to 4.8) | 0.7 (0.3–1.1) | 0.139 | 0.5 (0.1–0.8) | 0 | 0.5 (0.1–0.8) | 0.584 | 0.294 |
| Hyperactivity disorders | 4.2 (3.2–5.2) | 11.0 (4.8–17.2) | 3.8 (2.8–4.7) | < 0.001 | 1.3 (0.7–1.8) | 0 | 1.4 (0.7–1.9) | 0.366 | <0.001 |
| Oppositional disorders | 4.3 (3.3–5.3) | 11.0 (4.8–17.2) | 3.8 (2.8–4.8) | 0.001 | 1.7 (1.0–2.3) | 6.7 (0.2–13) | 1.5 (0.8–2.1) | 0.002 | <0.001 |
| Monosymptomatic enuresis at 11 years of age | |||||||||
| Yes (n=23) | No (n=1467) | p | Yes (n=8) | No (n=1434) | p | ||||
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | ||||||
| Any disorder | 17.4 (0.6–34.2) | 11.4 (9.6–13.0) | 0.370 | 12.5 (–17.1–42.1) | 7.5 (6.1–8.8) | 0.589 | |||
| Emotional disorders | 4.4(–4.7–13.4) | 4.7 (3.6–5.8) | 0.936 | 0 | 4.7 (3.6–5.8) | 0.531 | |||
| Anxiety disorders | 4.4 (–4.7–13.4) | 2.5(1.7–3.3) | 0.581 | 0 | 3.3(2.4–4.3) | 0.599 | |||
| Depression | 0 | 0.7(0.3–11) | 0.691 | 0 | 0.5 (0.1–0.8) | 0.843 | |||
| Hyperactivity disorders | 4.4 (–4.7–13.3) | 3.8 (2.8–4.7) | 0.880 | 0 | 1.3 (0.7–1.9) | 0.743 | |||
| Oppositional disorders | 8.7(–3.8–21.1) | 3.8 (2.8–4.8) | 0.230 | 0 | 1.5 (0.8–2.1) | 0.730 | |||
| Non-monosymptomatic enuresis at 11 years of age | |||||||||
| Yes (n=76) | No (n=1468) | p | Yes (n=53) | No (n=1434) | p | ||||
| (95% CI) | (95% CI) | (95% CI) | (95% CI) | ||||||
| Any disorder | 30.3 (19.7–40.8) | 11.4 (9.8–13) | <0.001 | 24.5 (12.6–36.5) | 7.5 (6.1–8.8) | <0.001 | |||
| Emotional disorders | 9.2 (2.6–15.9) | 4.7 (3.6–5.8) | 0.077 | 3.8 (−1.5 to 9.1) | 4.7 (3.6–5.8) | 0.760 | |||
| Anxiety disorders | 3.9 (−0.5 to 8.3) | 2.5 (1.7–3.3) | 0.459 | 1.9 (−1.9 to 5.7) | 3.3 (2.4–4.3) | 0.560 | |||
| Depression | 2.6 (−1.1 to 6.3) | 0.7 (0.3–1.1) | 0.059 | 0 | 0.5 (0.1–0.8) | 0.610 | |||
| Hyperactivity disorders | 13.0 (5.3–20.7) | 3.8 (2.8–4.7) | <0.001 | 0 | 1.3 (0.7–1.9) | 0.399 | |||
| Oppositional disorders | 11.7 (4.3–19) | 3.83.8 (2.8–4.8) | 0.001 | 7.6 (0.2–14.9) | 1.5 (0.8–2.1) | 0.001 | |||
Boys with urinary incontinence had higher rates of any disorder (29.6% vs. 11.6%), emotional (16.9% vs. 4.4%), anxiety (9.9% vs. 2.3%), hyperactivity (11.3% vs. 3.9%), and oppositional disorders (12.7% vs. 3.9%), as well as depression (4.2% vs. 0.6%). Girls also had higher rates of any psychiatric (19.5% vs. 7.5%) and hyperactivity disorders (3.9% vs. 1.1%) when compared with children without incontinence.
Boys with encopresis had higher rates of any psychiatric (31.9% vs. 11.8%), emotional (14.9% vs. 4.6%), anxiety (10.6% vs. 2.4%), and hyperactivity disorders (10.6% vs. 4%), and the same happened with girls regarding anxiety disorders (15.4%. 3.1%) when compared with children without encopresis (data not shown in the tables).
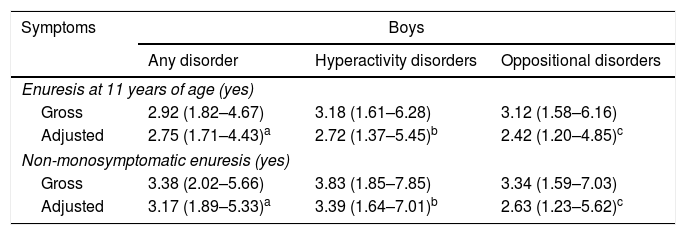
The multivariable analysis (Table 4) showed that the presence of non-monosymptomatic enuresis at 11 years of age maintained the association with psychiatric disorders (hyperactivity and oppositional disorders among boys; and oppositional disorders among girls), even after adjustment for confounding factors. Monosymptomatic enuresis was not associated with psychiatric disorders in both sexes at 6 or 11 years of age.
Gross odds ratios adjusted for psychiatric disorders at 11 years of age, according to the report of enuresis at 11 years of age. 2004 Pelotas Birth Cohort.
| Symptoms | Boys | ||
|---|---|---|---|
| Any disorder | Hyperactivity disorders | Oppositional disorders | |
| Enuresis at 11 years of age (yes) | |||
| Gross | 2.92 (1.82–4.67) | 3.18 (1.61–6.28) | 3.12 (1.58–6.16) |
| Adjusted | 2.75 (1.71–4.43)a | 2.72 (1.37–5.45)b | 2.42 (1.20–4.85)c |
| Non-monosymptomatic enuresis (yes) | |||
| Gross | 3.38 (2.02–5.66) | 3.83 (1.85–7.85) | 3.34 (1.59–7.03) |
| Adjusted | 3.17 (1.89–5.33)a | 3.39 (1.64–7.01)b | 2.63 (1.23–5.62)c |
| Girls | |||
|---|---|---|---|
| Any disorder | Hyperactivity disorders | Oppositional disorders | |
| Enuresis at 11 years of age (yes) | |||
| Gross | 3.69 (1.97–6.93) | 4.73 (1.57–14.2) | |
| Adjusted | 3.62 (1.89–5.95)d | 4.73 (1.57–14.2) | |
| Non-monosymptomatic enuresis (yes) | |||
| Gross | 4.03 (2.09–7.77) | 5.50 (1.82–16.6) | |
| Adjusted | 3.95 (2.0–7.81)d | 5.50 (1.82–16.6) | |
Despite the low prevalence of psychiatric disorders in the children assessed, the authors observed that it increased significantly in children with non-monosymptomatic enuresis.
Among the positive aspects of this study, there is the fact that all children of a birth cohort were assessed, as the study was not limited to children seeking treatment, which are often the most severe cases or those in which the condition already shows negative consequences in the children's or the families’ lives. Moreover, for definition of the outcomes, the study used a tool validated for Brazil that enables the diagnosis for psychiatrist disorders (DAWBA) rather than a simple tracking tool, as used in most studies.22,23
In turn, the present study presented limitation due to the absence of medical examinations, as the physical examination is recommended in the investigation of urinary problems. Additionally, mental, intestinal, and urinary symptoms were reported by the mothers in an interview, being subject to bias.
The present findings are consistent with the results observed in other populations. The Tokyo Early Adolescence study showed an independent association between enuresis and ADHD in a population of adolescents at 10 years of age. Other behavioral disorders were not verified in that study. From the biological standpoint, neurophysiology and neuroimaging studies suggest an immaturity in the development of the central nervous system common to both pathologies.24
In the study by Shreeram et al., 1,136 American children aged between 8 and 11 years were evaluated using data of the NHANES 2001-2004 study, and a risk 2.9 times higher of ADHD was observed15 among children with enuresis when compared with children without enuresis. Such finding is consistent with those of the present study, which showed a probability 3.4 times higher of ADHD among children with non-monosymptomatic enuresis.
Baeyens et al. found a presence of 15% of ADHD in a population of children with enuresis, in contrast with the rate of 3-5% among the overall population. Accordingly, Ferguson et al., in a longitudinal study in New Zealand, observed that children who still had enuresis after the age of 10 years showed conduct, attention, and hyperactivity problems at the age of 13 years and anxiety and introversion at the age of 15 years when compared with children whose enuresis stopped around 5 years of age.25
The International Children Continence Society (ICCS) recommends screening for behavioral and emotional problems, especially for ADHD, in children with enuresis.26
The study by Van Hoecke showed that children with enuresis, and especially with urinary incontinence, presented higher scores in the evaluation of low self-esteem, had concentration issues, were less cooperative, and were more likely to lose their temper when compared with children without enuresis.14
Von Gontard demonstrated that children with enuresis, urinary incontinence, and encopresis showed four times more risk to have behavioral comorbidities and psychological symptoms when compared with a normal population, and that these changes interfered with treatment, suggesting that both pathologies should be addressed.27
Uropsychological care focusing on both pathologies is important. Some researchers believe in a neurocentric rather than a vesicocentric assessment.28
The treatment of enuresis requires behavioral measures, and changes in the habits regarding liquid intake and frequency of urination. Adherence to treatment is important, as well as the persistence to follow the recommendations, both by the child and their family members, who many times may be intolerant towards the child.5,29 Some personality and behavioral characteristics may interfere with the results and must be evaluated. As Van Hoecke stated, children less motivated and with lower concentration may present difficulties in following the routine of liquid intake and eliminations (times scheduled for urinating), and might show less sensibility to the sign of a full bladder.14 Children less cooperative may not be perform the requested task, and low self-esteem leads to listlessness when they take too long to be succeeded in the treatment, which, in enuresis case, takes time. Irritable children get easily frustrated in the absence of immediate results and stop the treatment.
Emotional and behavioral disorders are frequent among children with enuresis, encopresis, and urinary incontinence, and it is recommended that pediatricians and other healthcare practitioners recognize the psychiatric disorders in patients with lower urinary tract dysfunction (LUTD), so that they can refer patients to specialists in order to reduce their suffering and enhance their prognosis. Accordingly, it is also necessary to alert the mental-care practitioners to the possibility of associating psychiatric disorders with LUTD.30
Another important data is that many families do not seek care for enuresis because of established family beliefs. Scholomer23 found that 55% sought treatment for enuresis in a clinic of urological problems (in children who were examined for other pathologies). Most mothers thought that heavy sleepiness, laziness, attempts to call attention to themselves, and emotional problems were the main causes of enuresis, and a common problem in the family. They attempted to control the problem by themselves before seeking help. Practitioners must screen for enuresis symptoms in children with psychiatrist disorders in order to help in the treatment.
It can be concluded that psychiatric disorders are more prevalent in children with non-monosymptomatic enuresis. It is recommended that pediatricians recognize and properly assess enuresis and its association with other urinary (especially urinary incontinence) and intestinal symptoms (encopresis), as well as the presence of psychiatric disorders, which are common in this population.
Funding2004 Cohort
This article used data from the study “2004 Pelotas Birth Cohort,” carried out by the Postgraduate program in Epidemiology of the Federal University of Pelotas, supported by the Brazilian Association of Collective Health–ABRASCO. From 2009 to 2013, the 2004 birth cohort was funded by the Wellcome Trust. Previous stages of the study were funded by the World Health Organization, the National Support Program for Centers of Excellence (PRONEX), the National Council for Scientific and Technological Development (CNPq), the Ministry of Health, and the Child's Pastoral.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Mota DM, Matijasevich A, Santos IS, Petresco S, Mota LM. Psychiatric disorders in children with enuresis at 6 and 11 years old in a birth cohort. J Pediatr (Rio J). 2019. https://doi.org/10.1016/j.jped.2018.11.010
Study conducted at Universidade Federal de Pelotas (UFPel), Faculdade de Medicina, Pelotas, RS, Brasil.