To generate prediction equations for spirometry in 4- to 6-year-old children.
MethodsForced vital capacity, forced expiratory volume in 0.5s, forced expiratory volume in one second, peak expiratory flow, and forced expiratory flow at 25–75% of the forced vital capacity were assessed in 195 healthy children residing in the town of Sete Lagoas, state of Minas Gerais, Southeastern Brazil. The least mean squares method was used to derive the prediction equations. The level of significance was established as p<0.05.
ResultsOverall, 85% of the children succeeded in performing the spirometric maneuvers. In the prediction equation, height was the single predictor of the spirometric variables as follows: forced vital capacity=exponential [(−2.255)+(0.022×height)], forced expiratory volume in 0.5s=exponential [(−2.288)+(0.019×height)], forced expiratory volume in one second=exponential [(−2.767)+(0.026×height)], peak expiratory flow=exponential [(−2.908)+(0.019×height)], and forced expiratory flow at 25–75% of the forced vital capacity=exponential [(−1.404)+(0.016×height)]. Neither age nor weight influenced the regression equations. No significant differences in the predicted values for boys and girls were observed.
ConclusionThe predicted values obtained in the present study are comparable to those reported for preschoolers from both Brazil and other countries.
Gerar equações de predição da espirometria em crianças de quatro a seis anos.
MétodosCapacidade vital forçada, volume expiratório forçado em 0,5 segundo, volume expiratório forçado em 1 segundo, pico de fluxo expiratório e fluxo expiratório forçado com 25-75% da capacidade vital forçada foram avaliados em 195 crianças saudáveis que residem na cidade de Sete Lagoas, Estado de Minas Gerais, Sudeste do Brasil. O método dos mínimos quadrados foi usado para derivar as equações de predição. O nível de significância foi estabelecido como p < 0,05.
ResultadosNo geral, 85% das crianças foram bem-sucedidas ao fazer as manobras espirométricas. Na equação de predição, a estatura foi a única variável preditora das variáveis espirométricas, da seguinte forma: capacidade vital forçada = exponencial [(-2,255) + (0,022 x estatura)], volume expiratório forçado em 0,5 segundo = exponencial [(-2,288) + (0,019 x estatura)], volume expiratório forçado em 1 segundo = exponencial [(-2,767) + (0,026 x estatura)], pico do fluxo expiratório = exponencial [(-2,908) + (0,019 x estatura)] e fluxo expiratório forçado com 25-75% da capacidade vital forçada = exponencial [(-1,404) + (0,016 x estatura)]. Nem a idade nem o peso influenciaram as equações de regressão. Não foi observada diferença significativa nos valores previstos em meninos e meninas.
ConclusãoOs valores previstos obtidos neste estudo são comparáveis àqueles relatados em crianças em idade pré-escolar tanto do Brasil quanto de outros países.
Pulmonary function tests supplement the clinical histories and physical examinations of individuals with respiratory problems and contribute to the diagnosis, prognosis, and monitoring of respiratory diseases, as well as assessments of the therapeutic effects of interventions.1
Spirometry is a universally accepted method for assessing pulmonary function, including lung volumes and flows, and is the most widely used method for detecting functional alterations in the pulmonary functions of adults, adolescents, and schoolchildren.1,2 However, spirometry has not yet been widely studied in Latin American or Brazilian preschool populations.1,3
The earliest studies that assessed spirometric maneuvers in preschoolers were published approximately 20 years ago.4,5 Currently, it is well established in the literature that 75–86% of preschoolers are able to acceptably and reproducibly perform spirometric maneuvers1,3,6–10 as evidenced by the availability of prediction equations for preschoolers from several countries.6,8,9,11–17 Additionally, a recent multicenter study16 proposed prediction equations for spirometric variables from preschoolers based on data collected from the children from 11 different countries (n=3777), including Brazil. An update was published in 2012 and included new multi-ethnic equations.18 Recently, Burity et al.19 described reference values based on 135 northeastern Brazilian preschoolers and identified height and sex as predictors of lung function parameters. However, these equations are not necessarily representative of the entire population of Brazilian preschoolers.
Due to the importance of spirometry in all age groups and the scarcity of prediction equations for spirometric variables for preschoolers in Brazil, the present study aimed to describe the prediction equations for spirometry in 4- to 6-year-old children residing in the town of Sete Lagoas, state of Minas Gerais, southeastern Brazil.
MethodsSetting and samplingThe subjects were recruited at randomly selected public and private schools in the town of Sete Lagoas according to the following inclusion criteria: age between 4 and 6 years (i.e., 48–83 months old); no chronic respiratory disease according to the American Thoracic Society and Division of Lung Disease ATS/DLD/78/C-questionnaire (i.e., total scores that are equal to or lower than 6)6,20; body mass index (BMI) between the 3rd and 95th percentiles for age21; birth weight greater than 2500g at a gestational age of 37–42 weeks20; no flu episodes within the previous seven days; no history of maternal smoking during pregnancy or exposure to tobacco smoking over the years preceding the spirometric assessment; no past history of thoracic or abdominal surgery; no thoracic malformations, genetic syndromes, metabolic dysfunctions, heart diseases, neuromuscular diseases, mental disorders, or cognitive deficits; and no use of medicines on a regular basis.
The study protocol and informed consent (provided by the parents or legal guardians) were approved by the Ethics in Research Committee of the Universidade Federal de Minas Gerais (ETIC No. 0612.0.203.000-09).
Measurement instruments and proceduresThe ATS-DLD-78-C questionnaire was used to rule out the presence of respiratory diseases and exposure to environmental pollutants. This questionnaire consists of questions about the symptoms, other illnesses and hospitalizations related to respiratory tract diseases, and it was completed by the parents or legal guardians. The overall scores ranged from 0 to 22, and scores greater than or equal to 7 were indicative of a chronic respiratory disease.6 Supplementary questions, for example, questions about gestational age, the neonatal period and concomitant diseases, were also included.
A handheld Koko spirometer (Koko®, PFT type; nSpire Health Inc., CO, USA) was used to assess the spirometric variables obtained from the forced expiratory maneuvers. This equipment meets all of the requirements of the ATS/ERS1 and displays real-time graphs of the flow/volume and volume/time curves. Following the ATS recommendations, a disposable mouthpiece and antibacterial filter that together result in a dead space of less than 2mL/kg were used. The accuracy of the equipment was verified daily via calibration using a three-liter manual syringe (COSMED, Pulmonary Function Equipment – Italy). The following spirometric variables were analyzed: FVC, FEV0.5, FEV1, FEF25–75, and PEF. The data for the forced expiratory time (FET) and back-extrapolated volume (BEV) were collected to ensure the qualities of the curves.1
The data from all of the questionnaires were analyzed, and the children who met the inclusion criteria were invited to participate in the study. Children whose parents/guardians authorized their participation in the study and signed an informed consent form were assessed during regular school activities.
The physical examinations were initiated by measuring the weight using a single scale (Filizola – São Paulo, Brazil) and the height using a Harpenden® stadiometer (Harpenden Skinfold Caliper, Mediflex Surgical Products, USA) (measurement range from 60.0cm to 210.0cm, wall mounted, with a precision of 0.1cm, with the child standing, barefoot, positioned in such a manner that the head, shoulders, buttocks, and heels lightly touched the vertical surface of the measuring device). Subsequently, blood pressure, heart rate, respiratory rate, oxygen saturation, and lung auscultation were assessed, and static and dynamic inspections of the breathing pattern were performed to confirm the absence of any clinical abnormality.
To perform spirometry, the recommended acceptability and reproducibility criteria were followed.1 Before the test, each child received age-appropriate instructions and then performed the maneuvers. The measurements were collected with the subject seated using a disposable well-adjusted mouthpiece (to prevent leaks), a nose clip, and computer-animation programs that provided instructions and stimuli to the participants.2 The subjects were asked to breathe in the tidal volume and then instructed to fill their lungs as much as possible and blow as strongly, rapidly and long as possible. The acceptability criteria were as follows: the flow-volume and volume-time curves were inspected, and maneuvers that were visibly inadequate were excluded, i.e., when the flow-volume curve did not exhibit a rapid rise to the peak flow and a smooth descending limb with no evidence of a cough or glottic closure; the BEV was equal or lower than 80mL or lower than 12.5% of the FVC; and the FET was greater than 10% of the PEF rate. The reproducibility criteria were as follows: the difference between the FVC and FEV1 was lower than 10% or 100mL for at least two reproducible maneuvers.1 The test was limited to 20min to ensure clinical applicability, and the subjects were allowed one minute of rest between two consecutive maneuvers that were conducted by the same investigator (DCF) in all subjects.
The volume–time and flow–volume curves were visually examined by two independent observers who were blinded to the children's past and current health status. Specifically, the maximum values of the FVC, FEV0.5, FEV1, and PEF were obtained using the appropriate and reproducible curve (the maximum values for each of the variables could come from different curves). The FEF25–75 value was selected from the curve that exhibited the largest sum of FVC and FEV1, and the FEV0.5 value was obtained from the curve with the greater FEV1 value or the greater FEV0.5 when the FET was ≤1s.1
Statistical analysisAccording to the age ranges (i.e., 48–59, 60–71, and 72–83 months) and sex (boys and girls), 180 healthy preschoolers were arbitrarily pre-defined within the target age range as the minimum that should be assessed in the present study. A cluster randomization was performed based on the official list of the existing public and private schools in the city of Sete Lagoas. Eleven schools were randomly selected (seven public and four private institutions) while maintaining a public/private school ratio of 1.75, which was based on the proportions of registered students. Then, all 4- to 6-year-old children registered in each school were invited to participate in the study.
The Kolmogorov–Smirnov test was used to verify data normality. The comparisons of the anthropometric data and spirometric data between the male and female children were performed using independent samples t-tests. One-way analysis of variance (ANOVA) followed by post hoc Hochberg multiple comparison tests were used to compare the anthropometric data and variables from the pulmonary function tests between the 4- to 6-year-old children.
To generate the prediction equations for the spirometric variables, the least mean squares method was used. First, logarithmic transformations were applied to the spirometric variables with Box–Cox analyses. Linear regressions were performed between the spirometric (dependent) variables and the height, weight, sex, and age (exploratory variables). Then, a multiple regression analysis was performed. Following the evaluation of the multiple regression analysis, the normality and homoscedasticity of the residuals were established using Q–Q plots. The residual assumptions were satisfied. The results were expressed as z-scores, i.e., multiples of the standard deviation of the mean, and the graphs with the regression curves and z-scores were plotted to facilitate the use of the equations in clinical practice and research.
All tests were assessed at an alpha of 0.05 with no adjustments for multiple comparisons. The data were analyzed using the R statistical language (Free Software Foundation – Boston, MA, USA) and SPSS (SPSS Inc. Released 2009. SPSS for Windows, Version 15.0, IL, USA).
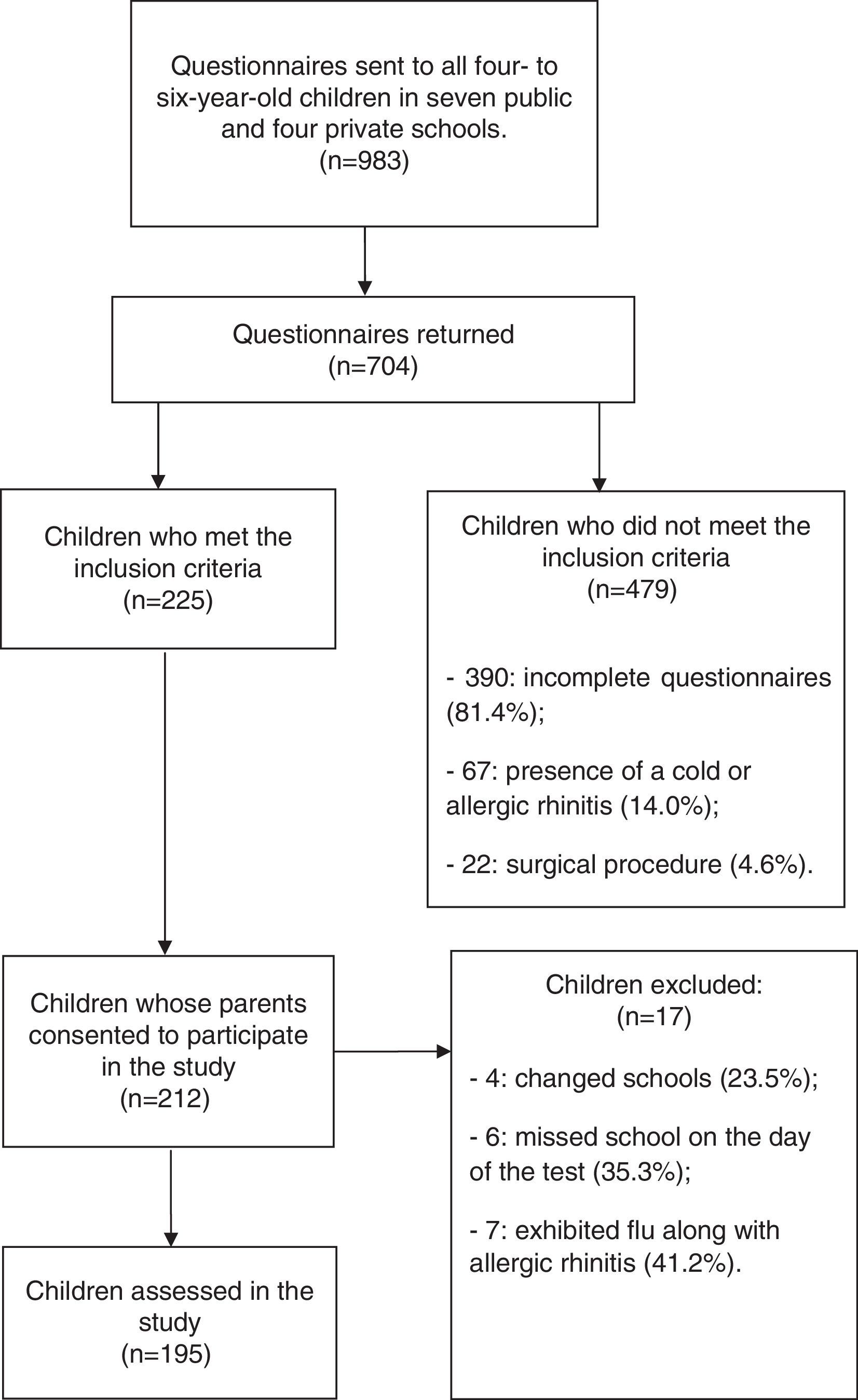
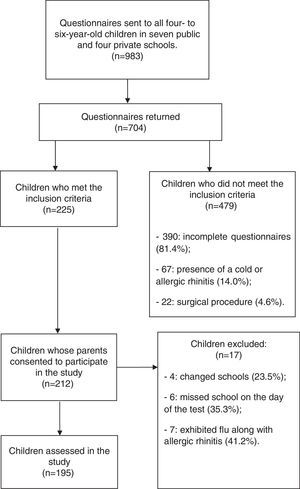
ResultsFig. 1 depicts the study flowchart and indicates that 195 children were initially assessed and that 131 (67%) public school and 64 (33%) private school students were enrolled in the study from June 2010 to August 2011.
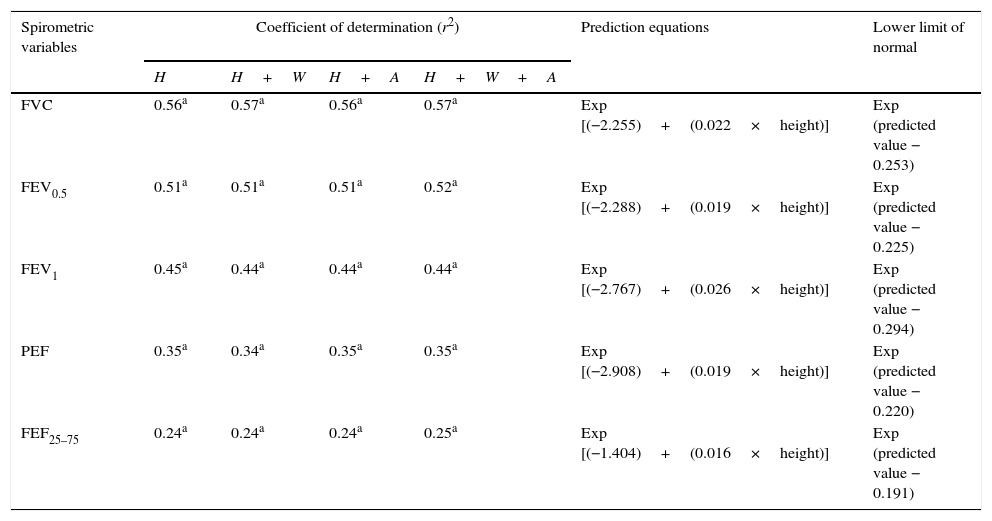
Table 1 presents the coefficients of determination (r2) of the regression equations for the spirometric variables with the independent variables of height, height+weight, height+age, and height+weight+age. The r2 values exhibited little variation (approximately 1%) when height was used as the single predictor of the spirometric variables with height+weight+age as the independent variables in the regression equations. Table 1 also presents the regression equations and the lower normal limits (i.e., −1.64 z-scores) for the spirometric variables with height as the single predictor.
Coefficient of determination of the multiple regression analyzes for spirometric variables, considering the explanatory variables: height, height+weight, height+age, and height+weight+age; as well as the lower limit of normal and prediction equations for spirometric variables according to height.
| Spirometric variables | Coefficient of determination (r2) | Prediction equations | Lower limit of normal | |||
|---|---|---|---|---|---|---|
| H | H+W | H+A | H+W+A | |||
| FVC | 0.56a | 0.57a | 0.56a | 0.57a | Exp [(−2.255)+(0.022×height)] | Exp (predicted value − 0.253) |
| FEV0.5 | 0.51a | 0.51a | 0.51a | 0.52a | Exp [(−2.288)+(0.019×height)] | Exp (predicted value − 0.225) |
| FEV1 | 0.45a | 0.44a | 0.44a | 0.44a | Exp [(−2.767)+(0.026×height)] | Exp (predicted value − 0.294) |
| PEF | 0.35a | 0.34a | 0.35a | 0.35a | Exp [(−2.908)+(0.019×height)] | Exp (predicted value − 0.220) |
| FEF25–75 | 0.24a | 0.24a | 0.24a | 0.25a | Exp [(−1.404)+(0.016×height)] | Exp (predicted value − 0.191) |
H, height (cm); W, weight (kg); A, age (months); Exp, exponential; FVC, forced vital capacity (L); FEV0.5, forced expiratory volume in 0.5s (L); FEV1, forced expiratory volume in one second (L); PEF, peak expiratory flow (L/min); FEF25–75, forced expiratory flow at 25–75% of the FVC (L/s).
The linear regression between the spirometric parameters (dependent variables) and height, weight, and age (independent variables) exhibited a statistically significant association. However, the spirometric variables did not present a statistically significant association with sex.
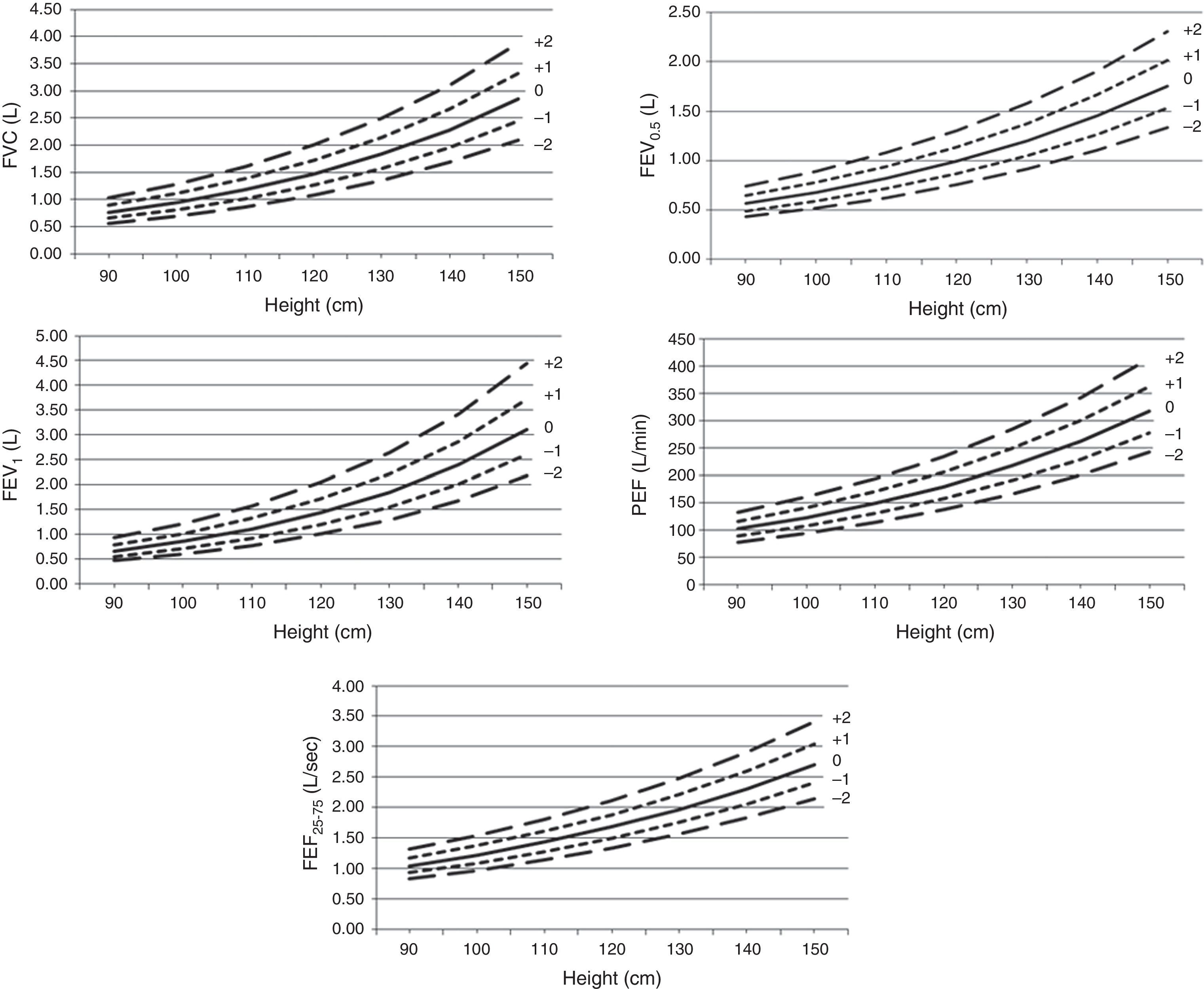
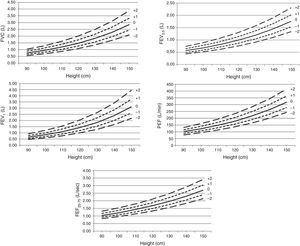
The graphs of the spirometric variables according to height in which the z-scores are plotted and shown in Fig. 2. As illustrated, shorter heights were associated with less variability in each of the spirometric parameters studied.
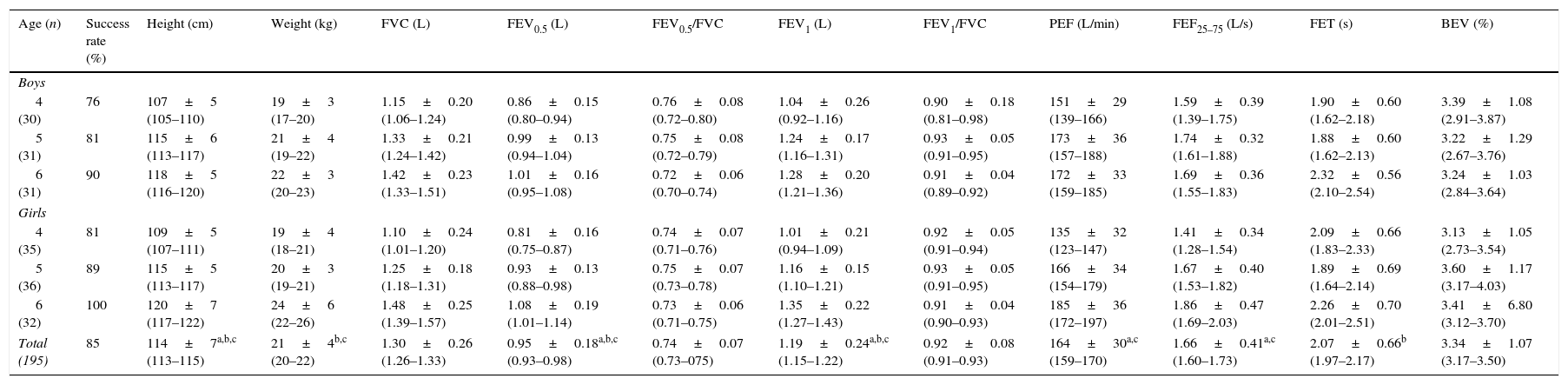
Table 2 presents the proportion of children who successfully performed spirometry, the anthropometric data, and the spirometric parameters by age of the 195 children. Overall, 85% of the children successfully performed the spirometric maneuvers, and the success rate progressively increased with age. The sample from which the curves were generated and the equations were derived was predominantly of mixed ethnicity (134 out of 166, i.e., 80.7%), white (27 out of 166, i.e., 16.3%), and those Asian/African descendants (only five out of 166, i.e., 3.0%). This information was obtained from parents’ report. The comparisons of the anthropometric data and spirometric variables between the boys and girls did not reveal significant differences (p>0.05, independent t-tests). Nonetheless, the age ranges indicated that weight, height, and most of the pulmonary function parameters exhibited progressive and statistically significant increases with age. Regarding the FET, a significant increase was observed only among the children aged 4–6 years. Only the BEV, FVC, FEV0.5/FVC, and FEV1/FVC among all of the investigated age ranges failed to exhibit statistically significant differences according to Hochberg test.
Anthropometric data, success rates, and observed values of the spirometric variables according to age, among the 195 assessed children.
| Age (n) | Success rate (%) | Height (cm) | Weight (kg) | FVC (L) | FEV0.5 (L) | FEV0.5/FVC | FEV1 (L) | FEV1/FVC | PEF (L/min) | FEF25–75 (L/s) | FET (s) | BEV (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Boys | ||||||||||||
| 4 (30) | 76 | 107±5 (105–110) | 19±3 (17–20) | 1.15±0.20 (1.06–1.24) | 0.86±0.15 (0.80–0.94) | 0.76±0.08 (0.72–0.80) | 1.04±0.26 (0.92–1.16) | 0.90±0.18 (0.81–0.98) | 151±29 (139–166) | 1.59±0.39 (1.39–1.75) | 1.90±0.60 (1.62–2.18) | 3.39±1.08 (2.91–3.87) |
| 5 (31) | 81 | 115±6 (113–117) | 21±4 (19–22) | 1.33±0.21 (1.24–1.42) | 0.99±0.13 (0.94–1.04) | 0.75±0.08 (0.72–0.79) | 1.24±0.17 (1.16–1.31) | 0.93±0.05 (0.91–0.95) | 173±36 (157–188) | 1.74±0.32 (1.61–1.88) | 1.88±0.60 (1.62–2.13) | 3.22±1.29 (2.67–3.76) |
| 6 (31) | 90 | 118±5 (116–120) | 22±3 (20–23) | 1.42±0.23 (1.33–1.51) | 1.01±0.16 (0.95–1.08) | 0.72±0.06 (0.70–0.74) | 1.28±0.20 (1.21–1.36) | 0.91±0.04 (0.89–0.92) | 172±33 (159–185) | 1.69±0.36 (1.55–1.83) | 2.32±0.56 (2.10–2.54) | 3.24±1.03 (2.84–3.64) |
| Girls | ||||||||||||
| 4 (35) | 81 | 109±5 (107–111) | 19±4 (18–21) | 1.10±0.24 (1.01–1.20) | 0.81±0.16 (0.75–0.87) | 0.74±0.07 (0.71–0.76) | 1.01±0.21 (0.94–1.09) | 0.92±0.05 (0.91–0.94) | 135±32 (123–147) | 1.41±0.34 (1.28–1.54) | 2.09±0.66 (1.83–2.33) | 3.13±1.05 (2.73–3.54) |
| 5 (36) | 89 | 115±5 (113–117) | 20±3 (19–21) | 1.25±0.18 (1.18–1.31) | 0.93±0.13 (0.88–0.98) | 0.75±0.07 (0.73–0.78) | 1.16±0.15 (1.10–1.21) | 0.93±0.05 (0.91–0.95) | 166±34 (154–179) | 1.67±0.40 (1.53–1.82) | 1.89±0.69 (1.64–2.14) | 3.60±1.17 (3.17–4.03) |
| 6 (32) | 100 | 120±7 (117–122) | 24±6 (22–26) | 1.48±0.25 (1.39–1.57) | 1.08±0.19 (1.01–1.14) | 0.73±0.06 (0.71–0.75) | 1.35±0.22 (1.27–1.43) | 0.91±0.04 (0.90–0.93) | 185±36 (172–197) | 1.86±0.47 (1.69–2.03) | 2.26±0.70 (2.01–2.51) | 3.41±6.80 (3.12–3.70) |
| Total (195) | 85 | 114±7a,b,c (113–115) | 21±4b,c (20–22) | 1.30±0.26 (1.26–1.33) | 0.95±0.18a,b,c (0.93–0.98) | 0.74±0.07 (0.73–075) | 1.19±0.24a,b,c (1.15–1.22) | 0.92±0.08 (0.91–0.93) | 164±30a,c (159–170) | 1.66±0.41a,c (1.60–1.73) | 2.07±0.66b (1.97–2.17) | 3.34±1.07 (3.17–3.50) |
FVC, forced vital capacity; FEV0.5, forced expiratory volume in 0.5s; FEV0.5/FVC, ratio between FEV0.5 and FVC; FEV1, forced expiratory volume in one second; FEV1/FVC, ratio between FEV1 and FVC; PEF, peak expiratory flow; FEF25–75, forced expiratory flow at 25–75% of the FVC; FET, forced expiratory time; BEV, back-extrapolated volume.
The data are presented as the means±the standard deviations with the 95% confidence intervals (in parentheses).
To the best of the authors’ knowledge, the present report is the second study designed to describe prediction equations for spirometric variables exclusively for Brazilian 4- to 6-year-old preschoolers.
The first study was published by Burity et al.19; these authors enrolled 321 children aged from 3 to 6 years (mean age, 60 months). However, only 135 children (69 boys and 66 girls) were able to perform all of the forced expiratory maneuvers. In contrast to the present study, the statistical analyses included logarithmic and linear regressions and did not include the least mean squares method. The latter method allows for the construction of funnel-shaped curves that better reflect the correlations between physical lung growth across the analyzed ages (4, 5, and 6 years of life) and functional parameters.
The main results of the present study are the following: progressive and statistically significant increases in the majority of the spirometric parameters were observed with increasing height, and the resulting prediction equations incorporated height as a single predictor. These results agree with previously reported results.6,9,15 Thus, the prediction equations for spirometric variables described in the present study were generated by considering height as the single independent variable. This choice of a single predictor was based on the following factors: the statistically non-significant variation in the coefficients of determination with the addition of the other possible independent variables (i.e., age, weight, and sex), the ease of use of the equations with single predictors in clinical practice, and the previous use of height as a single independent variable by several authors to derive prediction equations for spirometric parameters among preschoolers.6,8,11,13,15 Additionally, the values for the coefficient of determination (r2) that were found in the present study (Table 1) are similar to those previously described,9,12,15 including those of a study that enrolled northeastern Brazilian preschoolers.19 Overall, the r2 values reported in the literature for FVC ranged from 0.76 to 0.53; for FEV0.5, from 0.73 to 0.42; for FEV1, from 0.78 to 0.55; for PEF, from 0.78 to 0.38; and for FEF25–75, from 0.37 to 0.17.9,12,15,19
The graphs of the spirometric variables according to height in which the z-scores were plotted reflect the direct correlations between the spirometric variables and the increase in height. Therefore, with a progressive increase in height, the variables that were assessed in the present study presented wide variability. The graphs from previous studies resembled those of the present study in appearance.16,17
In contrast to the study with northeastern Brazilian children,19 in which significant differences between boys and girls were found, the present study did not find significant differences in the spirometric variables between male and female children, and this lack of differences has also been observed in similar studies.6,15 Possible reasons for this result include the lack of hormonal and nutritional differences between preschool males and females and the small sample size.
Additionally, strong agreements (i.e., z-scores close to zero) were observed in the comparisons of the spirometric values generated from our prediction equations and the values that were recently reported by Quanjer and coworkers based on 97,759 records of healthy nonsmokers aged 2.5–95 years from around the world.18 For example, the mean z-scores for the FVC, FEV1, FEV1/FVC ratio, and FEF25–75 obtained in the present study were −0.8, −0.00, +0.1, and +0.05, respectively; i.e., all of the parameters fell within the accepted range of ±0.5 z-scores. In other words, these values were lower than approximately 1–2% of the predicted values reported by Quanjer et al.,18 which are clinically irrelevant. However, the prediction equations proposed in the present study appear to be more applicable to populations similar to that of the present study, simply because these equations were generated from such a population.
Compared to the reference values described by Rosenthal et al.4 and Burity et al.19 and accounting for the children with heights of 110cm, the present predicted values are close to those that have been previously reported, i.e., FVC of 1.20L, 1.10L, and 1.18L, respectively, FEV1 of 1.10L, 1.05L, and 1.10L, respectively, and FEV1/FVC of 0.90, 0.95, and 0.93, respectively.
One of the limitations of the present study was that it did not include 3-year-old children, although the preschool age range is considered to begin at that age. However, access to these children would have been restricted due to the small number of schools in Sete Lagoas, particularly public schools, for children younger than 4 years old. Another limitation is the relatively small sample size of this study.
In summary, prediction equations for spirometric variables were generated for 4- to 6-year-old Brazilian children residing in the state of Minas Gerais. These results may be of importance to the field of pediatric respiratory health because these values can be used to optimize the diagnosis and clinical management of children with suspected or confirmed respiratory diseases. Pulmonary function tests are important to elucidate diagnostic hypotheses and improve clinical management. Reflecting the importance of their use, these tests are increasingly being used among the preschool population. The results of the present study may help to broaden the use of spirometry among preschoolers, as these results corroborate the findings of previous studies that have reported high success rates in the performance of spirometric maneuvers by preschoolers and an increase in the success rate with age.3,6,7,9,10,15,22
Given the continental characteristics of Brazil, further studies on this topic across the five macroregions of the country should be encouraged, and these studies should aim to obtain lung function data from a more representative population of Brazilian children.
FundingPró-Reitoria de Pesquisa da Universidade Federal de Minas Gerais, Brazil; Brazilian Research Agencies, Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq, Grant No. 309494/2013-3 [to VFP] and 303396/2012-1 [to PAMC]), and Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG, Grant No. PPM-00065-14 [to PAMC] and PPM-00287-15 [to VFP]).
Conflicts of interestThe authors declare no conflicts of interest.
The authors wish to thank Maria Ângela Gonçalves de Oliveira Ribeiro and Eliane Viana Mancuzo for reviewing a preliminary version of the manuscript and for their invaluable input.
Please cite this article as: França DC, Camargos PA, Jones MH, Martins JA, Vieira BP, Colosimo EA, et al. Prediction equations for spirometry in four- to six-year-old children. J Pediatr (Rio J). 2016;92:400–8.