this study aimed to simplify the diagnostic criteria of pre-hypertension (pre-HTN) and hypertension (HTN) in the pediatric age group, and to determine the accuracy of these simple indexes in a nationally-representative sample of Iranian children and adolescents.
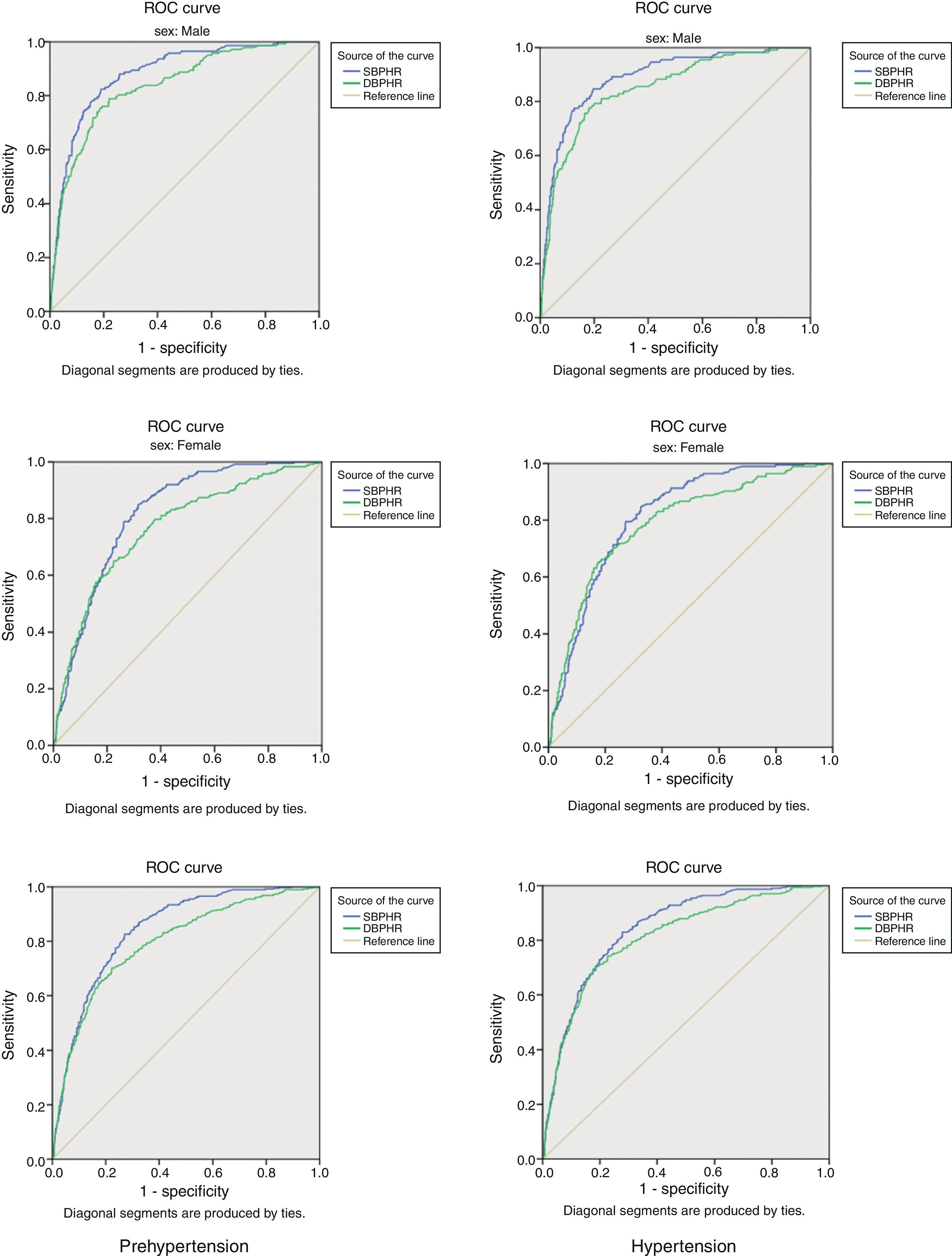
Methodthe diagnostic accuracy of the indexes of systolic blood pressure-to-height ratio (SBPHR) and diastolic BPHR (DBPHR) to define pre-HTN and HTN was determined by the area under the curve of the receiver operator characteristic curves.
Resultsthe study population consisted of 5,738 Iranian students (2,875 females) with mean (SD) age of 14.7 (2.4) years. The prevalences of pre-HTN and HTN were 6.9% and 5.6%. The optimal thresholds for defining pre-HTN were 0.73 in males and 0.71 in females for SBPHR, and 0.47 in males and 0.45 in females for DBPHR, respectively. The corresponding figures for HTN were 0.73, 0.71, 0.48, and 0.46, respectively. In both genders, the accuracies of SBPHR and DBPHR in diagnosing pre-HTN and HTN were approximately 80%.
ConclusionsBPHR is a valid, simple, inexpensive, and accurate tool to diagnose pre-HTN and HTN in adolescents. The optimal thresholds of SBPHR and DBPHR were consistent with the corresponding figures in other populations of children and adolescents with different racial and ethnic backgrounds. Thus, it is suggested that the use of these indexes can be generalized in programs aiming to screen elevated blood pressure in the pediatric age group.
este estudo visa simplificar os critérios de diagnóstico da pré-hipertensão (pré-HTA) e hipertensão (HTA) na faixa etária pediátrica e determinar a precisão desses índices simples em uma amostra nacionalmente representativa de crianças e adolescentes iranianos.
Métodoa precisão diagnóstica dos índices de relação pressão arterial sistólica/altura (RPASA) e RPAA diastólica (RPADA) para definir a pré-HTA e HTA foi determinada pela área sob as curvas de características de operação do receptor.
Resultadosa população estudada contou com 5738 alunos iranianos (2875 meninas) com idade média (DP) de 14,7 (2,4) anos. A prevalência de pré-HTA e HTA foi 6,9% e 5,6%. Os limites ideais para a definição de pré-HTA foram 0,73 em meninos e 0,71 em meninas com relação à RPASA e 0,47 em meninos e 0,45 em meninas com relação à RPADA, respectivamente. Os valores correspondentes com relação à HTA foram 0,73, 0,71, 0,48 e 0,46, respectivamente. Em ambos os gêneros, a precisão de RPASA e RPADA no diagnóstico de pré-HTA e HTA foi de aproximadamente 80%.
Conclusõesa RPAA é uma ferramenta válida, simples, barata e precisa no diagnóstico da pré-HTA e HTA em adolescentes. Os limites ideais de RPASA e RPADA foram compatíveis com os números correspondentes em outra população de crianças e adolescentes com diferentes históricos raciais e étnicos, assim, sugerimos que a utilização desses índices possa ser generalizada em programas de triagem com relação à PA elevada na faixa etária pediátrica.
Hypertension (HTN) is a global health problem, and it is well-documented that increased blood pressure (BP) becomes established in childhood.1,2 Nowadays, health care providers focus on the screening and treatment of hypertension in adults; however, they should also consider the importance of the BP tracking from early life and the increasing prevalence of pre-hypertension (pre-HTN) and HTN in the pediatric age group.3,4 A growing body of evidence indicates not only that HTN gradually damages the function of vital organs, but also that pre-HTN has the same harmful effects.5,6
The fourth report on the diagnosis, evaluation, and treatment of high BP in children and adolescents emphasized that all children older than 3 years attended to in a medical setting should have their BP measured.7 Since pre-HTN and HTN in children are classified as systolic BP (SBP) and/or diastolic BP (DBP) between 90th and 95th percentile, and ≥ 95th percentile, respectively, and considering that the accurate diagnosis of high BP requires adjusting the values for age, gender, and height, the interpretation of the BP level is time-consuming and difficult to use. This is a probably reason why, in many countries, BP measurement is not an integrated part of physical examination for healthy children. Providing simple indexes for interpreting the BP levels would increase the knowledge regarding the BP status of children and adolescents, and would help to identify those who need further follow-up for definitive diagnosis of HTN. In some populations, simplified indexes, such as SBP-to-height ratio (SBPHR) and DBP-to-height ratios (DBPHR), have been used for easy interpretation of BP levels in the pediatric age group.8,9 These studies have recommended determining the sensitivity and specificity of these indexes in various populations. Education regarding the prevalence of elevated BP in the pediatric population would be useful for policy makers, in order to highlight the importance of training health professionals about integrating BP measurement and tracking in healthy children, and to increase the public awareness about the importance of prevention and control of pre-HTN from early life.
This study aimed to simplify the diagnostic criteria of pre-HTN and HTN in children and adolescents, and to determine the accuracy of these simple indexes in a nationally-representative sample of Iranian children and adolescents, as the first national study of its kind in the pediatric population of the Middle East and North Africa (MENA).
MethodsStudy populationThe data used in this study were collected as a part of the national survey of school students’ high risk behaviors (2009-2010) as the third survey of the school-based surveillance system entitled the Childhood and Adolescence Surveillance and PreventIon of Adult Non-communicable disease (CASPIAN) Study.10,11 The third survey of this nationwide school-based health survey (CASPIAN-III Study) was conducted in 27 provinces of Iran. Details of data collection and the sampling framework have been explained elsewhere,12 and are presented here in brief.
Study participantsThe study was approved by institutional review boards at the national and provincial level. The Research and Ethical Committee of the Bureau of Population, Family, and School Health, Ministry of Health and Medical Education, and the Research and Ethical Committee of the Ministry of Education and Training approved the study. After complete explanation of the objectives and protocols of the study, informed consents were obtained from parents and oral assent from students. The present survey included 5,680 students aged 10-18 years, who were recruited by multistage random cluster sampling from the urban and rural areas of 27 provinces of Iran.
Procedure and measurementsA team of trained health care professionals and physicians recorded information, and conducted the physical examination under standard protocols by using calibrated instruments. Body mass index (BMI) was calculated as weight (kg) divided by height squared (m2).
SBP and DBP were measured on the right arm, with the individual in a sitting position and at rest for at least 5min, using standardized mercury sphygmomanometers and appropriate size cuff. Two measurements at two-minute intervals were recorded, and the average was used for the statistical analysis.7 The indexes were computed by using the following equations: SBPHR = SBP (mmHg) / height (cm) and DBPHR = DBP (mmHg) / height (cm).
Statistical analysisQuantitative variables were expressed as means (standard deviations), and categorical data as number (percentage). To determine the optimal threshold for predicting elevated BP, the receiver operator characteristic (ROC) curve analysis was plotted with an estimation of the variable's sensitivity and specificity. Optimal thresholds for SBPHR and DBPHR were assessed by the minimum value of 1−sensitivity2+1−specificity2,13 which represented the maximum sum of sensitivity and specificity.
The area under curve (AUC) corresponded to the overall ability of SBPHR and DBPHR as a diagnostic test for predicting elevated BP. The AUC value ranges between 0 to 1; it can be interpreted according to the following principles: test equal to chance (AUC = 0.5), less accurate (0.5 < AUC ≤ 0.7), moderately accurate (0.7 < AUC ≤ 0.9), highly accurate (0.9 < AUC ≤ 1.0), and perfect performance (AUC = 1.0). Data were analyzed by using the Statistical Package for Social Sciences (SPSS) version 16.0 (SPSS Inc. - Chicago, IL, USA); p-values of less than 0.05 were considered statistically significant.
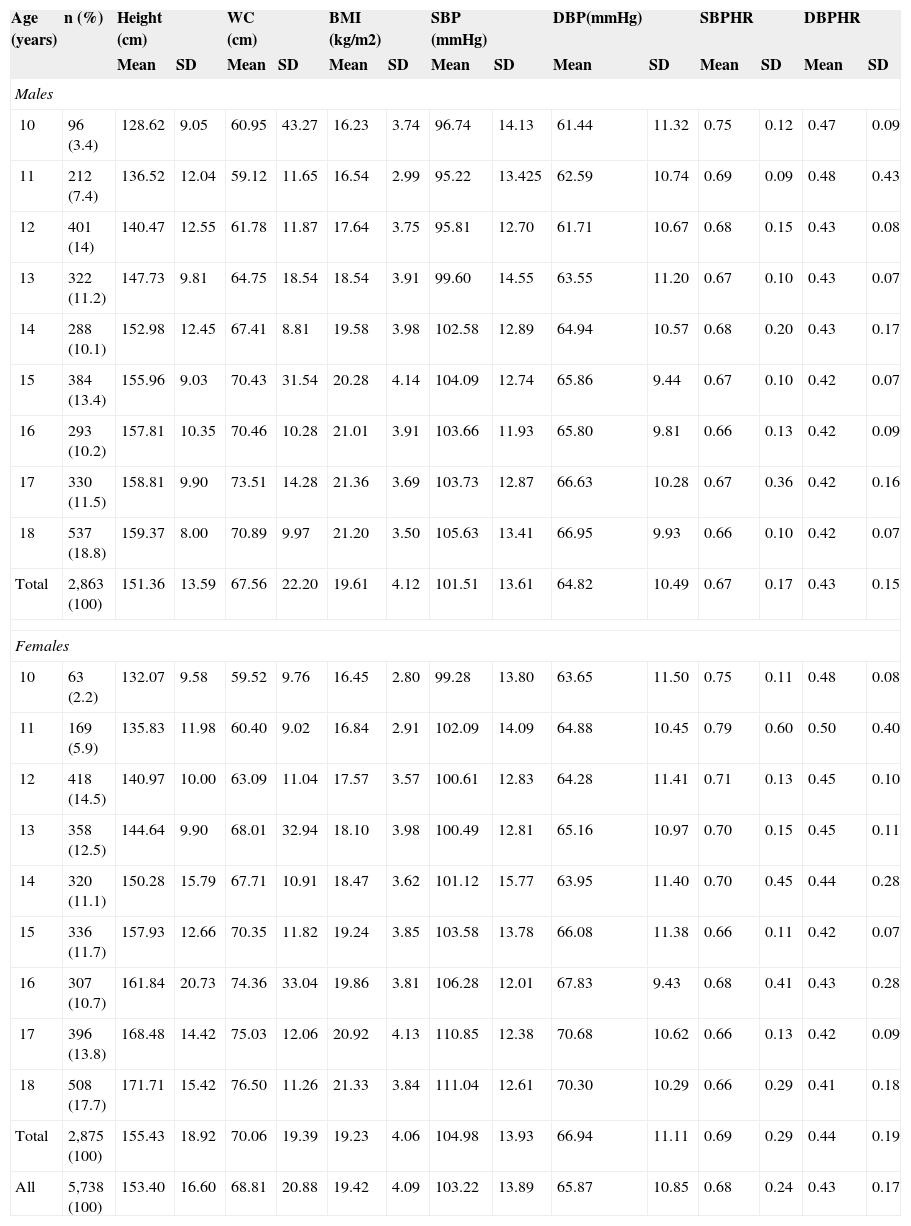
ResultsComplete data of 5,738 students were obtained for the current study, and are reported here. Participants consisted of 2,863 males and 2,875 females, with mean (SD) age of 14.7 (2.4) years. Table 1 presents the characteristics of the study participants. The mean (SD) of SBP and DBP were 103.22 (13.89) and 65.87 (10.85) mmHg, respectively. The prevalence of pre-HTN and HTN were 6.9% and 5.6%, respectively. The means (SD) for SBPHR and DBPHR were 0.68 (0.24) and 0.43 (0.17), respectively.
Characteristics of the study population by age and gender: the CASPIAN-III Study.
| Age (years) | n (%) | Height (cm) | WC (cm) | BMI (kg/m2) | SBP (mmHg) | DBP(mmHg) | SBPHR | DBPHR | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| Males | |||||||||||||||
| 10 | 96 (3.4) | 128.62 | 9.05 | 60.95 | 43.27 | 16.23 | 3.74 | 96.74 | 14.13 | 61.44 | 11.32 | 0.75 | 0.12 | 0.47 | 0.09 |
| 11 | 212 (7.4) | 136.52 | 12.04 | 59.12 | 11.65 | 16.54 | 2.99 | 95.22 | 13.425 | 62.59 | 10.74 | 0.69 | 0.09 | 0.48 | 0.43 |
| 12 | 401 (14) | 140.47 | 12.55 | 61.78 | 11.87 | 17.64 | 3.75 | 95.81 | 12.70 | 61.71 | 10.67 | 0.68 | 0.15 | 0.43 | 0.08 |
| 13 | 322 (11.2) | 147.73 | 9.81 | 64.75 | 18.54 | 18.54 | 3.91 | 99.60 | 14.55 | 63.55 | 11.20 | 0.67 | 0.10 | 0.43 | 0.07 |
| 14 | 288 (10.1) | 152.98 | 12.45 | 67.41 | 8.81 | 19.58 | 3.98 | 102.58 | 12.89 | 64.94 | 10.57 | 0.68 | 0.20 | 0.43 | 0.17 |
| 15 | 384 (13.4) | 155.96 | 9.03 | 70.43 | 31.54 | 20.28 | 4.14 | 104.09 | 12.74 | 65.86 | 9.44 | 0.67 | 0.10 | 0.42 | 0.07 |
| 16 | 293 (10.2) | 157.81 | 10.35 | 70.46 | 10.28 | 21.01 | 3.91 | 103.66 | 11.93 | 65.80 | 9.81 | 0.66 | 0.13 | 0.42 | 0.09 |
| 17 | 330 (11.5) | 158.81 | 9.90 | 73.51 | 14.28 | 21.36 | 3.69 | 103.73 | 12.87 | 66.63 | 10.28 | 0.67 | 0.36 | 0.42 | 0.16 |
| 18 | 537 (18.8) | 159.37 | 8.00 | 70.89 | 9.97 | 21.20 | 3.50 | 105.63 | 13.41 | 66.95 | 9.93 | 0.66 | 0.10 | 0.42 | 0.07 |
| Total | 2,863 (100) | 151.36 | 13.59 | 67.56 | 22.20 | 19.61 | 4.12 | 101.51 | 13.61 | 64.82 | 10.49 | 0.67 | 0.17 | 0.43 | 0.15 |
| Females | |||||||||||||||
| 10 | 63 (2.2) | 132.07 | 9.58 | 59.52 | 9.76 | 16.45 | 2.80 | 99.28 | 13.80 | 63.65 | 11.50 | 0.75 | 0.11 | 0.48 | 0.08 |
| 11 | 169 (5.9) | 135.83 | 11.98 | 60.40 | 9.02 | 16.84 | 2.91 | 102.09 | 14.09 | 64.88 | 10.45 | 0.79 | 0.60 | 0.50 | 0.40 |
| 12 | 418 (14.5) | 140.97 | 10.00 | 63.09 | 11.04 | 17.57 | 3.57 | 100.61 | 12.83 | 64.28 | 11.41 | 0.71 | 0.13 | 0.45 | 0.10 |
| 13 | 358 (12.5) | 144.64 | 9.90 | 68.01 | 32.94 | 18.10 | 3.98 | 100.49 | 12.81 | 65.16 | 10.97 | 0.70 | 0.15 | 0.45 | 0.11 |
| 14 | 320 (11.1) | 150.28 | 15.79 | 67.71 | 10.91 | 18.47 | 3.62 | 101.12 | 15.77 | 63.95 | 11.40 | 0.70 | 0.45 | 0.44 | 0.28 |
| 15 | 336 (11.7) | 157.93 | 12.66 | 70.35 | 11.82 | 19.24 | 3.85 | 103.58 | 13.78 | 66.08 | 11.38 | 0.66 | 0.11 | 0.42 | 0.07 |
| 16 | 307 (10.7) | 161.84 | 20.73 | 74.36 | 33.04 | 19.86 | 3.81 | 106.28 | 12.01 | 67.83 | 9.43 | 0.68 | 0.41 | 0.43 | 0.28 |
| 17 | 396 (13.8) | 168.48 | 14.42 | 75.03 | 12.06 | 20.92 | 4.13 | 110.85 | 12.38 | 70.68 | 10.62 | 0.66 | 0.13 | 0.42 | 0.09 |
| 18 | 508 (17.7) | 171.71 | 15.42 | 76.50 | 11.26 | 21.33 | 3.84 | 111.04 | 12.61 | 70.30 | 10.29 | 0.66 | 0.29 | 0.41 | 0.18 |
| Total | 2,875 (100) | 155.43 | 18.92 | 70.06 | 19.39 | 19.23 | 4.06 | 104.98 | 13.93 | 66.94 | 11.11 | 0.69 | 0.29 | 0.44 | 0.19 |
| All | 5,738 (100) | 153.40 | 16.60 | 68.81 | 20.88 | 19.42 | 4.09 | 103.22 | 13.89 | 65.87 | 10.85 | 0.68 | 0.24 | 0.43 | 0.17 |
BMI, body mass index; DBP, diastolic blood pressure; DBPHR, diastolic blood pressure-to-height ratio; SBP, systolic blood pressure; SBPHR, systolic blood pressure-to-height ratio; SD, standard deviation; WC, waist circumference.
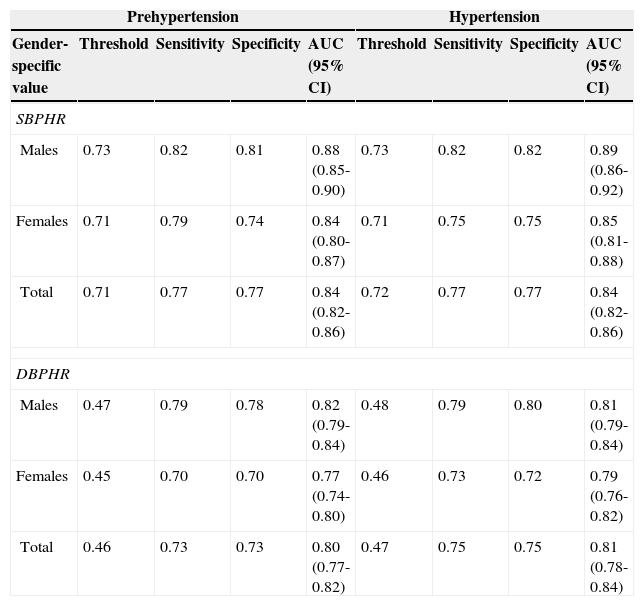
The sensitivity, specificity, and threshold of BPHR for identifying individuals with pre-HTN and HTN are presented in Table 2. The optimal thresholds for defining pre-HTN were 0.73 in males and 0.71 in females for SBPHR, and 0.47 in males and 0.45 in females for DBPHR, respectively. The corresponding figures for HTN were 0.73, 0.71, 0.48, and 0.46, respectively. The related ROC curves for identifying pre-HTN and HTN by BPHR are depicted in Fig. 1, which demonstrates that for both females and males, the AUC values of SBPHR are greater than those of DBPHR in diagnosing pre-HTN and HTN. The AUC values for the accuracy of SBPHR and DBPHR in diagnosing pre-HTN were 0.84 and 0.80, respectively, and the accuracy of SBPHR and DBPHR in diagnosing HTN was 0.84 and 0.81, respectively, which indicates suitable accuracy.
Receiver operator characteristic curve of blood pressure-to-height ratios for identifying children with pre-hypertension and hypertension: the CASPIAN-III Study.
| Prehypertension | Hypertension | |||||||
|---|---|---|---|---|---|---|---|---|
| Gender-specific value | Threshold | Sensitivity | Specificity | AUC (95% CI) | Threshold | Sensitivity | Specificity | AUC (95% CI) |
| SBPHR | ||||||||
| Males | 0.73 | 0.82 | 0.81 | 0.88 (0.85-0.90) | 0.73 | 0.82 | 0.82 | 0.89 (0.86-0.92) |
| Females | 0.71 | 0.79 | 0.74 | 0.84 (0.80-0.87) | 0.71 | 0.75 | 0.75 | 0.85 (0.81-0.88) |
| Total | 0.71 | 0.77 | 0.77 | 0.84 (0.82-0.86) | 0.72 | 0.77 | 0.77 | 0.84 (0.82-0.86) |
| DBPHR | ||||||||
| Males | 0.47 | 0.79 | 0.78 | 0.82 (0.79-0.84) | 0.48 | 0.79 | 0.80 | 0.81 (0.79-0.84) |
| Females | 0.45 | 0.70 | 0.70 | 0.77 (0.74-0.80) | 0.46 | 0.73 | 0.72 | 0.79 (0.76-0.82) |
| Total | 0.46 | 0.73 | 0.73 | 0.80 (0.77-0.82) | 0.47 | 0.75 | 0.75 | 0.81 (0.78-0.84) |
AUC, area under curve; CI, confidence interval; DBPHR, diastolic blood pressure-to-height ratio; SBPHR, systolic blood pressure-to-height ratio.
This large population-based study provided a simplified diagnostic tool for primary assessment of BP, and for detecting children and adolescents in need of further follow-up for identifying pre-HTN and HTN. In the present study, the optimal thresholds for SBPHR and DBPHR for diagnosing systolic/diastolic pre-HTN were 0.73 and 0.47 in males, and 0.71 and 0.45 in females, respectively. These findings are consistent with the some previous studies conducted in children and adolescents, which provided optimal thresholds of BPHR for diagnosing elevated BP, but also suggested the development of these indexes in various populations.8,9,14,15
In a study among 3,136 Han adolescents aged between 13 and 17 years, the optimal thresholds of SBPHR and DBPHR for defining pre-HTN were 0.75 and 0.48 for males, and 0.78 and 0.51 for females, respectively. The corresponding figures for defining HTN were 0.81 and 0.57 for males, and 0.84 and 0.63 for females, respectively.8 In a population-based study with 1,173 Nigerian adolescents aged 11 to 17 years, the optimal thresholds of SBPHR and DBPHR for diagnosing pre-HTN were 0.72 and 0.46 in males, and 0.73 and 0.48 in females; the corresponding figures for HTN were 0.75 and 0.51 in males and 0.77 and 0.50 in females.9 In a population-based study of 1,352 Han children aged 7 to 12 years, DBPHR cutoff values for elevated DBP were 0.51 and 0.60mmHg/cm in males, and 0.51 and 0.58mmHg/cm in females. SBPHR cutoff values for elevated SBP were 0.76 and 0.88 in males, and 0.78 and 0.90 in females.14 The National Health and Nutrition Examination Survey (NHANES) in 2006-2007 included the data of 3,775 American children and adolescents, and confirmed the high sensitivity and specificity of BPHR in detecting elevated BP in this age group. The cutoffs for SBPHR and DBPHR were ≥ 0.75 and ≥ 0.46 in males, and ≥ 0.75 and ≥ 0.48 in females, respectively.15 In all these studies,8,9,14,15 as well as in the current study, the cutoff points obtained are in a similar range, and BPHRs had high accuracy in identifying elevated BP in the pediatric age group. The similarity of the indexes obtained in the present and in previous studies, as well as the appropriate sensitivity and specificity of these indexes in all these studies, indicates that simple indexes of BPHR can be used in various populations of children and adolescents.
Currently, a large number of children and adolescents with pre-HTN and HTN remain undiagnosed. This problem is not restricted to low- and middle-income countries with limited health care facilities; even physicians with access to electronic files and computer programs in industrialized countries still have difficulties with integrating BP monitoring of children and adolescents into their routine clinical practice.16 Providing simple indexes for BPHR would help the implementation of scientific guidelines for routine measurement and tracking of BP from childhood.
By considering the strong effects of overweight, and environmental factors such as air pollution, noise pollution, and passive smoking on elevated BP,17–19 it is suggested that the prevalence of pre-HTN and HTN will continue to increase in the pediatric age group. Moreover, elevated BP has various adverse effects even in children and adolescents.20 Thus, using simplified diagnostic tools for SBPHR and DBPHR would help to screen and identify children and adolescents who need further assessment for elevated BP.
It should be acknowledged that obtaining BPHR indexes requires the measurement of both BP and height, and also requires the calculation of their ratio; thus, they are subject to measurement error. BPHR indexes cannot be considered as substitutes of the age- and gender-specific BP percentiles in the diagnosis of elevated BP, but they can be easily used as screening tools.
The optimal thresholds of SBPHR and DBPHR for defining elevated BP were consistent with the corresponding figures in other populations of children and adolescents with different racial and ethnic backgrounds,8,9,14,15 thus it is suggested that the use of these simple, inexpensive, and accurate indexes should be standardized into screening programs for elevated BP in the pediatric age group.
FundingThis study was conducted as part of a national school-based survey.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Kelishadi R, Heshmat R, Ardalan G, Qorbani M, Taslimi M, Poursafa P, et al. First report on simplified diagnostic criteria for pre-hypertension and hypertension in a national sample of adolescents from the Middle East and North Africa: the CASPIAN-III study. J Pediatr (Rio J). 2014;90:85–91.