To describe the characteristics of children and adolescentes with chronic diseases of outpatient clinics at a tertiary university hospital.
MethodsA cross-sectional study was performed with 16,237 patients with chronic diseases followed-up in one year. The data were collected through the electronic system, according to the number of physician appointments in 23 pediatric specialties. Patients were divided in two groups: children (0–9 years) and adolescents (10–19 years). Early (10–14 years) and late (15–19 years) adolescent groups were also analyzed.
ResultsOf the total sample, 56% were children and 46% were adolescents. The frequencies of following pediatric specialties were significantly higher in adolescents when compared with children: cardiology, endocrinology, hematology, nephrology/renal transplantation, neurology, nutrology, oncology, palliative and pain care, psychiatry, and rheumatology (p<0.05). The frequencies of emergency service visits (30% vs. 17%, p<0.001), hospitalizations (23% vs. 11%, p<0.001), intensive care unit admissions (6% vs. 2%, p<0.001), and deaths (1% vs. 0.6%, p=0.002) were significantly lower in adolescents than in children. However, the number of physician appointments (≥13) per patient was also higher in the adolescent group (5% vs. 6%, p=0.018). Further analysis comparison between early and late adolescents revealed that the first group had significantly more physician appointments (35% vs. 32%, p=0.025), and required more than two pediatric specialties (22% vs. 21%, p=0.047). Likewise, the frequencies of emergency service visits (19% vs. 14%, p<0.001) and hospitalizations (12% vs. 10%, p=0.035) were higher in early adolescents.
ConclusionsThis study evaluated a large population in a Latin American hospital and suggested that early adolescents with chronic diseases required many appointments, multiple specialties and hospital admissions.
Descrever características de crianças e adolescentes com doenças crônicas de clínicas ambulatoriais em um hospital universitário terciário.
MétodosUm estudo transversal foi realizado com 16.237 pacientes com doenças crônicas acompanhados em um ano. Os dados foram coletados por meio de dados do sistema eletrônico de acordo com o número de consultas médicas em 23 especialidades pediátricas. Os pacientes foram divididos em dois grupos: crianças (0-9 anos) e adolescentes (10-19 anos). Também foram analisados grupos de jovens adolescentes (10-14 anos) e adolescentes mais velhos (15-19 anos).
Resultados54% eram crianças e 46% eram adolescentes. As frequências das seguintes especialidades pediátricas foram significativamente maiores em adolescentes em comparação a crianças: cardiologia, endocrinologia, hematologia, nefrologia/transplante renal, neurologia, nutrologia, oncologia, cuidados paliativos e cuidado da dor, psiquiatria e reumatologia (p<0,05). As frequências de visitas a serviços de emergência (30%, em comparação a 17%, p<0,001), internações (23%, em comparação a 11%, p<0,001), internações em unidade de terapia intensiva (6%, em comparação a 2%, p<0,001) e óbitos (1%, em comparação a 0,6%, p=0,002) foram significativamente menores em adolescentes do que em crianças. Contudo, o número de consultas médicas (≥ 13) por paciente (também) foi maior em grupos de adolescentes (5%, em comparação a 6%, p=0,018). A comparação de análises adicionais entre jovens adolescentes e adolescentes mais velhos revelou que o primeiro grupo apresentou um número significativamente maior de consultas médicas (35%, em comparação a 32%, p=0,025) e precisou de mais de duas especialidades pediátricas (22%, em comparação a 21%, p=0,047). Da mesma forma, as frequências de visitas a serviços de emergência (19%, em comparação a 14%, p<0,001) e internações (12%, em comparação a 10%, p=0,035) foram maiores em jovens adolescentes.
ConclusõesEste estudo avaliou uma grande população em um hospital da América Latina e sugeriu que jovens adolescentes com doenças crônicas precisaram de muitas consultas, diversas especialidades e internações hospitalares.
The prevalence of pediatric chronic diseases has been rising in the last years. Indeed, disability-adjusted life-years are increasing for cardiovascular, onco-hematology, infectious, endocrine, chronic respiratory, renal, and musculoskeletal diseases.1–3
Children with chronic diseases have survived to adolescence, posing many new challenges to health policies.4 These patients require long-term medical follow-up in tertiary services due the high morbidity and mortality associated with certain diseases.5,6
In addition, children and adolescents with chronic diseases need multiple specialized pediatric appointments and a variety of hospital infrastructure, such as specialties ward, day hospital clinic, intensive care unit, and emergency department.5–8 There is a scarcity of studies evaluating pediatric chronic diseases in tertiary health centers,5–7 particularly assessing outpatient clinics in Latin America.
Therefore, the objective of the present study was to describe demographic data, physician appointments, pediatric specialties, hospital units’ attendance (day hospital, emergency, ward hospitalizations, and intensive care), and mortality in a large population of children and adolescentes with pediatric chronic diseases attended to at the outpatient clinics at one university hospital. Furthermore, comparisons between demographic data and characteristics of children and adolescents with pediatric chronic diseases attended to at outpatient clinics were performed, as well as comparisons between early and late adolescents.
MethodsFrom January to December 2015, a cross-sectional study was performed in patients with chronic diseases attended to at theoutpatient clinics of the Children's Hospital of Hospital das Clínicas da Faculdade de Medicina, Universidade de São Paulo (HC-FMUSP). Children or adolescents attended only at the emergency department, intensive care unit, and other hospitalizations were excluded. The study was approved by the Ethics Committee of HC-FMUSP.
Chronic diseases were classified according duration (over three months). The diagnosis of pediatric chronic illnesses was established according to physician scientific knowledge, validated methods, or tools based on professional standards or diagnostic classification criteria.4,9 The following 23 pediatric specialties were systematically evaluated according to electronic system data: allergy and immunology, cardiology, endocrinology, gastroenterology, genetics, hematology, hematopoietic cell transplantation, hepatology, (immunology), infectology, nephrology/renal transplantation, neurology, nutrology, oncology, orthopedics, palliative and pain care, pediatric surgery/liver transplantation, pneumology, psychiatry, rheumatology, and others (adolescent care, prematurity care, and teaching pediatrics clinic).
Data were collected through the electronic system of this tertiary university hospital, according to the number of physician appointments. This study assessed: demographic data (current age, gender, and place of residence), follow-up characteristics (duration, number of physician appointments per patient, number of specialties per patient), types of pediatric specialties in the service, number of day hospital clinic visits, and number of acute complications (number of emergency department visits, number of hospitalizations, number of intensive care unit admissions, and deaths).
Patients with chronic diseases were divided into two groups according to their current age: children (0–9 years) and adolescents (10–19 years), in accordance with the World Health Organization (WHO) criteria. Adolescents were further divided into early (10–14 years) and late (15–19 years) adolescence groups.
Statistical analysisThe results for continuous variables were presented as median (range) or mean±standard deviation. The results for categorical variables were presented as frequency and percentage. The comparisons between median (range) were performed by Mann–Whitney test, and between mean±standard deviation by Student's t-test. For categorical variables, the differences were calculated using Fisher's exact test. p-values <0.05 were considered statistically significant.
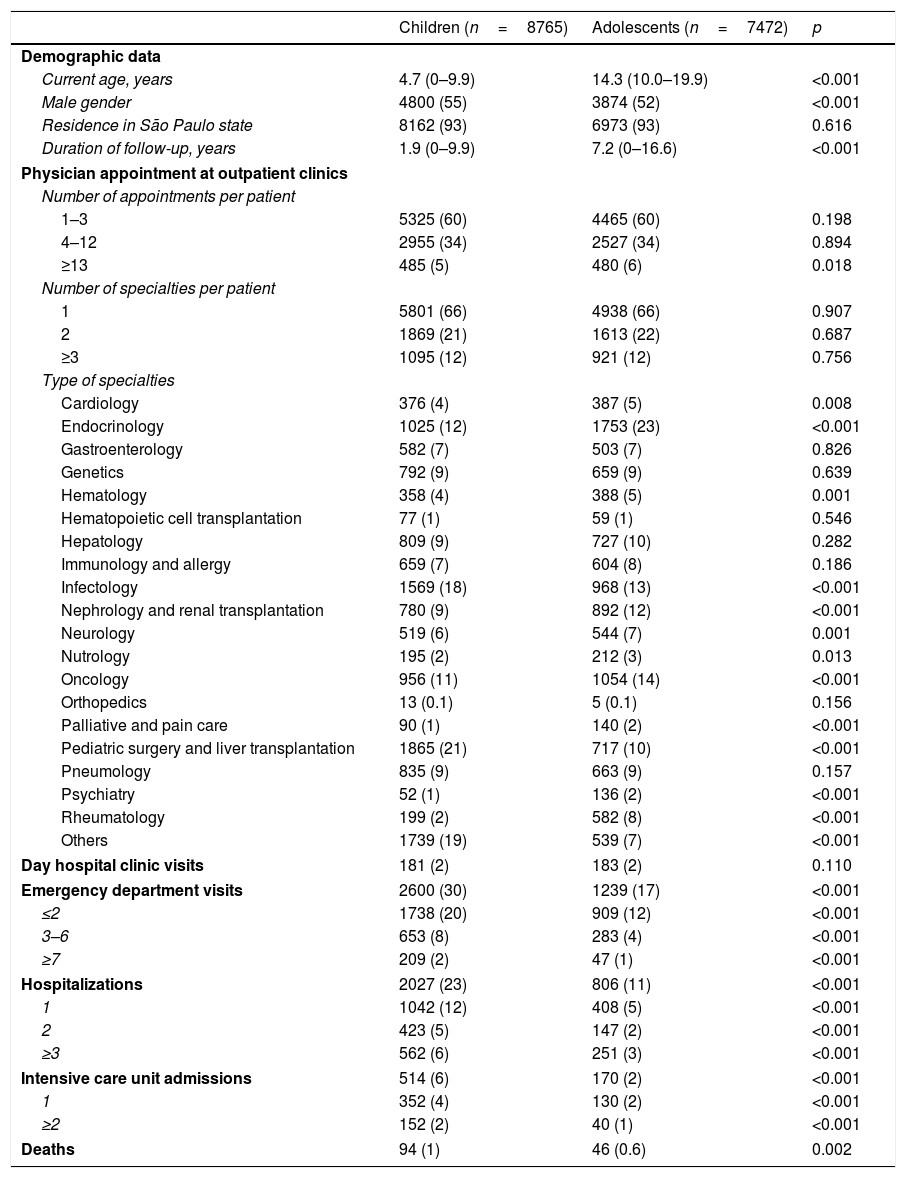
ResultsFrom January to December 2015, 16,237 children and adolescents with chronic diseases were attended to at the 23 pediatric specialties of this Children's Hospital. In this period, there were 84,671 physician appointments, 7664 hospitalizations, and 9735 emergency division visits. Of the total sample, 54% were children and 46% were adolescents. Table 1 presents the demographic data and characteristics of children and adolescentes with pediatric chronic diseases attended to at the outpatient clinics at this university hospital, which is a reference center for complex and severe diseases. The median follow-up duration (1.9 [0–9.9] vs. 7.2 [0–16.6] years, p<0.001) was significantly lower in children compared to adolescents. The frequency of male gender was higher in the former group (55% vs. 52%, p<0.001). The number of appointments per patient ≥13 was higher in adolescent group (5% vs. 6%, p=0.018; Table 1).
Demographic data and characteristics of children and adolescents with chronic pediatric diseases attended to at the outpatient clinics of a university hospital.
| Children (n=8765) | Adolescents (n=7472) | p | |
|---|---|---|---|
| Demographic data | |||
| Current age, years | 4.7 (0–9.9) | 14.3 (10.0–19.9) | <0.001 |
| Male gender | 4800 (55) | 3874 (52) | <0.001 |
| Residence in São Paulo state | 8162 (93) | 6973 (93) | 0.616 |
| Duration of follow-up, years | 1.9 (0–9.9) | 7.2 (0–16.6) | <0.001 |
| Physician appointment at outpatient clinics | |||
| Number of appointments per patient | |||
| 1–3 | 5325 (60) | 4465 (60) | 0.198 |
| 4–12 | 2955 (34) | 2527 (34) | 0.894 |
| ≥13 | 485 (5) | 480 (6) | 0.018 |
| Number of specialties per patient | |||
| 1 | 5801 (66) | 4938 (66) | 0.907 |
| 2 | 1869 (21) | 1613 (22) | 0.687 |
| ≥3 | 1095 (12) | 921 (12) | 0.756 |
| Type of specialties | |||
| Cardiology | 376 (4) | 387 (5) | 0.008 |
| Endocrinology | 1025 (12) | 1753 (23) | <0.001 |
| Gastroenterology | 582 (7) | 503 (7) | 0.826 |
| Genetics | 792 (9) | 659 (9) | 0.639 |
| Hematology | 358 (4) | 388 (5) | 0.001 |
| Hematopoietic cell transplantation | 77 (1) | 59 (1) | 0.546 |
| Hepatology | 809 (9) | 727 (10) | 0.282 |
| Immunology and allergy | 659 (7) | 604 (8) | 0.186 |
| Infectology | 1569 (18) | 968 (13) | <0.001 |
| Nephrology and renal transplantation | 780 (9) | 892 (12) | <0.001 |
| Neurology | 519 (6) | 544 (7) | 0.001 |
| Nutrology | 195 (2) | 212 (3) | 0.013 |
| Oncology | 956 (11) | 1054 (14) | <0.001 |
| Orthopedics | 13 (0.1) | 5 (0.1) | 0.156 |
| Palliative and pain care | 90 (1) | 140 (2) | <0.001 |
| Pediatric surgery and liver transplantation | 1865 (21) | 717 (10) | <0.001 |
| Pneumology | 835 (9) | 663 (9) | 0.157 |
| Psychiatry | 52 (1) | 136 (2) | <0.001 |
| Rheumatology | 199 (2) | 582 (8) | <0.001 |
| Others | 1739 (19) | 539 (7) | <0.001 |
| Day hospital clinic visits | 181 (2) | 183 (2) | 0.110 |
| Emergency department visits | 2600 (30) | 1239 (17) | <0.001 |
| ≤2 | 1738 (20) | 909 (12) | <0.001 |
| 3–6 | 653 (8) | 283 (4) | <0.001 |
| ≥7 | 209 (2) | 47 (1) | <0.001 |
| Hospitalizations | 2027 (23) | 806 (11) | <0.001 |
| 1 | 1042 (12) | 408 (5) | <0.001 |
| 2 | 423 (5) | 147 (2) | <0.001 |
| ≥3 | 562 (6) | 251 (3) | <0.001 |
| Intensive care unit admissions | 514 (6) | 170 (2) | <0.001 |
| 1 | 352 (4) | 130 (2) | <0.001 |
| ≥2 | 152 (2) | 40 (1) | <0.001 |
| Deaths | 94 (1) | 46 (0.6) | 0.002 |
Results are presented in n (%), median (range).
The pediatric specialties required were significantly higher in the adolescent group when compared with the children group: cardiology (4% vs. 5%, p=0.008), endocrinology (12% vs. 23%, p<0.001), hematology (4% vs. 5%, p=0.001), nephrology/renal transplantation (9% vs. 12%, p<0.001), neurology (6% vs. 7%, p=0.001), nutrology (2% vs. 3%, p=0.013), oncology (11% vs. 14%, p<0.001), palliative and pain care (1% vs. 2%, p<0.001), psychiatry (1% vs. 2%, p<0.001), and rheumatology (2% vs. 8%, p<0.001). In contrast, the frequency of emergency department visits (30% vs. 17%, p<0.001), hospitalizations (23% vs. 11%, p<0.001), intensive care unit admissions (6 vs. 2%, p<0.001), and deaths (1% vs. 0.6%, p=0.002) were significantly higher in children when compared with adolescents (Table 1).
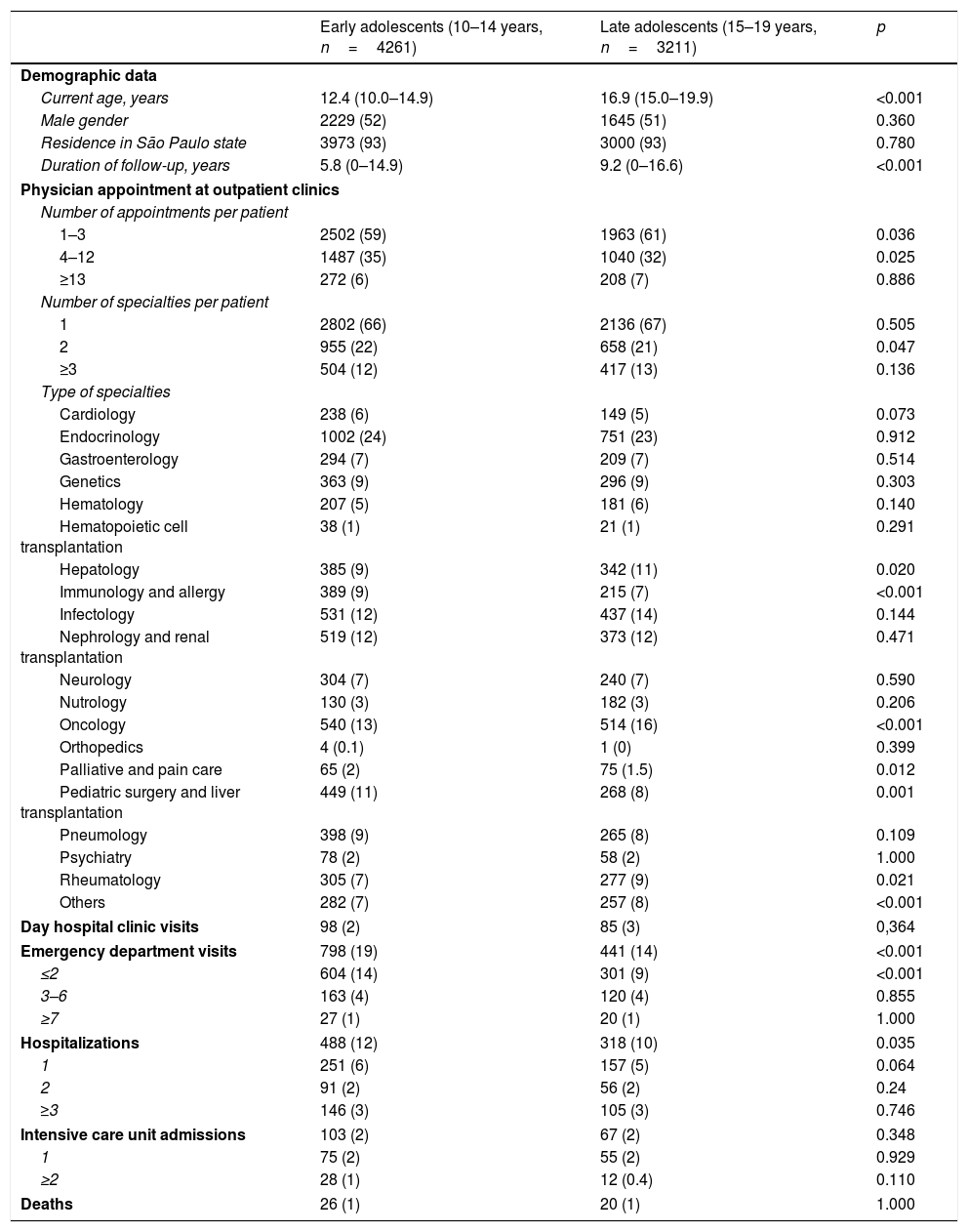
Table 2 illustrates the demographic data and characteristics of early and late adolescentes with chronic pediatric diseases attended to at the outpatient clinics at this university hospital. The median current age (12.4 [10.0–14.9] vs. 16.9 [15.0–19.9] years, p<0.001) and median follow-up duration (5.8 [0–14.9] vs. 9.2 [0–16.6] years, p<0.001) were significantly reduced in early adolescents compared to late adolescents. Early adolescents had significantly more physician appointments than late adolescents (4–12 appointments; 35% vs. 32%, p=0.025), and required more than two pediatric specialties (22% vs. 21%, p=0.047; Table 2).
Demographic data and characteristics of early and late adolescents with chronic pediatric diseases attended to at the outpatient clinics of a university hospital.
| Early adolescents (10–14 years, n=4261) | Late adolescents (15–19 years, n=3211) | p | |
|---|---|---|---|
| Demographic data | |||
| Current age, years | 12.4 (10.0–14.9) | 16.9 (15.0–19.9) | <0.001 |
| Male gender | 2229 (52) | 1645 (51) | 0.360 |
| Residence in São Paulo state | 3973 (93) | 3000 (93) | 0.780 |
| Duration of follow-up, years | 5.8 (0–14.9) | 9.2 (0–16.6) | <0.001 |
| Physician appointment at outpatient clinics | |||
| Number of appointments per patient | |||
| 1–3 | 2502 (59) | 1963 (61) | 0.036 |
| 4–12 | 1487 (35) | 1040 (32) | 0.025 |
| ≥13 | 272 (6) | 208 (7) | 0.886 |
| Number of specialties per patient | |||
| 1 | 2802 (66) | 2136 (67) | 0.505 |
| 2 | 955 (22) | 658 (21) | 0.047 |
| ≥3 | 504 (12) | 417 (13) | 0.136 |
| Type of specialties | |||
| Cardiology | 238 (6) | 149 (5) | 0.073 |
| Endocrinology | 1002 (24) | 751 (23) | 0.912 |
| Gastroenterology | 294 (7) | 209 (7) | 0.514 |
| Genetics | 363 (9) | 296 (9) | 0.303 |
| Hematology | 207 (5) | 181 (6) | 0.140 |
| Hematopoietic cell transplantation | 38 (1) | 21 (1) | 0.291 |
| Hepatology | 385 (9) | 342 (11) | 0.020 |
| Immunology and allergy | 389 (9) | 215 (7) | <0.001 |
| Infectology | 531 (12) | 437 (14) | 0.144 |
| Nephrology and renal transplantation | 519 (12) | 373 (12) | 0.471 |
| Neurology | 304 (7) | 240 (7) | 0.590 |
| Nutrology | 130 (3) | 182 (3) | 0.206 |
| Oncology | 540 (13) | 514 (16) | <0.001 |
| Orthopedics | 4 (0.1) | 1 (0) | 0.399 |
| Palliative and pain care | 65 (2) | 75 (1.5) | 0.012 |
| Pediatric surgery and liver transplantation | 449 (11) | 268 (8) | 0.001 |
| Pneumology | 398 (9) | 265 (8) | 0.109 |
| Psychiatry | 78 (2) | 58 (2) | 1.000 |
| Rheumatology | 305 (7) | 277 (9) | 0.021 |
| Others | 282 (7) | 257 (8) | <0.001 |
| Day hospital clinic visits | 98 (2) | 85 (3) | 0,364 |
| Emergency department visits | 798 (19) | 441 (14) | <0.001 |
| ≤2 | 604 (14) | 301 (9) | <0.001 |
| 3–6 | 163 (4) | 120 (4) | 0.855 |
| ≥7 | 27 (1) | 20 (1) | 1.000 |
| Hospitalizations | 488 (12) | 318 (10) | 0.035 |
| 1 | 251 (6) | 157 (5) | 0.064 |
| 2 | 91 (2) | 56 (2) | 0.24 |
| ≥3 | 146 (3) | 105 (3) | 0.746 |
| Intensive care unit admissions | 103 (2) | 67 (2) | 0.348 |
| 1 | 75 (2) | 55 (2) | 0.929 |
| ≥2 | 28 (1) | 12 (0.4) | 0.110 |
| Deaths | 26 (1) | 20 (1) | 1.000 |
Results are presented in n (%), median (range).
The frequencies of pediatric specialties were significantly higher in the early adolescent group when compared with the late group: immunology (9% vs. 7%, p<0.001), palliative and pain care (2% vs. 1.5%, p=0.012), and pediatric surgery/liver transplantation (11% vs. 8%, p=0.001). Likewise, the frequencies of emergency department visits (19% vs. 14%, p<0.001) and hospitalizations (12% vs. 10%, p=0.035) were higher in early adolescents than in late adolescents. In turn, hepatology (9% vs. 11%, p=0.020), oncology (13% vs. 16%, p<0.001), rheumatology (7% vs. 9%, p=0.021), and others (7% vs. 8%, p<0.001) were significantly higher in late adolescent group (Table 2).
DiscussionTo the best of the authors’ knowledge, this was the largest population that evaluating pediatric chronic diseases in a Latin American teaching hospital. This study evidenced that early adolescents with chronic diseases required many appointments and multiple specialties and hospital admissions.
The advantage of the present study was the inclusion of a large population, using a definition for pediatric chronic diseases.4,9 This university hospital is a Brazilian national reference center for various pediatric specialties that follows-up children and adolescents with chronic diseases. It has been recognized by the quality of its service, humanized care, capable professional team, and modern resources and researches directed to high complexity illnesses treatment for different diseases.10–16
The morbidity and mortality of children with chronic illnesses has been decreasing worldwide, mostly due to the advance in medical technologies, improvements in nutrition, hygiene conditions, vaccination, infectious diseases control, and new therapies to different diseases and comorbidities.17–19 Therefore, the early and late adolescent population with chronic health disabilities, which need high complexity medical follow-up in tertiary centers, has increased.8 Almost half of patients of the present study were adolescents with chronic diseases.
Interestingly, the adolescents of this study had a higher number of appointments over the course of one year than children, and accounted for the majority of outpatient clinic consultations in pediatric specialties. These findings indicated that adolescents’ health issues might be complex, as also reported in other studies.6 In contrast, adolescents needed less emergency care, hospital admissions, and had lower mortality, possibly suggesting lower disease severity comparing to children.
Moreover, adolescent medicine has been a growing area in both hospitals and community locations.20 This period of age includes heterogeneous groups, with peculiar characteristics of risk behaviors and burden of chronic diseases according to development phase.21–29 One of the findings of the present study was that the early adolescence group had more physician appointments and were followed-up by a high number of specialties. They also were attended more frequently in emergency department and needed a higher number of hospital admissions. These data suggested that this age group had major complexity and disease severity.
Thus, awareness for these age groups with chronic diseases should be a priority in multiprofessional teams in tertiary hospitals. Further longitudinal studies will be necessary, particularly assessing specific actions to promote adherence to clinics visits and therapies, transition status, and impact of health-related quality of life in these patients and their caregivers.
Most of the present patients were residents of the state of São Paulo. However, 7% of them lived in other states of this continental country. This patient migration is explained by the scarcity of health centers specialized in chronic pediatric disease in Brazil.
The main limitations of this study were its cross-sectional design, inclusion of the period of one year, and the lack of assessment of appointments for specific diseases according to each pediatric specialty. Furthermore, variables were analyzed according to administrative information of electronic system data, and electronic information needs human effort with chance for error. This pediatric referral health care system may not be representative of all tertiary and academic centers; moreover, the appointment, admission, and practice patterns may differ among hospitals. In addition, the sample power was not calculated, and therefore the non-significant statistical associations were not conclusive.
In conclusion, the study reported that early adolescents with chronic diseases had many appointments and multiple specialties and hospital admissions. Further large studies will be necessary to discriminate the main chronic diseases of children and adolescents and their impact on the overall development of these patients and in their relatives.
FundingThis study was supported by grants from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq303422/2015-7 to CAS), Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP2015/03756-4 to CAS), Federico Foundation, Switzerland (to CAS), and by Núcleo de Apoio à Pesquisa “Saúde da Criança e do Adolescente” da USP (NAP-CriAd) to MCS and CAS.
Conflicts of interestThe authors declare no conflicts of interest.
The authors are thankful to Ulysses Doria-Filho for the statistical analysis, and to Thiago de Freitas Passone, for assistance in data bank. The authors would like to thank all physicians of pediatric specialties, the members of the multiprofessional group, and the informatics team of this university hospital.
Please cite this article as: Alveno RA, Miranda CV, Passone CG, Waetge AR, Hojo ES, Farhat SC, et al. Pediatric chronic patients at outpatient clinics: a study in a Latin American University Hospital. J Pediatr (Rio J). 2018;94:539–45.