To evaluate the perception of parents or caregivers on the health-related quality of life (HRQOL) of children/adolescents with overweight/obesity and possible factors associated with this perception.
MethodsThis was a cross-sectional study involving 297 caregivers of children and adolescents with normal weight (n=170) and with overweight/obesity (n=127), from public and private schools in the study municipality. HRQOL scores obtained through the Child Health Questionnaire – Parent Form 50 (CHQ-PF50) were compared according to the nutritional status and gender of the children/adolescents. Multiple regression analysis was used to determine the predictive value of studied variables for the variation in HRQOL scores.
ResultsParents of children/adolescents with overweight/obesity attributed lower HRQOL scores to their children in the following domains: physical functioning (p<0.01; d=0.49), self-esteem (p<0.01; d=0.38), parental impact-emotional (p<0.05; d=0.29), family cohesion (p<0.05; d=0.26), physical summary score (p<0.05; d=0.29), and psychosocial summary score (p<0.05; d=0.25). In the multiple regression models, the variables with the highest contribution to the variation in HRQOL scores were: in the physical functioning domain, parental impact-time (β=0.23; p<0.05); self-esteem, nutritional status (β=−0.18; p≤0.01); emotional impact on parents, impact on parents’ time (β=0.31; p<0.05); and in family cohesion, global behavior (β=0.30; p<0.05).
ConclusionsA negative impact on HRQOL of children/adolescents with overweight/obesity was observed in the physical and psychosocial aspects. The nutritional status was the variable with the greatest contribution for the assessment the self-esteem of children and adolescents in this study.
Avaliar a percepção dos pais ou cuidadores a respeito da qualidade de vida relacionada à saúde (QVRS) de crianças/adolescentes com sobrepeso/obesidade e os possíveis fatores associados a essa percepção.
MétodosEstudo transversal com a participação de 297 cuidadores de crianças e adolescentes eutróficos (n=170) e com sobrepeso/obesidade (n=127), provenientes de escolas públicas e privadas do município do estudo. Escores de QVRS obtidos por meio do Child Health Questionnaire – Parent Form 50 (CHQ-PF50) foram comparados de acordo com o estado nutricional e sexo das crianças/adolescentes. Análises de regressão múltipla foram utilizadas para determinar o valor preditivo das variáveis estudadas para a variação dos escores de QVRS.
ResultadosPais de crianças/adolescentes com sobrepeso/obesidade atribuíram menores escores de QVRS para seus filhos nos domínios: função física (p<0,01; d=0,49), autoestima (p<0,01; d=0,38), impacto emocional dos pais (p<0,05; d=0,29), coesão familiar (p<0,05; d=0,26), Sumário do escore físico (p<0,05; d=0,29) e Sumário do escore psicossocial (p<0,05; d=0,25). Nos modelos de regressão múltipla, as variáveis com maior contribuição para a variação dos escores de QVRS foram: no domínio função física, impacto no tempo dos pais (ß=0,23; p<0,05); autoestima, estado nutricional (ß=-0,18; p ≤ 0,01); impacto emocional nos pais, impacto no tempo dos pais (ß=0,31; p<0,05); coesão familiar, comportamento global (ß=0,30; p<0,05).
ConclusõesHá impacto negativo na QVRS de crianças/adolescentes com sobrepeso/obesidade em aspectos físicos e psicossociais. O estado nutricional foi a variável de maior contribuição para a avaliação da autoestima das crianças e adolescentes do presente estudo.
The prevalence of obesity has significantly increased in recent decades in both developed and developing countries. In Brazil, approximately one-third of children between 5 and 9 years of age have excess weight.1 Among male and female adolescents, the prevalence is 21.7% and 19.4%, respectively.1
With the increase in obesity, the onset of type 2 diabetes, hepatic steatosis, and orthopedic problems, and an increased risk of cardiovascular complications such as hypertension, dyslipidemia, atherosclerosis, and coronary disease have been observed in children and adolescents, which results in a decrease in life expectancy.2 In the short term, the main consequences of obesity in the pediatric age range occur in the psychosocial context, such as low self-esteem, depressive symptoms, greater exposure to discrimination and bullying, and impaired health-related quality of life (HRQOL).3
Several studies have highlighted the negative impact on the perception of well-being, both in the physical and psychosocial dimensions, of children and adolescents with overweight and obesity, either reported by the children themselves or by their parents or caregivers. HRQOL assessment in children can be a problem, given the possible cognitive difficulties related to item interpretation.4 In this context, the perception of caregivers constitutes a very useful alternative for assessing the quality of life of children and adolescents.4
The Child Health Questionnaire – Parent Form 50 (CHQ-PF50) is a generic tool validated for Brazilian Portuguese and widely used in the literature to assess the quality of life of children and adolescents with chronic diseases from the parents’ perspective. Only one study used the CHQ-PF50 to verify the perception of well-being of children and adolescents with overweight and obesity. However, the reliability of internal consistency of the tool was not verified, which hinders result interpretation.5
This study aimed to evaluate, from the perspective of parents or caregivers, the HRQOL of children/adolescents with overweight/obesity and possible associated factors, using the CHQ-PF50.
MethodsThis was a cross-sectional study approved by the Ethics Committee of Universidade Federal de Uberlândia (129/05).
ParticipantsCaregivers (parents or guardians) of children and adolescents enrolled in public and private schools, aged between 9 and 12 years, with overweight, obesity, or normal weight, were invited to participate in the study. Public and private schools were included in order to allow the inclusion of children and adolescents from different socioeconomic and cultural levels, as this variable appears to contribute both to the prevalence of overweight/obesity and the quality of life.3 The onset of puberty was chosen because it is generally associated with greater physical and psychological vulnerability arising from the typical changes in this period of life.6 Caregivers who agreed to participate signed an informed consent and answered the sociodemographic questionnaire and the CHQ-PF50, which was self-applied.
Considering a prevalence of 2% for obesity and 10% for overweight,7 a maximum error of 5%, and the number of children and adolescents enrolled in the first stage of Elementary education at the private and public schools included in the study, the minimum number for the sample size was 138 parents of children/adolescents with overweight/obesity.
Anthropometric measurementsAnthropometric measurements were taken as described by the World Health Organization (WHO).8 To measure the weight, a Marte™ (Marte Científica, MG, Brazil) platform-type weighing scale was used, with a capacity up to 200kg and 50g precision; height was measured with a measuring tape 150cm long, with precision of 1mm, and the help of a wooden square.
The nutritional status of children and adolescents was assessed using the body mass index (BMI=weight/height2) anthropometric index for age, expressed as the difference between the observed value and the reference value for age and gender, with deviations from means quantified in percentiles, according to the reference population. The anthropometric profile of the Centers for Disease Control (CDC) was used as reference, with the following definitions: normal weight (BMI≥5th percentile and <85th percentile), overweight (IMC≥85th percentile and <95th percentile), and obesity (IMC≥95th percentile).9 Although this criterion is not used in Brazil as a reference for nutritional diagnosis, the CDC anthropometric standard is used by most studies of quality of life in children and adolescents with obesity,10 and its use allows for a better comparison and universalization of results. Additionally, when compared to the WHO criteria, the CDC standard has lower sensitivity and higher specificity,11 which was more appropriate for this study, as it did not aim to evaluate risk or prevention.
ProceduresAfter the schools participating in the study were selected by drawing lots, their principals or coordinators were contacted to receive information about the research objectives and later to allow the study to be conducted.
Anthropometric measurements of weight and height were taken, and the BMI was calculated to determine the nutritional status of children and adolescents from the fourth to seventh year of elementary school, aged 9–12 years. Children and adolescents who had overweight, obesity, or normal weight were selected by drawing lots according to the sampling plan. Subsequently, their caregivers were contacted by telephone to receive explanations about the study objectives and authorize their child's participation in the research. Children and adolescents diagnosed as having low weight (BMI<5th percentile) according to the CDC9 criteria were excluded, as well as those with low height for age (height<3rd percentile).
ToolsSocio-demographic questionnaireThe tool included information about the child (date of birth, gender) and personal information of caregivers (age, educational level, marital status, and family income).
Child Health Questionnaire – CHQ-PF50It is a generic tool for assessing health-related quality of life (HRQOL), which has been translated, culturally adapted, and validated for Brazilian Portuguese, aimed at children older than 5 years and adolescents.12 The CHQ-PF50 has a multidimensional characteristic and determines physical, emotional, and social well-being from the perspective of parents or guardians. The questionnaire consists of 50 items that constitute 15 domains: global health, physical functioning, limitations due to emotional aspects, limitations due to physical function, bodily pain, behavior, global behavior, mental health, self-esteem, health perception, change in health, parental impact-emotional, parental impact-time family activities, and family cohesion. The evaluation of each item uses the method of summed scores (Likert method). The final score of each domain ranges from 0 to 100. Higher scores indicate better function or sensation and, consequently, better quality of life. The scores are used to compare groups, and there is no cutoff value.12 Most domains refer to the experiences in the last four weeks, except the change in health domain, which refers to the experiences of the last 12 months. Ten domains are used to compose two summaries: physical and psychosocial.12
Statistical analysisDescriptive analysis was used for sociodemographic and clinical characterization of children and adolescents and their caregivers. To compare the demographic data between the groups, the Student's t-test (continuous variables) and the chi-squared test (categorical variables) were applied.
The internal consistency reliability was verified by Cronbach's α-coefficient for each multi-item scale; 0.5 was considered as the minimum acceptable value for the assessment of the tool internal consistency.13 In this study, the Cronbach's alpha coefficient was greater than 0.5 in all domains of the CHQ-PF50, except for the health perception domain (Cronbach's alpha=0.21), a fact that has occurred in the Brazilian version of the tool.13
Student's t-test was used to compare the mean domain scores and the CHQ-PF50 components of children and adolescents with overweight/obesity and normal weight and also to compare the CHQ-PF50 scores according to gender in the overweight/obesity group. The magnitude of the statistically significant differences was calculated based on the determination of the effect size (Cohen's d). Values of d equal to 0.2; 0.5; and 0.8 were considered as small, medium and large effect sizes, respectively.14
The correlations between the domains of the questionnaire and demographic data were evaluated by Spearman's correlation coefficient. Hierarchical multiple regression analysis was used to determine the predictive value of the assessed variables for the HRQOL scores of the studied population.
Data were analyzed using the SPSS Statistics program (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. NY, USA). The significance level for the rejection of the null hypothesis was set at p<0.05.
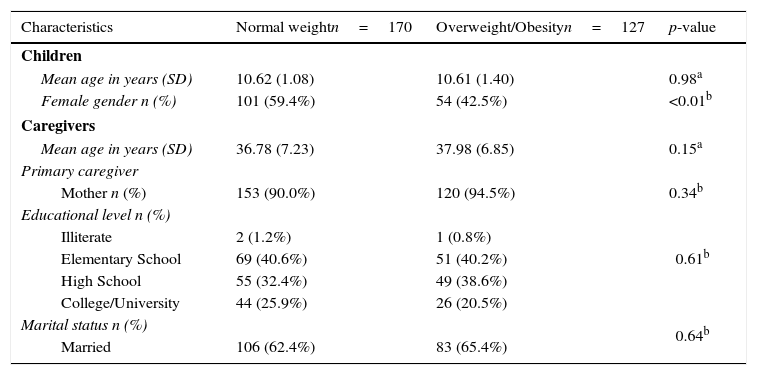
ResultsSociodemographic characteristicsA total of 360 caregivers of children and adolescents were invited to participate. Sixty-three participants were excluded due to incomplete data on the CHQ-PF50. Therefore, the study included 297 caregivers of children and adolescents with normal weight (n=170) and with overweight/obesity (n=127). The age of the children and adolescents ranged from 9 to 12 years (mean 10.6 years for normal weight and 10.63 for overweight/obesity). Most caregivers were mothers with complete elementary school level (Table 1).
Socio-demographic characteristics of participating parents/caregivers and children/adolescents.
| Characteristics | Normal weightn=170 | Overweight/Obesityn=127 | p-value |
|---|---|---|---|
| Children | |||
| Mean age in years (SD) | 10.62 (1.08) | 10.61 (1.40) | 0.98a |
| Female gender n (%) | 101 (59.4%) | 54 (42.5%) | <0.01b |
| Caregivers | |||
| Mean age in years (SD) | 36.78 (7.23) | 37.98 (6.85) | 0.15a |
| Primary caregiver | |||
| Mother n (%) | 153 (90.0%) | 120 (94.5%) | 0.34b |
| Educational level n (%) | 0.61b | ||
| Illiterate | 2 (1.2%) | 1 (0.8%) | |
| Elementary School | 69 (40.6%) | 51 (40.2%) | |
| High School | 55 (32.4%) | 49 (38.6%) | |
| College/University | 44 (25.9%) | 26 (20.5%) | |
| Marital status n (%) | 0.64b | ||
| Married | 106 (62.4%) | 83 (65.4%) | |
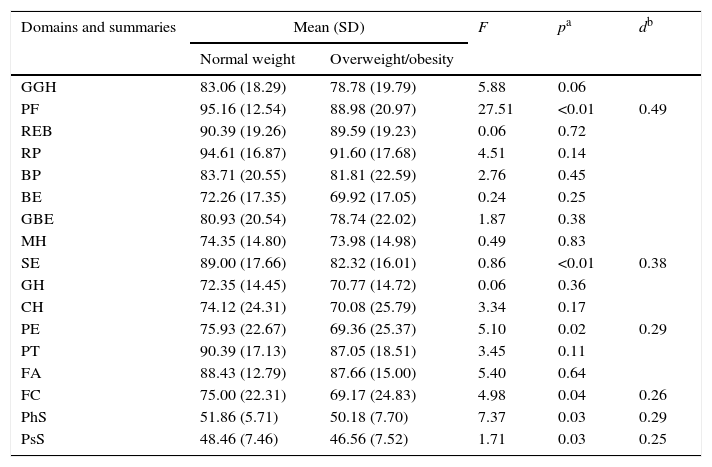
Parents of children and adolescents with overweight/obesity attributed lower scores of the CHQ-PF50 to the domains: physical functioning (p<0.01; d=0.49), self-esteem (p<0.01; d=0.38), parental impact-emotional (p<0.05; d=0.29), family cohesion (p<0.05; d=0.26), physical summary score (p<0.05; d=0.29), and psychosocial summary score (p<0.05; d=0.25; Table 2).
Quality of life scores obtained by the CHQ-PF50 of children/adolescents according to the nutritional status.
| Domains and summaries | Mean (SD) | F | pa | db | |
|---|---|---|---|---|---|
| Normal weight | Overweight/obesity | ||||
| GGH | 83.06 (18.29) | 78.78 (19.79) | 5.88 | 0.06 | |
| PF | 95.16 (12.54) | 88.98 (20.97) | 27.51 | <0.01 | 0.49 |
| REB | 90.39 (19.26) | 89.59 (19.23) | 0.06 | 0.72 | |
| RP | 94.61 (16.87) | 91.60 (17.68) | 4.51 | 0.14 | |
| BP | 83.71 (20.55) | 81.81 (22.59) | 2.76 | 0.45 | |
| BE | 72.26 (17.35) | 69.92 (17.05) | 0.24 | 0.25 | |
| GBE | 80.93 (20.54) | 78.74 (22.02) | 1.87 | 0.38 | |
| MH | 74.35 (14.80) | 73.98 (14.98) | 0.49 | 0.83 | |
| SE | 89.00 (17.66) | 82.32 (16.01) | 0.86 | <0.01 | 0.38 |
| GH | 72.35 (14.45) | 70.77 (14.72) | 0.06 | 0.36 | |
| CH | 74.12 (24.31) | 70.08 (25.79) | 3.34 | 0.17 | |
| PE | 75.93 (22.67) | 69.36 (25.37) | 5.10 | 0.02 | 0.29 |
| PT | 90.39 (17.13) | 87.05 (18.51) | 3.45 | 0.11 | |
| FA | 88.43 (12.79) | 87.66 (15.00) | 5.40 | 0.64 | |
| FC | 75.00 (22.31) | 69.17 (24.83) | 4.98 | 0.04 | 0.26 |
| PhS | 51.86 (5.71) | 50.18 (7.70) | 7.37 | 0.03 | 0.29 |
| PsS | 48.46 (7.46) | 46.56 (7.52) | 1.71 | 0.03 | 0.25 |
GGH, global health; PF, physical functioning; REB, role/social limitations-emotional/behavioral; RP, role/social limitations-physical; BP, bodily pain; BE, behavior; GBE, global behavior item; MH, mental health; SE, self-esteem; GH, general health perceptions; CH, change in health; PE, parental impact-emotional; PT, parental impact-time; FA, family activities; FC, family cohesion; PhS, physical summary score; PsS, psychosocial summary score.
There were no differences between the mean scores of the CHQ-PF50 domains of children and adolescents with overweight/obesity according to gender (p>0.05; data not shown).
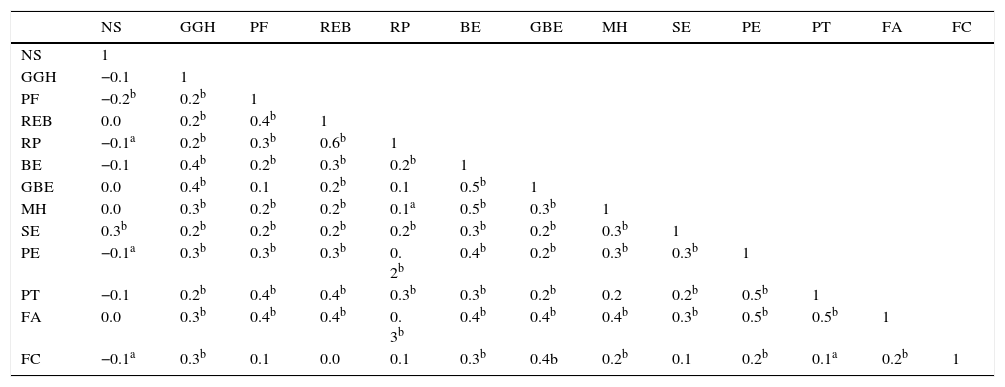
The correlations between the sociodemographic data and the domains of the CHQ-PF50 were weak (r<0.30), except between nutritional status (overweight/obesity or normal weight) and self-esteem (SE; p<0.01; Table 3).
Spearman's correlation coefficients between quality of life scores obtained through CHQPF-50 and sociodemographic variables of children and adolescents of the study.
| NS | GGH | PF | REB | RP | BE | GBE | MH | SE | PE | PT | FA | FC | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NS | 1 | ||||||||||||
| GGH | −0.1 | 1 | |||||||||||
| PF | −0.2b | 0.2b | 1 | ||||||||||
| REB | 0.0 | 0.2b | 0.4b | 1 | |||||||||
| RP | −0.1a | 0.2b | 0.3b | 0.6b | 1 | ||||||||
| BE | −0.1 | 0.4b | 0.2b | 0.3b | 0.2b | 1 | |||||||
| GBE | 0.0 | 0.4b | 0.1 | 0.2b | 0.1 | 0.5b | 1 | ||||||
| MH | 0.0 | 0.3b | 0.2b | 0.2b | 0.1a | 0.5b | 0.3b | 1 | |||||
| SE | 0.3b | 0.2b | 0.2b | 0.2b | 0.2b | 0.3b | 0.2b | 0.3b | 1 | ||||
| PE | −0.1a | 0.3b | 0.3b | 0.3b | 0. 2b | 0.4b | 0.2b | 0.3b | 0.3b | 1 | |||
| PT | −0.1 | 0.2b | 0.4b | 0.4b | 0.3b | 0.3b | 0.2b | 0.2 | 0.2b | 0.5b | 1 | ||
| FA | 0.0 | 0.3b | 0.4b | 0.4b | 0. 3b | 0.4b | 0.4b | 0.4b | 0.3b | 0.5b | 0.5b | 1 | |
| FC | −0.1a | 0.3b | 0.1 | 0.0 | 0.1 | 0.3b | 0.4b | 0.2b | 0.1 | 0.2b | 0.1a | 0.2b | 1 |
GGH, global health; PF, physical functioning; REB, role/social limitations-emotional/behavioral; RP, role/social limitations-physical; BE, behavior; GBE, global behavior item; MH, mental health; SE, self-esteem; PE, parental impact-emotional; PT, parental impact-time; FA, family activities; FC, family cohesion; NS, nutritional status.
Spearman's correlation test.
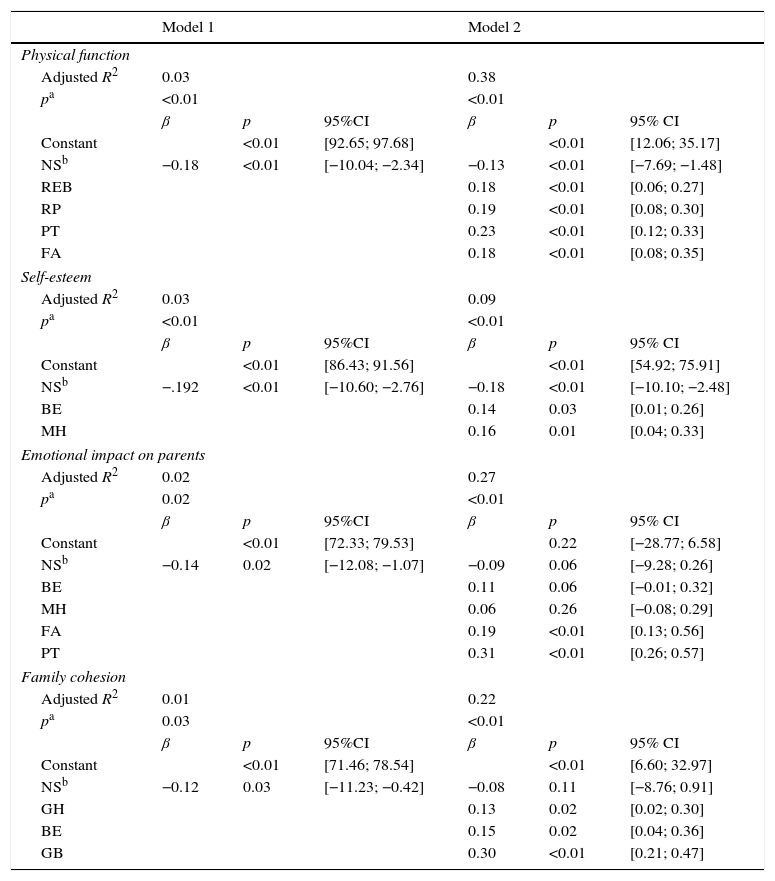
The domains of HRQOL that showed differences according to the nutritional status were included in the multivariate analysis as dependent variables. As independent variables, the nutritional status (overweight/obesity/normal weight) and the HRQOL domains with correlation coefficients >0.3 (r≥0.3) with the dependent variables were selected. For the dependent variable physical functioning, a model of high variance explanation (R2=0.39; p<0.05) was obtained for the variables nutritional status, limitations due to emotional problems, limitations due to physical function, parental impact-time, and family activities. The variable that contributed the most to the model was parental impact-time (β=0.23, p<0.05).
For the dependent variable self-esteem, a model of low variance explanation (R2=0.10, p≤0.01) was obtained with the variables nutritional status, behavior, and mental health. The variable that contributed the most negatively to the model was nutritional status (β=−0.18; p≤0.01). For the dependent variable parental impact-emotional, a model of high variance explanation (R2=0.28; p<0.05) was obtained for the variables nutritional status, global health, behavior, mental health, family activities, and parental impact-time. The variable that most contributed to the model was the parental impact-time (β=0.31, p<0.05). Regarding the family cohesion domain as the dependent variable, significant results were observed in both models (p<0.05), with moderate variance explanation with the variables nutritional status, global health, behavior, and global behavior (R2=0.23; p<0.05). The variable that most contributed to the model was global behavior (β=0.30; p<0.05; Table 4). The physical and psychosocial summaries were excluded from the multiple regression analysis to avoid the multicollinearity phenomenon.
Multiple linear regression models for associations between self-esteem, nutritional status, and psychological domains of quality of life.
| Model 1 | Model 2 | |||||
|---|---|---|---|---|---|---|
| Physical function | ||||||
| Adjusted R2 | 0.03 | 0.38 | ||||
| pa | <0.01 | <0.01 | ||||
| β | p | 95%CI | β | p | 95% CI | |
| Constant | <0.01 | [92.65; 97.68] | <0.01 | [12.06; 35.17] | ||
| NSb | −0.18 | <0.01 | [−10.04; −2.34] | −0.13 | <0.01 | [−7.69; −1.48] |
| REB | 0.18 | <0.01 | [0.06; 0.27] | |||
| RP | 0.19 | <0.01 | [0.08; 0.30] | |||
| PT | 0.23 | <0.01 | [0.12; 0.33] | |||
| FA | 0.18 | <0.01 | [0.08; 0.35] | |||
| Self-esteem | ||||||
| Adjusted R2 | 0.03 | 0.09 | ||||
| pa | <0.01 | <0.01 | ||||
| β | p | 95%CI | β | p | 95% CI | |
| Constant | <0.01 | [86.43; 91.56] | <0.01 | [54.92; 75.91] | ||
| NSb | −.192 | <0.01 | [−10.60; −2.76] | −0.18 | <0.01 | [−10.10; −2.48] |
| BE | 0.14 | 0.03 | [0.01; 0.26] | |||
| MH | 0.16 | 0.01 | [0.04; 0.33] | |||
| Emotional impact on parents | ||||||
| Adjusted R2 | 0.02 | 0.27 | ||||
| pa | 0.02 | <0.01 | ||||
| β | p | 95%CI | β | p | 95% CI | |
| Constant | <0.01 | [72.33; 79.53] | 0.22 | [−28.77; 6.58] | ||
| NSb | −0.14 | 0.02 | [−12.08; −1.07] | −0.09 | 0.06 | [−9.28; 0.26] |
| BE | 0.11 | 0.06 | [−0.01; 0.32] | |||
| MH | 0.06 | 0.26 | [−0.08; 0.29] | |||
| FA | 0.19 | <0.01 | [0.13; 0.56] | |||
| PT | 0.31 | <0.01 | [0.26; 0.57] | |||
| Family cohesion | ||||||
| Adjusted R2 | 0.01 | 0.22 | ||||
| pa | 0.03 | <0.01 | ||||
| β | p | 95%CI | β | p | 95% CI | |
| Constant | <0.01 | [71.46; 78.54] | <0.01 | [6.60; 32.97] | ||
| NSb | −0.12 | 0.03 | [−11.23; −0.42] | −0.08 | 0.11 | [−8.76; 0.91] |
| GH | 0.13 | 0.02 | [0.02; 0.30] | |||
| BE | 0.15 | 0.02 | [0.04; 0.36] | |||
| GB | 0.30 | <0.01 | [0.21; 0.47] | |||
GGH, general health; REB, role/social limitations-emotional/behavioral; RP, role/social limitations-physical; BE, behavior; GBE, global behavior item; MH, mental health; PT, parental impact-time; FA, family activities; NS, nutritional status.
The present study demonstrated that the caregivers perceived physical and psychosocial impairment in the HRQOL in children and adolescents with overweight and obesity in the domains physical function, self-esteem, emotional impact on parents and family cohesion, and in the physical and psychosocial summaries. However, the hierarchical multiple regression models indicated that excess weight was not the main determining factor for the negative impact on most domains of the CHQ-PF50. The presence of overweight/obesity was a major contributing factor only for the self-esteem domain.
Previous studies have also found that the presence of overweight or obesity is related to multidimensional impairment in the HRQOL of children and adolescents.7,15
The discrimination experienced by obese children and adolescents is rising. The impact starts at an early age, resulting in fewer friends, less affection from parents, and poorer school performance. With the experience of being bullied, both in the traditional and the cyber versions, the obese adolescent has little motivation to perform physical activity, avoids healthy lifestyles, and may have suicidal ideation.16 Additionally, it is known that those who remain obese for more than four years and have low self-esteem are more likely to develop risk behaviors such as alcohol consumption and smoking, when compared to their obese peers with normal self-esteem.17
Adolescence is a stage when peer approval is important for self-esteem development.17 Therefore, the bullying, criticism, and social isolation that many of these children and adolescents experience, whether by their family or friends, impair the development and consolidation of self-esteem, resulting in emotional problems such as depression, anxiety, low self-esteem, and low appraisal of one's body.15,17,18 It should also be considered, as indicated in the present study, that other factors contribute to the impaired perception of psychosocial well-being, such as disturbance in the family environment (emotional impact on parents) and poor family cohesion.19
The parents’ time limitation also appears to contribute to a worse perception of HRQOL related to physical function in children and adolescents with overweight or obesity.20 In the present study, this variable accounted for the highest contribution to the variance of the physical function model. Although parents of children/adolescents with overweight/obesity also assigned poorer quality of life to the physical function of their children in previous studies,21 the results of the present study lead to the conclusion that the nutritional status exerts less influence in this observation.
While acknowledging that parents generally underestimate the weight of their children and do not recognize overweight or obesity as a disease,22 this study identified an emotional impact on parents. However, a recent study23 demonstrated a greater awareness of parents about the real weight of their children by concluding that overweight mothers have a higher concern for the future weight of their children, even when these have normal weight. Additionally, parents with overweight or those who perceive that their child's weight constitutes a health problem are more willing to adopt changes to help their children.24 For these parents, the nutritional status of their children can bring concerns about their health, behavior, well-being, and school performance.20 In addition to the emotional impact observed on parents of children/adolescents with overweight/obesity, the need to get them involved in their children's treatment requires a change in their lifestyle. This involvement is often difficult, as many parents report lack of time to supervise their children's nutrition and physical activities.25 The parents’ behavior is of great importance in the treatment of these children and adolescents, as in early childhood parents serve as models and providers for children.26 Thus, parents are often the target of preventive public health interventions aimed at improving the child's diet,26 as prevention is currently considered to be the most effective measure to control childhood obesity.27 Programs of childhood obesity prevention and treatment that are based on family behavior are among the most effective and, therefore, have shown that parental involvement is the key for the success of health policies aimed at children and adolescents.28
Previous studies have shown poorer quality of life among obese female children and adolescents, from the perspective of parents.5 However, this difference was not observed in this study. The fact that the study population was at the beginning of puberty may explain this finding. At this age range, the adolescent has yet to experience the changes that are typical of this phase, which usually occurs after the age of 12 (menarche and hormonal changes),29 the age at which the differences between genders start to become evident.6
This study brings important contributions by showing the importance of the parents’ perspective on the HRQOL of children and by assessing the magnitude of the differences regarding the perception of HRQOL of children and adolescents according to their nutritional status. Another important contribution refers to building comprehensive models in an attempt to evaluate the behavior of a greater number of studied variables in the variation of HRQOL scores of children and adolescents in the study.
However, some limitations should be mentioned. This was a cross-sectional study, which does not allow for the assessment of the cause-and-effect association between the study variables. The reduction in the study sample size due to loss of data may have masked possible differences in quality of life scores of the analyzed groups. However, losses related to difficulties inherent to CHQ-PF50 are commonly observed in the studies that use this tool.5 Although the outcomes of the present study are restricted to the age group of 9–12 years, it is known that adolescence is a very important period for the psychosocial development of young individuals. The onset of puberty can be considered as the moment in which someone has a greater awareness of their own body size,18 and it is described as the period of greatest vulnerability for the development of obesity.30
From the perception of parents or caregivers, it can be concluded that there is a negative impact on the HRQOL of children and adolescents with overweight and obesity regarding the physical and psychosocial aspects. The impact on parents’ time was the variable that most contributed to the perception of physical function of their children. Excess weight was the variable with the highest negative impact when assessing the self-esteem of children and adolescents in this study. Knowing the perception of parents about the impact of obesity on quality of life of their children and the variables involved in this perception is crucial for the involvement of these caregivers in the prevention and treatment of obesity.
FundingFundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG) (PPM-00306-8); Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) (40973/2006-0).
Conflicts of interestThe authors declare no conflicts of interest.
To the Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG) and Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) for their financial support to this research project.
Please cite this article as: Nascimento MM, Melo TR, Pinto RM, Morales NM, Mendonça TM, Paro HB, et al. Parents’ perception of health-related quality of life in children and adolescents with excess weight. J Pediatr (Rio J). 2016;92:65–72.
Study conducted at Universidade Federal de Uberlândia, Uberlândia, MG, Brazil.