The identification of parental needs in Neonatal Intensive Care Units is essential to design and implement family-centered care. This article aims to validate the Neonatal Intensive Care Units Family Needs Inventory for the Portuguese population, and to propose a Short Form.
MethodsA linguistic adaptation of the Neonatal Intensive Care Units Family Needs Inventory, a self-report scale with 56-items, was performed. The instrument was administered to 211 parents of infants hospitalized in all level III Neonatal Intensive Care Units in the North of Portugal, 15–22 days after admission (July of 2013–June of 2014). The number of items needed to achieve reliability close to 0.8 was calculated using by the Spearman–Brown formula. The global goodness of fit of the scale was evaluated using the comparative fit index. Construct validity was assessed through association of each dimension score with socio-demographic and obstetric characteristics.
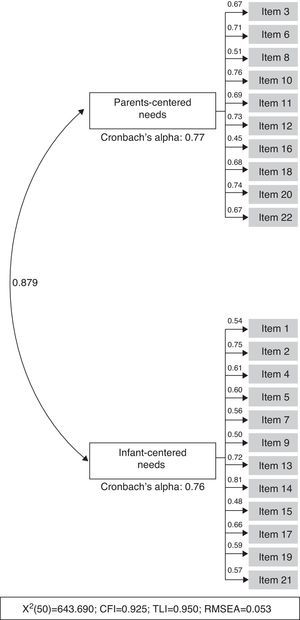
ResultsExploratory factor analysis revealed two dimensions, one focused on parents’ needs and another on the infant's needs. To compose the Short Form Inventory, items with ceiling effect were eliminated and 22 items were submitted to confirmatory analysis, which supported the existence of two dimensions (CFI=0.925). The Short Form showed a high degree of reliability (alpha≥0.76). Less educated and older parents more frequently attributed a significantly higher importance to parent-centered needs, while parents of multiples revealed a tendency to value infant-centered needs.
ConclusionsThe Short Form of the Neonatal Intensive Care Units Family Needs Inventory is a brief, simple, and valid instrument with a high degree of reliability. Further studies are needed to explore associations with practices of family-centered care.
A identificação de necessidades parentais em Unidades de Cuidados Intensivos Neonatais (UCINs) é essencial para planejar e implementar cuidados centrados na família. Este artigo pretende validar o Inventário de Necessidades da Família em UCIN na população portuguesa e propor uma Versão Curta do mesmo.
MetodologiaFoi realizada uma adaptação linguística do Inventário de Necessidades da Família na UCIN, uma escala de autorrelato com 56 itens. O instrumento foi aplicado a 211 pais de bebês internados em todas as UCINs de nível III no Norte de Portugal 15 a 22 dias após a internação (julho de 2013-junho de 2014). O número de itens necessários para atingir uma confiabilidade próxima a 0,8 foi calculado pela fórmula de Spearman-Brown. A adequação global da escala foi avaliada pelo índice de ajuste comparativo (CFI). A validade de construto foi avaliada através da associação do escore de cada dimensão com características sociodemográficas e obstétricas.
ResultadosA análise fatorial exploratória revelou duas dimensões, uma focada nas necessidades dos pais e outra, nas necessidades do bebê. Para compor a Versão Curta do Inventário, os itens com efeito teto foram eliminados, e 22 itens foram submetidos a análise confirmatória, que sustentou a existência de duas dimensões (CFI=0,925). A Versão Curta apresentou alto grau de confiabilidade (alfa ≥ 0,76). Pais mais velhos e com menor escolaridade atribuíram, mais frequentemente, maior importância à subescala de necessidades centradas nos pais enquanto os pais de gêmeos revelaram uma tendência de valorizar as necessidades centradas nos bebês.
ConclusõesA Versão Curta do Inventário de Necessidades da Família em UCIN é um instrumento breve, simples e válido com alto grau de confiabilidade. São necessários estudos adicionais para explorar as associações com práticas de cuidados centrados na família.
The improvement in the quality of antenatal and neonatal care led to a decrease in perinatal mortality and morbidity in the last three decades,1 but prematurity is still the worldwide leading direct cause of neonatal death and short- and long-term morbidity.2 The hospitalization of a newborn in a neonatal intensive care unit (NICU) constitutes a disruptive life event with impact on family health.3,4 During the hospitalization period, parents need to assume new roles under adverse conditions,5 such as physical separation from the child, structured and controlled opportunities of interaction, difficulties in feeling part of the infant's care, and fear for his/her survival and future development, while also experiencing feelings of hope, love, and happiness.3,6,7 Parents have reported the importance of obtaining information and guidance,8 trusting in the healthcare team,9 and experiencing support from staff members and from his/her partner.9,10
Family-centered care, defined as provision of care that is respectful of and responsive to parents preferences, needs, and values, is essential for a successful design and implementation of evidence-based practices in NICU.11 Therefore, the identification of parental needs may contribute for diminishing the risk for the development of parental stress and several psychopathological symptoms.9,12
The NICU Family Needs Inventory is a reliable self-report instrument to assess the parents’ needs during an infant's hospitalization in NICU.13 To listen to parents is particularly important in a context where healthcare professionals and parents tend to identify different parental needs.14 To the best of the authors’ knowledge, the NICU Family Needs Inventory is the only scale specifically designed and validated for the NICU setting, but its utility for health research, as well as for counseling and clinical practice, is limited by its length (56-items). A shorter version of the Inventory, brief and easy to administrate, but also valid and with a high degree of reliability, would actively contribute to the identification of the specific needs of each family, and for their inclusion in health care, while lessening the intrusion and ensuring the ethical principles of respect for autonomy, non-maleficence, beneficence, and justice.15
Thus, this study aimed to validate the Neonatal Intensive Care Unit (NICU) Family Needs Inventory for the Portuguese population, and to propose a Short Form.
MethodsOriginal instrumentThe NICU Family Needs Inventory13 was the instrument used for data collection. It is a self-reported scale divided into five subscales: support, information, comfort, assurance, and proximity. It consists of 56 need statements designed to measure the importance attributed to family needs by mothers and fathers in the NICU setting, ranging from 1 to 4 (not important, slightly important, important, and very important, respectively). Each item could also be classified as not applicable, if the participants had never experienced the specific need. Permission to use or modify the inventory was granted by the original author.
Linguistic adaptationTwo native Portuguese speakers proficient in English translated NICU Family Needs Inventory and an expert committee, with backgrounds in Public Health, Psychology, and Sociology, ensured conceptual and item equivalence. The discrepancies between the two translations were solved by consensus and merged into a single Portuguese version. After completing the Inventory, parents were invited to report eventual doubts and suggestions.
Sample and recruitmentThe adapted version of the Inventory was administered to a cohort of parents of very preterm infants, which has been previously described.16 Briefly, all parents of very preterm infants born between July 1, 2013 and June 30, 2014 who were hospitalized in all level III NICU that provided subspecialty care for critically ill newborn infants17 in the Northern Health Region of Portugal (n=7), were consecutively invited to participate in the study. Parents were approached during their hospital stay by a NICU healthcare professional (neonatologist or nurse), who was responsible for the presentation of the study and invitation to participate, 15–22 days after birth. Only parents with infants born before 32 weeks of gestation and still hospitalized in NICU at the time of the interview were considered eligible to participate in the study. Parents with serious illness that precluded NICU visitation (e.g. severe chronic conditions), families who were absent from NICU during the hospitalization period, and parents whose infants were discharged or transferred to another hospital were excluded. Among the 126 eligible couples, 122 (98.6%) agreed to participate. The final sample included 120 mothers and 91 fathers (in 89 cases, both parents participated in the study). Refusals were justified by lack of time to participate (n=3) and psychological unavailability (n=1). During data collection, two mothers were absent due to medical complications and 31 fathers were absent due to professional commitments or emigration.
Trained interviewers were responsible for interviewing mothers and fathers, separately. Data on socio-demographic characteristics were collected through face-to-face interviews, using a structured questionnaire. Afterwards, the parents were asked to fill the NICU Family Needs Inventory.13 Clinical records were reviewed to retrieve data on multiple pregnancy, gravidity, and pregnancy complications (which included infectious, placental, hemorrhagic, and cardiovascular complications). Data on neonatal birth weight and gestational age were also collected. According to the World Health Organization definitions, extremely low birth weight and extremely premature infants were defined as those with birth weight below 1000g and gestational age under 28 weeks, respectively.18
The present investigation was approved by the Ethics Committee of the seven Hospitals with NICU where data was collected and by the National Committee for Data Protection. Each participant signed an informed consent.
Statistical analysisDue to the low variability in the response scale, items were dichotomized as very important (scoring 4) or not very important (scoring 3 or less, combining the answers not important, slightly important, and important) for analysis. Exploratory factor analysis for dichotomous variables was performed to assess the dimensionality of the scale, whether the construct study is a single concept or multiple concepts. When items are used to form scale they should all be correlated with one another, and they should have internal consistency. Cronbach's alpha was used to measure internal consistency and a Cronbach alpha value of 0.8 or higher was considered as good internal consistency.
Considering that the aim of the study was to construct a short-form, the Spearman–Brown formula19 allowed for the estimation of the minimum number of items needed to achieve reliability close to 0.8. Items with the best item-fit statistics for the one-parameter logistic model (Rasch model) were included in the Short Version. This ensured that items with similar psychometric quality were selected. The global goodness of fit of the Short Version was evaluated using the comparative fit index (CFI), the Tucker–Lewis Index (TLI), and the root mean squared error approximation (RMSEA), obtained from the confirmatory factor analysis. Cut off values above 0.9 for CFI and TLI, and below 0.10 for RMSEA indicated a good fit of the model.20
To assess the construct validity of the Short Version, the authors measured the association of each dimension score with socio-demographic and obstetric characteristics of the participants, and a multilevel model with a random effect by couple was used to estimate the differences between groups, correcting for the couple dependency. It was assumed that those with more adverse social environments would be more likely to attribute higher importance to parents-centered needs. The subscales scores of the Short Version were calculated as the sum of all items after dichotomization. When items were classified as non-applicable, the score was calculated as the mean of all items answered multiplied by the total number of items in each subscale (n=10 for the parents-centered needs subscale and n=12 for the infant-centered needs subscale).
Statistical analyses were performed using the software STATA 11.0 (StataCorp. 2009. Stata Statistical Software: Release 11. College Station, TX, USA), R 2.12.1 (R Statistical Programming Language 2.12.1), and MPlus (MPlus version 5.2.).
ResultsThe majority of the participants had less than 35 years of age (70.1%), 63.0% had more than nine years of education, and 65.4% reported a household monthly income above € 1000. This was the first pregnancy for 55.5% of the participants and 42.7% had a pregnancy complication. In this sample, 29.9% of the participants had an extremely low birth weight delivery, 21.3% an extremely preterm delivery, and 23.7% of the pregnancies were multiple (Table 1).
Associations between the score of each subscale of the Short Version with socio-demographic and obstetric characteristics of the participants (n=211).
| Totaln (%) | Parents-centered needsMean (SD) | p | Infant-centered needsMean (SD) | p | |
|---|---|---|---|---|---|
| Overall | 3.5 (2.6) | 8.6 (2.7) | |||
| Sex | |||||
| Female | 120 (56.9) | 3.7 (2.6) | 8.8 (2.7) | ||
| Male | 91 (43.1) | 3.3 (2.4) | 0.239 | 8.3 (2.7) | 0.230 |
| Age (years) | |||||
| <35 | 148 (70.1) | 3.3 (2.3) | 8.5 (2.6) | ||
| ≥35 | 63 (29.9) | 4.1 (3.0) | 0.037 | 8.8 (2.9) | 0.516 |
| Education (years) | |||||
| <9 | 78 (37.0) | 4.3 (2.5) | 8.7 (2.9) | ||
| ≥9 | 133 (63.0) | 3.1 (2.5) | <0.001 | 8.5 (2.6) | 0.600 |
| Household monthly income (€) | |||||
| ≤1000 | 72 (34.6) | 3.9 (2.6) | 8.4 (3.0) | ||
| >1000 | 136 (65.4) | 3.4 (2.6) | 0.149 | 8.7 (2.6) | 0.518 |
| Gravidity | |||||
| 0 | 117 (55.5) | 3.7 (2.6) | 8.8 (2.6) | ||
| ≥1 | 94 (44.5) | 3.4 (2.5) | 0.446 | 8.2 (2.9) | 0.111 |
| Pregnancy complicationsa | |||||
| Yes | 90 (42.7) | 3.4 (2.7) | 8.3 (2.6) | ||
| No | 121 (57.4) | 3.6 (2.5) | 0.530 | 8.8 (2.9) | 0.256 |
| Multiple pregnancy | |||||
| Yes | 50 (23.7) | 4.0 (2.6) | 9.4 (2.8) | ||
| No | 161 (76.3) | 3.4 (2.5) | 0.117 | 8.3 (2.7) | 0.024 |
| Extremely premature deliveryb | |||||
| Yes | 45 (21.3) | 3.5 (2.8) | 8.4 (3.0) | ||
| No | 166 (78.7) | 3.6 (2.5) | 0.943 | 8.6 (2.7) | 0.692 |
| Extremely low birth weight deliveryc | |||||
| Yes | 63 (29.9) | 3.3 (2.5) | 8.4 (2.6) | ||
| No | 148 (70.1) | 3.6 (2.6) | 0.375 | 8.6 (2.8) | 0.547 |
SD, standard deviation.
Note: The subscales scores were calculated as the sum of all items after dichotomization as very important or not very important (combining the answers not important, slightly important and important). In the case of having items classified as non-applicable, the score was calculated as the mean of all items answered multiplied by the total number of items in each subscale (n=10 for parents-centered needs subscale and n=12 for infant-centered needs subscale).
Includes the following complications: gestational hypertension; preeclampsia; eclampsia; HELLP syndrome; gestational diabetes mellitus; acute pyelonephritis; metrorragia; placenta previa; placental abruption; fetal malformations; pulmonary infection; urinary tract infections; threat of miscarriage; and cholestasis of pregnancy.
Overall, 60.7% of the need statements were identified as very important needs (mean score>3.5) by the participants and none of the statements were ranked as not important. Only one item (1.8%), “to have a pastor, clergy, or other person from my church visit”, was regarded as slightly important (mean score between 1.5 and 2.5).
Exploratory factor analysis for dichotomous variables revealed two dimensions, with almost all of the items associated to needs centered on the parents in the first dimension, and all those associated with infant-centered needs in the second (Table 2).
Proportion of participants who answered “very important” in each item, standardized factor loadings for two factors in exploratory factor analysis (EFA).
| Very important | Two factor EFA | ||
|---|---|---|---|
| n (%) | std.z1 | std.z2 | |
| Item | |||
| 1 | 191 (91.4) | 0.673 | −0.173 |
| 2 | 147 (72.1) | 0.365 | 0.196 |
| 3 | 157 (75.5) | 0.652 | −0.173 |
| 4 | 178 (84.8) | 0.658 | 0.137 |
| 5 | 200 (95.7) | 0.773 | −0.099 |
| 6 | 186 (91.6) | 0.723 | −0.022 |
| 7 | 139 (66.2) | 0.644 | −0.065 |
| 8 | 96 (45.7) | 0.389 | 0.402 |
| 9 | 96 (49.5) | 0.319 | 0.460 |
| 10 | 189 (90.0) | 0.848 | −0.094 |
| 11 | 181 (86.6) | 0.754 | −0.116 |
| 12 | 104 (50.0) | 0.454 | 0.288 |
| 13 | 167 (80.7) | 0.450 | 0.255 |
| 14 | 197 (94.7) | 0.994 | 0.651 |
| 15 | 63 (31.3) | 0.440 | 0.358 |
| 16 | 131 (63.6) | 0.636 | −0.039 |
| 17 | 152 (73.8) | 0.493 | 0.094 |
| 18 | 139 (67.5) | 0.701 | 0.006 |
| 19 | 101 (49.3) | 0.262 | 0.328 |
| 20 | 186 (89.0) | 0.902 | −0.424 |
| 21 | 56 (27.3) | 0.404 | 0.455 |
| 22 | 22 (11.7) | −0.112 | 0.941 |
| 23 | 120 (57.7) | 0.643 | 0.081 |
| 24 | 35 (17.7) | −0.009 | 0.884 |
| 25 | 142 (68.3) | 0.614 | 0.265 |
| 26 | 114 (54.6) | 0.546 | 0.315 |
| 27 | 101 (45.6) | 0.557 | 0.407 |
| 28 | 96 (45.9) | 0.482 | 0.422 |
| 29 | 100 (48.1) | 0.312 | 0.272 |
| 30 | 90 (43.3) | 0.221 | 0.694 |
| 31 | 106 (56.1) | 0.274 | 0.290 |
| 32 | 110 (53.1) | 0.411 | 0.407 |
| 33 | 98 (47.3) | 0.317 | 0.528 |
| 34 | 169 (82.0) | 0.595 | 0.272 |
| 35 | 196 (94.2) | 0.824 | 0.021 |
| 36 | 173 (83.6) | 0.650 | 0.104 |
| 37 | 158 (79.0) | 0.612 | 0.266 |
| 38 | 191 (91.8) | 0.893 | 0.000 |
| 39 | 201 (96.6) | 1.008 | −0.023 |
| 40 | 192 (92.3) | 0.948 | −0.348 |
| 41 | 92 (44.4) | 0.028 | 0.835 |
| 42 | 160 (78.8) | 0.747 | 0.094 |
| 43 | 59 (52.2) | 0.621 | 0.358 |
| 44 | 93 (46.0) | 0.494 | 0.445 |
| 45 | 71 (60.2) | 0.619 | 0.341 |
| 46 | 131 (64.5) | 0.637 | 0.208 |
| 47 | 91 (46.4) | 0.415 | 0.507 |
| 48 | 174 (84.1) | 0.698 | 0.268 |
| 49 | 183 (89.7) | 0.632 | 0.153 |
| 50 | 157 (76.6) | 0.569 | 0.081 |
| 51 | 44 (22.1) | 0.306 | 0.467 |
| 52 | 195 (96.1) | 0.806 | −0.037 |
| 53 | 195 (95.6) | 0.967 | 0.015 |
| 54 | 167 (81.9) | 0.460 | 0.092 |
| 55 | 176 (87.6) | 0.651 | −0.038 |
| 56 | 195 (95.1) | 0.784 | 0.095 |
Note: Total of participants may not add 211 in each item due to the non-applicable response option. The items included in the dimension focusing on infant-centered needs are presented at bold.
To compose the Short Form Inventory, all the items with ceiling effect (more than 90% of participants answered “very important”) were eliminated, which corresponded to items 1, 5, 14, 35, 38, 39, 40, 52, 53, and 56 of the original scale (Table 3). According to the Spearman–Brown prediction formula, 10 and 12 items were included in the dimensions focusing on parents-centered needs and infant-centered needs, respectively. The items with a better fit within dimension 1 were selected, taking into account the item-fit statistics for the Rasch model (Appendix 1).
Presentation of the items composing the Portuguese Short Version of the Neonatal Intensive Care Unit (NICU) Family Needs Inventory.
| Item numberShort Version | Item numberNICU Family Needs Inventory | Previous subscale | Short-Form dimension |
|---|---|---|---|
| 1 | 3 | Proximity | Infant-centered needs |
| 2 | 4 | Information | Infant-centered needs |
| 3 | 8 | Comfort | Parents-centered needs |
| 4 | 11 | Information | Infant-centered needs |
| 5 | 13 | Information | Infant-centered needs |
| 6 | 15 | Support | Parents-centered needs |
| 7 | 16 | Information | Infant-centered needs |
| 8 | 19 | Support | Parents-centered needs |
| 9 | 20 | Information | Infant-centered needs |
| 10 | 21 | Comfort | Parents-centered needs |
| 11 | 22 | Support | Parents-centered needs |
| 12 | 24 | Comfort | Parents-centered needs |
| 13 | 25 | Comfort | Infant-centered needs |
| 14 | 27 | Support | Infant-centered needs |
| 15 | 29 | Proximity | Infant-centered needs |
| 16 | 31 | Support | Parents-centered needs |
| 17 | 32 | Comfort | Infant-centered needs |
| 18 | 33 | Information | Parents-centered needs |
| 19 | 36 | Information | Infant-centered needs |
| 20 | 47 | Support | Parents-centered needs |
| 21 | 50 | Assurance | Infant-centered needs |
| 22 | 51 | Support | Parents-centered needs |
Confirmatory factor analysis supported that both dimensions were reflected in the Short Form version of the Inventory (Fig. 1). Overall, the Short Form NICU Family Needs Inventory showed a high degree of reliability, with a Cronbach's alpha of 0.77 for the parents-centered needs dimension and 0.76 for the infant-centered needs dimension. A significant correlation was observed between the two dimensions, indicating a considerable dependence between the subscales. The CFI, TLI, and RMSEA values obtained from confirmatory factor analysis indicated an adequate goodness of fit in this study sample (X2 (50)=643.690; CFI=0.925; TLI=0.950; RMSEA=0.053).
The five subscales of the original Inventory (assurance, proximity, information, comfort, and support) were reorganized within the two new dimensions obtained in the Short Form version. Support and comfort needs were mainly included in the parents-centered needs subscale, while information, assurance, and proximity were predominantly included in the infant-centered needs subscale (Table 3).
Associations between each subscale of the Short Version score with socio-demographic and obstetric characteristics of the participants are presented in Table 1. Parents of infants hospitalized in NICU classified, on average, the infant-centered needs subscale as more important than the parents-centered needs subscale (mean (SD): 8.6 (2.4) [range: 0–12]; 3.5 (2.6) [range: 0–10], respectively). Overall, a high concordance was observed in the perception of needs between couples for the infant-centered needs subscale (35.0%), while the concordance regarding the parents-centered needs subscale was much lower (14.3%).
Parents with more than 34 years of age and with less than ten years of education were significantly more likely to attribute a higher importance to the subscale focusing on the parents’ needs than those younger and more educated (mean (SD): 3.3 (2.3) vs. 4.1 (3.0), p=0.037; mean (SD): 4.3 (2.5) vs. 3.1 (2.5), p<0.001). Also, parents of multiples revealed a significant tendency to value infant-centered needs, in comparison with those without a multiple pregnancy (mean (SD): 9.4 (2.8) vs. 8.3 (2.7), p=0.024).
DiscussionIn the present study, the authors propose a Short Form of the NICU Family Needs Inventory, a brief and valid instrument for the Portuguese population. It is composed by 22 items divided into two subscales, one focusing on parents-centered needs and another on infant-centered needs. The Short Form Inventory presented a high degree of reliability to assess the parental needs of parents during their child's hospitalization in NICU, and had a high internal consistency in both dimensions. Also, an adequate goodness of fit ensured that the model fit the data analyzed well.
Overall, all items of the Short Form of the Inventory were highly valued by the parents, underlining the relevance of those issues for the design of parent-friendly NICU settings and highlighting the importance of family-centered care in such a context.11 In fact, previous studies concluded that, during the hospitalization period, parents face particular infant-centered needs, such as need of information,6,8 assurance,9,10 and proximity6 that intertwine with their own needs of comfort10 and social support.9,10 Access to accurate and consistent information, the need to trust in the healthcare team, as well as, assuming responsibility for the infant, by comforting, visiting, breastfeeding, bathing, diapering, and touching the child, increase parents’ sense of control and empowerment, contributing to their involvement in infant's health and care by focusing on their child.21,22 At the same time, establishing genuine relationships with the staff, relying on their partner for physical help and emotional support, making the environment more homelike, and the possibility of accommodation at bedside improve parents’ satisfaction with the healthcare23 and contribute for their health and well-being by focusing on their own needs.24,25
The four categories of response of the original instrument (not important, slightly important, important and very important) must be included in the Short Form administration sheet, in order to allow a higher variability of responses and a better discrimination of the parental perception of needs in NICU. However, this proposal suggests the dichotomization of the scores into not very important and very important for purposes of data analysis, which facilitates the interpretation of the results.
This is, to the best of the authors’ knowledge, the only reliable and valid instrument available to evaluate parental needs during infants’ hospitalization in NICU and there is no gold standard for this construct. Therefore, criterion validity was not assessed in the present study, since it was not possible to compare the results with an existing instrument or an external and objective measure of the construct.26 The strategy implemented for assessing construct validity consisted in measuring the association of each dimension score with socio-demographic and obstetric characteristics of the participants. The authors concluded that older and less educated parents were significantly more likely to attribute higher importance to parents-centered needs, suggesting the re-entrenchment of social inequalities inside NICU. It highlights how social factors, namely socioeconomic position, impact on valuing parental needs during hospitalization of their infants.
Also, mothers attributed higher importance to both parents and infant needs, although not reaching statistical significance. These results were expected since mothers frequently take over the care of the child during hospitalization.9 In fact, the idea of intensive motherhood, in which mothering is exclusive, wholly child centered, emotionally involving, and time consuming,27 is reinforced in NICU. The assumption that mothers, more than fathers, should be devoted to child care and self-sacrifice,28 through the naturalization and devaluation of the pain and suffering during hospitalization, might have justified the predominance of infant-centered needs over parents-centered needs. These results emphasize the previously described focus on infants’ health and prognosis over the fulfillment of parents’ needs.29
A major strength of this study is the proposal of a brief and easy to administrate instrument, simple to score and to interpret. Although most of parents have time available to answer to the full inventory, this does not mean that they have the emotional availability to do so. A very preterm delivery and hospitalization in NICU leads to an emotional chaos in which parents frequently report feelings of fear, sadness, guilt, or failure.5 Considering parents’ emotional availability is particularly relevant in a context where healthcare professionals and researchers must act according to fundamental ethical principles, including the minimization of the burden and the decrease of the intrusion into the private lives of parents of children hospitalized in NICU. Therefore, the Short Form of the Inventory can contribute to increase parental participation and to minimize the burden, while allowing for the identification and inclusion of family needs in healthcare, taking into account essential ethical principles.15
Some limitations of the present study should be acknowledged and discussed. Although the sample size was relatively small for a factor analysis, it has been argued that the increase in precision gained from sample sizes over 50 is rarely worth the effort.30 Also, data were collected from all level III NICU located in the North of Portugal, and the proportion of refusals was very low, ensuring the representativeness of the sample.
The Short Form Inventory demonstrated good psychometric properties. However, further studies comparing the performance of the instrument with the original one, according to the parents’ socio-demographic characteristics and reproductive and obstetric history, as well as to infants’ characteristics at birth and prognosis, are needed. Furthermore, it is important to determine its robustness and reliability in different cultural, economic, and political contexts.
In conclusion, the Short Form of the NICU Family Needs Inventory is a valid and reliable instrument to measure parents-centered and infant-centered needs, by combining the five subscales of the original Inventory. This shorter version of the Inventory, valid for the Portuguese population, is brief and easy to administrate.
FundingThis study was partially based upon a work supported by European Regional Development Fund (ERDF) funding from the Operational Programme Factors of Competitiveness (COMPETE) within the project “Parenting roles and knowledge in neonatal intensive care units” (FCOMP-01-0124-FEDER-019902), and by national funding from the Foundation for Science and Technology (Portuguese Ministry of Education and Science) and by the grants IF/00956/2013 (to SS), SFRH/BPD/103562/2014 (to EA), and PD/BD/105830/2014 (to MA).
Conflicts of interestThe authors declare no conflicts of interest.
The authors thank all participants and health professionals of the seven Neonatal Care Units where the study was conducted, for their collaboration and assistance during participants’ recruitment.
Please cite this article as: Alves E, Severo M, Amorim M, Grande C, Silva S. A short form of the neonatal intensive care unit family needs inventory. J Pediatr (Rio J). 2016;92:73–80.
Study conducted at Instituto de Saúde Pública, Universidade do Porto (ISPUP), Porto, Portugal.