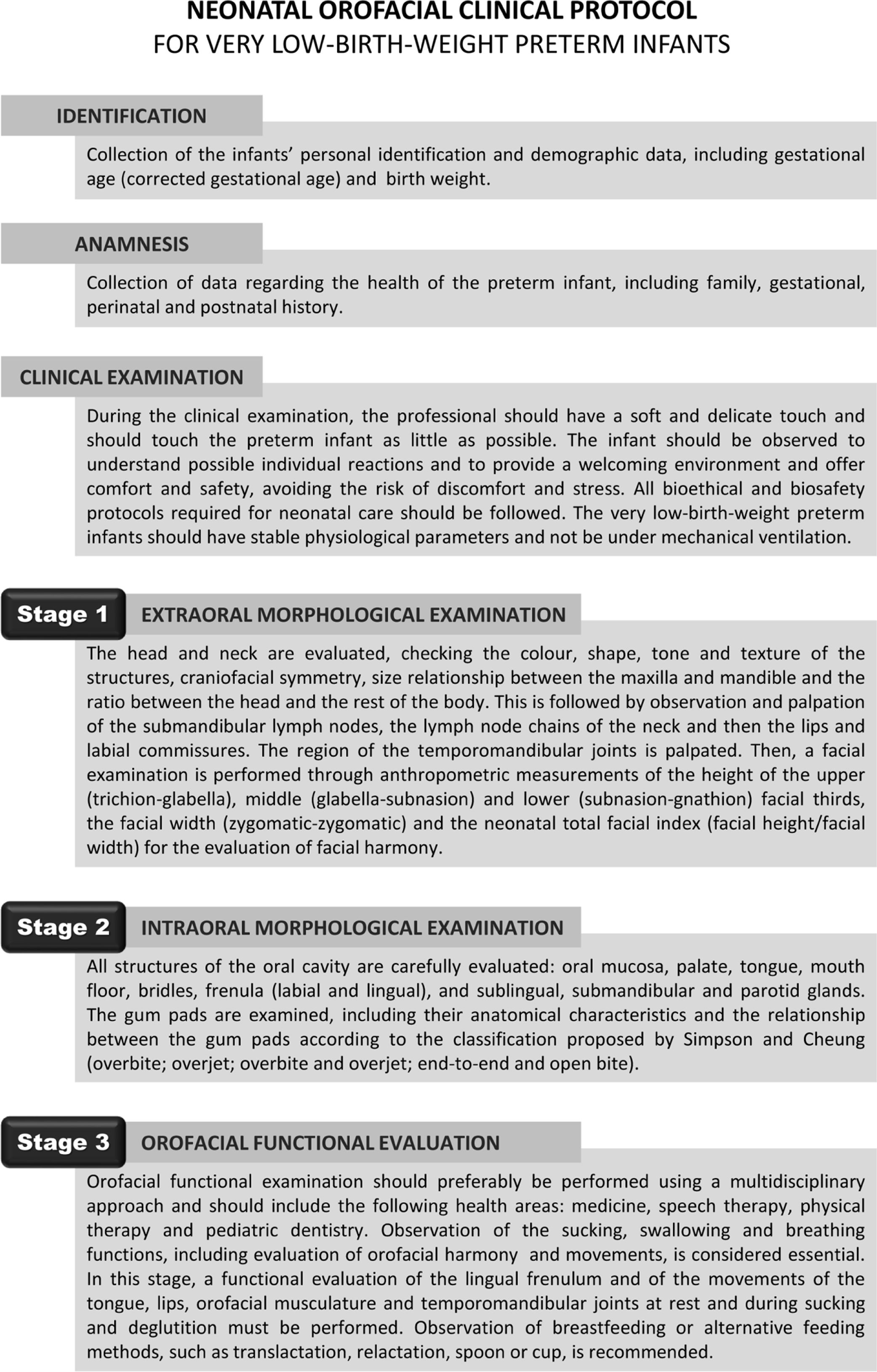
To evaluate the orofacial characteristics of very low-birth-weight preterm infants through anthropometric facial measures, orofacial anteroposterior analysis and the relationship between the gum pads.
MethodOrofacial examinations was performed in 154 infants, classified into two groups: Group A comprised 54 very low-birth-weight infants who were examined after clinical stabilization and before hospital discharge, and Group B comprised 100 full-term infants.
ResultsThe average anthropometricmeasurements in millimetres for Group A and Group B were as follows: upper third:30.2 and 31.1; middle third: 24.2 and 25.9; lower third: 27.6 and 29.9; facial width: 64.8and 81.4. Regarding the orofacial anteroposterior analysis, the results showed that in99% of these infants, the mandible was in a retrognathic position relative to the maxilla.Group A and Group B had the following distributions of the relationship between thegum pads: overbite-overjet: 43% and 77%; overjet: 39% and 17%; open bite: 15% and3%; end-to-end: 2% and 1%; overbite: both 2%.
ConclusionThe very low-birth-weight preterm infants showed the upper third with the highest values in the facialharmony analysis, followed by the lower third and the middle third; and exhibited themandible in a retrognathic position relative to the maxilla, and with overbite-overjet themost prevalent type of gum pad relationship. The study emphasizes the importance of orofacial examination during neonatal hospitalization and the investigation of birth weight and gestational age in a multidisciplinary therapeutic approach that includes orofacial neonatal evaluation and actions that promote oral health, besides foster follow-up studies.
Preterm infants are deprived of a period of intense intrauterine growth and development by prematurity itself. Postnatal complications may also occur, particularly during hospitalization in the neonate intensive care unit (NICU), due to weight loss and morbidities soon after birth. Several complications of prematurity have negative effects on health, growth and development throughout childhood, leading to a high overall under-5 mortality rate.1,2 Prematurity may also result in alterations in orofacial growth and development and may cause morphological and functional changes that may lead to sensorimotor dysfunctions in the stomatognathic system, increase the risk of dental enamel hypoplasia, palatal alteration, muscle hypotonia, and impaired quality of sucking, swallowing and breathing; these changes have potential future consequences for oral health and malocclusion.3–6
The World Health Organization considers oral health an indicator of an individual’s general health, well-being and quality of life.7 It is believed that the onset of oral diseases, changes in orofacial growth and malocclusions is usually a gradual process that begins in early childhood, justifying early preventive and interceptive actions that promote oral health and adequately stimulate all structures of the stomatognathic system to favour the harmonious growth and development of the entire orofacial complex. Ideally, these efforts to promote child oral health should begin early and be implemented by pediatricians and pediatric dentists working in an integrated manner and using strategies specific to the needs of preterm infants.8–10
The face and oral cavity should not be neglected during neonatal physical examinations, especially of very low-birth-weight preterm infants, and a neonatal dental examination consisting of an extra and intraoral morphological and functional examination guided by an integrative axis established through dialogue and the exchange of multidisciplinary knowledge must be included to ensure the best, most individualized neonatal care possible. Thus, the present study sought to identify neonatal dental characteristics and non-invasive measures for an accurate neonatal orofacial examination that includes anthropometric facial assessment and assessment of the relationship between the gum pads and to provide guidance for actions that promote oral health.
Individuals and methodsAn observational study was conducted on a sample of 154 children classified into two groups: Group A, consisting of 54 very low-birth-weight preterm infants, and Group B, consisting of 100 full-term infants. The study was approved by the Research Ethics Committee of the School of Medicine of the University and the Ethics Committee of the Clinics Hospital in accordance with all the provisions in Resolution 196/96 of the National Health Council on Guidelines and Norms Regulating Human Research.
The individuals studied were selected from a sample, following all study inclusion and exclusion criteria, where they were part of a consecutive and voluntary population that originated exclusively from a Centre I of the Children’s Institute of the Clinics Hospital. Participants were selected over a 20 months period (October/2016- August/2018) according to the general and oral health inclusion and exclusion criteria. To be included in the study, infants in Group A should have been born preterm and with very low birth weight (≤366/7 gestational weeks and <1,500 g a≥1,000 g,1 have stable physiological parameters and not be under mechanical ventilation; in turn, infants from Group B should have been born at term (≥307 gestational weeks).11 Chronological age was categorized as the actual age of the full-term infant after birth; however, for preterm infants, the corrected gestational age (the age adjusted to reflect the degree of prematurity of a full-term infant born at 40 gestational weeks) was used. Infants with erupted teeth, oral pathologies and malformations, and facial asymmetries and those with confirmed or suspected diagnoses of congenital malformations, genetic syndromes and severe neurological sequelae that could compromise orofacial growth and development (hydrocephalus, microcephaly and facial paralysis) were excluded from the study. The neonatal dental examination was performed by a researcher with specialization in pediatric dentistry. An initial pilot project was carried out with five infants, where anthropometric measurements and gum pads relationship were closed twice for calibration. The Kappa was 0.95 and 1.0 respectively. An intercalibration was performed where every 10 examinations were doubled 1. The Kappa was 0.91 (Group A) and 0,85 (Group B) for anthropometric measurements and 1.0 (Group A) 0.89 (Group B) for gum pads relationship.
The researcher identified the orofacial characteristics, including the facial anthropometric measurements and the relationship between the gum pads. Preventive guidelines related to oral health promotion were provided by the researcher to the family members who participated in this study. In an effort to standardize the anthropometric measurements used in the study, the infants were examined lying down with the head positioned along the Frankfurt vertical plane and the body aligned. The anthropometric landmarks were palpated, and their precise locations were marked with a special pencil. For the anthropometric measurement of the face in the NICU, two instruments were used: (a) sterilizable Willis compass with rounded edges; and (b) Digimess® digital caliper with a capacity of 150 mm and 0.01 mm accuracy for immediate verification of the measurement obtained with the Willis compass. The facial anthropometric measurements were selected based on landmarks, measurements and orofacial anthropometric indices provided in scientific literature.12,13 The facial analysis was performed in two planes: vertical and horizontal. The face was vertically evaluated in three thirds. The upper third (Tr-G) corresponded to measurements between the trichion (Tr) and glabella (G) landmarks; the trichion was considered the point on the hairline, and the glabella was the most prominent midline point between the eyebrows. The middle third (G-Sn) corresponded to measurements between the glabella (G) and subnasion (Sn) landmarks; the subnasion landmark was considered the midpoint of the angle at the columella base, where the lower edge of the nasal septum and the surface of the upper lip meet. The lower third (Sn-Gn) corresponded to measurements between the subnasion (Sn) and gnathion (Gn) landmarks; the gnathion point was considered the lowest midpoint of the lower border of the mandible. The total facial height was considered the sum of the upper, middle and lower thirds (Tr-Gn). The face was horizontally assessed using the distance between the anthropometric landmarks known as zygomatic (Zy), which were considered the most prominent anatomical points of the zygomatic region of the right and left sides of the face (Zy-Zy). The facial proportion was determined by calculating the neonatal total facial index, obtained by the ratio between total facial height and facial width.
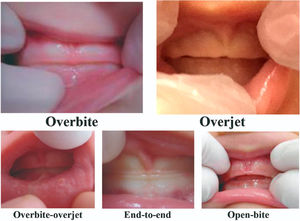
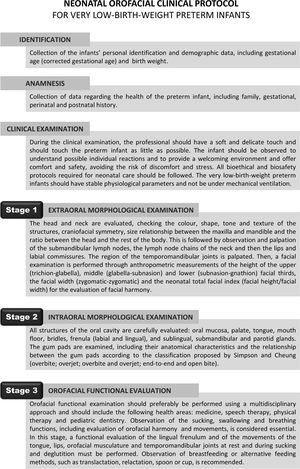
For the clinical evaluation of the relationship between the gum pads, the head of the infant was in a normal resting position. In this study, the relationship between the gum pads was described using the classification of Simpson and Cheung14 and was divided into 5 types (Fig. 1): overbite; overjet (horizontal overlap), overbite-overjet (simultaneous vertical and horizontal overlap), end-to-end (without vertical or horizontal overlap) and open bite (space between the gum pads).
A descriptive statistical analysis of the sample was performed in which the qualitative variables were presented as absolute (n) and relative (%) frequencies and the quantitative variables were presented as the mean, standard deviation, confidence interval and minimum and maximum values. The quantitative variables were analysed by Student’s t-test for normally distributed data. In all analyses, a significance level of 5% (p-value < 0.05) was adopted, and the statistical software Stata 15 was used (StataCorp 2017, Stata Statistical Software: Release 1, College Station, TX: StataCorp LLC).
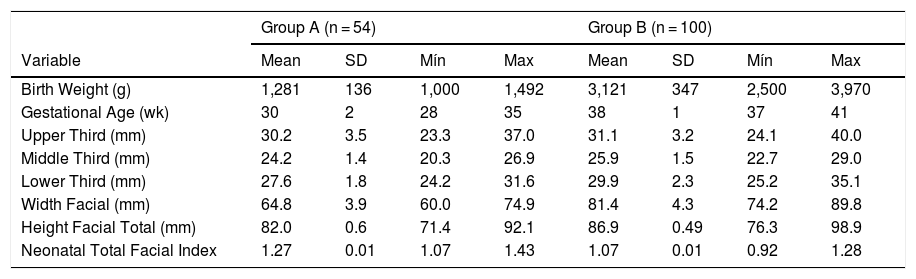
ResultsIn the facial harmony analysis of groups A and B (Table 1), the facial thirds had the same mean ascending sequence of anthropometric values: the upper third had the highest values, followed by the lower third and finally the middle third, which had the lowest values. Group A was examined at 35 (±1) weeks of correct gestational age (minimum 33 and maximum 36 weeks), around 1 month of chronologic age, after stable physiological parameters, and the facial anthropometric analysis showed that the Group A had lower total facial height and facial width and a higher neonatal total facial index (mean: 1.27 and 1.07; p < 0,001 when compared to the Group B at 38 ±1 weeks of gestational age. Regarding the orofacial anteroposterior analysis, the results showed that in 99% of the infants, the mandible was in a retrognathic position relative to the maxilla. The overbite-overjet type of gum pad relationship was the most prevalent in both groups, totalling 65% of the sample (n = 154), but the proportions differed significantly between the two groups (Group A:43%; Group B:77%). The overjet type of relationship was found in 39% of cases in Group A and 17% of Group B, while the open-bite type of relationship was found in 15% of cases in Group A and 3% of Group B. The overbite type of relationship was found in 2% of cases in each Group A and Group B, and the end-to-end type of relationship was found in 2% of cases in Group A and 1% of Group B (Supplementary Table S1). In the Pearson’s chi-square (chi2) test, the relationship between the gum pads was significantly different between Groups A and B, with a p-value of 0.001.
Descriptive characteristics of the groups: very-low-weight preterm infants and full-term infants.
| Group A (n = 54) | Group B (n = 100) | |||||||
|---|---|---|---|---|---|---|---|---|
| Variable | Mean | SD | Mín | Max | Mean | SD | Mín | Max |
| Birth Weight (g) | 1,281 | 136 | 1,000 | 1,492 | 3,121 | 347 | 2,500 | 3,970 |
| Gestational Age (wk) | 30 | 2 | 28 | 35 | 38 | 1 | 37 | 41 |
| Upper Third (mm) | 30.2 | 3.5 | 23.3 | 37.0 | 31.1 | 3.2 | 24.1 | 40.0 |
| Middle Third (mm) | 24.2 | 1.4 | 20.3 | 26.9 | 25.9 | 1.5 | 22.7 | 29.0 |
| Lower Third (mm) | 27.6 | 1.8 | 24.2 | 31.6 | 29.9 | 2.3 | 25.2 | 35.1 |
| Width Facial (mm) | 64.8 | 3.9 | 60.0 | 74.9 | 81.4 | 4.3 | 74.2 | 89.8 |
| Height Facial Total (mm) | 82.0 | 0.6 | 71.4 | 92.1 | 86.9 | 0.49 | 76.3 | 98.9 |
| Neonatal Total Facial Index | 1.27 | 0.01 | 1.07 | 1.43 | 1.07 | 0.01 | 0.92 | 1.28 |
min, minimum; max, maximum; wks, weeks; Test, Student’s t.
Group A, Group of very-low-birth-weight preterm infants.
Group B, Group of full-term newborns.
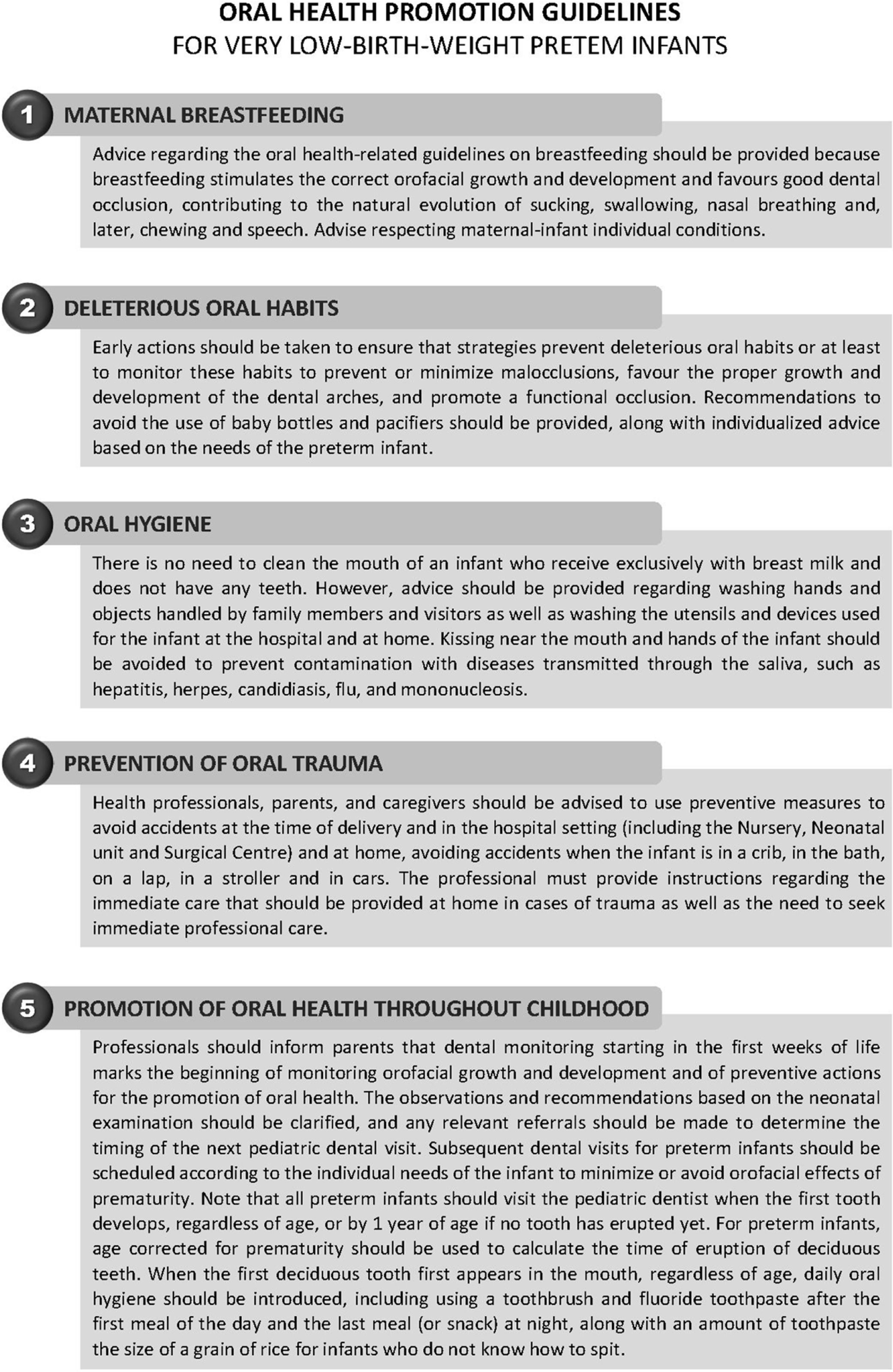
In this study, a neonatal dental clinical protocol was suggested that involved minimal and risk-free intervention for the infant, especially very low-birth-weight preterm infants (Figs. 2 and 3).
DiscussionThe evolution of very low-birth-weight preterm infants is frequently characterized by a series of events that can compromise health, growth, development and quality of life in the perinatal, neonatal and postnatal follow-up periods.1,2 It is assumed that the greater deviations and alterations of orofacial structures, the more compromised the orofacial movements and functions of very low-birth-weight preterm infants may be due to morphological limitations.3–5 Thus, there is a need for health professionals to monitor orofacial growth and development and the possibility of inadequate oral stimulation since birth to intervene as early as possible and re-establish correct orofacial physiology using a multiprofessional neonatal therapeutic approach.
Facial anthropometric studies warn that although infants can have differing facial types, there is an average pattern of facial harmony throughout the population; in addition, when considering what is a normal anthropometric facial pattern, one must also consider the potential influence of racial factors on the diversity of facial shape in infants.15–18 For this reason, it is necessary to determine the normal range of facial parameters for each population.
Groups A and B had significantly different gestational ages and birth weights (Table 1). Even when the corrected gestational age for Group A was used, there are still three weeks of difference between the groups, and especially the groups were characterized by completely different perinatal and postnatal stimuli and conditions that can interfere with neonatal health and growth and development. Therefore, the objective of this study was to determine reference values for the facial proportions of full-term infants to provide a better understanding of the characteristics and needs of very low-birth-weight preterm infants in the population studied.
In the assessment of facial proportion, a higher neonatal total facial index was observed for Group A compared to Group B. Clinically, this finding could reveal differences in facial growth proportion between the total facial length and width between the Groups A and B in the neonatal period, before the age adjusted to reflect the degree of prematurity of a full-term infant born at 40 gestational weeks, which is considered the zero mark for full-term birth for Group A. This finding is relevant for further research questions in neonatal in terms of the differential diagnosis between a normal facial pattern from the still intrauterine period and a pattern of orofacial alterations in very low-birth-weight preterm births. However, the scarcity of studies on neonatal facial assessment, as well as the lack of assessment of the facial thirds and the total facial index in very low-birth-weight preterm infants and full-term infants, makes it difficult to compare the results of this study.
It is noteworthy that in childhood, there is considerable vertical facial growth that occurs mainly in the middle and lower thirds of the face.19 This fact most likely explains why the proportions of the facial thirds in childhood may be different from the proportions in adulthood. At the same time, in childhood, the growth and development of the middle and lower thirds may be influenced by oral and nasal functions. Due to prematurity, and depending on the comorbidities present, changes in the posture and muscle tone of very low-birth-weight preterm infants may occur that may hinder or prevent the proper positioning of the head and neck and correct sucking, swallowing, nasal breathing and movements of the lips, tongue and the orofacial musculature.3 These consequences of prematurity may increase the risk of effects on the growth and development of the facial thirds in preterm infants.
In the analysis of the orofacial profiles of Groups A and B, the results showed that in almost all the studied children, the mandible was in a retrognathic position relative to the maxilla. These results confirmed the findings in infants observed by Simpson and Cheung,14 Clinch,20 Flinck et al.,21 Almeida et al.22 and Dinis et al.23 Considering these results, there is a consensus in classic and contemporary studies on the intermaxillary relationship, which showed a higher prevalence of the retrognathic position of the mandible relative to the maxilla. Clinch20 reported that this retrognathic mandibular position relative to the maxilla at birth is a striking feature at birth and may originate from the ventral position of the foetus in the amniotic cavity.
In the evaluation of the relationship between the gum pads in the edentulous oral cavity, overbite-overjet was the type of relationship most frequently observed in both Group A and Group B (Supplementary Table S1); however, there were significant differences between the study groups. A comparison of studies using the same relationship classification method showed that the results of the present study are similar to the findings of Simpson and Cheung14 for full-term infants and those of Almeida et al.22 for preterm infants of unspecified gestational age and birth weight. However, there was a greater occurrence of overjet-overbite in Group B of the present study than in full-term infants in the study of Simpson and Cheung,14 and conversely, a lower occurrence of overjet-overbite in Group A in the present study compared to the preterm infants in Almeida et al.22 Studies of infants by Clinch,20 Flinck et al.21 and Dinis et al.23 did not use the methodology proposed by Simpson and Cheung,14 preventing a comparison of the results. Simpson and Cheung14 described the overbite-overjet type relationship between the gum pads as a natural condition at birth. Thus, the opposing surfaces of the gum pads, which overlap slightly in the vertical and horizontal plane (overbite-overjet), provide a more efficient way for milk extraction during breastfeeding.24 It is noteworthy that Group A showed a significantly higher prevalence of overjet and open bite when compared to the group of full-term infants, in contrast to the findings of Almeida et al.,22 who did not find open-bite and overjet in preterm infants and concluded that there was no significant difference in the type of relationship between the gum pads of preterm infants compared to data from the literature on full-term infants. There are no reports on the relationship between the gum pads in a specific sample of very low-birth-weight preterm infants for adequate comparison of the results of the current study. Furthermore, there is no consensus in the literature on the impact of the relationship between the gum pads in the edentulous oral cavity on future deciduous dentition.
An interesting fact about the facial growth of individuals aged between 2 and 32 years who were born preterm was observed in the study by Van Erum et al.,25 who traced lateral cephalograms (teleradiographs) to analyse craniofacial growth and showed mandibular retrognathism with increased facial height, resulting in a divergent facial pattern (long face). At the same level of importance are the studies by Lian et al.26 that analysed cephalometric tracings on the teleradiographs of individuals aged between 6 and 14 years with obstructive sleep apnoea who were born preterm and at term and stated that preterm infants have a different craniofacial morphology compared to full-term infants, suggesting that preterm infants had a longer vertical mandibular length, indicating a dolichocephalic facial profile (long face). Paulsson and Bondemark,27 who also evaluated cephalometric tracings, reported that several craniofacial parameters differ significantly among children born preterm and at term. On the other hand, regarding dental occlusion in preterm infants, Seow,28 in his review on the effects of preterm birth on oral growth and development, reported a high prevalence of class II occlusion, in which the maxilla is found in a protruding position relative to the mandible (horizontal overlap). However, Harila et al.29 mentioned that preterm infants could have a relatively higher prevalence of and predisposition towards the development of anterior open-bite malocclusion compared to full-term infants. Another noteworthy study is that of Objois and Gebeile-Chauty,6 who reported in an epidemiological clinical study that very premature and extremely premature birth (gestational age ≤32 weeks) represents a risk factor for the need for orthodontic treatment and that therefore, prematurity is a public health problem. The recent study by Maaniitty et al.30 indicates that, in deciduous dentition, the prevalence of dental crowding is higher among children born very premature when compared to term children. These cited studies showed statistically significant differences in orofacial characteristics in preterm compared to full-term children, but, did not show that some characteristics could be observed as early as in the edentulous oral cavity stage. These orofacial examination are crucial and it should be done prior to the hospital discharge, as environmental factors from different household habits may also influence orofacial growth and development and highlight the need for oral health promotion actions that influences the orofacial growth and development for families of premature infants (Figs. 2 and 3). In conclusion, the study emphasizes the importance of orofacial examination during hospitalization (NICU) and the investigation of birth weight and gestational age in a multidisciplinary therapeutic approach that includes orofacial neonatal evaluation and actions that promote oral health, besides foster follow-up studies.
Conflict of interestThe authors declare no conflict of interest.
Please cite this article as: Ruiz DR, Diniz EM, Krebs VL, Carvalho WB. Orofacial characteristics of the very low-birth-weight preterm infants. J Pediatr (Rio J). 2020;97:96–102.