To evaluate mortality in adolescents and young adult patients with chronic diseases followed in a Latin American tertiary hospital.
MethodsA cross-sectional retrospective study was performed in a tertiary/academic hospital in the state of São Paulo, Brazil. Death occurred in 529/2850 (18.5%) adolescents and young adult patients with chronic diseases, and 25/529 (4.7%) were excluded due to incomplete medical charts. Therefore, 504 deaths were evaluated.
ResultsDeaths occurred in 316/504 (63%) of early adolescent patients and in 188/504 (37%) of late adolescent/young adult patients. Further comparisons between early adolescents (n=316) and late adolescent/young adult patients (n=188) with pediatric chronic diseases at the last hospitalization showed that the median disease duration (22.0 [0–173] vs. 43.0 [0–227] months, p<0.001) was significantly lower in early adolescents vs. late adolescent/young adult patients. The median number of previous hospitalizations was significantly lower in the former group (4.0 [1–45] vs. 6.0 [1–52], p<0.001), whereas the last hospitalization in intensive care unit was significantly higher (60% vs. 47%, p=0.003). Regarding supportive measures, palliative care was significantly lower in the younger group compared to the older group (33% vs. 43%, p=0.02). The frequencies of renal replacement therapy (22% vs. 13%, p=0.02), vasoactive agents (65% vs. 54%, p=0.01), and transfusion of blood products (75% vs. 66%, p=0.03) were significantly higher in the younger group. The five most important etiologies of pediatric chronic diseases were: neoplasias (54.2%), hepatic diseases/transplantation (10%), human immunodeficiency virus (5.9%), and childhood-onset systemic lupus erythematosus and juvenile idiopathic arthritis (4.9%). Autopsy was performed in 58/504 (11%), and discordance between clinical and postmortem diagnoses was evidenced in 24/58 (41.3%).
ConclusionsAlmost 20% of deaths occurred in adolescents and young adults with distinct supportive care and severe disease patterns. Discordance between clinical diagnosis and autopsy was frequently observed.
Avaliar a mortalidade entre adolescentes e pacientes adultos jovens com doenças crônicas acompanhados em um hospital terciário na América Latina.
MétodosFoi feito um estudo retrospectivo transversal em um hospital terciário/universitário no Estado de São Paulo, Brasil. Houve mortalidade de 529/2.850(18,5%) pacientes adolescentes e adultos jovens com doenças crônicas, porém 25/529(4,7%) foram excluídos devido a prontuários médicos incompletos. Portanto, foram avaliados 504 óbitos.
ResultadosOcorrem 316/504(63%) óbitos entre pacientes no início da adolescência e 188/504(37%) pacientes no fim da adolescência/adultos jovens. As comparações adicionais entre os pacientes no início da adolescência (n = 316) e no fim da adolescência/pacientes jovens (n = 188) com doenças crônicas pediátricas na última internação mostraram que a duração média da doença [22,0 (0-173) em comparação com 43,0 (0-227) meses, p < 0,001], foi significativamente menor nos pacientes no início da adolescência em comparação com os pacientes no fim da adolescência/adultos jovens. O número médio de internação anterior foi significativamente menor no primeiro grupo [4,0 (1-45) em comparação com 6,0 (1-52), p < 0,001], ao passo que a última internação na unidade de terapia intensiva foi significativamente maior (60% em comparação com 47%, p = 0,003). Com relação a medidas de suporte, o cuidado paliativo foi significativamente menor no grupo de pacientes no início da adolescência em comparação com o grupo de pacientes no fim da adolescência (33% em comparação com 43%, p = 0,02). As frequências de terapia de substituição renal (22% em comparação com 13%, p = 0,02), agentes vasoativos (65% em comparação com 54%, p = 0,01) e transfusão de hemoderivados (75% em comparação a 66%, p = 0,03) foram significativamente maiores no primeiro grupo. As cinco etiologias mais importantes de doenças crônicas pediátricas foram: neoplasias (54,2%), doenças hepáticas/transplante (10%), vírus da imunodeficiência humana (5,9%), lúpus eritematoso sistêmico de início na infância e artrite idiopática juvenil (4,9%). Foi feita autópsia em 58/504 (11%) e a discordância entre os diagnósticos clínico e pós-morte foi comprovada em 24/58 (41,3%).
ConclusõesQuase 20% dos óbitos ocorreram em adolescentes e adultos jovens com diferentes padrões de cuidados de suporte e doenças graves. A discordância entre o diagnóstico clínico e a necropsia foi frequentemente observada.
Chronic illnesses have been growing in recent years, resulting in considerable morbidity.1,2 Children and adolescents with chronic conditions that have survived during childhood need follow-up in inpatient and outpatient clinics.3 These chronic diseases may have new disease flare-ups and disease sequelae, which may require multiple hospitalizations and result in a high mortality rate during adolescence and young adulthood.3–7
A recent study reported that early adolescents with chronic diseases required more appointments, multiple specialties, and more hospital admissions compared to late adolescents/young adults.3 However, there are few studies evaluating death in adolescents with pediatric chronic diseases in tertiary hospitals,5–9 particularly assessing the characteristics of death, causes of death, and autopsy in a large population of deceased adolescent and young adult patients.
Therefore, the objective of this study was to evaluate death in adolescents and young adult patients with chronic diseases followed in a tertiary Latin American hospital. Furthermore, comparisons between demographic data, death characteristics, and pediatric specialties in early and late adolescence and young adulthood were performed, as well as assessment of discrepancies between clinical and autopsy diagnoses.
MethodsFrom January 2000 to December 2015, a cross-sectional study based on retrospective chart review was performed regarding death in adolescents and young adult patients with chronic diseases followed at Children's Hospital of Hospital das Clínicas da Faculdade de Medicina, Universidade de São Paulo, São Paulo state, Brazil. Inclusion criteria were patients with chronic diseases, aged from 10 to 20 years. The exclusion criterion was incomplete medical charts. The Ethics Committee of the University Hospital approved this study.
Chronic illnesses were classified as those with over three months of duration. The diagnosis of pediatric chronic disease was established according to valid methods, standardized tools, or diagnostic classification criteria.3,10 Pediatric specialties were divided into: allergy & immunology, cardiology, endocrinology, gastroenterology, genetics, hematology, hematopoietic cell transplantation, hepatology, infectious diseases, nephrology/renal transplantation, neurology, nutrition, oncology, palliative and pain care, pediatric surgery/liver transplantation, pneumology, psychiatry, and rheumatology.
The data of the last hospitalization were systematically reviewed through the medical records. Demographic data included: age at death, gender, place of residence, and disease duration. Characteristics of the last and previous hospitalizations evaluated the following variables: number of previous hospitalizations, duration and location of last hospitalization at pediatric intensive care units (PICU), emergency room, pediatric wards, operating rooms, and others. Medical interventions included assessment of: palliative care, surgical procedures, renal replacement therapy, antibiotic and antifungal use, vasoactive agents, albumin use, blood products use, respiratory support, central catheterization, and non-resuscitation order.
Death certificates were also evaluated. Death registration in Brazil is in compliance with the International Form of Medical Certificate of Cause of Death, according to World Health Organization.11 The present study evaluated the death certificates according to immediate cause of death (final disease or condition resulting in death) and underlying cause of death (disease or injury that initiated the events resulting in death).
Permission to perform an autopsy was requested from the families. Autopsy certificate and premortem clinical and laboratorial diagnoses were also revised. Disagreements between the autopsy certificate and premortem clinical and laboratorial diagnoses were classified according to modified Goldman criteria.8,9,12,13 Class I error included major misdiagnoses (if it had been known before death, possibly required change of therapy, and could have improved survival or cure). Class II diagnostic error was defined as major unexpected findings whose detection before death possibly would not require a change in therapy or change the patient's survival with chronic disease because the patient had already been treated appropriately for the missed condition, or no efficacious therapy was available at that time, or it was too late to introduce effective treatment to change the outcome. Class III comprised diseases that were related to the terminal process but not directly associated with death, and which detection before death did not require a change in therapy and consequently to the outcome. Class IV comprised relevant diagnoses unrelated to the cause of death that could have influenced the outcome if properly diagnosed and treated. Class V was defined as the absence of unexpected findings.
Patients with chronic diseases were divided in two groups: early (10–14 years) and late adolescent/young adult patients (15–20 years).
Statistical analysisThe results for continuous variables were presented as median (range) or mean±standard deviation. The results for categorical variables were presented as frequency and percentage. For categorical variables, analysis of 2×2 and 3×2 contingency tables were performed and compared using Fisher's exact test. For 3×2 contingency tables using Fisher's exact test, a post-hoc analysis by 2×2 chi-squared test was also assessed to determine where the difference occurred between the groups. Additional analysis of 3×4 contingency tables was carried-out using chi-squared test to assess differences between medical records, death certificate, and autopsies. The comparisons between median (range) were performed by the Mann–Whitney or Kruskal–Wallis test, and mean±standard deviation by Student's t-test, as appropriate. Values of p<0.05 were considered statistically significant.
ResultsIn this period, death occurred in 2850 newborns, children, adolescents and young patients. Of them, deaths occurred in 529/2850 (18.5%) adolescents and young patients with chronic diseases. Of note, 25/529 (4.7%) patients were excluded due to incomplete medical charts. Therefore, 504 deaths were evaluated. Death certificate was available in 428/504 (85%) patients and the five leading immediate causes of death for these patients were: respiratory failure, n=142/428 (33.2%); sepsis/septic shock, n=82/428 (19.1%); multiple organ dysfunction syndrome, n=53/428 (12.3%); intracranial hypertension, n=24/429 (5.6%); and neoplasia, n=17/428 (3.9%). The three leading underlying causes of death for these patients were: neoplasia, n=115/428 (26.8%); pneumonia, n=47/428 (10.9%); and sepsis/septic shock, n=44/428 (10.3%).
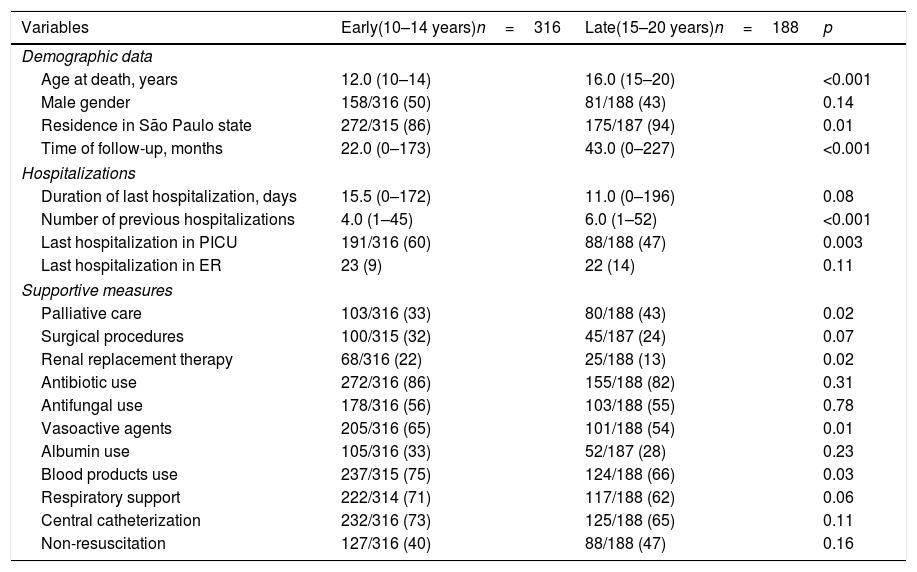
Deaths occurred in 316/504 (63%) of early adolescents and in 188/504 (37%) of late adolescent/young adult patients. Further comparisons between early adolescents (n=316) and late adolescent/young adult patients (n=188) with pediatric chronic diseases at the last hospitalization showed that the median time of follow-up (22.0 (0–173) vs. 43.0 [0–227] months, p<0.001) was significantly lower in early adolescents vs. late adolescent/young adult patients. The median number of previous hospitalizations was significantly lower in the former group (4.0 [1–45] vs. 6.0 [1–52], p<0.001), whereas the last hospitalization with a stay in PICU was significantly higher (60% vs. 47%, p=0.003) (Table 1).
Demographic data and characteristics of death comparisons of 504 early adolescent and late adolescent/young adult patients with pediatric chronic diseases at their last hospitalization in a Latin America university hospital over a period of 16 consecutive years.
| Variables | Early(10–14 years)n=316 | Late(15–20 years)n=188 | p |
|---|---|---|---|
| Demographic data | |||
| Age at death, years | 12.0 (10–14) | 16.0 (15–20) | <0.001 |
| Male gender | 158/316 (50) | 81/188 (43) | 0.14 |
| Residence in São Paulo state | 272/315 (86) | 175/187 (94) | 0.01 |
| Time of follow-up, months | 22.0 (0–173) | 43.0 (0–227) | <0.001 |
| Hospitalizations | |||
| Duration of last hospitalization, days | 15.5 (0–172) | 11.0 (0–196) | 0.08 |
| Number of previous hospitalizations | 4.0 (1–45) | 6.0 (1–52) | <0.001 |
| Last hospitalization in PICU | 191/316 (60) | 88/188 (47) | 0.003 |
| Last hospitalization in ER | 23 (9) | 22 (14) | 0.11 |
| Supportive measures | |||
| Palliative care | 103/316 (33) | 80/188 (43) | 0.02 |
| Surgical procedures | 100/315 (32) | 45/187 (24) | 0.07 |
| Renal replacement therapy | 68/316 (22) | 25/188 (13) | 0.02 |
| Antibiotic use | 272/316 (86) | 155/188 (82) | 0.31 |
| Antifungal use | 178/316 (56) | 103/188 (55) | 0.78 |
| Vasoactive agents | 205/316 (65) | 101/188 (54) | 0.01 |
| Albumin use | 105/316 (33) | 52/187 (28) | 0.23 |
| Blood products use | 237/315 (75) | 124/188 (66) | 0.03 |
| Respiratory support | 222/314 (71) | 117/188 (62) | 0.06 |
| Central catheterization | 232/316 (73) | 125/188 (65) | 0.11 |
| Non-resuscitation | 127/316 (40) | 88/188 (47) | 0.16 |
PICU, pediatric intensive care unit; ER, emergency room.
Results are presented as n (%), median (range).
Regarding medical interventions, palliative care was significantly lower in early adolescents compared to late adolescent/young adult patients (33% vs. 43%, p=0.02), and this intervention increased in the last eight years in the present university hospital. The frequencies of renal replacement therapy (22% vs. 13%, p=0.02), vasoactive agents (65% vs. 54%, p=0.01), and blood product transfusions (75% vs. 66%, p=0.03) were significantly higher in the former group (Table 1).
The five most important etiologies of pediatric chronic diseases were: neoplasia (54.2%), hepatic diseases and liver transplantation (10%), HIV (5.9%), childhood-onset systemic lupus erythematosus, and juvenile idiopathic arthritis (4.9%). The majority of HIV patients (60%) died before 2004. The five leading pediatric specialties associated to death in adolescent and young adult patients with chronic diseases were: oncology (n=273/504, 54.2%), pediatric surgery and liver transplantation (n=33/504, 6.5%), infectious diseases (n=30/504, 5.9%), hepatology (n=27/504, 5.3%), and rheumatology (n=25/504, 4.9%).
Further comparisons were performed between HIV death/HIV prevalence in three periods: 2000–2005, 2006–2010, and 2011–2015. A decrease of HIV mortality/HIV prevalence was significantly observed between these three specific time cutoffs (19/74 25.5% vs. 10/95 [10.5%] vs. 2/83 [2.4%], p=0.00003).
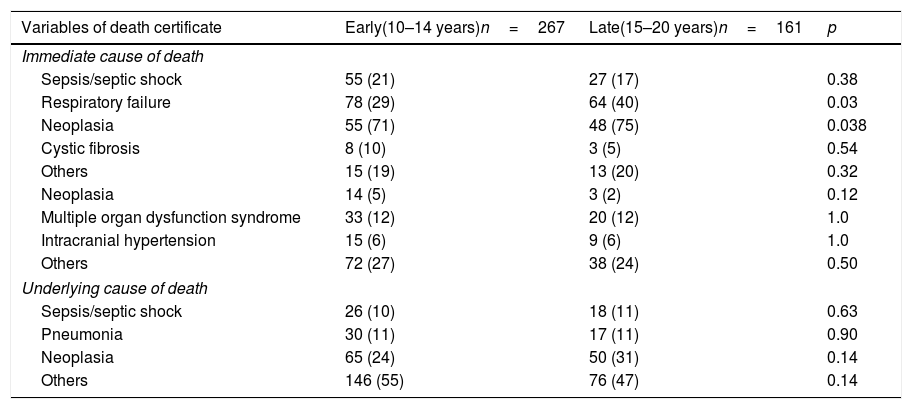
Death certificates were available in 428/504 (85%) patients. Table 2 shows causes of death according to death certificates revealed that respiratory failure, as immediate cause of death, was significantly lower in early adolescents compared to late adolescent/young adult patients (29% vs. 40%, p=0.03), particularly in patients with neoplasia (71% vs. 75%, p=0.038). No differences were observed between the others immediate causes of death and the underlying causes of death in both groups (p>0.05, Table 2).
Cause of death comparisons between 428 early adolescent and late adolescent/young adult patients with pediatric chronic diseases at their last hospitalization in a Latin America university hospital over a period of 16 consecutive years.
| Variables of death certificate | Early(10–14 years)n=267 | Late(15–20 years)n=161 | p |
|---|---|---|---|
| Immediate cause of death | |||
| Sepsis/septic shock | 55 (21) | 27 (17) | 0.38 |
| Respiratory failure | 78 (29) | 64 (40) | 0.03 |
| Neoplasia | 55 (71) | 48 (75) | 0.038 |
| Cystic fibrosis | 8 (10) | 3 (5) | 0.54 |
| Others | 15 (19) | 13 (20) | 0.32 |
| Neoplasia | 14 (5) | 3 (2) | 0.12 |
| Multiple organ dysfunction syndrome | 33 (12) | 20 (12) | 1.0 |
| Intracranial hypertension | 15 (6) | 9 (6) | 1.0 |
| Others | 72 (27) | 38 (24) | 0.50 |
| Underlying cause of death | |||
| Sepsis/septic shock | 26 (10) | 18 (11) | 0.63 |
| Pneumonia | 30 (11) | 17 (11) | 0.90 |
| Neoplasia | 65 (24) | 50 (31) | 0.14 |
| Others | 146 (55) | 76 (47) | 0.14 |
Results are presented as n (%).
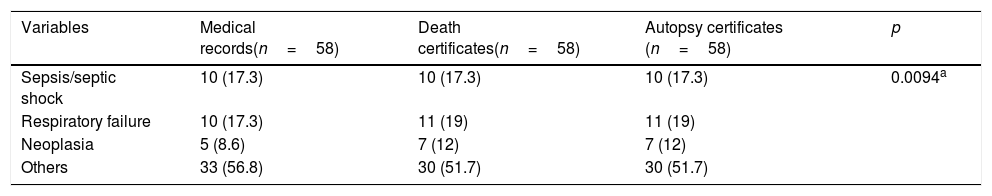
Autopsy certificates were available in 58/504 (11%) patients. According to modified Goldman criteria, complete concordance (class V) between clinical and postmortem diagnoses was evidenced in 34/58 (58.6%) patients. Discrepancies were observed in 24/58 (41.3%): 3/58 (5.2%) had a class I discrepancy, 6/58 (10.3%) had a class III discrepancy, and 15/58 (25.9%) had a class IV discrepancy. Among the autopsies classified as I, cavernous sinus thrombosis was identified exclusively at autopsy in one acute lymphoblastic leukemia patient. Non-cardiogenic pulmonary edema associated with acute kidney injury was solely diagnosed in the other acute lymphoblastic leukemia patient. Fungal infection (invasive aspergillosis) was observed exclusively at autopsy in one childhood-onset systemic lupus erythematosus patient.
Table 3 includes immediate cause of death according to medical records, death certificates, and autopsy certificates in patients with pediatric chronic diseases at their last hospitalization in a Latin America university hospital for a period of 16 consecutive years. No differences were observed between these three groups (p=0.994, Table 3).
Immediate cause of death according to medical records, death certificates, and autopsy certificates in patients with pediatric chronic diseases at their last hospitalization in a Latin America university hospital over a period of 16 consecutive years.
| Variables | Medical records(n=58) | Death certificates(n=58) | Autopsy certificates (n=58) | p |
|---|---|---|---|---|
| Sepsis/septic shock | 10 (17.3) | 10 (17.3) | 10 (17.3) | 0.0094a |
| Respiratory failure | 10 (17.3) | 11 (19) | 11 (19) | |
| Neoplasia | 5 (8.6) | 7 (12) | 7 (12) | |
| Others | 33 (56.8) | 30 (51.7) | 30 (51.7) |
To the best of the authors’ knowledge, this study evaluated the largest death population in adolescent and young adult patients with chronic diseases followed-up in a Latin American university hospital.
The advantages of this study were the inclusion of a large death population, using a definition for pediatric chronic conditions,3,10 and evaluation of discordance between clinical and postmortem diagnoses.8,9,12,13 This quaternary care medical center serves as a reference center for children and adolescents, especially those with chronic illnesses.3,14–22
In the present study, almost two-thirds of deaths occurred in early adolescents. Indeed, these patients had high PICU hospitalizations, and required more vasoactive agents, blood product transfusions, and renal replacement therapy, reflecting that this younger population had more severe conditions. Acute kidney injury is well-known risk factor for mortality in early and late adolescents23 and young adults.24
Additionally, it was identified that late adolescent and young adult patients had longer disease duration and a higher number of previous hospitalizations. This finding was also described for young adults with chronic disease, since the rate of hospital admission was associated with the mortality rate.4 The high frequency of palliative care in this group may be related to malignancies. In this university hospital, palliative care intervention for pediatric chronic conditions has been systematically carried-out over the last eight years.
The majority of etiologies of chronic diseases associated with death were severe conditions with unpredictable course, particularly neoplasia, liver conditions, HIV, and autoimmune diseases. Cancer also had the highest rate of admission in adolescents and young adults with chronic diseases, as the primary diagnosis in a tertiary hospital in Spain.4 Importantly, the survival of HIV patients in Brazil has improved in recent years using an efficient program with highly active anti-retroviral therapy for all patients,19 and the majority of deaths were observed before this established program, as observed herein.
Another important point about the etiologies of pediatric chronic diseases was the high prevalence of hepatic diseases and liver transplantation. This is due to the specific situation of this tertiary hospital, since it is a reference center for the most serious hepatic diseases in Brazil, mainly related to acute liver failure.25
According to death certificate, the most relevant immediate causes of death were respiratory failure and sepsis/septic shock, mainly in patients with chronic infections and immunosuppressive conditions. These cause of death were also reported in other studies with immunosuppressed chronic disease patients during hospitalization in PICUs and emergency rooms.4,18–22
The vast majority of the present study's patients were residents of São Paulo State, particularly the late adolescent and young adult patients. This patient migration to this university hospital may be related to the lack of comprehensive pediatric health care centers closer to their homes.
Autopsy was relevant to identify events that had not been clarified or that were uncertain at the time of death.8,9,12 In the present study, autopsy showed infectious disease, cardiovascular events, and thrombotic events not diagnosed previously; it was important to determine undetected or doubtful causes of death and should always be considered. The rate of autopsy performance was only 11%. Autopsy rates have decreased in recent years, and this finding may be related to the high number of this institution's patients with severe chronic diseases and long-term follow-up, as well as parental refusal based on religious or ethical beliefs.
This study had limitations due to retrospective design and possible missing data. A high prevalence of hepatic disease was also a selection bias. The site of infection and the microbiologic etiology of sepsis were not assessed. This institution's care system may not be representative of all tertiary hospitals in Latin America.
In conclusion, almost 20% of deaths occurred in adolescents and young adults with specialized patterns of supportive care and severe diseases. Discrepancy between the clinical diagnosis and autopsy was observed in 40% of patients.
FundingThis study was supported by grants from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq 303422/2015-7 to CAS), the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP 2015/03756-4 to CAS), the Federico Foundation, Switzerland (to CAS), and by the Núcleo de Apoio à Pesquisa “Saúde da Criança e do Adolescente” da USP (NAP-CriAd) to MCS and CAS.
Conflicts of interestThe authors declare no conflicts of interest.
The authors wish to express gratitude to all the physicians of pediatric specialties that followed-up children and adolescents with chronic diseases at this university hospital. They also thank the pathologists that evaluated the autopsies of these patients over the last 16 years.
Please cite this article as: Ramos GF, Ribeiro VP, Mercadante MP, Ribeiro MP, Delgado AF, Farhat SC, et al. Mortality in adolescents and young adults with chronic diseases during 16 years: a study in a Latin American tertiary hospital. J Pediatr (Rio J). 2019;95:667–73.