Maternal depression and anxiety have been found to negatively affect fetal and neonatal growth. However, the independent effects of maternal depression and anxiety on fetal-neonatal growth outcomes and trajectories remain unclear. This study aimed to analyze simultaneously the effects of maternal prenatal depression and anxiety on (1) neonatal growth outcomes, and (2), on fetal-neonatal growth trajectories, from the 2nd trimester of pregnancy to childbirth.
MethodsA sample of 172 women was recruited and completed self-reported measures of depression and anxiety during the 2nd and 3rd trimesters of pregnancy, and at childbirth. Fetal and neonatal biometrical data were collected from clinical reports at the same assessment moments.
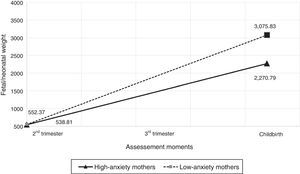
ResultsNeonates of prenatally anxious mothers showed lower weight (p=0.006), length (p=0.025), and ponderal index (p=0.049) at birth than neonates of prenatally non-anxious mothers. Moreover, fetuses-neonates of high-anxiety mothers showed a lower increase of weight from the 2nd trimester of pregnancy to childbirth than fetuses-neonates of low-anxiety mothers (p<0.001). Considering maternal depression and anxiety simultaneously, only the effect of maternal anxiety was found on these markers of fetal-neonatal growth outcomes and trajectories.
ConclusionThis study demonstrates the independent longitudinal effect of maternal anxiety on major markers of fetal-neonatal growth outcomes and trajectories, simultaneously considering the effect of maternal depression and anxiety.
Foi constatado que a depressão e ansiedade materna afetam negativamente o crescimento fetal e neonatal. Contudo, o efeito independente da depressão e ansiedade materna sobre os resultados e as trajetórias de crescimento fetal e neonatal continua incerto. Este estudo visou analisar simultaneamente o efeito da depressão e ansiedade materna pré-natal (1) sobre os resultados de crescimento neonatal e (2) sobre as trajetórias do crescimento fetal-neonatal a partir do 2° trimestre de gravidez até o parto.
MétodosUma amostra de 172 mulheres foi recrutada e as mesmas relataram graus de depressão e ansiedade no 2° e 3° trimestre de gravidez e parto. Os dados biométricos fetais e neonatais foram coletados dos prontuários clínicos nas mesmas ondas de avaliação.
ResultadosOs neonatos de mães ansiosas no período pré-natal mostraram menor peso (p=0.006), comprimento (p=0.025) e índice ponderal (p=0.049) no nascimento que os neonatos de mães não ansiosas no período pré-natal. Além disso, os neonatos de mães muito ansiosas mostraram um menor aumento de peso do 2° trimestre de gravidez até o parto que os fetos-neonatos de mães pouco ansiosas (p<0.001). Considerando simultaneamente a depressão e a ansiedade maternal, apenas o efeito da ansiedade materna foi constatado nesses marcadores de resultados e trajetórias de crescimento fetal-neonatal.
ConclusãoEste estudo demonstra o efeito longitudinal independente da ansiedade materna sobre os principais marcadores de resultados e trajetórias de crescimento fetal-neonatal, considerando simultaneamente o efeito da depressão e ansiedade materna.
The short-term consequences of prenatal depression and anxiety on pregnant women's physical health include obstetric complications and physical symptoms, which are both associated with lower fetal and neonatal growth and lower autonomic nervous system (ANS) maturation.1,2 Depression and anxiety share a common genetic pathway, and often appear simultaneously, making it difficult to assess their independent effects. Thus, when analyzing the effects of maternal depression and anxiety, it may be important to consider both simultaneously, in order to control their mutual effects and to better identify the independent effect of each one.3
Various studies have found similar effects of maternal prenatal depression and anxiety on fetal growth, behavior, and ANS maturation. Both fetuses of depressed and anxious mothers were found to present lower estimated weight and higher total fetal activity.4–6 In addition, studies have found that both fetuses of depressed or anxious mothers show higher heart rate reactivity compared with fetuses of non-depressed or non-anxious mothers.2,7–10
Moreover, studies also have found similar effects of maternal prenatal depression and anxiety on neonatal growth, behavioral, and maturation outcomes. Both neonates of prenatally depressed or anxious mothers presented higher risk of premature birth and low weight, both major problems of infant health.11–13 Neonates of depressed or anxious mothers were found to present disorganized sleep patterns and frequent changes of mood.2 Lower maturation was also found in neonates of prenatally depressed or anxious mothers, including less vagal tonus, and lower neurobehavioral maturity.2,11,13,14 Furthermore, both neonates of prenatally depressed or anxious mothers were found to show higher levels of cortisol and lower levels of dopamine and serotonin when compared with hormonal levels of neonates of prenatally non-depressed or non-anxious mothers.15 Other studies also reported that both infants of prenatally depressed or anxious mothers present increased admission rates to the neonatal care unit and growth retardation during the first year of life.16,17
Few studies have simultaneously considered maternal depression and anxiety when analyzing the effect on fetal/neonatal growth and behavior. When simultaneously considering maternal depression and anxiety, studies only found an independent effect of maternal anxiety on fetal/neonatal growth and behavior.18–20 One cross-sectional study only found an effect of maternal anxiety on fetal growth and behavior (fetuses of anxious mothers presented lower estimated weight and higher activity at mid-pregnancy).18 Additionally, two longitudinal studies only found an effect of maternal anxiety on fetal-neonatal growth trajectories (higher maternal anxiety during pregnancy was associated with lower increase of fetal-neonatal weight).19,20 However, these studies only included one assessment of maternal prenatal depression and anxiety (during pregnancy) when analyzing their effect on fetal/neonatal growth, not addressing the longitudinal effect of both maternal depression and anxiety.
Both maternal depression and anxiety were found to negatively affect fetal and neonatal growth. Despite these effects having been widely documented in literature, the independent effects of maternal depression and anxiety on fetal-neonatal growth outcomes and trajectories remain unclear. Moreover, there is a lack of studies that have simultaneously addressed the independent longitudinal effect of maternal depression and anxiety on fetal-neonatal growth trajectories. This study aimed to simultaneously analyze the effect of maternal prenatal depression and anxiety on (1) neonatal outcomes, and (2), on fetal-neonatal growth trajectories, from the 2nd trimester of pregnancy to childbirth.
MethodParticipantsThe sample was comprised of 172 mothers recruited at a public health service in Northern Portugal during the 1st trimester of pregnancy (8–14 gestational weeks). Inclusion criteria were: able to read and write in Portuguese; resident in Portugal for at least one year; at most 14 weeks pregnant; and, singleton gestations without medical and/or obstetric complications. From the 172 mothers who completed the 1st moment of assessment, 88.4% (n=152) completed all the three moments of assessment.
ProceduresThis study was conducted in accordance with the Declaration of Helsinki and was previously approved by the ethics committees of all institutions involved. Women willing to participate provided written informed consent, after an explanation of the study aims and procedures. This study had a longitudinal design with three assessment moments: 2nd trimester of pregnancy (20–24 gestational weeks), 3rd trimester of pregnancy (30–34 gestational weeks), and childbirth (1–3 postnatal days). Mothers repeatedly completed a measure of depression and anxiety. Obstetric records and fetal and neonatal biometrical data were collected from clinical reports during the 2nd and 3rd trimester of pregnancy, and at childbirth. To avoid potential errors associated with estimated age, gestational age was estimated based on mothers’ last menstrual period and confirmed using ultrasound measurements.
MeasuresSocio-demographic and obstetric information was obtained using a socio-demographic questionnaire. To assess maternal depression, the Portuguese version of the Edinburgh Postnatal Depression Scale (EPDS)21,22 was used. The EPDS is a self-reported scale composed of ten items on a four-point Likert scale. A cutoff point of 10 was suggested to screen for depression in Portuguese women.22 Several studies have used this scale in women during pregnancy and the postnatal period.18–20 The Portuguese version of the EPDS showed good internal consistency in women during pregnancy and the postnatal period (α=0.85).18,22 In the present study, Cronbach's alpha coefficients ranged from 0.84 to 0.85.
To assess maternal anxiety, the Portuguese version of the State-Trait Anxiety Inventory (STAI)23,24 was used. The STAI is composed of two subscales: one to assess anxiety as an emotional state (STAI-S) and another to assess the trait of anxiety (STAI-T), each containing 20 items scored on a four-point Likert scale. A cutoff point of 45 was suggested to screen for high anxiety in Portuguese women.24 Several studies have used this measure in women during pregnancy and the postnatal period.18,19 The Portuguese version of the STAI-S showed good internal consistency in women during pregnancy and the postnatal period (α ranged from 0.87 to 0.93).24 In the present sample, Cronbach's alpha coefficients of STAI-S ranged from 0.89 to 0.93.
To assess fetal growth, estimated fetal weight (measured in grams) was obtained from the obstetric ultrasounds at the 2nd and 3rd trimesters of pregnancy. These measures were obtained following a standard clinical measurement protocol by an obstetrician from the research team. Estimated fetal weight was calculated using the Hadlock formula.25
To assess neonatal growth outcomes, neonatal weight, length (measured in centimeters), ponderal index (100×[weight/length3]), and gestational age at birth (measured in weeks) were collected from medical reports. These measures were suggested by previous research as major markers of fetal-neonatal growth and outcomes.18–20
Data analysis strategyTo simultaneously analyze the effect of maternal prenatal depression and anxiety on neonatal outcomes, a two-way multivariate analysis of covariance (MANCOVA) was performed. In the model, maternal prenatal depression and anxiety (mean of the scores at the 2nd and 3rd trimester of pregnancy; coded as 0=EPDS<10 and 1=EPDS≥10 for depression; 0=STAI-S<45 and 1=STAI-S≥45 for anxiety) were included as independent variables and neonatal growth outcomes (weight, length, ponderal index, and gestational age at birth) as dependent variables. The mother's weight before pregnancy and tobacco and coffee consumption during pregnancy were included as covariates. The two-way MANCOVA was performed using SPSS (IBM Corp; SPSS Statistics for Windows, version 23.0. USA). The effect size, measured as partial eta squared (ηp2), was presented for the two-way MANCOVA results.
To simultaneously analyze the effects of maternal depression and anxiety on fetal-neonatal growth trajectories, growth curve models (GCM) were estimated using multilevel modeling. Time 0 was defined as the date of the first assessment during the 2nd trimester of pregnancy (baseline) and the time variable was scored in weeks since the baseline until the childbirth. Scale scores for fetal-neonatal weight, maternal depressive (EPDS scores), and anxiety symptoms (STAI-S scores) were examined at each assessment moment. Fixed effects for maternal depressive and anxiety symptoms (time-varying effects centered on their grand means) were included in the model. Two different models were performed (the unconditional model and the model with predictors). The mother's weight before pregnancy and tobacco and coffee consumption during pregnancy were included as covariates. Significant interactions were interpreted and graphed using one standard deviation above and below the grand mean of the predictor variables as high and low values. A deviance difference test was performed between the unconditional model and the model with predictors to examine model fit improvements. GCMs were performed in a pairwise person-period dataset using SPSS version 23.0 (SPSS Inc., United States). The resulting data consisted of 516 potential observations (172 participants by three time points). The effect size r was estimated for all significant effects.
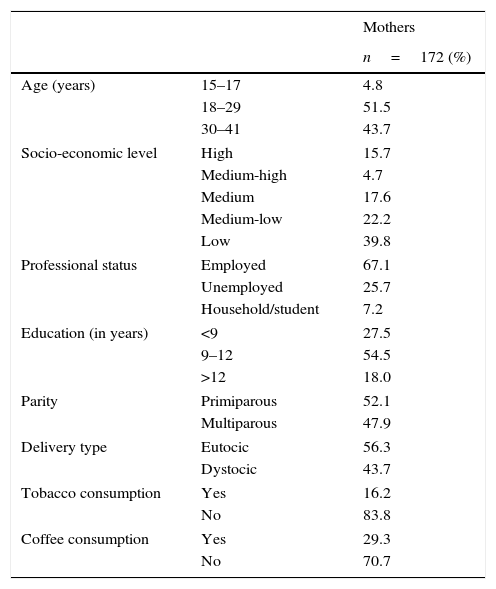
ResultsNearly all the mothers were Portuguese (92.1%), white (94.8%), married or cohabiting (86.8%), and living with a partner (86.2%). More than half were aged between 18 and 29 years old (M=27.69, SD=5.82), were of medium-low or low socio-economic level (62.0%), were employed (67.1%), and had between nine and 12 years of education (54.5%). Additionally, more than a half of the mothers were primiparous (52.1%) and had an eutocic delivery (with or without epidural; 56.3%). The majority reported no tobacco consumption during pregnancy (83.8%), more than a half reported no coffee consumption (70.7%), and all reported no alcohol and drug consumption during pregnancy.
More than a half of the neonates were males (56.3%) and born with a length ≥50cm (63.5%). The majority were not reanimated at birth (94.0%), born with a weight between 2500 and 4199g (91.0%), a ponderal index ≥2.50 (81.2%), a gestational age at birth of ≥37 weeks (95.8%), and had an Apgar score between 7 and 10 at the 1st (92.6%) and 5th minute (98.8%), respectively (Table 1).
Mothers’ obstetric and socio-demographic characteristics and neonates’ biometric data.
| Mothers | ||
|---|---|---|
| n=172 (%) | ||
| Age (years) | 15–17 | 4.8 |
| 18–29 | 51.5 | |
| 30–41 | 43.7 | |
| Socio-economic level | High | 15.7 |
| Medium-high | 4.7 | |
| Medium | 17.6 | |
| Medium-low | 22.2 | |
| Low | 39.8 | |
| Professional status | Employed | 67.1 |
| Unemployed | 25.7 | |
| Household/student | 7.2 | |
| Education (in years) | <9 | 27.5 |
| 9–12 | 54.5 | |
| >12 | 18.0 | |
| Parity | Primiparous | 52.1 |
| Multiparous | 47.9 | |
| Delivery type | Eutocic | 56.3 |
| Dystocic | 43.7 | |
| Tobacco consumption | Yes | 16.2 |
| No | 83.8 | |
| Coffee consumption | Yes | 29.3 |
| No | 70.7 | |
| Neonates | ||
|---|---|---|
| n=168 (%) | ||
| Sex | Male | 56.3 |
| Female | 43.7 | |
| Reanimation | Yes | 6.0 |
| No | 94.0 | |
| Weight (g) | <2500 | 6.6 |
| 2500–4199 | 91.0 | |
| ≥4200 | 2.4 | |
| Length (cm) | <50 | 63.5 |
| ≥50 | 36.5 | |
| Ponderal Index | <2.50 | 18.8 |
| ≥2.50 | 81.2 | |
| Gestational age at birth (weeks) | <37 | 4.2 |
| ≥37 | 95.8 | |
No associations and differences were found between the mothers that completed and did not complete the three assessment moments, regarding mothers’ and neonates’ variables.
Additionally, no associations and differences were found between the mothers that completed and did not complete the three assessment moments in all the study variables at each moment of assessment.
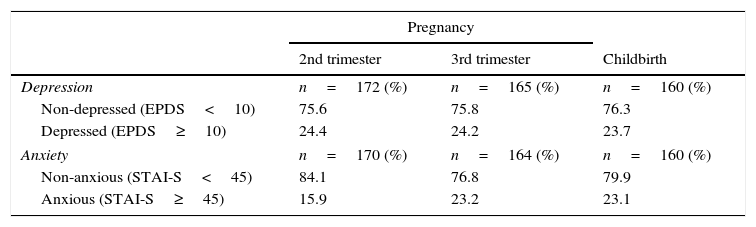
Descriptive statistics for all study variables at each assessment were performed (Table 2). Significant associations were found among the study variables at the baseline (r ranging from −0.289, p<0.05, to 0.652, p<0.001). No association was found between fetal weight and maternal depressive symptoms at the baseline.
Descriptive statistics of study variables across time.
| Pregnancy | |||
|---|---|---|---|
| 2nd trimester | 3rd trimester | Childbirth | |
| Depression | n=172 (%) | n=165 (%) | n=160 (%) |
| Non-depressed (EPDS<10) | 75.6 | 75.8 | 76.3 |
| Depressed (EPDS≥10) | 24.4 | 24.2 | 23.7 |
| Anxiety | n=170 (%) | n=164 (%) | n=160 (%) |
| Non-anxious (STAI-S<45) | 84.1 | 76.8 | 79.9 |
| Anxious (STAI-S≥45) | 15.9 | 23.2 | 23.1 |
| M | SD | M | SD | M | SD | |
|---|---|---|---|---|---|---|
| Fetal/neonatal weight | 417.51 | 120.66 | 1722.36 | 397.96 | 3177.64 | 479.97 |
| Depressive symptoms | 6.78 | 4.38 | 6.48 | 4.39 | 6.17 | 4.84 |
| Anxious symptoms | 36.48 | 8.98 | 37.77 | 10.28 | 36.66 | 10.32 |
M, mean; SD, standard deviation; EPDS, Edinburgh Postnatal Depression Scale; STAI-S, state anxiety inventory.
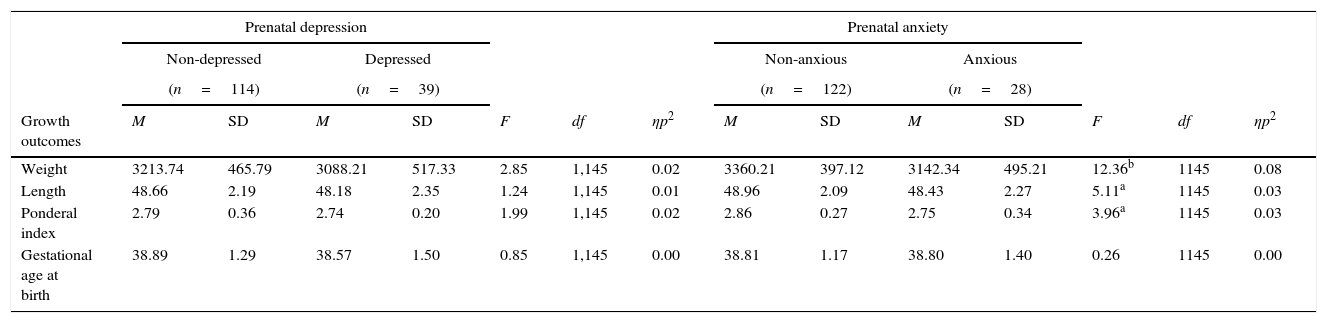
The two-way MANCOVA revealed significant multivariate effects of maternal prenatal anxiety on neonatal growth outcomes, Wilk's Lambda=0.91, F(4,142)=3.29, p=0.013, ηp2=0.09. Results revealed significant univariate effects of prenatal maternal anxiety on neonatal weight, neonatal length, and on neonatal ponderal index. Neonates of prenatally anxious mothers showed lower weight, length, and ponderal index at birth than neonates of prenatally non-anxious mothers. No significant univariate effects of prenatal maternal anxiety were found on neonatal gestational age at birth (Table 3).
The effect of maternal prenatal depression and anxiety on neonatal growth outcomes.
| Prenatal depression | Prenatal anxiety | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-depressed | Depressed | Non-anxious | Anxious | |||||||||||
| (n=114) | (n=39) | (n=122) | (n=28) | |||||||||||
| Growth outcomes | M | SD | M | SD | F | df | ηp2 | M | SD | M | SD | F | df | ηp2 |
| Weight | 3213.74 | 465.79 | 3088.21 | 517.33 | 2.85 | 1,145 | 0.02 | 3360.21 | 397.12 | 3142.34 | 495.21 | 12.36b | 1145 | 0.08 |
| Length | 48.66 | 2.19 | 48.18 | 2.35 | 1.24 | 1,145 | 0.01 | 48.96 | 2.09 | 48.43 | 2.27 | 5.11a | 1145 | 0.03 |
| Ponderal index | 2.79 | 0.36 | 2.74 | 0.20 | 1.99 | 1,145 | 0.02 | 2.86 | 0.27 | 2.75 | 0.34 | 3.96a | 1145 | 0.03 |
| Gestational age at birth | 38.89 | 1.29 | 38.57 | 1.50 | 0.85 | 1,145 | 0.00 | 38.81 | 1.17 | 38.80 | 1.40 | 0.26 | 1145 | 0.00 |
M, mean; SD, standard deviation.
Note: Mother's weight before pregnancy and tobacco and coffee consumption during pregnancy were included as covariates.
No significant multivariate effects of prenatal maternal depression were found on neonatal growth outcomes, Wilk's Lambda=0.95, F(4,142)=1.92, p=0.110, ηp2=0.05.
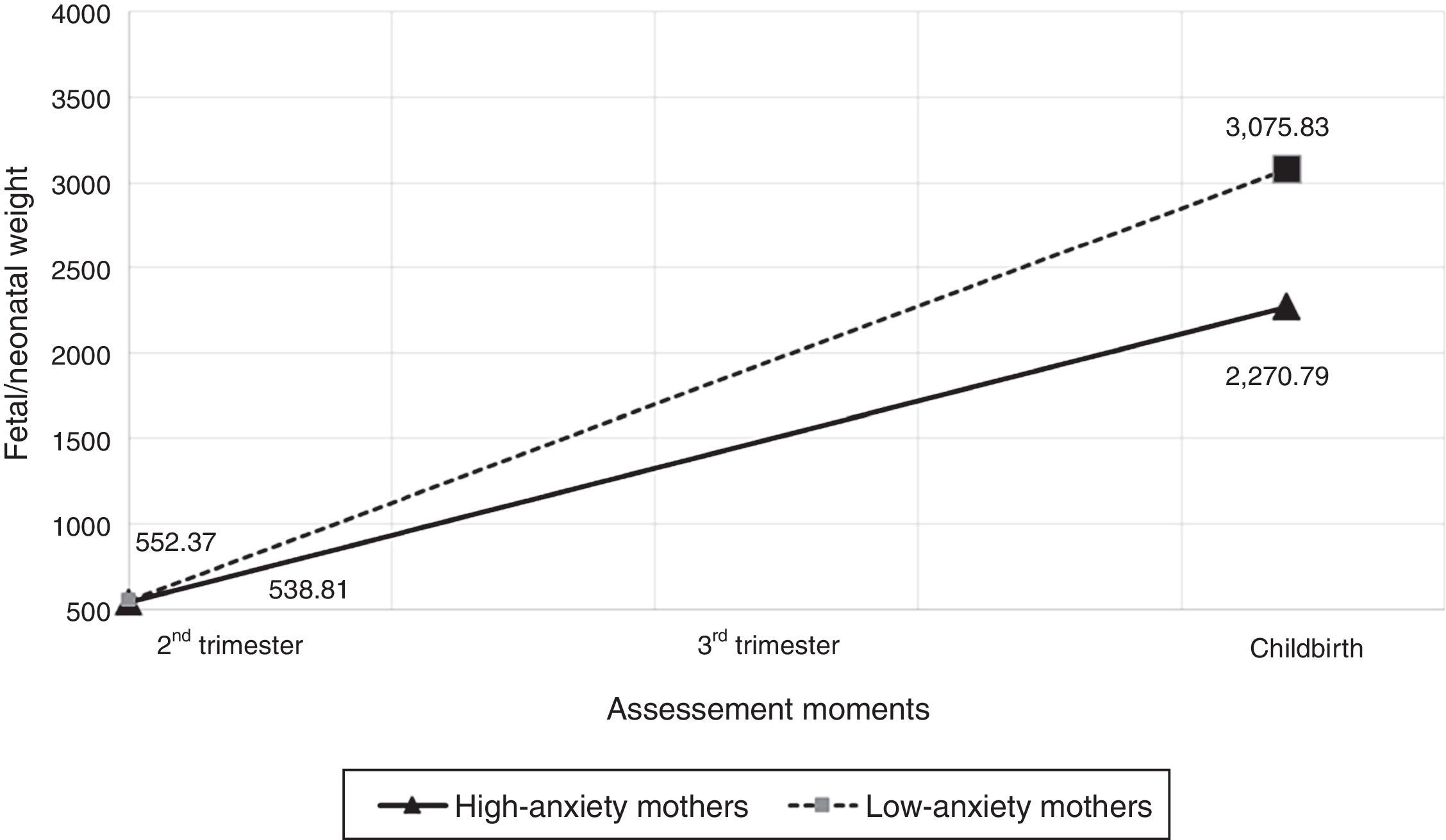
The effects of maternal depression and anxiety on fetal-neonatal growth trajectories, from the 2nd trimester of pregnancy to childbirthThe main effects over time were found on fetal-neonatal weight, b=96.71, SE=1.71, 95% CI=[93.33, 100.08], p<0.001, effect size r=0.95. From the 2nd trimester of pregnancy to childbirth, fetal-neonatal weight increased, on average, 97g per week. Additionally, interaction effects of anxiety symptoms and time were found, b=2.65, SE=0.10, 95% CI=[2.45, 2.86], p<0.001, effect size r=0.86. Fetuses-neonates of high-anxiety mothers showed a lower increase of weight from the 2nd trimester of pregnancy to childbirth than fetuses-neonates of low-anxiety mothers (Fig. 1). No main effects of maternal anxiety symptoms were found on fetal weight.
No main effects of maternal depressive symptoms were found on fetal weight. Likewise, no effects of the interaction between maternal depressive symptoms and time, and no effects of the interaction between maternal depressive symptoms, maternal anxiety symptoms, and time were found. Intercept and random effects (intercept+time; residuals) were statistically significant (all values of p<0.001). The deviance difference test showed that the model with predictors (maternal depressive and anxiety symptoms) provided a good fit to the data, χ2(5)=138.87, p<0.001.
DiscussionSimultaneously considering the effect of maternal prenatal depression and anxiety, a significant independent effect of prenatal maternal anxiety was found on major markers of neonatal growth outcomes. Neonates of prenatally anxious mothers showed lower weight, length, and ponderal index at birth than neonates of prenatally non-anxious mothers. These results are consistent with prior research that found that neonates of anxious mothers were born with lower weight, length, and ponderal index.2 Moreover, simultaneously considering maternal depression and anxiety, a significant interaction effect of maternal anxiety symptoms and time was found on a major marker of fetal-neonatal growth. This result suggested an effect of maternal anxiety symptoms on fetal-neonatal weight trajectories, from the 2nd trimester of pregnancy to childbirth. Fetuses-neonates of anxious mothers showed a lower increase of weight, from the 2nd trimester of pregnancy to childbirth, than fetuses-neonates of non-anxious mothers. These findings suggest that maternal anxiety negatively affect this major marker of normative fetal-neonatal growth trajectories, from the prenatal period to childbirth, even when simultaneously considering the effect of maternal depression. This result is consistent with previous research that found a lower increase of weight in fetuses-neonates of anxious mothers than in fetuses-neonates of non-anxious mothers from pregnancy to childbirth.18,19
Several underlying mechanisms have been suggested to explain the effect of maternal anxiety on fetal-neonatal growth. Epigenetic mechanisms have been proposed as possible mediators of the prenatal anxiety effect on fetal-neonatal growth. Studies have suggested that prenatal anxiety can permanently alter fetal physiology, namely hyperactivation of the fetal hypothalamic pituitary adrenal (HPA) axis.26,27 Literature has also suggested the mother's HPA hyperactivation as a mediator of the maternal prenatal anxiety effect on fetal-neonatal growth.28 Prenatal anxiety could be a stressor for pregnant women, stimulating the HPA-axis to produce higher levels of glucocorticoids. Maternal glucocorticoids can be transduced to the fetus by transplacental transport and by stress-induced release of placental hormones into fetal circulation. Increased fetal cortisol contributes to the maturation of organ systems required for extra-uterine survival. However, excessive levels of feto-placental glucocorticoid may result in intrauterine growth restriction.28 Further, maternal prenatal anxiety has been associated with generally reduced food intake and low intake of essential vitamins and fatty acids (e.g., folic acid, vitamin B12).29
Major concerns about low birth weight, length, and ponderal index emerged due to their negative effect on infant health, associated with higher perinatal mortality: mechanical ventilation, supplemental oxygen support, later oral feeding, retinopathy, bronchopulmonary dysplasia, pneumothorax, intraventricular hemorrhage, and other pediatric complications.30 Moreover, more developmental problems were identified in low birth weight neonates, including problems of attention, cognition, and neuromotor functioning, and increasing the risk of early childhood morbidity.30
Some limitations should be pointed out. The voluntary nature of the participation in the study may have lead to a selection bias. Mothers who agreed to participate and completed all moments of assessment may be those who feel more satisfied and involved with the pregnancy experience. However, no differences were found between the participants who completed and did not complete all the moments of assessment. A higher sample size might increase the statistical power of the analysis. A standardized clinical interview to assess depression and anxiety could increase the validity of the results. However, both measures showed good internal consistency. Unmeasured confounding factors may have influenced the effects described. However, some of these factors (mother's weight before pregnancy, tobacco and coffee consumption during pregnancy) were controlled in the analysis.
This study demonstrates the independent longitudinal effect of maternal anxiety on major markers of fetal-neonatal growth outcomes and trajectories, simultaneously considering the effect of maternal depression and anxiety. This highlights an increased necessity of systematic screening for anxiety during pregnancy. These findings also suggested that fetuses of anxious mothers are those who might benefit from individualized care in neonatal care units.
Suggestions to future research can be indicated. Future studies could simultaneously explore the independent effects of both maternal depression and anxiety on other markers of fetal-neonatal growth, behavior, and maturation. Future research could also explore the mediator role of epigenetic and endophenotypic mechanisms on the effect of maternal prenatal anxiety on fetal-neonatal growth outcomes and trajectories.
Conflicts of interestThe authors declare no conflicts of interest.
This study was conducted at the Psychology Research Center (UID/PSI/01662/2013), University of Minho, and supported by the Portuguese Foundation for Science and Technology and the Portuguese Ministry of Education and Science through national funds and co-financed by FEDER through COMPETE2020 under the PT2020 Partnership Agreement (POCI-01-0145-FEDER-007653). This study was also supported by FEDER Funds through the Programa Operacional Factores de Competitividade – COMPETE and by National Funds through FCT – Fundação para a Ciência e a Tecnologia under the project PTDC/SAU/SAP/116738/2010.
Please cite this article as: Pinto TM, Caldas F, Nogueira-Silva C, Figueiredo B. Maternal depression and anxiety and fetal-neonatal growth. J Pediatr (Rio J). 2017;93:452–9.