To characterize a sample of Brazilian patients with maple syrup urine disease (MSUD) diagnosed between 1992 and 2011.
MethodsIn this retrospective study, patients were identified through a national reference laboratory for the diagnosis of MSUD and through contact with other medical genetics services across Brazil. Data were collected by means of a chart review.
ResultsEighty-three patients from 75 families were enrolled in the study (median age, 3 years; interquartile range [IQR], 0.57–7). Median age at onset of symptoms was 10 days (IQR 5–30), whereas median age at diagnosis was 60 days (IQR 29–240, p=0.001). Only three (3.6%) patients were diagnosed before the onset of clinical manifestations. A comparison between patients with (n=12) and without (n=71) an early diagnosis shows that early diagnosis is associated with the presence of positive family history and decreased prevalence of clinical manifestations at the time of diagnosis, but not with a better outcome. Overall, 98.8% of patients have some psychomotor or neurodevelopmental delay.
ConclusionIn Brazil, patients with MSUD are usually diagnosed late and exhibit neurological involvement and poor survival even with early diagnosis. We suggest that specific public policies for diagnosis and treatment of MSUD should be developed and implemented in the country.
Caracterizar uma amostra de pacientes brasileiros com a doença da urina de xarope de bordo (DXB) diagnosticados entre 1992 e 2011.
MétodosNeste estudo retrospectivo, os pacientes foram identificados por meio de um laboratório de referência nacional para o diagnóstico de DXB e por meio do contato com outros serviços de genética médica no Brasil. Os dados foram coletados por meio de uma revisão de prontuários.
Resultados83 pacientes de 75 famílias foram incluídos no estudo (idade média: 3 anos; intervalo interquartil (IQR): 0,57-7). A idade média no surgimento dos sintomas era de 10 dias (IQR: 5-30), ao passo que a idade média no diagnóstico era de 60 dias (IQR: 29-240; p=0,001). Somente três (3,6%) pacientes foram diagnosticados antes do surgimento de manifestações clínicas. Uma comparação entre pacientes com (n=12) e sem (n=71) um diagnóstico precoce mostra que o diagnóstico precoce está associado à presença de histórico familiar positivo e à redução na prevalência de manifestações clínicas no momento do diagnóstico, porém sem melhor resultado. Em geral, 98,8% dos pacientes têm algum atraso no desenvolvimento psicomotor ou neurológico.
ConclusãoNo Brasil, os pacientes com DXB normalmente recebem um diagnóstico tardio e exibem um envolvimento neurológico e baixa sobrevivência, mesmo com um diagnóstico precoce. Sugerimos que políticas públicas específicas para o diagnóstico e tratamento da DXB sejam desenvolvidas e implementadas no país.
Maple syrup urine disease (MSUD) is an autosomal recessive genetic disorder caused by deficient activity of the branched-chain alpha-keto acid dehydrogenase complex (BCKDC). Deficiency of this enzyme complex leads to high levels of the branched-chain amino acids (BCAA) leucine, valine, and isoleucine. Leucine and its keto analog 2-oxoisocaproic acid are particularly toxic to the central nervous system (CNS). Although the incidence of MSUD worldwide is usually estimated as being 1:185,000 newborns (NB),1 data retrieved from newborn screening suggest this rate can be higher; in Germany, for instance, the incidence is estimated at 1:133,000 NB,2 and in some Mennonite and Pennsylvania Dutch communities in the United States, it may be as high as 1 in 200 live births.3
Neonatal screening by tandem mass spectrometry (MS/MS), also known as expanded newborn screening, enables diagnosis of MSUD while the patient is still asymptomatic, as well as early treatment onset–two essential factors in improving the clinical course.3 Before the introduction of expanded newborn screening, the severe form (classical MSUD) was believed to account for 75-80% of cases,4 but recent data suggest the milder forms of MSUD can account for up to 50% of diagnosed cases.5 In the classical form, symptoms first occur between the 4th and 7th day of life, and often include respiratory changes, encephalopathy, a characteristic odor, seizures, and coma.6 In the acute phase, prompt, aggressive treatment to reduce leucine levels is required, which should consist of a high-rate glucose infusion to stimulate insulin secretion and suppress protein catabolism. If this fails, invasive interventions such as peritoneal dialysis, hemodiafiltration or hemodialysis may be required. During the maintenance phase, treatment usually consists of dietary BCAA restriction and supplementation with thiamine and a BCAA-free formula,6–8 although liver transplantation is a good alternative.9–11
The Brazilian Public Newborn Screening Program was implemented in 2001 and does not include screening for MSUD. The BCAA-free formula, a high-cost product, is not provided by the public Brazilian Unified Health System (Sistema Único de Saúde, SUS). Furthermore, the laboratory tests required for diagnosis of this condition are also not provided through the SUS, and are only available at a few select university centers or private medical laboratories. Regarding liver transplantation, there is no coordinated countrywide network aiming to improve liver transplantation conditions for patients with metabolic disorders. Finally, there are no data on the prevalence of this disease in Brazil.
The objective of this study was to outline the profile of Brazilian patients with MSUD from 1992 to 2011 so as to contribute to the consolidation of specific public policies for MSUD in the country.
MethodsThis retrospective, multicenter, longitudinal study was approved by the local Institutional Review Board.
Patients were identified from the records of the Inborn Errors of Metabolism Laboratory of the Medical Genetics Service, a university-based service that serves as a nationwide referral center for the diagnosis and treatment of inborn errors of metabolism, and from the records of the Inborn Errors of Metabolism Hotline (Serviço de Informações sobre Erros Inatos do Metabolismo - SIEM) run by the same Medical Genetics Service.12 This laboratory probably accounts for most MSUD diagnoses made in the country; the necessary workup is provided at no cost to the patient or referring physician, and is usually covered by research funding. Quantitation of BCAAs by high-performance liquid chromatography (HPLC) and urine organic acid analysis have been available at the laboratory since 1994; automatic amino acid analysis and MS/MS are also currently available, but alloisoleucine detection is no longer performed. The SIEM is a toll-free telephone hotline, established in 2001, that provides information to physicians and other healthcare providers involved in the diagnosis and treatment of patients with suspected or confirmed IEMs.
To be included in the study, a patient should present: 1) a significant increase in blood BCAA levels, on more than one measurement, as determined by a gold-standard method (HPLC-based BCAA quantitation or automatic amino acid analyzer or MS/MS); and 2) a biochemically confirmed diagnosis of MSUD, established between 1992 and 2011.
Data collection forms were filled out for each patient by their attending physician or one of the study investigators by means of a review of available patient records and charts. For deceased patients, the date of the last available record was considered the date of study enrollment.
Definition of study variablesDiagnosis was considered “early” if the patient had been diagnosed before the 15th day of life. The duration of disease until diagnosis was defined as the time elapsed between the onset of clinical manifestations and the biochemical diagnosis of MSUD. Presence and severity of psychomotor and neurodevelopmental delay were assessed on the basis of the impressions of each patient's attending neurologist or pediatrician. MSUD was classified into variants according to the criteria usually cited in the literature.1
Statistical analysisAll statistical analyses were carried out in the Statistical Package for the Social Sciences (SPSS®, Statistics for Windows, Chicago, USA) 18.0 software environment. Variables were only taken into account for analysis if data were available for at least 60% of the sample.
For descriptive analysis, data were expressed as absolute and relative frequencies. Asymmetrically distributed continuous variables were expressed as medians and interquartile ranges. The chi-square test and Fisher's exact test were used to determine associations between categorical variables. The Kruskal–Wallis and Mann–Whitney U tests were used to compare the medians of different characteristics. The significance level was set at 5%.
ResultsOne hundred and nineteen patients with clinical or laboratory evidence of MSUD (“potential MSUD” patients) were identified, 83 of whom met the inclusion criteria. Of these, 48 were alive at the time of the study, 20 died before the start of the study, and 15 lacked information regarding survival.
The patients enrolled in the study came from all five regions of Brazil. The median age at inclusion was 3 years (IQR 0.57–7.00 years; range, 30 days–23 years). Forty-six (55.4%) were male, 75 (90.4%) were unrelated and 14 (18.7%) had a family history of MSUD. Consanguinity was reported in 17 families (22.7%).
DiagnosisThe median age at diagnosis was 60 days (IQR 29–240 days; range, 7 days–10 years). The median leucine level at diagnosis was 1,693μmol/L (IQR 965–2,836μmol/L; reference range, 80–200μmol/L).
Eighty patients (96.4%) had clinical manifestations of MSUD at the time of diagnosis (median age at symptom onset, 10 days; IQR 5–30 days; range, 1 day–2 years). The most common manifestations were seizures (51.2%) and hypoactivity (50%). Other presenting symptoms included poor feeding, poor sucking and changes in respiratory pattern (48.7% each), hypotonia (48.2%), characteristic odor (42.5%), lethargy (41.2%), metabolic acidosis (31.2%), vomiting (30.0%), and encephalopathy (20.0%). The characteristic odor of MSUD was reported by health care providers as a strong, “soy sauce-like,” “caramel-like,” or sweet scent, which was most detectable in patients hospitalized due to metabolic decompensation. There was a statistically significant difference between median age at symptom onset and median age at diagnosis (p=0.001).
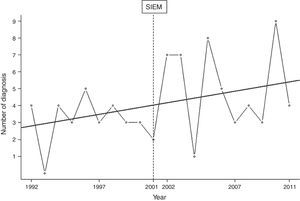
Fig. 1 shows the distribution of the number of diagnoses per year, revealing an upward trend in diagnoses over the course of the study period. However, comparison of median age at diagnosis between 1992 and 2001 (90 days; IQR 36–270; n=31) and between 2002 and 2011 (53 days; IQR 20–202; n=52) revealed no statistically significant difference (p=0.053). The median time elapsed between symptom onset and diagnosis was 60 days (IQR 28–240) over the first decade of the study and 37 days (IQR 9–180) during the second decade (p=0.075). Considering all MSUD patients who were alive as of 2011 (n=48), 13 had been diagnosed between 1992 and 2001 and 35 between 2002 and 2011.
Only 12 patients had been diagnosed early. In three of these cases, diagnosis was made before symptom onset as a result of neonatal screening at a private laboratory; at the time of writing, one of these patients is 4 years old and has normal neurological and psychomotor development, and the other two patients, aged 1 year and 6 years, have mild and moderate psychomotor and neurodevelopmental delays respectively. Table 1 presents a comparison between patients with and without an early diagnosis of MSUD.
Influence of early diagnosis on the course of MSUDa.
| Early diagnosis (n=12) | Late diagnosis(n=71) | p | |
|---|---|---|---|
| Positive family history (n=14/83) | 5/12 (41.6%) | 9/71 (12.6%) | 0.034 |
| Severity of developmental delay (n=58/83) | |||
| None (n=1) | 1/12 (8.3%) | 0/46 (0%) | 0.230 |
| Severe (n=15) | 2/12 (16.7%) | 13/46 (28.3%) | |
| Moderate (n=20) | 4/12 (33.3%) | 16/46 (34.8%) | |
| Mild (n=22) | 5/12 (41.7%) | 17/46 (37%) | |
| Leucine ≥ 1000μmol/L at diagnosis (n=53/73) | 9/12 (75%) | 44/61 (72.1%) | 0.716 |
| Symptoms present at diagnosis (n=80/83) | 9/12 (75%) | 71/71 (100%) | 0.02 |
| Diagnosis period (n=83/83) | |||
| 1992-2001 (n=31) | 2/12 (16.7%) | 29/71 (40.8%) | 0.195 |
| 2002-2011 (n=52) | 10/12 (83.3%) | 42/71 (59.1%) | |
| Survival as of 2011 (n=68/83) | |||
| Alive (n=48) | 9/12 (75%) | 39/56 (69.6%) | 0.866 |
| Dead (n=20) | 3/12 (25%) | 17/56 (30.4%) | |
The most common clinical manifestations at the time of patient enrollment were psychomotor and neurodevelopmental delay (98.8%) and poor nutritional status (74.7%). Two patients were overweight.
Median age at diagnosis was not significantly associated with severity of developmental delay (n=58/83; p=0.31), nor were elevated leucine levels (n=57/73; p=0.961).
Seventy-three (88.0%) patients had classic MSUD (median age at diagnosis, 60 days; IQR 27.5–180 days), eight (9.6%) had intermediate MSUD (median age at diagnosis, 257 days; IQR 33.7–668 days), and two (2.4%) had intermittent MSUD (age at diagnosis, 6 and 7 years respectively). For patients with the intermediate form, the most common clinical manifestations at diagnosis were food avoidance and respiratory abnormalities, while for patients with the intermittent form, those manifestations were seizures and respiratory abnormalities. All patients with the intermediate/intermittent forms were alive at the time of writing.
TreatmentFifty-eight (69.9%) patients were being managed by neurologists, 56 (67.5%) by medical geneticists, 49 (59.0%) by pediatricians, and 46 (55.4%) by dietitians. Other professionals involved in patient management and follow-up included neonatologists, gastroenterologists, physician nutrition specialists, speech and language pathologists, and physical therapists.
The patients in our sample received follow-up at 16 treatment centers, with a median of five patients per center (IQR 1.75–6.5). Use of an MSUD-specific metabolic formula was reported in 62 of 73 patients (74.7%). Three patients had undergone liver transplantation; in two cases, the procedure was performed in Brazil. Thirty-seven patients (59.7%) received the metabolic formula regularly (median age, 5 years; IQR 1-7.5 years); those who reported failures in formula supply had a median age of 2 years (IQR 0.5-5.00). Median time elapsed between diagnosis and receipt of the formula was 17.5 days (IQR 5.75–30 days). There was no significant association between severity of developmental delay and regularity of formula supply (n=40/62, p=0.074).
DeathsOf the patients for whom data were available (n=68), 20—all with classic MSUD—died before the start of the study. Median age at death was 225 days (IQR 127.5–365 days). There was no statistically significant correlation between fatal outcome and leucine levels at diagnosis (p=0.568).
DiscussionTo the best of our knowledge, this is the first study to outline a profile of Brazilian patients with MSUD. The current Brazilian population is estimated at 190,732,694, with 2,944,928 live births occurring per year.13 Therefore, considering a mean incidence of MSUD of 1:100,000 in the country, we would expect approximately 300 new diagnoses of the disease over a 10-year period—a much lower estimate than the sample actually included in the study. This suggests that MSUD is underdiagnosed in the country.
MSUD meets most of the Wilson and Jungner14 criteria for screening: for instance, there is a recognizable latent or early symptomatic stage and an accepted treatment for patients with recognized disease. In countries where MSUD is included in neonatal screening, patients are usually diagnosed before the 10th day of life.3,4 Conversely, in countries where MSUD is not included in public neonatal screening programs, such as Brazil, diagnosis is usually delayed, occurring at ages similar to those reported for our sample.15,16 The predominance of classic MSUD and symptomatic patients in our sample could be also due to the non-inclusion of MSUD in the public neonatal screening program, as the literature suggests that newborn screening enables earlier diagnosis of milder forms of the condition.5
As expected, patients with a positive family history were tested earlier than patients with no family history of MSUD; this was probably due to genetic counseling of families who had already had one child with the condition and were thus aware of the risk of recurrence and the need for early investigation.
Our study found an upward trend in the number of MSUD diagnoses over the past decade, which coincided with the establishment of the SIEM hotline and the implementation of a public neonatal screening program by the Brazilian Ministry of Health.17 The reasons behind this trend are unknown, but it may reflect greater awareness of IEMs in general by health care providers, as well as greater awareness of the early clinical manifestations of these conditions. Nevertheless, the increase was not statistically significant, and there was no significant difference in age at diagnosis between the two periods, which corroborates our belief that a substantial portion of MSUD patients continue to die undiagnosed and untreated in Brazil. A similar situation is seen in Malaysia, where newborn screening does not include MSUD: the diagnosis is often late and MSUD appears to be less prevalent than expected.18
Psychomotor and neurodevelopmental delays were detected in practically all patients in the sample. Just over half of patients who received the MSUD-specific metabolic formula reported that the formula was supplied regularly. However, most patients exhibited inadequate nutritional status. It bears stressing that MSUD patients should always be followed by nutritional care providers, and only half of the patients in our sample had the support of a registered dietitian.19 Most patients who received metabolic formula, however, were monitored by dietitians (data not shown). Neurologists were the professionals most often responsible for patient follow-up, which may be secondary to the high frequency of developmental delay in this sample.
In Brazil, time between diagnosis and receipt of the metabolic formula is long and variable. When patients were diagnosed in the acute stage of the disease, during a hospital stay due to metabolic decompensation, they were likely to be started on metabolic formula on the date of diagnosis (if the formula is available at the hospital of admission, of course). Conversely, patients who were diagnosed at a non-acute stage of the disease and treated on an outpatient basis were likely to receive the formula only much later; in fact, these patients usually secure access to the metabolic formula through litigation. Again, it bears stressing that use of the BCAA-free formula is essential, as it ensures the amount of protein required for proper growth and development.1 Recently, studies have been conducted in rats with newly induced classical and intermediate MSUD to assess the consequences of rapid BCAA buildup and assess potential treatment options, such as norleucine.20
Leucine levels at diagnosis were high, with a median value of 1,693μmol/L. Leucine levels in excess of 1,000μmol/L are considered critical, as they may produce irreversible damage or even death.3,21,22 However, there was no significant association between severity of developmental delay and leucine levels at diagnosis. This may be attributable to the fact that long-term metabolic control is considered a more decisive determinant of psychomotor and cognitive development than leucine levels at diagnosis.22
In this study, the advantage of early diagnosis appears to have been lost due to a lack of short- and long-term clinical management. As reported for Filipino patients,15 no clinical protocol for management of acute-stage MSUD is available in Brazil, and patients do not receive the metabolic formula reliably. Conversely, in a study by Morton et al. 4 in which patients had access to the formula and a clinical protocol was followed in the acute stage of the disease, the overall outcome was better and patients achieved more adequate development.
In light of the recent adoption of a specific public policy for diagnosis and management of rare diseases in Brazil,23,24 we suggest the following steps should be taken to further improve the quality of life of MSUD patients in the country: a) expand the public newborn screening program to include MSUD among the identified disorders; b) develop the ability to conduct alloisoleucine testing locally; c) make the specific metabolic formulas available to all patients, without the need for legal intervention; d) establish a national center specializing in liver transplantation for metabolic disorders; and e) establish a network of multidisciplinary teams comprising physicians, nurses and dietitians specialized in the treatment of inborn errors of metabolism to develop national protocols for MSUD management. The creation of the Brazilian MSUD Network (http://redexaropedobordo.com.br/), established in 2010 to promote education on the diagnosis and management of MSUD and supported by a Brazilian research agency and by the Ministry of Science and Technology, is one of the first steps toward this goal.
FundingThis study was supported by the Brazilian Coordination for Improvement of Higher Education Personnel (CAPES), Fundo de Incentivo à Pesquisa e Eventos (FIPE-HCPA) and the Brazilian National Council of Scientific and Technological Development (CNPq)–grant no. MCT/CNPq/CT-SAÚDE 57/2010.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the professionals from the Brazilian MSUD Network who contributed to this paper, as well as the staff of the Medical Genetics Service at Hospital de Clínicas de Porto Alegre, Brazil, especially those professionals involved in the biochemical analysis of patients with suspected metabolic disorders.
Please cite this article as: Herber S, Schwartz IV, Nalin T, Netto CB, Junior JS, Santos ML, et al. Maple syrup urine disease in Brazil: a panorama of the last two decades. J Pediatr (Rio J). 2015;91:292–8.
Study conducted at Universidade Federal do Rio Grande do Sul (UFRGS), Porto Alegre, RS, Brazil.