To assess if magnetic resonance enterography is capable of showing evidence/extent of disease in pediatric patients with biopsy-proven celiac disease by comparing with a control group, and to correlate the magnetic resonance enterography findings with anti-endomysial antibody level, which is an indicator of gluten-free dietary compliance.
MethodsThirty-one pediatric patients (mean age 11.7±3.1 years) with biopsy-proven celiac disease and 40 pediatric patients as a control group were recruited in the study. The magnetic resonance enterography images of both patients with celiac disease and those of the control group were evaluated by two pediatric radiologists in a blinded manner for the mucosal pattern, presence of wall thickening, luminal distention of the small bowel, and extra-intestinal findings. Patient charts were reviewed to note clinical features and laboratory findings. The histopathologic review of the duodenal biopsies was re-conducted.
ResultsThe mean duration of the disease was 5.6±1.8 years (range: 3–7.2 years). In 24 (77%) of the patients, anti-endomysial antibody levels were elevated (mean 119.2±66.6RU/mL). Magnetic resonance enterography revealed normal fold pattern in all the patients. Ten (32%) patients had enlarged mesenteric lymph nodes.
ConclusionAlthough a majority of the patients had elevated anti-endomysial antibody levels indicating poor dietary compliance, magnetic resonance enterography did not show any mucosal abnormality associated with the inability of magnetic resonance enterography to detect mild/early changes of celiac disease in children. Therefore, it may not be useful for the follow-up of pediatric celiac disease.
Avaliar se a enterografia por ressonância magnética consegue comprovar/mostrar a extensão da doença em pacientes pediátricos com doença celíaca comprovada por biópsia comparando com um grupo de controle e correlacionar os achados da enterografia por ressonância magnética com o nível de anticorpo antiendomísio indicador de dieta sem glúten.
Métodos31 pacientes pediátricos (idade média entre 11,7±3,1 anos) com doença celíaca comprovada por biópsia e 40 pacientes pediátricos em um grupo de controle foram recrutados no estudo. As imagens da enterografia por ressonância magnética dos pacientes com doença celíaca e no grupo de controle foram avaliadas por dois radiologistas pediátricos às cegas para o padrão da mucosa, presença de espessamento da parede, dilatação luminal do intestino delgado e achados extraintestinais. Os prontuários dos pacientes foram revisados para anotação de características clínicas e achados laboratoriais. A avaliação histopatológica das biópsias duodenais foi feita novamente.
ResultadosA duração média da doença foi 5,6±1,8 anos (faixa de 3-7,2 anos). Em 24 (77%) dos pacientes, os níveis anticorpo antiendomísio estavam elevados (média 119,2±66,6 RU/mL). A enterografia por ressonância magnética revelou um padrão de pregas normal em todos os pacientes. 10 (32%) dos pacientes apresentaram gânglios linfáticos mesentéricos aumentados.
ConclusãoApesar de a maioria dos pacientes possuir níveis elevados de anticorpo antiendomísio, indicando uma dieta pobre, a enterografia por ressonância magnética não mostrou nenhuma anomalia na mucosa associada à incapacidade de a enterografia por ressonância magnética detectar alterações leves/precoces de doença celíaca nas crianças. Portanto, ela pode não ser útil no acompanhamento da doença celíaca pediátrica.
Celiac disease (CD), a malabsorption syndrome with an autoimmune origin, affects approximately 1% of the population.1,2 The incidence of CD has increased over the decades, presumably due to increased exposure to gluten, awareness of the broad spectrum of clinical presentation, and the availability of sensitive and specific diagnostic tools.3–6 However, the ‘iceberg model’ indicates the extent of undiagnosed population with CD.7 Thus, CD represents a substantial health problem worldwide, affecting both adults and the pediatric population.8
In genetically susceptible children, the disease is triggered by exposure to gluten-containing foods. It predominantly affects the duodenum and jejunum; however, the entire small bowel can be involved. The mucosal changes are characterized by villous atrophy, crypt hyperplasia, thickening of the basement membrane under the surface of epithelium, reduced number of goblet cells, and signs of inflammation.9 The clinical features are broad and nonspecific. The spectrum of clinical presentation in CD may be classified as: (a) classical form, related with intestinal symptoms and predominantly diagnosed in pediatric patients; (b) atypical form, presentation often with extra-intestinal symptoms such as iron deficiency; (c) silent form; and (d) latent form, patients are asymptomatic and diagnosed during screening due to presence of family history or CD-related conditions, such as type 1 diabetes mellitus, Down syndrome, and juvenile idiopathic arthritis. In latent form, the serologic tests are positive when accompanied with either no histopathologic change in the intestine or only an increase in intraepithelial lymphocytes (Marsh stage 1). The positivity of the serological tests including anti-endomysial (EMA) and anti-tissue transglutaminase (tTG) antibodies in the course of exposure to gluten-containing food and both serological and clinical improvement following gluten-free diet aid in making the diagnosis of CD. The definitive diagnosis is established by endoscopic duodenal or jejunal biopsy.10
The characteristic imaging finding of CD is small bowel mucosal fold abnormality, which includes blunting of folds, reduction in the number of jejunal folds, and increase in the number of ileal folds depending on the extent and degree of involvement. These mucosal fold changes have traditionally been evaluated using barium studies. Magnetic resonance enterography (MRE) is a relatively new but well-established radiation-free method for bowel assessment, particularly in inflammatory bowel disease.11,12 Since MRE enables visualization of the entire small bowel, it has been shown to be beneficial in determining the extent of the disease, CD-related complications including ulcerative jejunoileitis and malignancies, and refractory CD in patients with persisting symptoms despite gluten-free diet.13–16 However, the studies focused on CD using MRE were conducted particularly in adult study groups and there is scarcity of such studies in the literature evaluating findings of CD by MRE in children.17
The histopathologic examination of the patients with CD does not give sufficient information about the extent of the disease, since it is confined to duodenum and proximal jejunum. Thus, the purpose of this prospective, single center study was to determine if MRE is capable of showing extent of the disease in pediatric patients with biopsy proven CD by comparing with a control group and correlating the MRE findings with anti-EMA level, which is an indicator of gluten-free dietary compliance.18
Materials and methodsPatientsThis study was approved by the institutional review board and is compatible with Declaration of Helsinki. Written informed consent was obtained from the parents of all patients. It was conducted between January 2014 and January 2015. The patients who were being followed up with the diagnosis of CD by the pediatric gastroenterology clinics of this institution were recruited in the study. The inclusion criteria included children above 5 years of age with the ability to comply with breath-holding instructions and stay still throughout the procedure without need for sedation. The diagnosis of CD was based on the criteria outlined by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition.8
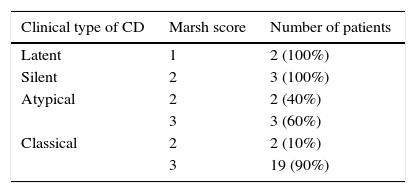
Patient chart reviewPatient charts were reviewed prior to MRE examinations for clinical features and laboratory findings, and subsequently recorded by a pediatric gastroenterologist (E.S.). The histopathologic examinations of the previously obtained (at the time of diagnosis) duodenal biopsies of the patients were re-analyzed by a pathologist (K.D.) who was blinded to clinical features. The patients were scored and grouped according to the Marsh classification, which is obtained from the histopathologic examination and reflects the severity of the disease (Table 1). Marsh classification consists of four stages (0–3) constructed based on several features of biopsy specimen: Stage 0 reflects normal biopsy, while stage 1, stage 2, and stage 3 are predominantly associated with increased intraepithelial lymphocytes, crypt hyperplasia, and villous atrophy, respectively.19,9
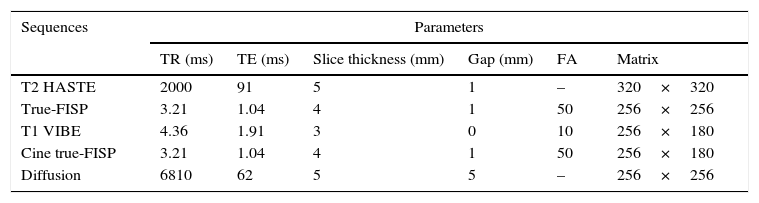
MR enterography techniquePatients were scanned by a 1.5T clinical scanner (Magnetom, Aera – Siemens Healthcare; Erlangen, Germany) with an 18-channel body coil. Prior to MRE examination, 24 patients with CD were non-compliant, while eight were compliant with gluten-free diet. The preparation for MRE consisted of fasting for 4–6h and administration of mannitol solution (3%) as an oral contrast medium. MRE performed in supine position with the following sequences: Coronal T2-weighted half-Fourier acquisition single-shot turbo spin-echo (HASTE) in order to evaluate the distension of the small intestine, CINE imaging with coronal fast imaging with steady-state free precession (True-FISP), axial (with fat saturation) and coronal True-FISP, coronal T2-weighted HASTE with fat saturation, axial single-shot fast spin-echo echo planar diffusion weighted imaging (b=50, 400, 800s/mm2), and prior to and following, intravenous gadolinium-based contrast medium injection (0.1mmol/kg) axial and coronal 3D T1-weighted volumetric interpolated breath-hold examination with fat saturation (VIBE). Hyoscine butylbromide (Buscopan; Boehringer – Ingelheim, Germany) was administered intravenously twice slowly over 2min at a dose of 0.3mg/kg, with a maximum dose of 20mg to eliminate bowel movement and contraction; following the CINE imaging and prior to contrast agent administration. The sequence parameters are presented in Table 2.
Sequence parameters of MRI acquisition.
| Sequences | Parameters | |||||
|---|---|---|---|---|---|---|
| TR (ms) | TE (ms) | Slice thickness (mm) | Gap (mm) | FA | Matrix | |
| T2 HASTE | 2000 | 91 | 5 | 1 | – | 320×320 |
| True-FISP | 3.21 | 1.04 | 4 | 1 | 50 | 256×256 |
| T1 VIBE | 4.36 | 1.91 | 3 | 0 | 10 | 256×180 |
| Cine true-FISP | 3.21 | 1.04 | 4 | 1 | 50 | 256×180 |
| Diffusion | 6810 | 62 | 5 | 5 | – | 256×256 |
MRI, magnetic resonance imaging; HASTE, half-Fourier acquisition single-shot turbo spin-echo; True-FISP, fast imaging with steady-state free precession; VIBE, volumetric interpolated breath-hold examination; TR, time of repetition; TE, time of echo; FA, flip angle.
The MRE examinations of 40 pediatric patients (mean age: 8.0±1.2 years; age range: 5–8.4 years), as a control group, who were scanned with the suspicion of inflammatory bowel disease but had normal imaging findings, and the patient group with the diagnosis of CD were anonymized and sent back to a clinical picture-archiving and communication system by a pediatric radiologist (M.S.D.) who did not take part in the image evaluation.
The images were independently assessed by two pediatric radiologists (S.D., G.K., four and five years of experience in reading MREs, respectively) in a manner blinded to the patients’ clinical information. Each MRE was scored for the absence (0) or presence (1) of one-fold pattern abnormalities of the duodenal, jejunal, and ileal loops; (2) enhancement, diffusion restriction, and increased thickness of the small bowel wall; (3) increased diameter of the bowel loops, (4) intussusception, and (5) mesenteric lymph nodes, fatty infiltration, and vascular engorgement. They specifically looked for duodenal fold loss, ilealization of the jejunum (
Additionally, the radiologists were asked to rate the images of each patient with an incremental three-point scale (0=inadequate, 1=moderate, 2=adequate) for small bowel distention.
ResultsA total of 45 pediatric patients with the diagnosis of CD were recruited in the study initially. Nine of the patients whose duodenal biopsy and histopathologic examination were carried out in another center and five patients who could not tolerate the MRE acquisition (due to associated chronic diseases such as IgA deficiency, Turner syndrome, type 1 diabetes mellitus, and Down syndrome that might have caused the patients to be incompatible) were excluded.
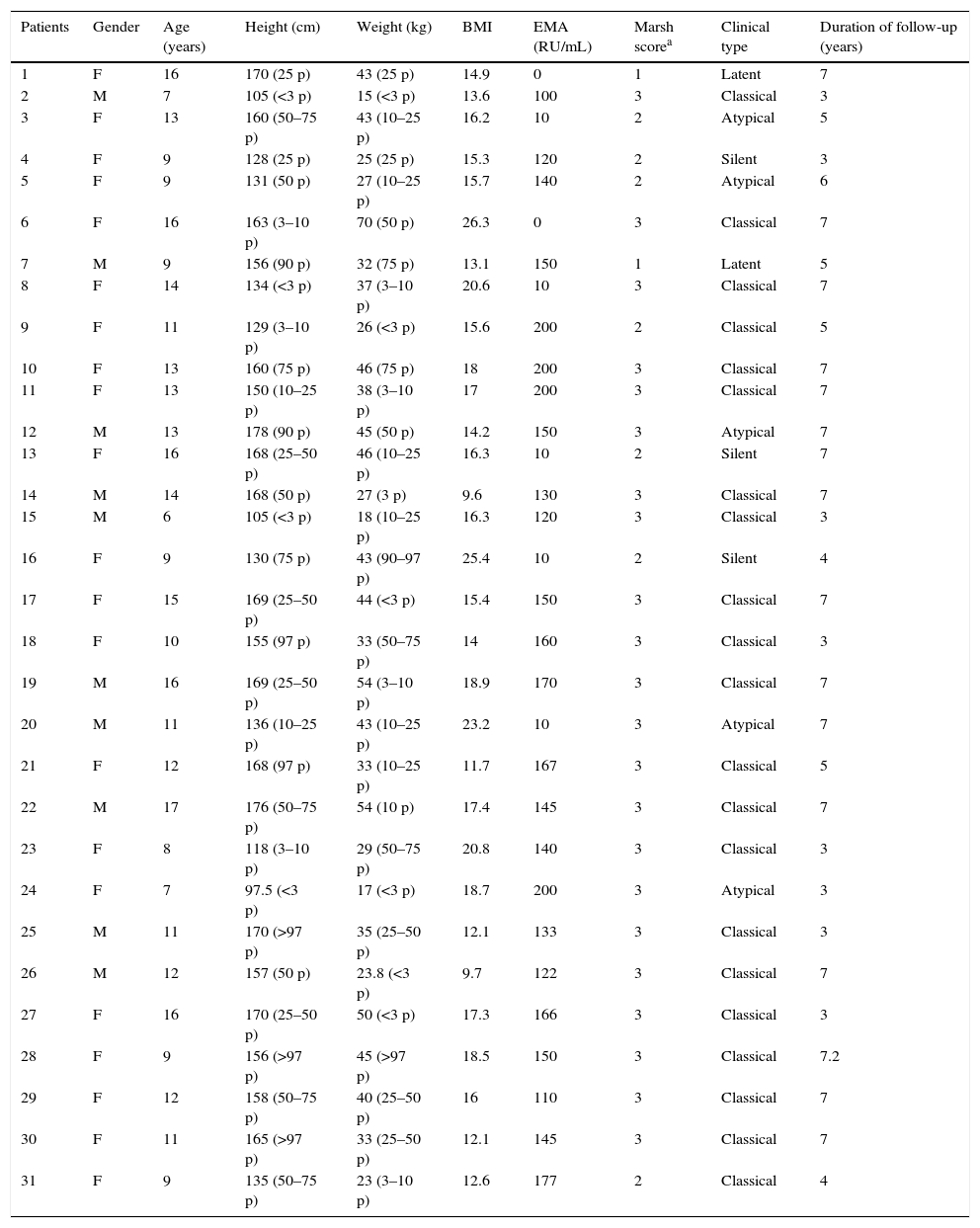
Finally, 31 children with CD (ten boys and 21 girls; mean age 11.7±3.1 years and age range 6–16 years) were included. Twenty-one (68%) patients out of 31 were categorized as classical, five (16%) as atypical, two (6%) as latent, and three (10%) as silent CD. The presenting symptom for all the patients with classical CD was chronic diarrhea, abdominal distension, and pain. Patients with atypical CD presented with constipation and accompanying iron deficiency anemia resistant to oral Fe. There were no signs/symptoms of the patients with latent and silent CD. They were diagnosed by screening conducted due to increased risk for CD because of family history.
The mean duration of the disease was 5.6±1.8 years (range 3–7.2 years). In 24 patients who were non-compliant with the gluten-free diet, EMA levels were elevated (mean 119.2±66.6RU/mL and range 0–200RU/mL). In this institution, anti-EMA levels of 0–20RU/mL are considered to be within normal limits while levels of 21–200RU/mL are considered elevated. The average time between measurement of the serum EMA level and MRE examination was 12±3.0 days (range 8–16 days). Prior to MRE examination, patients with non-elevated EMA and ten out of 24 patients with elevated EMA were all free of symptoms. Fourteen patients with elevated EMA presented with either abdominal pain or diarrhea. Patient demographics and laboratory findings are listed in Table 3.
Clinical and laboratory features of the study group.
| Patients | Gender | Age (years) | Height (cm) | Weight (kg) | BMI | EMA (RU/mL) | Marsh scorea | Clinical type | Duration of follow-up (years) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 16 | 170 (25 p) | 43 (25 p) | 14.9 | 0 | 1 | Latent | 7 |
| 2 | M | 7 | 105 (<3 p) | 15 (<3 p) | 13.6 | 100 | 3 | Classical | 3 |
| 3 | F | 13 | 160 (50–75 p) | 43 (10–25 p) | 16.2 | 10 | 2 | Atypical | 5 |
| 4 | F | 9 | 128 (25 p) | 25 (25 p) | 15.3 | 120 | 2 | Silent | 3 |
| 5 | F | 9 | 131 (50 p) | 27 (10–25 p) | 15.7 | 140 | 2 | Atypical | 6 |
| 6 | F | 16 | 163 (3–10 p) | 70 (50 p) | 26.3 | 0 | 3 | Classical | 7 |
| 7 | M | 9 | 156 (90 p) | 32 (75 p) | 13.1 | 150 | 1 | Latent | 5 |
| 8 | F | 14 | 134 (<3 p) | 37 (3–10 p) | 20.6 | 10 | 3 | Classical | 7 |
| 9 | F | 11 | 129 (3–10 p) | 26 (<3 p) | 15.6 | 200 | 2 | Classical | 5 |
| 10 | F | 13 | 160 (75 p) | 46 (75 p) | 18 | 200 | 3 | Classical | 7 |
| 11 | F | 13 | 150 (10–25 p) | 38 (3–10 p) | 17 | 200 | 3 | Classical | 7 |
| 12 | M | 13 | 178 (90 p) | 45 (50 p) | 14.2 | 150 | 3 | Atypical | 7 |
| 13 | F | 16 | 168 (25–50 p) | 46 (10–25 p) | 16.3 | 10 | 2 | Silent | 7 |
| 14 | M | 14 | 168 (50 p) | 27 (3 p) | 9.6 | 130 | 3 | Classical | 7 |
| 15 | M | 6 | 105 (<3 p) | 18 (10–25 p) | 16.3 | 120 | 3 | Classical | 3 |
| 16 | F | 9 | 130 (75 p) | 43 (90–97 p) | 25.4 | 10 | 2 | Silent | 4 |
| 17 | F | 15 | 169 (25–50 p) | 44 (<3 p) | 15.4 | 150 | 3 | Classical | 7 |
| 18 | F | 10 | 155 (97 p) | 33 (50–75 p) | 14 | 160 | 3 | Classical | 3 |
| 19 | M | 16 | 169 (25–50 p) | 54 (3–10 p) | 18.9 | 170 | 3 | Classical | 7 |
| 20 | M | 11 | 136 (10–25 p) | 43 (10–25 p) | 23.2 | 10 | 3 | Atypical | 7 |
| 21 | F | 12 | 168 (97 p) | 33 (10–25 p) | 11.7 | 167 | 3 | Classical | 5 |
| 22 | M | 17 | 176 (50–75 p) | 54 (10 p) | 17.4 | 145 | 3 | Classical | 7 |
| 23 | F | 8 | 118 (3–10 p) | 29 (50–75 p) | 20.8 | 140 | 3 | Classical | 3 |
| 24 | F | 7 | 97.5 (<3 p) | 17 (<3 p) | 18.7 | 200 | 3 | Atypical | 3 |
| 25 | M | 11 | 170 (>97 p) | 35 (25–50 p) | 12.1 | 133 | 3 | Classical | 3 |
| 26 | M | 12 | 157 (50 p) | 23.8 (<3 p) | 9.7 | 122 | 3 | Classical | 7 |
| 27 | F | 16 | 170 (25–50 p) | 50 (<3 p) | 17.3 | 166 | 3 | Classical | 3 |
| 28 | F | 9 | 156 (>97 p) | 45 (>97 p) | 18.5 | 150 | 3 | Classical | 7.2 |
| 29 | F | 12 | 158 (50–75 p) | 40 (25–50 p) | 16 | 110 | 3 | Classical | 7 |
| 30 | F | 11 | 165 (>97 p) | 33 (25–50 p) | 12.1 | 145 | 3 | Classical | 7 |
| 31 | F | 9 | 135 (50–75 p) | 23 (3–10 p) | 12.6 | 177 | 2 | Classical | 4 |
BMI, body mass index; <15, underweight; 15–24, normal; >24, overweight; EMA, anti-endomysial antibody; 0–20RU/mL, normal; 20–200RU/mL, elevated; p, percentile.
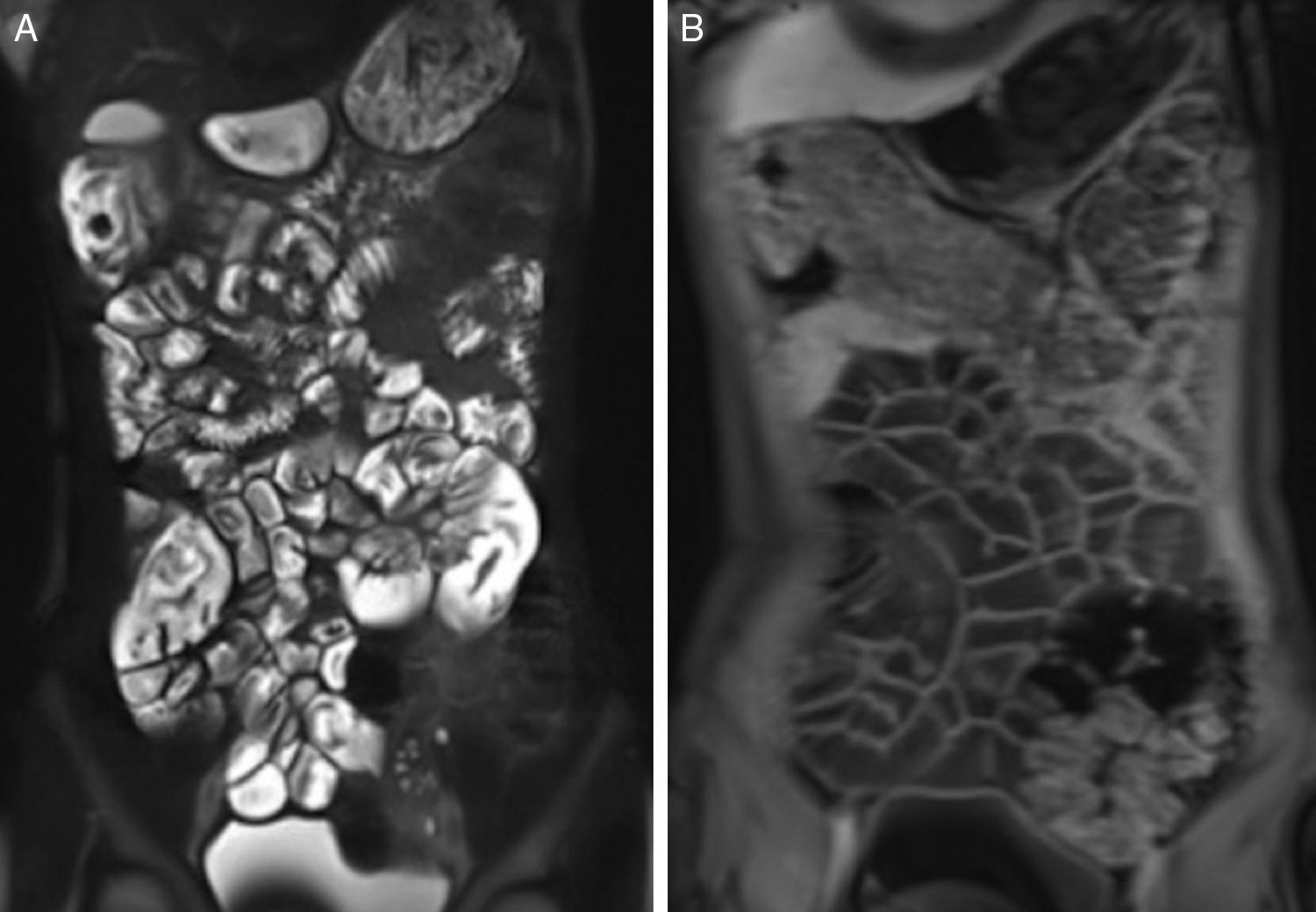
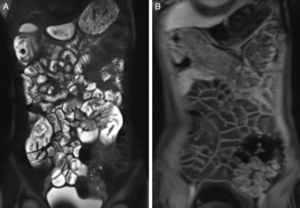
The two radiologists rated all the examinations of the patients with CD and the control group as ‘0’: fold pattern was interpreted as normal in all the patients. There was no duodenal fold loss, ilealization of the jejunum, jejunization of the ileum, or global loss of valvulae. The wall thickness was within normal limits (mean: 1.5±0.26 and 1.58±0.28mm for jejunum and ileum, respectively). Abnormal enhancement or diffusion restriction of the bowel wall was not encountered (Fig. 1).
16-Year-old female patient with diagnosis of celiac disease; T2-weighted HASTE (A) and T1-weighted fat-saturated VIBE (B) images acquired following intravenous contrast administration reveal no fold pattern abnormalities of the intestines. HASTE, half-Fourier acquisition single-shot turbo spin-echo; VIBE, volumetric interpolated breath-hold examination.
Ten patients out of 31 (32%) were detected to have mesenteric lymph nodes with >1cm short-axis diameter. No other extra-intestinal abnormalities were detected.
The radiologists rated the images of patients with CD as ‘adequate’ in 25 (81%) and 27 (87%) out of the 31 examinations (substantial inter reader agreement, κ=0.73), and the images of control group patients as ‘adequate’ in 34 (85%) and 32 (80%) out of 40, respectively (almost perfect inter-reader agreement, κ=0.82), while the rest were scored as ‘moderate’ for small bowel distention.
Examinations were well tolerated and no significant adverse effects occurred.
DiscussionThis study performed to assess MRE findings of CD in children did not reveal any imaging abnormalities. Several studies have shown fold pattern abnormalities on imaging in patients with uncomplicated CD.20,21 The findings include decreased number of jejunal folds (
Five out of 31 (16%) patients in the study group were diagnosed with either latent or silent CD. The histopathologic examination of the duodenal biopsies of these patients revealed either Marsh stage 1 or 2. Tomei et al.13 reported that 90% of their patients diagnosed with silent CD had normal fold pattern. Although there is a limited number of studies focusing on MRE findings of CD, the large experience in Crohn's disease has revealed the inability of MRE to exhibit mucosal changes, but for inflammatory wall involvement.22 In accordance with this fact, in the current study all the patients diagnosed with either silent or latent CD had no fold pattern abnormalities on MRE. In fact, in this study that consisted of a majority (68%) of children with the classical form, no fold abnormalities were seen in any patients.
Increased levels of EMA were detected in 77% of the patients prior to MRE acquisition. The antibodies including EMA and tTG are essential for the follow-up of patients with CD and have been reported to have a good correlation with gluten-free dietary compliance in both adult and pediatric patients.23 Increased levels of EMA indicate non-compliance of the patient, i.e., not strictly adhering to gluten-free diet.24 van den Bosch et al. reported a good correlation between response to gluten-free diet and enteroclysis findings as compared to biopsy in adults with CD.23 However, there are no such studies related to MRE. An alternative explanation, at least in part, for absence of imaging finding in patients with normal anti-EMA levels could be prevention of mucosal damage with gluten-free diet.
The extraluminal radiologic manifestations of CD include enlarged mesenteric lymph nodes, mesenteric vascular engorgement, and transient intussusceptions. Enlarged (>1cm short-axis diameter) mesenteric lymph nodes are the most common extraluminal finding associated with CD, seen in up to 42% cases.25 The size of lymph nodes decreases with treatment with gluten-free diet and their persistence should raise the suspicion of lymphoma.25,26 These hypertrophic lymph nodes may act as an inception point for intussusception, which can be the initial presentation in 57% of the patients with CD.27 Mesenteric vascular engorgement is a nonspecific sign of the disease. While enlarged mesenteric lymph nodes were the only and the most common extraluminal finding in the current patients, intussusception and vascular engorgement were not detected.
This study has a few limitations. Although the total number of study patients was relatively acceptable, the patient group was diverse, including patients with classical, atypical, silent, and latent CD. Since the both patients with silent and latent CD had lower Marsh scores associated with mild mucosal changes that might have resulted in lack of MRE findings, a study conducted with a larger, homogenized patient group may be worth further investigation. Since radiological follow-up was not performed, serial MRE images acquired at the time of diagnosis and following initiation of gluten-free diet would help assess radiological changes in the course of disease. Lastly, the histopathologic examination of the duodenal biopsy was performed at the time of diagnosis. The comparison of recently obtained biopsy results with imaging findings would enable making a more plausible hypothesis on the relation of imaging findings and histopathologic changes.
In conclusion, despite elevated EMA levels in the majority of children, indicating poor dietary compliance, this study did not show any significant MRE findings in biopsy-proven CD, indicating inability of MRE to detect mild and/or early mucosal damage (suggested by lower Marsh score) seen in children with CD. Therefore, it may not be useful as a diagnostic test for CD or for follow-up. However, as indicated by some authors previously,17 MRE may be useful for detection of suspected complications of CD, such as stricture and lymphoma, evaluation of CD non-responsive to gluten-free diet, and to exclude alternative diagnoses.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Koc G, Doganay S, Sevinc E, Deniz K, Chavhan G, Gorkem SB, et al. Magnetic resonance enterography in pediatric celiac disease. J Pediatr (Rio J). 2017;93:413–9.