To assess the effect of Leisure-time physical activity (LTPA) on cardiometabolic risk by nutritional status in Mexican children and adolescents.
MethodsThis was a cross-sectional study conducted with 1,309 participants aged between 5 and 17 years. Nutritional status was classified according to the BMI Z-score by age and gender. A previously validated questionnaire was used to evaluate LTPA; a cardiometabolic risk score was calculated. Multiple linear regression analysis was performed to assess the effect of LTPA on cardiometabolic risk.
ResultsAfter adjusting for risk factors, mild LTPA were positively associated with cardiometabolic risk score (βMildvsIntenseLTPA: 0.68; 95% CI: 0.18 to 1.18; pfortrend = 0.007). This association became stronger when estimated for overweight (β MildvsIntenseLTPA: 1.24; 95% CI: 0.24 to 2.24; pfortrend = 0.015) and obese participants (β MildvsIntenseLTPA: 1.02; 95% CI: 0.07 to 1.97; pfortrend= 0.045).
ConclusionMild LTPA was positively associated with cardiometabolic risk in overweight and obese children and adolescents. Given the emerging childhood obesity epidemic in Mexico, these results may be useful in the design of strategies and programs to increase physical activity levels in order to achieve better health.
Avaliar o efeito da prática de AFL sobre o risco cardiometabólico em crianças e adolescentes mexicanos de acordo com sua situação nutricional.
MétodosEstudo transversal realizado com 1309 participantes de 5 a 17 anos de idade. A situação nutricional foi classificada de acordo com o escore z de IMC por idade e sexo. Um questionário validado anteriormente foi utilizado para avaliar a AFL; foi calculado um escore de risco cardiometabólico. A análise de regressão linear múltipla foi realizada para avaliar o efeito de AFL sobre o risco cardiometabólico.
ResultadosApós o ajuste de acordo com os fatores de risco, a AFL leve foi positivamente associada ao escore de risco cardiometabólico (βAFLLevexIntensa: 0,68; IC 95%: 0,18 a 1,18; Pparatendência = 0,007). Essa associação foi mais intensa quando estimada para participantes acima do peso (βAFLLevexIntensa: 1,24; IC 95%: 0,24 a 2,24; Pparatendência = 0,015) e obesos (βAFLLevexIntensa: 1,02; IC 95%: 0,07 a 1,97; Pparatendência = 0,045).
ConclusãoA AFL leve foi positivamente associada ao escore de risco cardiometabólico em crianças e adolescentes acima do peso e obesos. Considerando a epidemia de obesidade infantil emergente no México, esses resultados poderão ser úteis na elaboração de estratégias e programas para aumentar os níveis de atividade física a fim de obter uma saúde melhor.
The prevalence of overweight and obesity among children and adolescents presents an increasing trend, especially in developing countries.1 According to the World Health Organization (WHO), by the year 2010 there were close to 42 million overweight children.2 Conversely, the Americas are the region with the highest prevalence of overweight and obesity worldwide.3 In Mexico, according to the National Health and Nutrition Survey 2012 (ENSANUT), the combined prevalence of overweight and obesity was 34.4% in school-age children (5-11 years) and 35% in adolescents (12 and 19 years);4 these prevalences are slightly higher than those reported in 2006.5
Overweight and obesity in children and adolescents has been associated with alterations in the cardiometabolic profile or in its different components.6,7 Likewise, it is associated with the early onset of diabetes mellitus and atherosclerotic processes that predispose young adults to cardiovascular diseases.6 Alterations in the metabolic profile have been reported among children and adolescents in Mexico; according to the ENSANUT 2012, 0.7% of adolescents reported a previous diagnosis of diabetes, while 1.8% reported a previous diagnosis of hypertension.4 Studies conducted among children have revealed a prevalence of abnormal glucose level close to 10%, and a prevalence of over 15for to lipid profile alterations.8
The protective role of physical activity on cardiometabolic risk in children and adolescents has been described in the literature.9 Studies have demonstrated that vigorous physical activity improve levels of total cholesterol, low-density lipoproteins (C-LDL), triglycerides, high-density lipoproteins (C-HDL), insulin resistance, and blood pressure, and decrease waist circumference in this population group.9,10 Meanwhile, leisure-time physical activity (LTPA) has been inversely associated with a reduction in the prevalence of overweight and obesity among children and adolescents. Also, among obese subjects, LTPA improves the cardiometabolic profile.11,12 International observational studies demonstrate that high levels of LTPA are significantly associated with a lower metabolic syndrome score in every body mass index (BMI) category.11,12 In contrast, low levels of LTPA in overweight or obese children and adolescents increase the likelihood of developing metabolic syndrome or the alteration of its components.11
In Mexico, epidemiologic evidence about the association of LTPA on the metabolic profile in children and adolescents is scarce and inconclusive;13,14 few cross-sectional studies reported a prevalence of metabolic disorders and metabolic syndrome, but found no associations with physical activity.8,15
This study aimed to assess the effect of the practice of LTPA on the cardiometabolic risk of Mexican children and adolescents according to their nutritional status.
Materials and methodsStudy designBetween June of 2011 and July of 2012, a cross-sectional study was conducted with a representative sample of healthy children and adolescents residents of Mexico City. Its objective was to characterize and assess the association between genetics and lifestyle with obesity. Participants were recruited in four units of the Mexican Institute of Social Security (IMSS). Each unit was located in different geographical areas of Mexico City (Unit Morelos, North; Unit Independencia, South; Unit Netzahualcoyotl, East; and Unit Cuauhtémoc, West). The study was approved by the ethical committees of the Mexican Institute of Social Security and of the Mexican National Institute of Public Health. Before starting the study, the research protocol was explained to both parents and children. Both parents and children who agreed to participate signed an informed consent and assent, respectively.
Study populationFor the current study, a sample of 1,442 children and adolescents were randomly selected. The subject's age ranged from 5 to 17 years; the subjects resided in the west and north area of Mexico City, without a previous diagnosis of diabetes, hypertension, dyslipidemia, or any type of physical or mental impairment. The exclusion criteria comprised children that at the moment of the interview had a diagnosis of infectious disease or gastrointestinal disorders; children who had been treated with antibiotic in the two months prior to the interview; and participants with incomplete questionnaires, anthropometric measures, and biological samples.
InformationParticipants were directly interviewed by personnel previously trained in conducting structured interviews and obtaining anthropometric and blood pressure measures; they were blinded to the study hypothesis. Information on socio-demographic characteristics, personal and family medical history, dietary habits, and practice of LTPA was collected. The anthropometric measures and blood pressure of every child were obtained.
Biochemical measuresThe venous blood sample was obtained after 8-12hours of overnight fasting. Blood samples were separated in serum and plasma, and were then stored at -70°C. Determination of glucose, high-density lipoproteins (C-HDL), low-density lipoproteins (C-LDL), triglycerides, and total cholesterol values were conducted using the Clinical Chemistry System ILAB 300 Plus equipment with controls and calibration curves determined by the Instrumentation Laboratory Company (Instrumentation Laboratory, Massachusetts, USA).
Anthropometric measures and arterial pressureEach of the participants was measured and weighed by previously standardized nutritionists. Before the procedures, participants were asked to take off their shoes, jackets, sweaters, as well as all the heavy objects in their pockets that could alter the weight (keys, glasses, marbles, bracelets, toys, etc.). Weight was measured with a 0.1kg precision using a previously calibrated Seca Clara 803 (SECA, Hamburg, Germany) scale. Height was registered to the nearest decimeter (0.1cm) using a Seca 213 (SECA, Hamburg, Germany) portable stadiometer; participants were standing with their shoulders relaxed. Nutritional status was determined calculating each participant's BMI Z-score by age and gender through the WHO Anthro Plus software (version 1.0.4, 2009).16 Participants with a BMI Z-score by age and gender between -0.99 and 0.99 were classified as normal weight; those with a BMI Z-score between 1 and 1.99, as overweight; and those with a Z-score ≥ 2, as obese. The abdominal circumference was measured at the top of the right iliac crest after a normal exhalation with a 0.1cm precision using a Seca 201 (SECA, Hamburg, Germany) ergonomic fiberglass measuring tape.
After the child had rested for 5min in a quiet environment, blood pressure was measured using a mercury sphygmomanometer with an appropriate-sized cuff on the right arm and the child seated, following international protocols.17
Leisure-time physical activity (LTPA)Each participant with its mother or caregiver answered a questionnaire on the frequency of LTPA practice, which was an adapted and updated version of a previously validated questionnaire, from a low and middle income population of Mexico City, with reproducibility values of r=0.38 to moderate physical activity and r=0.55 to vigorous physical activity.18 The LTPA questionnaire included questions that inquired the frequency (days per week) and duration (never, minutes per day or hours per day) of sports activities (i.e., playing football or soccer, riding a bicycle, etc.) during leisure time, walking as transport-related physical activity, and popular games during the week prior to the application of the instrument.
The type of LTPA and the time spent practicing it were converted to metabolic equivalents (mets/hour/week) by through the Food Processor Nutrition Analysis and Fitness Software version 10.12.0 (ESHA Research Inc., Oregon, USA). The LTPA (mets/hour/week) was categorized in tertiles whose cut-off points were determined based on the normal-weight participants’ LTPA distribution. Thus, LTPA was classified as mild (≤ 21.72 mets/hour/week), moderate (21.73 to 53.1 mets/hour/week), and intense (> 53.1 mets/hour/week). Children whose LTPA and total energy consumption was lower or greater than 3 standard deviations from the mean were excluded from the analysis (61/1,441 children or 4.23% of the sample).
Cardiometabolic risk scoreSo far, there is no consensus in the cut-off points for the cardiometabolic profile indicators in children and adolescents, and the continuous cardiometabolic risk score has been recommended.11 Based on this, the cardiometabolic risk score was calculated as the sum of standardized levels of waist circumference, glucose, C-HDL, C-LDL, triglycerides, total cholesterol, systolic blood pressure (SBP), and diastolic blood pressure (DBP); the standardized levels of C-HDL were included in the score in its inverse presentation (1/C-HDL) because they are inversely related to cardiometabolic risk.11 A higher score indicates a less favorable cardiometabolic profile.
Statistical analysisSocio-demographic characteristics and LTPA were compared between the nutritional status using the chi-squared test. Since the total energy intake, biochemical components, and the cardiometabolic risk score had an asymmetrical distribution, their comparison between the nutritional status groups was conducted using the Kruskal-Wallis test.
Plausible covariates considered in this analysis included: age, gender, nutritional status, parents educational level, total energy intake, and sedentary time. Since the cardiometabolic risk score was a continuous variable, multiple linear regression models were estimated to evaluate the effect of LTPA on cardiometabolic risk. LTPA and sedentary time were included in the regression model as dummies variables, and intense LTPA and less than 14.68hours per week of sedentary activities were reference categories. The multivariate regression model was adjusted through a stepwise method. Interaction between the practice of LTPA and nutritional status was tested by including multiplicative terms; afterwards, the effect of LTPA on cardiometabolic risk was calculated in each category of nutritional status. Trend tests were estimated by including the LTPA into the regression model as a continuous variable. A p-value < 0.05 was considered a statistically significant, except for the interaction, where the p-value was < 0.25. Data analysis was performed using the statistical software Stata version 12.0 (STATA Corporation, College Station, Texas, USA).
ResultsOut of 1,441 subjects (9.22%), 133 were excluded due to implausible values of total energy intake, LTPA, sedentary time values, or missing anthropometric or biochemical data. A final sample size of 1,309 participants was included in the analysis; socio-demographic characteristics (age, gender, parents educational level, etc) of excluded subjects were similar to the characteristics of those included in this study (data not shown).
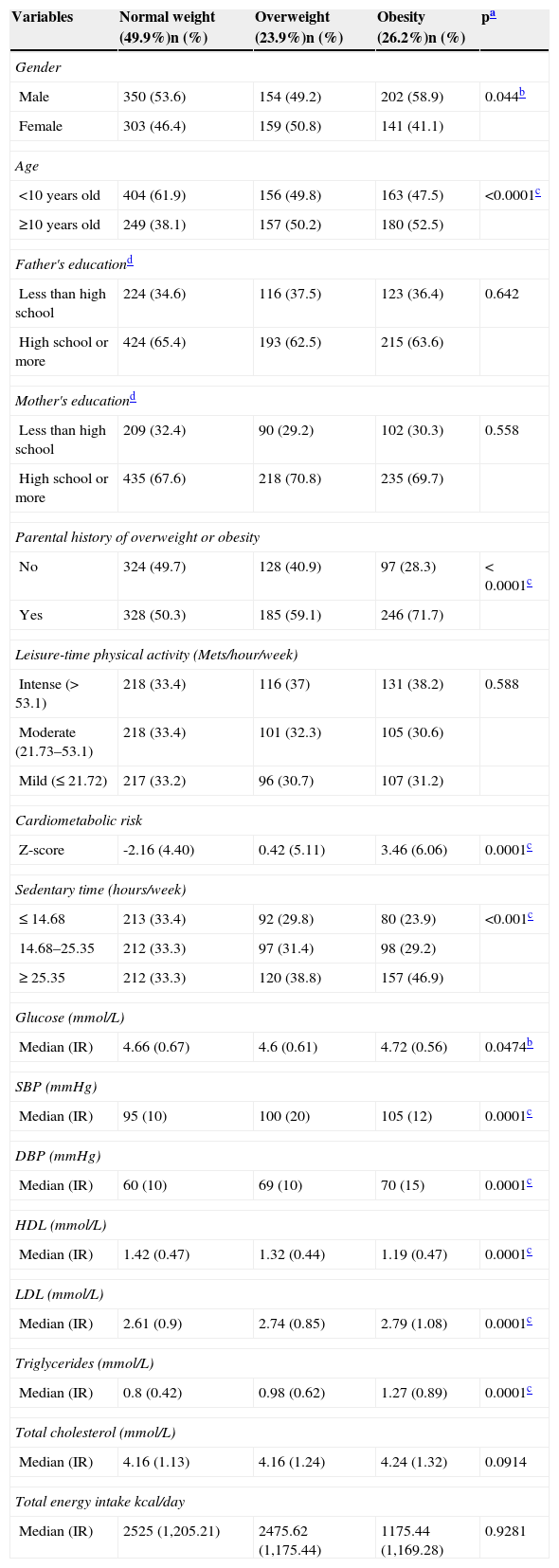
The median age of the study population was 9 years, with an interquartile range of 3; 53.9% of the participants were male; 23.9% were overweight and 26.2% were obese. The median cardiometabolic risk score was -0.40, with an interquartile range of 6.06. Regarding LTPA, 35.5% of the subjects practiced intense LTPA (> 53.1 mets/hour/week) and 32.4% practiced moderate LTPA (21.73 to 53.1 mets/hour/week; data not shown). The distribution of socio-demographic, biochemical characteristics, and LTPA according to nutritional status are presented in Table 1. All the variables – except LTPA, father's and mother's educational level, total cholesterol, and energy intake – were distributed significantly different among the three nutritional status categories. Median of SBP, DBP, C-LDL, and triglyceride levels were statistically higher among overweight and obese children compared with normal-weight children. Furthermore, an increasing trend in the value of these variables was observed in each of the nutritional status categories. In contrast, the median C-HDL level was lower among overweight and obese subjects when compared to the normal-weight subjects.
Distribution of the socio-demographic and biochemical characteristics and LTPA in the study population by nutritional status.
| Variables | Normal weight (49.9%)n (%) | Overweight (23.9%)n (%) | Obesity (26.2%)n (%) | pa |
|---|---|---|---|---|
| Gender | ||||
| Male | 350 (53.6) | 154 (49.2) | 202 (58.9) | 0.044b |
| Female | 303 (46.4) | 159 (50.8) | 141 (41.1) | |
| Age | ||||
| <10 years old | 404 (61.9) | 156 (49.8) | 163 (47.5) | <0.0001c |
| ≥10 years old | 249 (38.1) | 157 (50.2) | 180 (52.5) | |
| Father's educationd | ||||
| Less than high school | 224 (34.6) | 116 (37.5) | 123 (36.4) | 0.642 |
| High school or more | 424 (65.4) | 193 (62.5) | 215 (63.6) | |
| Mother's educationd | ||||
| Less than high school | 209 (32.4) | 90 (29.2) | 102 (30.3) | 0.558 |
| High school or more | 435 (67.6) | 218 (70.8) | 235 (69.7) | |
| Parental history of overweight or obesity | ||||
| No | 324 (49.7) | 128 (40.9) | 97 (28.3) | < 0.0001c |
| Yes | 328 (50.3) | 185 (59.1) | 246 (71.7) | |
| Leisure-time physical activity (Mets/hour/week) | ||||
| Intense (> 53.1) | 218 (33.4) | 116 (37) | 131 (38.2) | 0.588 |
| Moderate (21.73–53.1) | 218 (33.4) | 101 (32.3) | 105 (30.6) | |
| Mild (≤ 21.72) | 217 (33.2) | 96 (30.7) | 107 (31.2) | |
| Cardiometabolic risk | ||||
| Z-score | -2.16 (4.40) | 0.42 (5.11) | 3.46 (6.06) | 0.0001c |
| Sedentary time (hours/week) | ||||
| ≤ 14.68 | 213 (33.4) | 92 (29.8) | 80 (23.9) | <0.001c |
| 14.68–25.35 | 212 (33.3) | 97 (31.4) | 98 (29.2) | |
| ≥ 25.35 | 212 (33.3) | 120 (38.8) | 157 (46.9) | |
| Glucose (mmol/L) | ||||
| Median (IR) | 4.66 (0.67) | 4.6 (0.61) | 4.72 (0.56) | 0.0474b |
| SBP (mmHg) | ||||
| Median (IR) | 95 (10) | 100 (20) | 105 (12) | 0.0001c |
| DBP (mmHg) | ||||
| Median (IR) | 60 (10) | 69 (10) | 70 (15) | 0.0001c |
| HDL (mmol/L) | ||||
| Median (IR) | 1.42 (0.47) | 1.32 (0.44) | 1.19 (0.47) | 0.0001c |
| LDL (mmol/L) | ||||
| Median (IR) | 2.61 (0.9) | 2.74 (0.85) | 2.79 (1.08) | 0.0001c |
| Triglycerides (mmol/L) | ||||
| Median (IR) | 0.8 (0.42) | 0.98 (0.62) | 1.27 (0.89) | 0.0001c |
| Total cholesterol (mmol/L) | ||||
| Median (IR) | 4.16 (1.13) | 4.16 (1.24) | 4.24 (1.32) | 0.0914 |
| Total energy intake kcal/day | ||||
| Median (IR) | 2525 (1,205.21) | 2475.62 (1,175.44) | 1175.44 (1,169.28) | 0.9281 |
Values are expressed in frequencies and percentages for categorical variables and in medians and interquartile ranges (IR) for quantitative variables.
HDL, high-density lipoproteins; LDL, low-density lipoproteins.
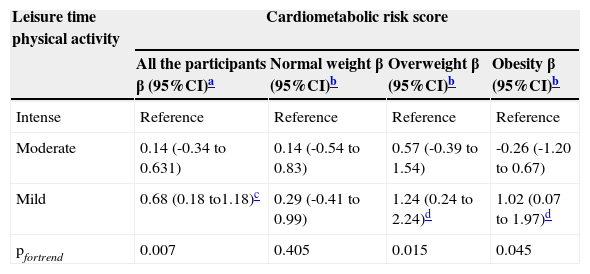
In the multivariate regression model, mild LTPA compared with intense LTPA increased significantly the cardiometabolic risk score (β MildvsIntenseLTPA: 0.68; 95% CI: 0.18 to 1.18; pfortrend=0.007). An interaction between nutritional status on the association of mild LTPA and the cardiometabolic risk score was found in the overweight and obese group (p=0.124 and 0.220, respectively). When stratified by nutritional status, a significant increase in cardiometabolic risk score was observed between overweight children that practice mild LTPA compared with those who practice intense LTPA (β MildvsIntenseLTPA: 1.24; 95% CI: 0.24 to 2.24; pfortrend=0.015). Also among obese participants, a similar trend in cardiometabolic risk score was observed between the practice of mild compared with intense LTPA (β MildvsIntenseLTPA: 1.02; 95% CI: 0.07 a 1.97; pfortrend=0.045), respectively (Table 2).
Linear regression model of LTPA and cardiometabolic risk score in the participants.
| Leisure time physical activity | Cardiometabolic risk score | |||
|---|---|---|---|---|
| All the participants β (95%CI)a | Normal weight β (95%CI)b | Overweight β (95%CI)b | Obesity β (95%CI)b | |
| Intense | Reference | Reference | Reference | Reference |
| Moderate | 0.14 (-0.34 to 0.631) | 0.14 (-0.54 to 0.83) | 0.57 (-0.39 to 1.54) | -0.26 (-1.20 to 0.67) |
| Mild | 0.68 (0.18 to1.18)c | 0.29 (-0.41 to 0.99) | 1.24 (0.24 to 2.24)d | 1.02 (0.07 to 1.97)d |
| pfortrend | 0.007 | 0.405 | 0.015 | 0.045 |
In this study, it was observed that children and adolescents that practice mild LTPA had a higher cardiometabolic risk score than their peers with intense LTPA. This association was observed especially among the overweight and obese participants. This finding is relevant for the population of interest, since it gives a rationale for increasing the practice of LTPA to prevent cardiovascular and metabolic complications in overweigh and obese children and adolescents, among whom, according to the evidence, excess BMI and waist circumference increase the likelihood of developing diabetes type 2 and cardiovascular diseases.6,19
The present results suggest that the practice of intense LTPA can play a protective role in the cardiometabolic risk in overweight and obese participants, finding that is consistent with previously reported results in overweight or obese children and adolescents, among whom the beneficial effect of physical activity on the different components of the metabolic profile has been shown.20 A meta-analysis found that aerobic exercise interventions among children or adolescents with obesity, hypercholesterolemia, or arterial hypertension reduce the levels of triglycerides by 3%, of SBP by 1.4%, of DBP by 0.4%, and increase C-HDL concentrations by 0.3%.10 Furthermore, a decrease of glucose and total cholesterol levels has been observed after at least four-week aerobic exercise interventions in this population group.20,21
A plausible biological explanation of the inverse association between LTPA and the cardiometabolic risk score observed in the present study could be attributed to the effect of the physical activity on the insulin resistance, adiponectin production, and endothelial function.22 The practice of sporadic or regular physical activity increases the content and translocation of the GLUT4 transporter and stimulates the production of insulin-sensitive muscle fibers.22 Experimental and observational epidemiological studies in children and adolescents have shown that aerobic exercise improves insulin dynamics in overweight or obese subjects,11 and that the practice of physical activity reduces the likelihood of insulin resistance in adolescents.23
Furthermore, research indicates that exercise interventions, with or without a dietary intervention, significantly increase serum levels of adiponectin in children and adolescents regardless of overweight status.24,25 The effect of physical activity on endothelial function has been demonstrated by the decrease of blood pressure and the improvement of the endothelial function and the anti-aterogenic activity;22 randomized clinical trials have shown that aerobic physical activity and resistance programs enhance the endothelial function in overweight or obese adolescents.26
The observed trend between the practice of LTPA and cardiometabolic risk in overweight and obese participants, where cardiometabolic risk significantly increased in participants who reported less LTPA, suggests a possible biological gradient between these two traits. The dose-response relationship has constituted a controversial result in the research on physical activity in children and adolescents.10 The reasons that account for the difficulty to establish dose-response relationships have to do with the variety of methods to measure the practice of physical activity, the absence of cut-off points for the cardiometabolic profile components, the lack of unifying criteria for the diagnosis of metabolic syndrome in this age group, and the variability of physical activity interventions conducted through the clinical trials.10
In the present study, an overweight and obesity prevalence that was higher than results published previously in children and adolescents from the city was observed.8,27 The possible explanation could be the different systems used to classify nutritional status in children and adolescents; in the present study, BMI Z-score cut-off points of the WHO were used. The literature indicates that the overweight and obesity prevalence found by the WHO criteria is generally higher than that established by Centers for Disease Control and Prevention (CDC) and the International Obesity Task Force (IOTF) criteria.28
The strength of this study lies in the size of the sample used, which reduces the probability of a type II error. This study is one of the first to be conducted in Mexico that evaluated the association between the practice of LTPA and the cardiometabolic profile by nutritional status in children and adolescents. These results constitute useful evidence to support the rationale that the practice of LTPA is a strategy to mitigate cardiometabolic risk in children and adolescents, particularly among those who suffer from overweight and obesity.
Nevertheless, the study has some limitations. Its cross-sectional nature limits the determination of a temporal relationship between the practice of LTPA and cardiometabolic risk in the population of interest. Therefore, the results should be interpreted cautiously. The sexual maturity of the participants was not taken into account; this is an important issue, given that physiological insulin resistance is characteristic to this stage of the vital cycle. However, this does not invalidate the present results, since insulin resistance per se does not account for the entire variability of the cardiometabolic risk in the age group of interest;19 additionally, the pubertal status is correlated with the age, and this variable was included in the model to adjust the results.
Finally, the authors believe there was a low probability of a differential report of the practice of LTPA using a frequency questionnaire, since the participants and the interviewers were blinded to the study hypothesis. Also, the use of a questionnaire for the measurement of the practice of LTPA is a limitation; however, it is important to point out that it is the instrument of choice to measure physical activity at the population level, especially in developing countries, due to its low cost,29,30 and its use is still valid in epidemiological studies.
In conclusion, an increase in the cardiometabolic risk score was associated with the practice of mild LTPA, especially in overweight and obese children and adolescents. This is an important result, due to the rapid increase in the prevalence of childhood overweight and obesity observed in the last years in this country. The practice of LTPA appears to have a positive impact, since it contributes to the prevention of cardiovascular and metabolic complications in overweight and obese children and adolescents, and therefore its practice could reduce the load of chronic disease at an early age.
FundingThis work was supported by the CONACYT SALUD-2005-C02-14412; SSA/IMSS/ISSSTE-CONACYT 2012 -180808, Proyectos Estratégicos IMSS 2004-3601-0020; Fundación IMSS, A.C., and the Gonzalo Rio Arronte Foundation.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Cárdenas-Cárdenas LM, Burguete-Garcia AI, Estrada-Velasco BI, López-Islas C, Peralta-Romero J, Cruz M, et al. Leisure-time physical activity and cardiometabolic risk among children and adolescents. J Pediatr (Rio J). 2015;91:136–42.