To investigate the relationship between lactate acid level and hospitalization mortality in neonatal necrotizing enterocolitis (NEC).
MethodPaediatric-specific critical care database collected clinical data from the intensive care unit of Children's Hospital Affiliated to Zhejiang University Medical College from 2010 to 2018. Clinical and laboratory examination information of NEC patients was collected and divided into the death group and discharge group to find out the risk factors affecting the prognosis through univariate and multivariate analysis.
ResultsAmong 104 NEC neonates, the admission age was 7.5 days and the weight was 2.03 kg. Comparing the death group with the discharge group, there were significant differences in therapeutic regimen, pH, serum albumin, total protein, creatinine and lactate acid. Multivariate and threshold effect analysis showed that lactate acid had a linear correlation with hospital mortality, and newborns who died in the hospital had much higher lactate levels than those who were discharged. The mortality of NEC newborns increased by 40–45% for every 1 mmol/L increase in lactate acid level.
ConclusionsThere was a correlation between lactate acid level and hospital mortality in newborns with NEC, and lactate acid level was an important index to evaluate the prognosis of NEC.
Neonatal necrotizing enterocolitis (NEC) is one of the most serious digestive diseases in newborns with high incidence and fatality, its mortality can be as high as 20–30%.1 The pathogenesis is complicated and not well defined. Prematurity, low birth weight, birth ischemia and hypoxia, intestinal flora imbalance and improper feeding methods are the main risk factors for NEC.2,3 Neonates, especially those with NEC, often suffer from hypoxemia and insufficient tissue perfusion. Blood lactate acid is an important index reflecting tissue hypoxia and low perfusion. Several studies indicate that the blood lactate level is significantly associated with in-hospital mortality of children.4-6 However, the lactate level change in NEC has rarely been studied.
PIC (Paediatric-specific critical care database (http://pic.nbscn.org)) is a large pediatric-specific, single-center, bilingual database established by the National Clinical Research Center for Child Health of China, contains clinical data of all children admitted to the Intensive care unit (ICU) between 2010 and 2018, on a total of 12,881 pediatric critically ill patients.7 PIC currently contains data such as: laboratory measurements from within the hospital, charted observations during a patient's stay in the intensive care unit, vital signs recorded while a patient is present in the operating room, and structured symptoms extracted from notes regarding the patient's stay. This study retrospectively analyzed the clinical data and laboratory indicators of patients diagnosed with NEC included in the PIC database to define the effect of lactate acid level on the outcome of newborns with NEC.
MethodsThe diagnosis was recorded by the International Statistical Classification of Diseases and Related Health Problems, 10th (ICD-10) system. In the ICD-10 system, p77.x00 represents NEC. The authors searched for p77.x00 in admission diagnosis and discharge diagnosis. Initially, 228 patients were enrolled in this retrospective cohort study. After duplicate checking according to the hospitalization number, 171 patients were included. The authors next excluded 66 patients with an ICU stay ≤ 2 days and 1 patient with congenital anal atresia. Ultimately, a total of 104 patients were included.
Diagnosis of NECNeonatal digestive system diseases often manifest as abdominal distension, hematochezia, vomiting and diarrhea, those symptoms need to be differentiated among NEC, congenital megacolon and congenital intestinal malrotation. The authors verified each newborn's main symptoms as well as the admission and discharge diagnoses one by one, to confirm that NEC was the main disease diagnosis rather than other digestive disorders. The authors excluded the patients who stayed in ICU for less than 2 days, because these patients died quickly due to serious illness, or got better after a short stay. Analysis of those patients could bias the results.
Primary outcomeThe outcomes of newborns were divided into the discharge group and the death group. Some newborns were hospitalized again due to enteritis and ileostomy after being treated and discharged from the hospital. The second admission records of these newborns will not be included. The outcome of their first hospitalization was considered as the discharge group, and the outcome of their second hospitalization was not considered. In the "Patient" project of the PIC dataset, death was selected as the outcome indicator. In the stage of NEC patients' inclusion, the authors confirmed that NEC was the main disease through the description of main symptoms, admission, and discharge diagnosis. Therefore, NEC in the diagnosis of discharge could be regarded as the cause of death.
Clinical data extractionGet permission to use the PIC database after completing the Collaborative Institutional Training Initiative (CITI) registration. The clinical data of the neonates were extracted in the PIC database based on the unique hospitalization number. The general data and laboratory indicators were taken into analysis including the day of admission, the weight of admission, gender, therapeutic regimen (operative treatment and conservative treatment), blood glucose, pH, albumin, total protein, C reaction protein (CRP), creatinine, lactate acid, total bilirubin, fecal occult blood test (FOBT), hemoglobin, white blood cell count (WBC), K+, Na+, Cl−. Following admission, routine blood and biochemical tests were performed repeatedly, and the worst value of indicators was used for statistical analysis.
Statistical analysisThe statistical analyses were performed using EmpowerStats and R software. All the data that fit into a normal distribution were expressed as the mean (SD), independent-sample t-tests were used for the group comparisons; median (IQR) was used for measurement data that did not conform to normal distribution, Wilcoxon rank sum test was used for comparison between groups; the counting data were expressed by cases and percentage, and χ2 test or Fisher exact test was used for comparison between groups. According to the results of the comparison between discharge and death groups, the laboratory indexes with statistical differences were extracted and analyzed. Univariate regression analysis was carried out for each laboratory index with a statistical difference, multivariate regression analysis was performed on indicators with linear correlation in the outcome. The results were expressed by OR value and 95%CI. After that, the authors further analyzed whether there had a curve relationship and threshold effect between outcome indicator and variable indicators. Segmented regression analysis, likelihood ratio test, and the bootstrap re-sampling analysis were used to segment the curve of variable value and analysis the relationship between line segments to assess the presence of a threshold effect. The difference was statistically significant with p < 0.05.
ResultsClinical dataA total of 104 neonates with NEC were included in this retrospective cohort study, including 9 (8.7%) in-hospital death and 95 improved discharge (including 12 secondary admissions). The average age from birth to admission to ICU was 7.5 (3,17) days. The weight at admission was 2.03 (1.67,2.71) kg. There were 34 female patients and 70 male patients. A total of 51 patients received surgical treatment, 53 patients received conservative treatment.
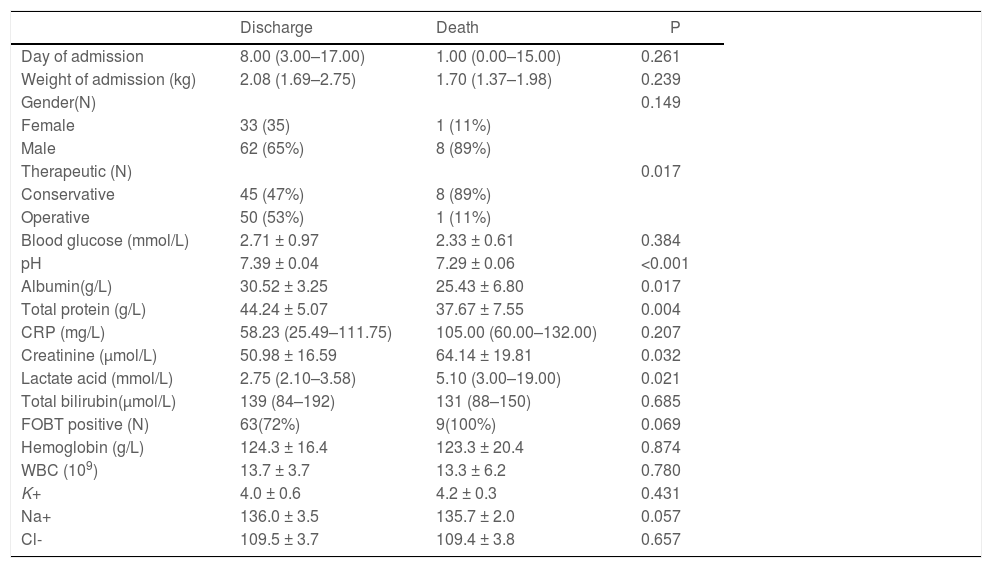
Comparison of clinical data for NEC patientsAccording to the outcome, the newborns were divided into two groups: the discharge group and the death group. Compared with the discharge group, there were significant differences in therapeutic regimen, pH, serum albumin, total protein, creatinine and lactate acid in the death group, but there was no significant difference in age, weight, gender, blood glucose, C-reactive protein, total bilirubin, electrolyte, hemoglobin and WBC (Table 1).
Clinical data of NEC newborns.
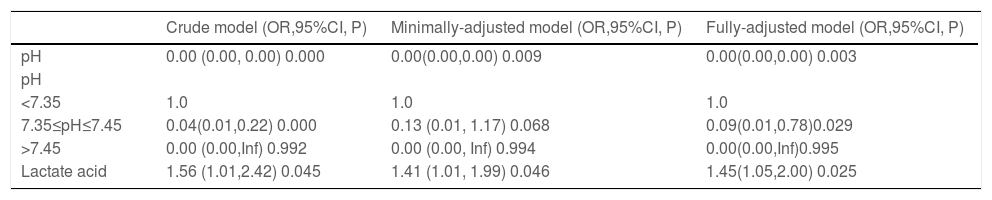
The authors took three steps to confirm the linear relationship between the mortality of NEC patients and pH or lactate acid. First, the pH and lactate acid were used for regression analysis. Then the age, weight and gender were included in the regression analysis, finally, the covariances with a statistical difference including the therapeutic regimen, serum albumin, total protein, and creatinine were further involved in the regression analysis. As the results of univariate analyses may be affected by confounding factors. Multivariate regression analysis was adjusted for the indicators that were significant in univariate analysis. In the process of analyzing pH, the results of univariate and multivariate analysis showed that pH was significantly related to the mortality of NEC. However, due to the characteristics of pH, it can be divided into three situations: low-pH, optimal-pH, and high-pH. After stratified analysis, the authors could see that the results of mortality related with pH were not stable and reliable. Both univariate and multivariate analyses showed that lactate acid was significantly correlated with mortality. The Fully-adjusted model showed that for every 1 mmol/L increase in lactate acid the risk of mortality increased by 45% in NEC patients (OR = 1.45) (Table 2).
The relationship between NEC, pH, and lactate acid in different models.
Crude model: not adjust other covariants.
Minimally-adjusted model: adjust for age, weight, gender.
Fully-adjusted model: Adjust for albumin, total protein, therapeutic regimen, creatinine on the basis of Minimally-adjusted model.
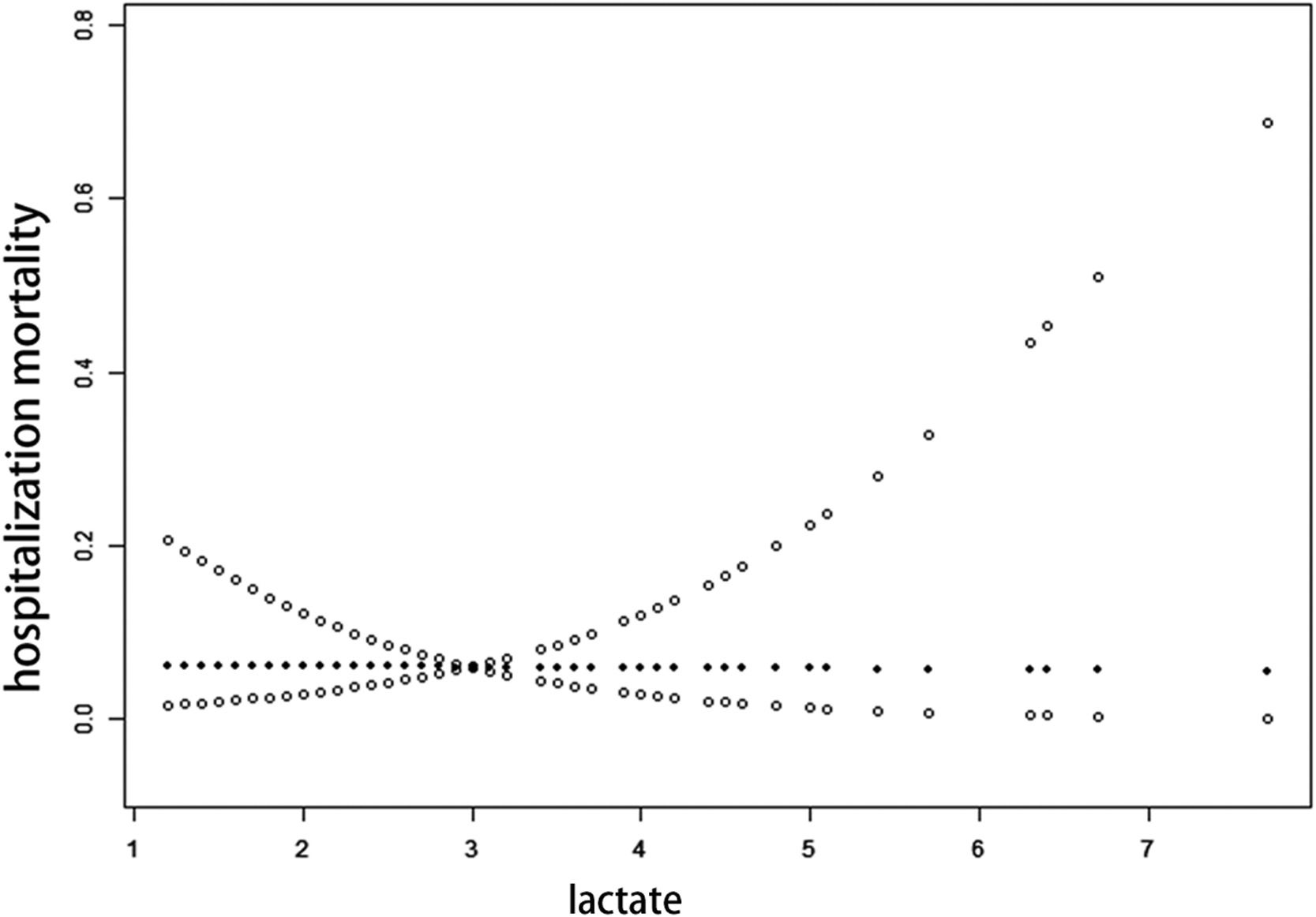
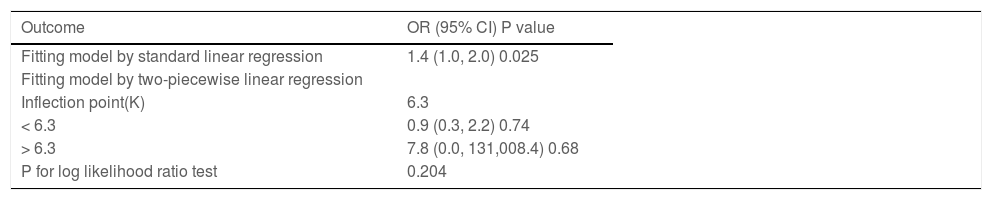
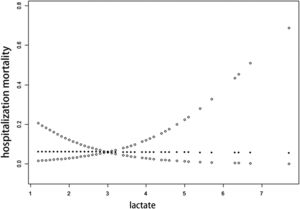
To further define the range of lactate acid change as a function of mortality in NEC patients, the authors analyzed the range of lactate changes as a function of mortality through a threshold effect, which showed that there was no obvious threshold effect between lactate acid and NEC mortality, but there was a significant linear relationship between them. Assuming a curvilinear relationship between lactate and mortality in NEC, the authors divided lactate into two straight lines which were less than 6.3 mmol/L and greater than 6.3 mmol/L. The P value of the likelihood ratio test showed that there was no statistical difference between the two lines, which indicated that the relationship between lactate acid and mortality was linear rather than curvilinear (p = 0.204). OR values indicated that each 1 mmol/L increase in lactate acid was associated with a 40% increase in mortality of NEC patients (Figure 1, Table 3).
In order to confirm the relationship between lactate acid level and mortality, the authors further analyzed the results of repeated measurements of lactate acid. All the repeated measurements of lactate acid were included, and both groups measured lactate acid frequency equally (p = 0.28) (Supplementary A). The repeated measurement results showed that the lactate acid level in the discharge group was 1.95 ± 0.55 mmol/L, and 3.46±1.96 mmol/L in the death group. The difference between the two groups was statistically significant (p<0.0001).
DiscussionThe mortality of NEC is extremely high. The main symptoms at admission are abdominal distension, bloody stool and vomiting, which makes it difficult to diagnose at the early stage. Unfortunately, NEC often develops into peritonitis, intestinal perforation and septic shock rapidly. The pathogenesis of NEC is complex, which is related to many factors such as preterm delivery, improper feeding, hypoxic-ischemic injury, and flora imbalance.8,9 Current studies have shown that preterm delivery and low birth weight, low Apgar score, neonatal pneumonia, and the use of indomethacin in the treatment of patent ductus arteriosus can increase the risk of NEC in infants.10,11 However, research on the influencing factors of prognosis is not sufficient. In the present study, all the newborns included were hospitalized in the intensive care unit, which was more complex in development and general condition. The present study does not only concerns the factors related to the prognosis of NEC, but more importantly, the authors explore the influence of lactate acid change on the mortality of NEC newborns.
Critical illness databases such as Medical Information Mart for Intensive Care (mimic), eICU (combination of critical care units throughout the United States) collect a large number of clinical information on critically ill patients and provide a rich source of research data for numerous investigators worldwide. However, these data are mainly for adults, and there is no special database for data collection and analysis of children or adolescents in the world. Obviously, it is inappropriate to apply the research results of adult patients to pediatric patients. PIC database relies on Zhejiang University Children's Medical Center, which contains information on a total of 13,499 admissions in 12,881 pediatric patients, is currently the largest clinical data database for children worldwide.7 In this study, the outcome and laboratory indicators of patients with NEC were extracted for prognostic analysis.
In this study, it was found that there was a significant linear correlation between lactate acid and the mortality of newborns with NEC. Univariate and multivariate regression analysis showed that the OR value was 1.45, and the threshold effect analysis showed that OR value was 1.4. The results were similar which suggested that when lactate acid increased 1 mmol/L, the mortality increased by about 40–45%. Although the mechanism leading to NEC is complicated, the pathophysiological process behind them is defensively reflex blood redistribution, decreased blood flow and intestinal mucosal ischemia and necrosis and further developed into intestinal mucosal barrier dysfunction and intestinal bacterial translocation. Blood lactate acid level is an indicator that sensitively reacts to tissue perfusion and hypoxia. There was a high mean difference in blood lactate levels between severe and mild malaria patients. Among patients with severe malaria, there were also significant differences in blood lactate acid values between dead and surviving patients.12 Lactate acid greater than 36 mg/dL was associated with mortality of sepsis children in the emergency department.4 One systematic review evaluated 96 clinical studies, including patients with sepsis, trauma or after cardiac surgery and found that lower blood lactate acid levels were associated with better clinical outcomes.13 Treatment for NEC could change the blood lactate acid with the ultimate aim of maintaining tissue perfusion. Blood lactate acid level maintained at a high level often indicates that the organ and tissue perfusion failed to be improved or had a trend to get worse.14,15 The present study observed a significant association between high lactate acid levels with higher mortality of NEC patients. In the death group, the lactate acid level is significantly higher than in the discharge group, regardless of repeated measurements or the worst test result.
In between-group analysis, there was no statistical difference in admission age and weight. This seemed to be inconsistent with previous research.16 The reason might be that the patients the authors included were from the pediatric intensive care unit with the poor general condition. The difference might not appear obvious for critically ill children in the ICU, as all the infants have low body weight (Supplementary B, C). In between-group analysis, there were statistical differences in albumin, total protein, pH, creatinine, and therapeutic regimen. As albumin accounts for more than 50% of total protein, which is an important nutrient for the human body and studies proved that serum albumin correlated with the development and prognosis of necrotizing enterocolitis.17,18 Hikaru extracted clinical data from 1505 children in the PIC database based on creatinine levels and found that hyperlactatemia, low pH, and hypocapnia were associated with 28-day mortality in children with acute kidney injury.19 Sepsis decreases lactate acid clearance. A high pH value may further slow lactate acid clearance.20 These laboratory indicators were also important biomarkers in NEC.
The most important limitation of this study is the retrospective design, which leads to missing and incomplete data. Since the status of infants at birth was not recorded, the dataset could not capture information about the circumstances of birth and delivery. A large number of studies have confirmed that prematurity, low birth weight and low Apgar score at 5 min are the major risk factors of NEC.21-23 Thus, by not considering gestational age and birth weight, the true impact of lactate on NEC outcomes is not accurate enough. More research is needed to conclude whether evaluating prognosis by lactate value is generally applicable.
Based on the PIC database, through the analysis of lactate acid level and hospital mortality in NEC newborns, it was found that each increase in 1 mmol/L of lactate acid increases the mortality by 40–45%. Lactate acid is widely well-recognized as an important clinical indicator by most clinicians. However, research on lactate acid in neonatal intensive care units is rare, and this study could complement this field. These findings can provide a reference and basis for the evaluation of clinical mortality for NEC. Further, the present results indicate that early and active correction of acidosis is beneficial to survival and crucial for treatment success.
ConclusionThe present findings suggested that the lactate acid level was related to the hospital mortality in NEC patients, and the neonatal mortality increased by 40–45% for every 1 mmol/L increase in lactate acid level.
Ethics approval and informed consentThe establishment of this database was approved by the Massachusetts Institute of Technology (MIT), and data used in this study were de-identified in accordance with Health Insurance Portability and Accountability Act (HIPAA) standards. The data was fully anonymized by removing all HIPAA to protected health information identifiers that could uniquely identify the individual in structured data sources. Applicants must sign an agreement to ensure data security and protect privacy. Therefore, the ethical approval statement was waived for this study. The informed consent was waived because of the retrospective nature of this study. And procedures were conducted according to the Declaration of Helsinki.
Availability of data and materialsData can be downloaded from http://pic.nbscn.org/
Authors' contributionsYuting Wang and Lei Zheng participated in the design of the study, and wrote the main manuscript. Yuting Wang and Lifei Lai were responsible for downloading and sorting data. Qi Zhang participated in statistical analyses.
Funding sourcesThis work was supported by the National Natural Science Foundation of China. (No.82070072).
The authors acknowledge the PIC database for providing their platforms and contributors for uploading their meaningful datasets.