To verify if the connection of electrodes for heart and transcutaneous oxygen monitoring interfere with the measurement of electrical bioimpedance in preterm newborns.
MethodsThis was a prospective, blinded, controlled, cross-sectional, crossover study that assessed and compared paired measures of resistance (R) and reactance (Xc) by BIA, obtained with and without monitoring wires attached to the preterm newborn. The measurements were performed in immediate sequence, after randomization to the presence or absence of electrodes. The sample size calculated was 114 measurements or tests with monitoring wires and 114 without monitoring wires, considering for a difference between the averages of 0.1 ohms, with an alpha error of 10% and beta error of 20%, with significance <0.05.
ResultsNo differences were observed between the R (677.37±196.07 vs. 677.46±194.86) and Xc (31.15±9.36 vs. 31.01±9.56) values obtained with and without monitoring wires, respectively, with good correlation between them (R: 0.997 and Xc: 0.968).
ConclusionThe presence of heart and/or transcutaneous oxygen monitoring wires connected to the preterm newborn did not affect the values of R or Xc measured by BIA, allowing them to be carried out in this population without risks.
Verificar se a conexão de eletrodos e fios de monitoração cardíaca e transcutânea de oxigênio interferem na aferição da bioimpedância elétrica em recém-nascidos pré-termo (RNPT).
MetodologiaEstudo prospectivo, cego, randomizado, transversal, crossover, em que foram mensuradas e comparadas medidas pareadas de resistência (R) e reatância (Xc) por meio da BIA, obtidas com e sem os fios de monitoração acoplados aos RNPT. As medidas foram feitas em sequência imediata, após aleatorização para a presença ou ausência dos eletrodos. O tamanho amostral calculado foi de 114 aferições ou exames com fios de monitoração e 114 sem fios de monitoração, considerando para uma diferença entre as médias de 0,1 ohms, com erro alfa de 10% e erro beta de 20%, com significância<0,05.
ResultadosNão foram observadas diferenças entre os valores de resistência (677,37±196,07 vs 677,46±194,86) e reatância (31,15±9,36 vs 31,01±9,56) obtidos com e sem fios de monitoração respectivamente, com boa correlação entre ambos (resistência:0,997 e reatância:0,968).
ConclusãoA presença de fios de monitoração cardíaca e/ou transcutânea de oxigênio não interferiu nos valores da resistência ou da reatância aferidos pela BIA em RNPT. Recomenda-se, então, esse exame, sem riscos, para essa população.
Among the methods used for assessing body composition, bioelectrical impedance analysis (BIA) has been widely used, especially for being non-invasive, painless, practical, safe, low-cost, and easily performed at the bedside. Another reason for its use is the fact that it estimates, in addition to body components, the distribution of fluids in the intra- and extracellular spaces, as well as the quality, size and integrity of cell membranes.1,2 It can be repeated as often as necessary, thus allowing for the follow-up of patients of different ages, body weight, and health status.
It is therefore a promising tool to be incorporated into clinical research and routine evaluation of patients from different medical specialties, including neonatology.3
Currently, in addition to the limited data available on BIA in newborns, mainly preterm ones, there is no consensus on the methodological standardization of this exam for this population.4 For instance, it has been suggested that being attached to a monitoring wire precludes the performance of the BIA. However, the continuous monitoring of several physiological parameters is required to maintain the safety of newborns in intensive care.
The objective of this study was to verify whether, in fact, the presence of electrodes and wires for heart and transcutaneous oxygen monitoring attached to preterm newborns interfere with the values of resistance (R) and reactance (Xc) measured by BIA.
MethodsThis was a prospective, blinded, randomized, crossover study that compared measurements made by BIA for the evaluation of R and Xc in preterm infants with and without heart and transcutaneous oxygen monitoring wires.
The test was standardized as follows: the internal electrode (detector – red color) of the arm was placed on the dorsal surface of the right wrist between the ulnar and radius bones, whereas the outer electrode (emitter – black color) was placed on the third metacarpal; the internal leg electrode was placed on the anterior surface of the right ankle, between the prominent portions of the bones, whereas the external was placed on the surface of the third metatarsus.5
During the examinations, both the examiner and the parents/guardians were asked not to touch the newborn, who was placed on the dorsal position, with the limbs separated, without touching metal, to avoid reduction/random dispersion of electric current. The examination lasted approximately 5min.
The collection was carried out for 1h and 30min after the end of the feeding, to prevent the manipulation of the newborn from causing emetic episodes or interfering with digestion. The preterm newborns were carefully observed by the researcher throughout the examination period.
The R and Xc measurements were performed using the single-frequency equipment (BIA 101 Quantum II – RJL Systems, USA), which applies a sinusoidal alternating current of 50kHz and 800μA.1
The measurements were performed in immediate sequence, after drawing lots for randomization of the presence or absence of electrodes (“yes” or “no” raffle). When assessing the database, the presence or absence of monitoring wires connected to the newborn was not known by researchers and/or statistician, i.e., the analysis was blinded.
The study included all preterm infants with gestational age (GA) between 24 and 36 weeks and six days, who were hemodynamically stable and could stay for at least 10min without heart and transcutaneous oxygen monitoring. Infants on mechanical ventilation were not assessed, as the authors believed it would be too risky to keep them without monitoring, even for a few minutes.
All preterm infants with congenital malformations, hemodynamically unstable, and those receiving vasoactive drugs were excluded from the study, as well as those whose families refused to participate.
The sample size of 114 measurements or tests with monitoring wires and 114 without wires was calculated for a difference between the means of 0.1 ohms, with an alpha error of 10% and beta error of 20%.
The variables were presented by measures of central tendency and analyzed by paired t-test. A significance level ≤5% was used and the data were analyzed using SPSS (SPSS Inc. Released 2007. SPSS for Windows, Version 16.0, USA).
The study was approved by the Research Ethics Committee (REC), registered under No. 193/2010, CAAE No. 0153.0.258.000-10.
ResultsA total of 114 measures were carried out in preterm infants attached to heart and transcutaneous oxygen monitoring wires, as well as 114 measures in preterm newborns not attached to these wires. Altogether, 90 newborns were assessed, of whom 70 were evaluated once, 16 were evaluated twice, and four were evaluated three times, with a minimum interval of one week between measurements.
The birth weight (BW) of the participants ranged from 630g to 1980g. Of these, 7% had BW between 500g and 750g; 10%, between 751g and 1000g; 51%, between 1001g and 1500g; and 33%, between 1501g and 2000g. On average, the assessments were performed in preterm infants with chronological age of 15 days (range 9–33 days).
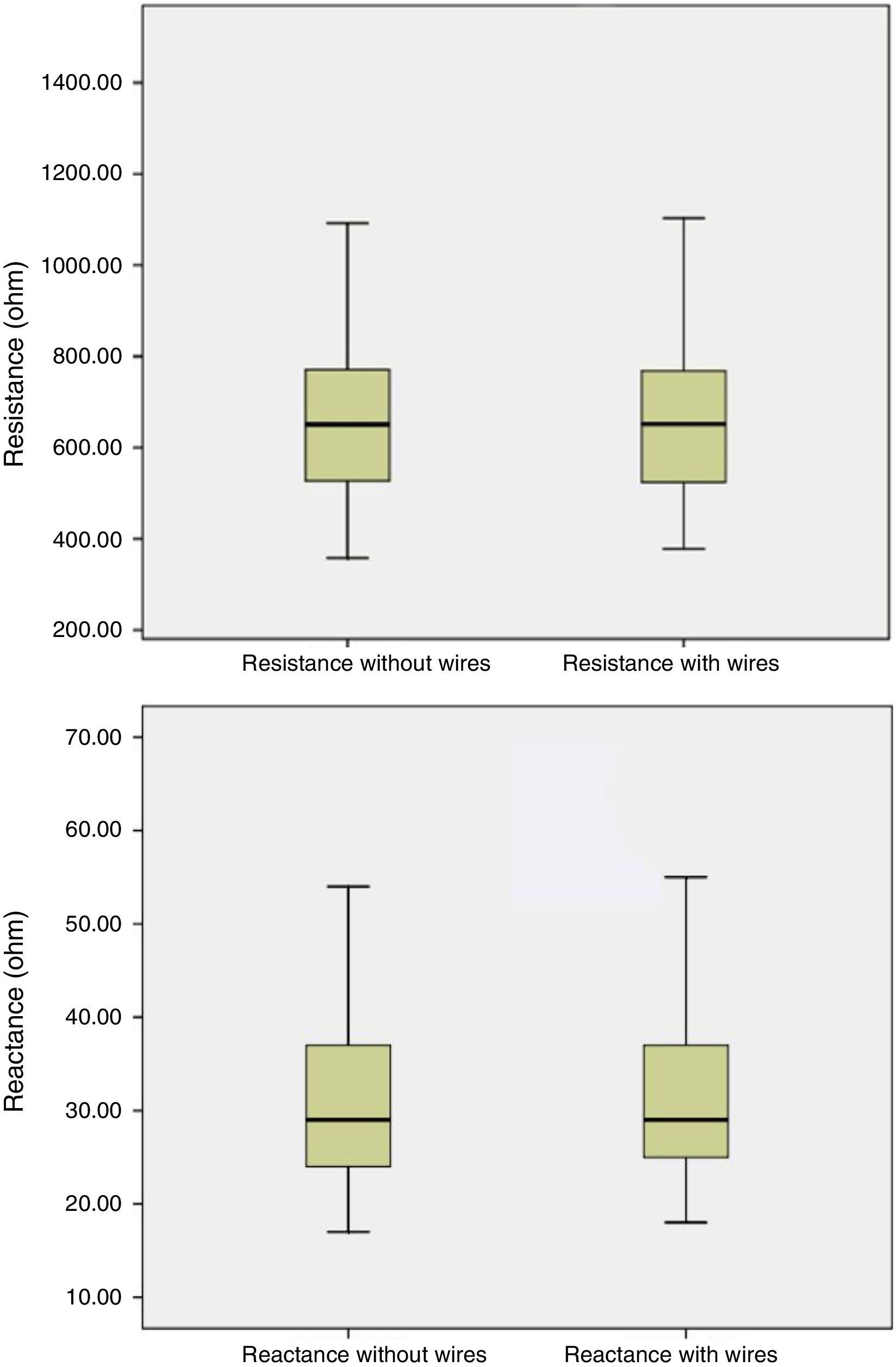
No differences were observed between the R and Xc values obtained with and without monitoring wires, with a good correlation between measurements (Fig. 1). Means and standard deviations of the R measured with and without the presence of electrodes for heart and oxygen saturation monitoring were 677.37±196.07 and 677.46±194.86 ohms (p=0.952), respectively; the means of Xc were 31.15±9.56 and 31.01±9.56 ohms (p=0.532), respectively. The correlations between the paired measures of R and Xc were, respectively, 0.997 and 0.968 (p<0.001).
DiscussionThe results of this study make it clear that the presence of electrodes for heart and transcutaneous oxygen saturation monitoring attached to the preterm infant does not interfere with R and Xc measurements performed by single-frequency equipment.
In studies conducted in the adult population, Foster and Lukaski affirmed that, although the electric fields that are induced by the BIA in the body are much lower than those of the susceptibility limits of devices such as implanted pacemakers and defibrillators, in the absence of a detailed safety analysis, it is wise to avoid performing body impedance measurements in individuals with such devices.6 It is believed that there could be a dispersion of the electric current induced by BIA, mainly of electrodes for heart monitoring, as they are suitable for sensing the electrical variations produced by heart muscle depolarization.
In turn, Kyle et al. state that, although bioimpedance interference has not been verified in pacemakers and defibrillators, heart monitoring is recommended in these cases; when monitoring is not possible, bioimpedance is contraindicated.7
Studies carried out by Lingwood et al., in adult and neonatal populations, show that single-frequency devices are susceptible to significant interference and the possibility of errors when used in newborns and adults attached to monitoring equipment necessary in an intensive care scenario.8–10 These studies, in addition to having a small sample size, were carried out with a different methodology than the current study.
The present authors believe that there was no dissipation of electrical current through electrodes attached/applied to the skin of the newborns, or if there was, it was small enough not to generate statistically significant differences.
In the current study, which aimed to evaluate interference on BIA measurement technique in a specific population, the use of paired mean comparison analysis, i.e. one measure taken twice from the same subject, completely refutes the possibility of interference of the research subject on the results. That is, it gender, gestational age, weight, or any other characteristic of the assessed newborns were irrelevant, as they were their own controls. Moreover, the calculation of sample size greatly increases the power of the statistical test used.
Newborns, in general and, more precisely, those preterm, are susceptible, shortly after birth, to a very severe loss of body water. When they are healthy, their organs can cope well with these losses and generate homeostatic balance rapidly. However, in critically-ill or very premature newborns, this homeostatic balance can be severely damaged.
Preterm infants are also more likely to develop some conditions that correlate either with excessive administration of fluids, such as bronchopulmonary dysplasia and patent ductus arteriosus, or hypovolemia, such as arterial hypotension and metabolic acidosis. Therefore, a strict control of fluid and electrolyte balance is essential in the clinical management of preterm infants.11
The possibility of assessing critically-ill newborns in neonatal intensive care units without exposing them to the risk of being without monitoring, even for a few minutes, makes it possible to add to neonatal care an easy-to-use, noninvasive tool with very interesting research possibilities.
The measurement of total body water and its variations, the inference of volumes of other body compartments, among others, increases an entire arsenal of data rapidly available at the bedside to help in the clinical decisions of neonatologists.12 Additionally, these data are crucial in a population that, up to now, has many gaps in the understanding of their fluid homeostasis.
Currently, R and Xc measurements obtained by BIA are used for analysis of the bioelectrical impedance vector (BIVA). In this analysis, the use of formulas or mathematical models is not required, and it is believed that it is only affected by a measurement error and the biological variability of the assessed subjects. A vector is plotted from the measurements of R and Xc, and this vector is compared with a known reference population. By determining the vector position and angle, called phase angle, one can determine, among others, the degree of normality of the individual's fluid distribution, clinical severity and even predict the associated mortality.2,12–14
Many questions still remain regarding the optimal methodology to analyze R and Xc in the pediatric and neonatal population. Even the use of BIA to calculate total body water and of other body compartments is criticized, as there are no validated literature equations for children younger than 6 years.1,7 However, the authors have not found an easier method than BIA to be applied at the bedside.
The definition of a single standard for the performance of BIA measures in preterm infants is important for its validity, allowing for comparison and interpretation of results.
In conclusion, the use of single-frequency BIA to measure R and Xc in preterm infants did not suffer interference from the electrodes used for heart and transcutaneous oxygen saturation monitoring in the assessed population.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Comym VC, Macedu YS, Neves EK, Bueno AC, Fernandez HC, Moreira ME, et al. Interference of heart and transcutaneous oxygen monitoring in the measurement of bioelectrical impedance analysis in preterm newborns. J Pediatr (Rio J). 2016;92:528–31.
Study carried out at Universidade Federal Fluminense, Niterói, RJ, Brazil.