To verify the effects of an intervention program including physical exercise and recreational activities, as well as nutritional counseling, on the health-related quality of life of obese children.
MethodsThis was a controlled clinical trial. The initial study population included children aged eight to 11 years with a body mass index (BMI) > 97th percentile for age and gender, according to the criteria of the World Health Organization, totaling 44 children matched by gender and age, as case (n = 22) and control groups (n = 22). BMI and self-reported health-related quality of life by Pediatric Quality of Life Inventory were measured before and after 12 weeks of intervention (three times weekly). The control group did not participate in the intervention.
ResultsThirty-two children completed the study (16 in each group). The case group showed significant reduction in BMI (p = 0.001) and improved quality of life in the physical (p = 0.001), emotional (p = 0.014), social (p = 0.004), and psychosocial (p = 0.002) domains, as well as in overall quality of life (p = 0.001), which was not observed in the control group.
ConclusionThe program was effective in improving the health and quality of life of obese children.
Verificar os efeitos de um programa de intervenção com exercício físico, atividades recreativas e orientação nutricional na qualidade de vida relacionada à saúde de crianças obesas.
MétodosTrata-se de um ensaio clínico controlado. A população inicial do estudo envolveu crianças com idades entre oito e 11 anos e com índice de massa corporal acima de 97 percentil por idade e sexo, conforme os critérios da Organização Mundial de Saúde, totalizando 44 crianças pareadas em sexo e idade, sendo: grupo caso (n = 22) e grupo controle (n = 22). Determinou-se, antes e após 12 semanas de intervenção (três vezes semanais), o índice de massa corporal e a qualidade de vida relacionada à saúde autorrelatada pelo questionário PedsQL. O grupo controle não participou da intervenção.
ResultadosCompletaram o estudo 32 crianças (16 em cada). O grupo caso apresentou redução significativa do índice de massa corporal (p = 0,001) e melhorou a qualidade de vida nos domínios físico (p = 0,001), emocional (p = 0,014), social (p = 0,004), psicossocial (p = 0,002) e qualidade de vida geral (p = 0,001), o que não foi observado no grupo controle.
ConclusãoO programa foi efetivo na melhora da saúde e da qualidade de vida de crianças obesas.
The increasing worldwide prevalence of obesity in children and adolescents is a matter of concern, considering its association with several comorbidities, among them cardiovascular disease.1 In addition to its association with diabetes mellitus type 2, hypertension, dyslipidemia, acute myocardial infarction and stroke,1 childhood obesity also appears to be involved in psychological and social consequences, as it may impair the self-esteem of young obese individuals and may result in psychological consequences in the long term.2 Studies have shown an association between low quality of life and obesity in childhood and adolescence.3–6
Poor eating habits, sedentary lifestyle, and genetic predisposition are possible factors related to the development of obesity in young people. The practice of regular physical activities can prevent the onset of this condition. In addition to the benefits in the prevention and treatment of diabetes, obesity, metabolic syndrome,7 and improvement of the lipid profile,8,9 physical activities can also have an impact on the health-related quality of life of obese children and adolescents.10
The benefits of physical exercise and nutritional counseling on obesity are known in the young population.9,11 Other studies have shown positive effects of physical exercise with recreational activities and nutritional guidance on the components of metabolic syndrome12 and body mass index (BMI) of obese children.13 The benefits of exercise on quality of life are also highlighted; however, none of these studies were conducted in Brazil,3,10,14,15 and one was performed with a similar methodology as used in the present study.10
Considering the gaps, this study assessed the effects of an intervention program with physical exercise and recreational activities combined with nutritional counseling on the health-related quality of life of obese children.
MethodsThis was a controlled clinical trial. The initial population of the study involved children aged between 8 and 11 years and with BMI above the 97th percentile for age and gender, according to the criteria of the World Health Organization (WHO), thus considered obese.16 The children were consecutively recruited from the Pediatric Cardiology Outpatient Clinic of the Hospital Infantil Joana de Gusmão (HIJG) of Florianópolis/SC, Brazil (a state referral center for this disease), in the period January-July 2009. The inclusion criteria were obese children between 8 and 11 years of age treated at HIJG and residents of Florianópolis/SC. The exclusion criteria were participation in any weight loss program, or physical or mental disability. All children that met the inclusion criteria and who sought treatment during this period were invited by the physicians of the institution to participate in the study. During the recruitment period, approximately 120 obese children aged 8 to 11 years were attended to at the outpatient clinic, and of these, approximately 90 met the inclusion criteria.
The head researcher was contacted by 77 parents of children who showed interest in participating in the program. Of these, 32 children studied in the morning and 45 in the afternoon. Due to logistical reasons, the program was held in the afternoon. Thus, children who studied in the morning were allocated to the case group (intervention participants) (n = 32), and those studying in afternoon were allocated to the control group, respecting the pairing for gender and age (n = 45). Losses that occurred between the initial contact and the beginning of the program totaled ten in the case group and 23 in the control group. Thus, each group initially consisted of 22 children, totaling 44 matched obese children. Children in the control group did not participate in the intervention; however, they maintained the conventional treatment (monitoring and traditional medical treatment). All children were instructed to maintain their usual activities during the study period and were advised by the hospital medical staff regarding the practice of physical activity and nutritional guidance during follow-up.
This study is part of a larger study,17 which used a clinically significant difference in systolic blood pressure of 15mmHg and a standard deviation of 15mmHg in the population of obese children to calculate the sample size, with type I error of 5% and type II error of 20% (pilot study), as this is the most important risk factor and the one that determines early cardiovascular consequences in childhood and adolescence.18 Considering these parameters, the minimum sample size was 16 subjects in each group. To this number, 25% were added for potential losses and refusals, which coincided with the number of children that participated until the end of the study.17
After the start of the program, the following exclusion criteria were used: children from the case group who did not attend at least 90% of sessions, whether or not these sessions were regular, 19 and/or those whose parents or guardians did not participate in the nutrition guideline sessions; children from the control group whose pairs from the case group failed to participate in the intervention or were excluded from analysis.
ProceduresAll children underwent health-related anthropometric, demographic, clinical, and quality of life assessments that were self-reported in the hospital during the morning, from 7:30 AM to 12 PM, from one week before to one week after the start and end of program.
To characterize the sample, a questionnaire on sociodemographic and clinical aspects, which was completed by the child's parent or guardian, was applied. In addition, information on sexual maturity (pubic hair), determined according to the model proposed by Tanner, was collected.20
An electronic scale with a 100-gram resolution, calibrated before the measurements, was used to measure body mass. Children were weighed standing barefoot, wearing shorts and T-shirts. A portable stadiometer with a 1-mm resolution fixed to a wall without baseboard was used to measure height, taking as reference points the vertex and the plantar regions, following the procedures described by Lohman.21 BMI was determined by the formula: weight (kg) divided by height (m) squared. Anthropometric measurements were performed twice by the same examiner, using a third measurement and calculating the mean, in case of disagreement.
The Pediatric Quality of Life Inventory (PedsQL 4.0, generic version for children22) was used to assess the health-related quality of life, after being validated for the Brazilian population.23 The PedsQL 4.0 comprises 23 items divided into four domains (physical, emotional, social, and school). Questions are answered according to a scale from 0 to 4 (never, almost never, sometimes, many times/often, almost always) and regarding the last month experienced by the child. The items are measured and converted to a linear scale from 0 to 100, yielding a mean; the higher the score, the better the quality of life.22 The overall quality of life is determined by the mean of all domains, while the psychosocial aspect is determined by the mean score of the social, emotional, and school domains. The questionnaire was designed to assess the dimensions of physical, mental, and social health, following the proposal of the WHO, considering the role of the school domain.23 The instrument has two parallel questionnaire formats, one for children and one for parents. This study considered only the version for children (self-report).
Intervention programThe intervention program consisted of physical exercises with recreational activities, and nutritional counseling to children and parents, for 12 consecutive weeks. The physical exercises were performed in a gym and on a field (twice weekly) and a pool (once weekly), at the Sports Center (Centro de Desportos –CDS) of the Universidade Federal de Santa Catarina (UFSC), Brazil. Nutritional guidelines were given in a classroom of the CDS/UFSC (one session per week). The exercises were performed in three weekly sessions, lasting 60minutes each, totaling 36 sessions. Each session consisted of stretching/warm-up (5-10minutes), aerobic exercises (40-45minutes), and cool-down (5-10minutes). The exercises were pre-programmed, developed by two physical education professionals and one physical education student, and consisted of moderate to vigorous intensity recreational activities.12,19 The main focus of the planned activities was recreational and aerobic characteristics. Some examples of activities were: pre-sports games (mini-soccer, mini-handball, mini-basketball, swimming, mini-water polo, athletics); adapted games; dynamic outdoor activities (tracks); jumping on a trampoline; walking; jogging; jumping rope; dancing; tug-of-war; explosive races; relays; abdominal crunches; and stretching.
The physical exercises were performed aiming at an intensity of 65% to 85% of maximum heart rate (MHR),19 determined by the formula (MHR = 208-0.7 x age).24 The heart rate was followed individually through a Polar heart rate monitor (S610i) during all activities, seeking to ensure its maintenance within the recommended range.
Nutritional counseling was performed by a nutritionist and a group of nutrition students from UFSC, and consisted of weekly meetings with parents and children with educational and informative purposes, aiming to encourage them to adopt healthier eating habits. During these meetings there were lectures on nutrition education, using the adapted Brazilian food pyramid,25 as well as games and activities related to the theme. Guidelines on healthy cooking were also provided.
Descriptive statistics procedures were initially performed when analyzing the data. Student's t-tests for paired and unpaired samples were used for the analysis of data with normal distribution (anthropometric data), whereas the Wilcoxon test and Mann-Whitney's U-test were used for the analysis of data with non-normal distribution (data related to quality of life). All statistical analyses were performed using the Statistical Package for Social Sciences (SPSS) 17.0, and the significance level was set at p < 0.05.
This study was approved by the Ethics Committee of the –UFSC, under protocol No. 302/08. After the end of the study, all children continued to receive medical follow-up at the local hospital.
ResultsOf the 44 children who started the program, six cases were lost on follow-up. As the subjects were matched, their respective pairs in the control group were excluded, totaling 16 in each group (8 males and 8 females in each). When compared to the initial profile, there were no significant differences in relation to all analyzed variables between participants who completed or abandoned the study (p > 0.05).
The mean age in the study group was 9.6 years and 9.4 years in the control group (p = 0.890). All children attended public schools in the city of Florianópolis, state of Santa Catarina, had physical education classes three times a week, and were at prepubertal and pubertal stages. Most belonged to families with monthly incomes between two and five Brazilian minimum wages. In the case group, the time devoted to watching television or using the computer was 3.6±1.8hours/day, and in the control group, it was 3.1±1.5hours/day, with no significant difference between the groups (p = 0.460). In the case group, one child was medicated for nephrotic syndrome and one for gastroesophageal reflux. In the control group, one child was medicated for hypertension, one for depression, and one for bronchial asthma. The remaining children did not use any drugs regularly.
The comparative analysis of BMI and the quality of life domains demonstrated no statistically significant differences between the case and control groups in the pretest: BMI (p = 0.258), physical (p = 0.232), emotional (p = 0.295), social (p = 0.464), school (p = 0.502), and psychosocial domains (p = 0.473), as well as overall quality of life (p = 0.291). However, in the post-test, there was a difference between groups in the physical (p < 0.001), emotional (p = 0.030), social (p = 0.007), and psychosocial (p = 0.002) domains, as well as overall quality of life (p < 0.001), with higher values in the case group. The groups did not differ in BMI (p = 0.060) and in the school domain of quality of life (p = 0.201) in the post-test period.
It was observed that the case group presented, at the end of the program, a significant reduction in BMI (p = 0.001), from 26.4kg/m2 (95% CI = 24.55 to 28.59) to 25.5kg/m2 (95% CI = 23.47 to 27.54). Although there was no statistically significant difference (p = 0.078), the BMI of the control group increased from 28.3kg/m2 (95% CI = 25.62 to 31.14) to 28.7kg/m2 (95% CI = 25.98 to 31.47). All children remained above the 97th percentile.16
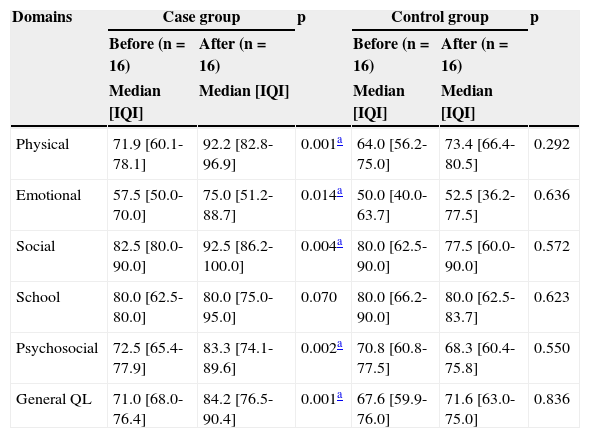
Table 1 shows the results of the program impact on the health-related quality of life domains. It was observed that the case group showed significant improvement in the physical, emotional, social, and psychosocial domains, as well as overall quality of life, according to self-reporting by the children. There were no changes in these variables in the control group.
Health-related domains of quality of life of the PedsQL before and after the intervention in the case and control groups - Florianópolis, Santa Catarina, Brazil, 2010.
| Domains | Case group | p | Control group | p | ||
|---|---|---|---|---|---|---|
| Before (n = 16) | After (n=16) | Before (n = 16) | After (n = 16) | |||
| Median [IQI] | Median [IQI] | Median [IQI] | Median [IQI] | |||
| Physical | 71.9 [60.1-78.1] | 92.2 [82.8-96.9] | 0.001a | 64.0 [56.2-75.0] | 73.4 [66.4-80.5] | 0.292 |
| Emotional | 57.5 [50.0-70.0] | 75.0 [51.2-88.7] | 0.014a | 50.0 [40.0-63.7] | 52.5 [36.2-77.5] | 0.636 |
| Social | 82.5 [80.0-90.0] | 92.5 [86.2-100.0] | 0.004a | 80.0 [62.5-90.0] | 77.5 [60.0-90.0] | 0.572 |
| School | 80.0 [62.5-80.0] | 80.0 [75.0-95.0] | 0.070 | 80.0 [66.2-90.0] | 80.0 [62.5-83.7] | 0.623 |
| Psychosocial | 72.5 [65.4-77.9] | 83.3 [74.1-89.6] | 0.002a | 70.8 [60.8-77.5] | 68.3 [60.4-75.8] | 0.550 |
| General QL | 71.0 [68.0-76.4] | 84.2 [76.5-90.4] | 0.001a | 67.6 [59.9-76.0] | 71.6 [63.0-75.0] | 0.836 |
General QL, general quality of life; IQI, interquartile intervals; PedsQL, Pediatric Quality of Life Inventory.
The present study demonstrates the importance of a multidisciplinary intervention on the health-related quality of life of obese children, showing effects in the reduction of BMI and improvement in quality of life, especially in the physical, emotional, social, and psychosocial domains, as well as in overall quality of life.
One of the strengths of this study was that the sample was gender- and age-matched, minimizing the possible influence of these variables on the investigated parameters.3
The suggested exercises were playful and recreational, showing that this type of activity, when accompanied by nutritional counseling, also has positive effects on obese children. Despite different methodologies, studies have demonstrated the positive effects of intervention programs on the quality of life of obese children, which is in agreement with the results of this study.3,10,14,15
The present findings are clinically important due to the negative impact of obesity on quality of life, which can be similar to that of children with cancer undergoing chemotherapy,26 when evaluated using the same methodology. This suggests that advances in certain areas may represent a significant improvement on the daily routine of obese children, especially regarding their self-esteem, social relationships, and daily activities.
The improvement in the emotional aspect is clinically important, as a previous study found a higher rate of depressive symptoms in obese children undergoing outpatient treatment, when compared to the non-obese,27 and these symptoms may be present in approximately 11% of obese children.28 These symptoms have been identified as variables that significantly influence the quality of life and are associated with lower adherence to intervention programs for weight control, creating a vicious cycle.29 Thus, the importance of a multidisciplinary team in the treatment of this complex disease is well-established.10,14
The quality of life improvement in the physical domain can be associated to the benefits of physical activity in maintaining health, reflecting the child's ability to perform everyday activities. The PedsQL questions related to this domain are associated to difficulties in walking, running, playing sports, or feeling low on energy, with difficulties being frequently reported by obese children.6 However, after participating in the intervention program, these difficulties were reported less frequently, which may indicate that a healthy occupation during leisure time constitutes an effective means to contribute to a satisfactory quality of life.
No effects were observed in the school domain of quality of life after the intervention; however, studies suggest that this domain is not as affected in obese children as the other aspects.6,30
The results of the present study demonstrate that a program for the treatment of obesity is associated with improvement in health-related quality of life. However, one study limitation was that other health problems that could interfere with quality of life were not diagnosed, and cultural and social factors that could also affect quality of life were not completely controlled in this study. In an attempt to achieve sample homogenization, groups were selected from a single treatment center.
Nevertheless, the initial data showed a similarity between the groups in all investigated parameters. The questionnaire was self-reported and the responses given by the children may not match the reality; in addition, children may have different interpretations of the intervals determined in PedsQL. The duration of the program effect on HRQoL(Health-Related Quality of Life) and on maintenance of a healthier lifestyle is also unknown. Long-term data related to quality of life have not been well described to confirm this conclusion, and should be interpreted with caution. The results of Duncan et al.15 demonstrated that, despite the health-related quality of life improvement after physical training, the scores were not sustained six weeks after the intervention, which may suggest the need for an ongoing program of intervention for this particular group.
The sample loss (27.28%) during the intervention was not expected, and was higher than those of other studies in obese children.9,13 Some factors may have contributed to the sample loss, such as transportation difficulties, as many children depended on public transportation and the program lacked financial resources, and the difficulty to ensure the presence of a parent/tutor. However, the power of the sample was greater than 95%, considering each group of 16 subjects, a difference in the overall quality of life score of 13 points, and standard deviation of 8.5 in the case group and 9.7 in the control group.
Another relevant aspect is that even though it was a physical exercise program with recreational activities, children remained within the target zone during the sessions for approximately 40minutes, according to data from the HR monitor, with individual variations; circuit and trampoline activities maintained the greatest time within the recommended target zone, which may indicate that in many sessions, moderate to vigorous intensity activities predominated.
The multidisciplinary intervention program was effective in reducing BMI and improving the quality of life in the physical, emotional, social, and psychosocial domains, as well as overall quality of life. The results point to the multiple benefits of an intervention program with exercise and nutritional counseling, in addition to conventional treatment for obese children. The quality of life assessment should be taken into account when planning for obesity control, and it may serve as an additional criterion in the evaluation of treatment effects, and may have a valuable role in maintaining healthy habits. This approach can help in treatment adherence, obesity control, and relapse prevention in the medium and long term.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the medical staff at Hospital Infantil de Florianópolis (physicians and nurses), the students of Nutrition and Physical Education at Universidade Federal de Santa Catarina who collaborated with this study, and the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior for the PhD scholarship.
Please cite this article as: Poeta LS, Duarte MF, Giuliano IC, Mota J. Interdisciplinary intervention in obese children and impact on health and quality of life. J Pediatr (Rio J). 2013;89:499–504.