To review the clinical characteristics, comorbidities, and management of insomnia in childhood and adolescence.
SourcesThis was a non-systematic literature review carried out in the PubMed database, from where articles published in the last five years were selected, using the key word “insomnia” and the pediatric age group filter. Additionally, the study also included articles and classic textbooks of the literature on the subject.
Data synthesisDuring childhood, there is a predominance of behavioral insomnia as a form of sleep-onset association disorder (SOAD) and/or limit-setting sleep disorder. Adolescent insomnia is more associated with sleep hygiene problems and delayed sleep phase. Psychiatric (anxiety, depression) or neurodevelopmental disorders (attention deficit disorder, autism, epilepsy) frequently occur in association with or as a comorbidity of insomnia.
ConclusionsInsomnia complaints in children and adolescents should be taken into account and appropriately investigated by the pediatrician, considering the association with several comorbidities, which must also be diagnosed. The main causes of insomnia and triggering factors vary according to age and development level. The therapeutic approach must include sleep hygiene and behavioral techniques and, in individual cases, pharmacological treatment.
Revisar as características clinicas, as comorbidades e o manejo da insônia na infância e adolescência.
Fonte dos dadosRevisão não sistemática da literatura realizada na base dados PubMed,onde foram selecionados artigos publicados nos últimos 5 anos, selecionados com o uso da palavra chave insônia e o filtro faixa etária pediátrica. Adicionalmente foram também incluídos artigos e livros texto clássicos da literatura sobre o tema.
Síntese dos dadosNa infância existe predomínio da insônia comportamental na forma de distúrbio de início do sono por associações inadequadas e/ou distúrbio pela falta de estabelecimento de limites. Na adolescência a insônia está mais associada a problemas de higiene do sono e atraso de fase. Transtornos psiquiátricos (ansiedade, depressão) ou do neurodesenvolvimento (Transtorno do déficit de atenção, autismo, epilepsias) ocorrem com frequência em associação ou como comorbidade do quadro de insônia.
ConclusõesA queixa de insônia nas crianças e adolescentes deve ser valorizada e adequadamente investigada pelo Pediatra, levando em consideração a associação com diversas comorbidades, que também devem ser diagnosticas. As causas principais de insônia e fatores desencadeantes variam de acordo com a idade e nível de desenvolvimento. A abordagem terapêutica deve incluir medidas de higiene do sono e técnicas comportamentais, e em casos individualizados tratamento farmacológico.
Sleep disorders (SD) are a frequent complaint in routine medical appointments and increasingly, the pediatrician must be able to adequately establish their diagnosis and management, thus avoiding referral to specialist consultations, as well as unnecessary and excessive examinations/interventions.
SD mostly present as the primary entity, but may also be associated with several organic diseases (e.g., asthma, obesity, neuromuscular diseases, gastroesophageal reflux disease, epilepsy, attention disorder, autism spectrum disorder) or psychiatric comorbidities (anxiety, depression, bullying).
Clinical presentation is variable and multiple. During the first years of life, the most frequent complaints are difficulty falling asleep and/or frequent nocturnal awakenings, followed by parasomnias (confusional arousals) and sleep-disordered breathing (obstructive apnea-hypopnea syndrome). From preschool age onwards, disorders related to inadequate sleep hygiene occur and, in adolescence, the disorders are related to circadian issues (delayed sleep phase) or excessive movement during sleep (restless leg syndrome [RLS]).
This review will assess a frequent SD, i.e., insomnia, which may present in different clinical forms during childhood, with varied management. The clinical features, diagnosis, comorbidities, and treatments will be assessed, aiming to give the pediatrician an overview of the problem and to provide tools for its diagnosis and management.
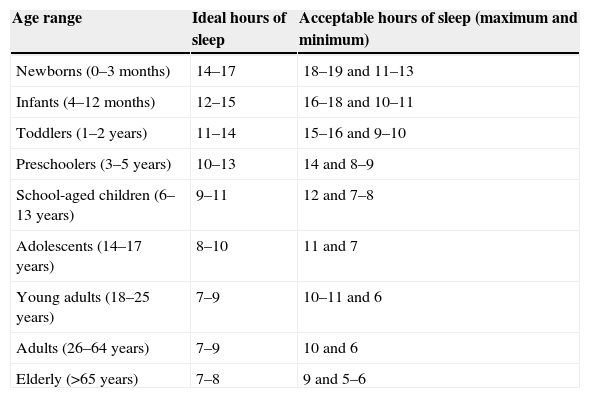
Sleep characteristics and classification of SDRecommendations about sleep duration in children and adolescents vary according to the source used. Recently, the National Sleep Foundation published a consensus based on an expert panel, stating the ideal number of sleeping hours for every age group and a variability range that contains the acceptable number of sleeping hours (Table 1).1
Sleep duration.a
| Age range | Ideal hours of sleep | Acceptable hours of sleep (maximum and minimum) |
|---|---|---|
| Newborns (0–3 months) | 14–17 | 18–19 and 11–13 |
| Infants (4–12 months) | 12–15 | 16–18 and 10–11 |
| Toddlers (1–2 years) | 11–14 | 15–16 and 9–10 |
| Preschoolers (3–5 years) | 10–13 | 14 and 8–9 |
| School-aged children (6–13 years) | 9–11 | 12 and 7–8 |
| Adolescents (14–17 years) | 8–10 | 11 and 7 |
| Young adults (18–25 years) | 7–9 | 10–11 and 6 |
| Adults (26–64 years) | 7–9 | 10 and 6 |
| Elderly (>65 years) | 7–8 | 9 and 5–6 |
Nocturnal awakenings occur frequently in childhood and its distribution varies with age. In the first six months of life, they are concentrated in one to two evening peaks; after the sixth month, they follow a distribution that accompanies the sleep cycle (which lasts 90–120min) and occur more commonly in the REM stage. In these cases, it is common that the child goes back to sleep spontaneously.2
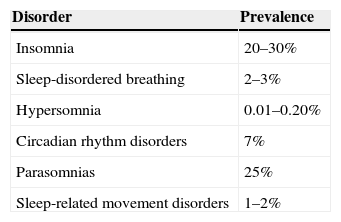
The classification of SD is proposed by the American Academy of Sleep Medicine and the Chronic Insomnia Definition-ICSD-3, which is the updated version of ICSD-2, was published in 2005. This classification review maintained the basic principles of the previous one, identifying seven major SD categories: insomnia, sleep-disordered breathing, central hypersomnia, circadian rhythm disorders, movement disorders during sleep, parasomnias, and others.2 There was a standardization of diagnostic criteria for adults and children, maintaining the recognition of specific age-dependent situations. Table 2 shows the prevalence of different SD in childhood, according to the American Academy of Sleep Medicine.3
Insomnia definitionInsomnia can be defined as difficulty initiating sleep (considered in children as the difficulty to fall asleep without a caregiver's intervention); maintaining sleep (frequent awakenings during the night and difficulty returning to sleep without a caregiver's intervention); or waking up earlier than the usual schedule with inability to return to sleep. Insomnia can cause distress and social, professional, educational-academic, or behavioral impairment.2
Insomnia prevalenceSD that manifest with difficulty falling asleep and/or difficulty maintaining sleep (due to nocturnal awakenings) affect approximately 30% of children. The increase in prevalence, which has been observed in recent years, is closely related to social habits in the family, as there is often a difference between the child's natural sleep-alertness rhythm and social requirements. This disorder, when chronic, can result in deleterious effects on cognitive development, mood regulation, attention, behavior and quality of life, not only of the child but the entire family, resulting in parents’ sleep deprivation, with consequences for their work activities.4,5
Data on the prevalence of insomnia vary with age. In the first two years, the rates are high, around 30%, and after the third year of life the prevalence remains stable at around 15%. It is worth mentioning that, as insomnia definition and diagnosis vary widely among the available studies, this fact directly influences the data on prevalence.4,5
In a population-based study conducted in Pennsylvania, it was demonstrated that one out of five children or pre-adolescents have insomnia symptoms; the highest prevalence (approximately 30%) is observed in girls aged 11–12 years, which appears to be more related to hormonal changes than to anxiety/depression.6
Another large population-based study was carried out in China, using two data collection stages, with a five-year interval between them. An increase in insomnia prevalence from 4.2% to 6.6% and incidence from 6.2% to 14.9% was demonstrated. The initial cases were associated with health issues (laryngopharyngitis) and lifestyle (caffeine intake, smoking), whereas the new cases were associated with parents’ low educational level, alcohol intake, and mental illness.7
A population-based study conducted in Norway with adolescents showed that, on weekdays, the average number of sleep hours was 6h 25m, leading to a deficit of approximately 2h; most subjects (65%) showed long latency to sleep onset (>30min). The prevalence of insomnia in this population was 23.8% according to the DSM-IV criteria, 18.5% using the DSM-V, and 13.6% when quantitative criteria were used.8
Types of insomnia according to age rangeIn children, insomnia has clearly defined behavioral characteristics and can be defined as two main types, sleep-onset association disorder (SOAD) and limit-setting SD.9
- 1)
SOAD
In this condition, the infant learns to sleep under a specific condition (object, circumstance), which usually requires intervention/presence of parents. After a nocturnal physiological awakening, he/she needs the same intervention to resume sleeping. Although the number of awakenings is normal for their age group, the problem occurs due to the inability to return to sleep alone, which prolongs the alertness period. Diagnosis is based on the history of long latency to sleep onset, requiring specific and pre-determined conditions, as well as the need for caregiver intervention during the nocturnal awakenings. By definition, two or three awakenings/night, lasting between 5 and 10min or longer, occur five times a week.
This type of insomnia tends to disappear at approximately 3–4 years of age. Polysomnography is normal if the associations are present to facilitate sleep onset. The differential diagnosis with other types of insomnia is made through the rapid sleep onset in the presence of the initial conditions. The therapeutic approach is through the gradual extinction of the association stimulus.2,5
- 2)
Limit-setting SD
It is typical in preschool and school-age children, characterized by the parents’ difficulty in setting limits and rules for bedtime or having them followed. As a result, the child refuses to sleep or stay asleep all night. Excuses for not going to sleep are a common occurrence (hunger, thirst, “one more story…”), with parents usually giving in. Total sleep time may be reduced by 1–2h, with approximately three to five awakenings that result in the child leaving the bed or calling the parents. Polysomnography is normal, as once the child sleeps, sleep architecture is adequate. For the differential diagnosis, it is important to analyze the parents’ relationship and attitude with the child.
Management essentially involves parents, who should establish the limits/rules and maintain them firmly, and utilize behavioral techniques. It is acceptable to use sleep-inducing antihistamines or benzodiazepines for a limited period of time, while behavioral techniques are consolidated.2,5
Some children may experience a combination of the two types of behavioral insomnia.5
Studies have shown that sleep plays a crucial role in the healthy development of adolescents. However, changes in sleep patterns are very common in adolescence, due to biological and environmental factors such as late bedtime, inadequate sleep hygiene, and sleep restriction and fragmentation. Insomnia in this age group is associated with a poor prognosis in terms of mental health, school performance, and risk behavior.2
In adolescence, insomnia may be related to inadequate sleep hygiene and delayed sleep phase, or it can have a psychophysiological origin.
- 1)
Insomnia due to inadequate sleep hygiene:
During adolescence, insomnia has characteristics related to changes in social habits (tendency to sleep later) and sleep hygiene problems. The following habits are considered to be inadequate sleep hygiene: sleeping after 11pm and waking up after 8am; irregular sleep schedule between weekdays and the weekend; use of stimulating substances or drugs (licit and illicit); excess caffeine in the late afternoon or at night; and/or use of electronic devices in the bedroom before going to bed (TV, computer, mobile). Social and family pressures, hormonal changes, and the need for belonging to a group also influence sleep quality.10
Insomnia due to poor sleep hygiene leads to an increase in sleep latency and reduction in total sleep time. As a consequence, it results in excessive daytime sleepiness and/or hyperactivity, academic and relationship problems, and sleep-wake cycle inversion.11,12 It is important to make the differential diagnosis with psychiatric disorders such as depression and schizophrenia, noting that insomnia may be the initial symptom of these morbidities. Therapeutic management consists in following an adequate sleep hygiene routine, behavioral therapy and, in selected cases, the use of melatonin.5
- 2)
Delayed sleep phase insomnia:
It is defined as the delay in the sleep schedule that leads to a late awakening. This is a circadian rhythm disorder that occurs in adolescents due to hormonal changes, with a shift in the nocturnal sleep time as a function of the endogenous pacemaker. It is a common cause of insomnia and can occur at other ages, in addition to adolescence.
Conflicts occur because the bedtime does not match the sleep schedule; the adolescent refuses to go to sleep and has trouble waking up in the following morning. It results in symptoms of sleep deprivation, hyperactivity, aggression, and even learning disabilities, due to excessive daytime sleepiness. After they manage to fall sleep, sleep is tranquil, with adequate structure and duration (if they do not have to be awakened in the morning). The attempt to compensate for sleepiness with naps during the day or unlimited sleep time on weekends leads to more nocturnal delayed sleep phase.
Optimal management consists in readjusting sleep onset time. The use of low-dose melatonin (1mg) in the late afternoon was shown to be effective in correcting delayed sleep phase in a double-blinded study conducted with an adolescent population.13 The association between delayed sleep phase as a cause of insomnia in adolescents has been extensively assessed in the literature. In population-based study, carried out in Norway, including 10,220 adolescents aged 16–18 years, delayed sleep phase was observed in 3.3% of the population; over half of these adolescents (54% girls and 57% boys) also met the criteria for insomnia. Additionally, the delayed sleep phase diagnosis resulted in a three-fold increased risk for school absenteeism in males and 1.8-fold in females.14
- 3)
Psychophysiological insomnia:
Characterized by a combination of previously experienced associations and hypervigilance. The complaint consists of an exaggerated preoccupation with sleep, getting to sleep, and the adverse effects of “not sleeping” on the following day. This type of situation occurs through a combination of risk factors (genetic vulnerability, psychiatric comorbidities), triggering factors (stress), and other factors (poor sleep hygiene, caffeine intake, etc.).5
Among the factors that predispose to insomnia are: birth order (more prevalent in the first-born and/or only child), genetic factors (positive family history); temperament (mood variability); presence of maternal psychopathology or depression; caregivers’ behavior during the nocturnal awakenings (the tendency to make the child fall asleep while holding him/her on one's lap or pick up the infant in one's arms immediately after the nocturnal awakening tends to make insomnia a chronic condition); night feeding (nocturnal awakenings are more common in infants who are breastfed between 6 and 12 months and persist longer in children who continue to be breastfed after 12 months); and co-sleeping (frequently associated with insomnia).2
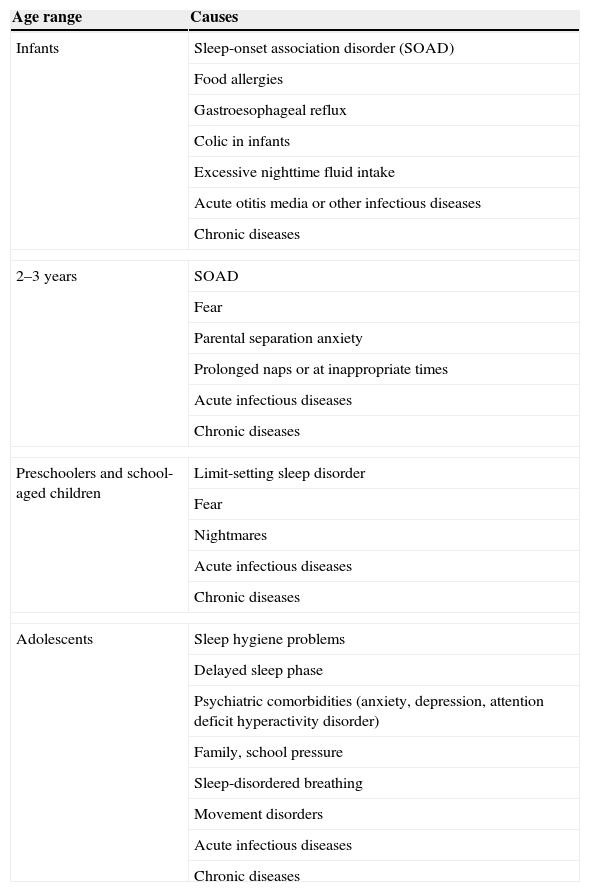
Different causes of insomnia or its precipitating factors are directly related to the child's neuropsychological development stage and/or typical characteristics of adolescence, as detailed in Table 3. The division by age group is an instructive presentation; however, overlaps between different age groups can occur. It should be noted that an irregular and erratic sleep routine can also lead to insomnia at all ages, as well as acute and/or chronic systemic diseases. Although scarcely discussed in childhood, the genetically determined characteristic of short sleep duration (an individual who sleeps well, but has a total duration of sleep below the average expected for age and level of development) can occur, and these cases have normal sleep quality (organization).15
Causes and/or triggering factors of insomnia according to the age group.
| Age range | Causes |
|---|---|
| Infants | Sleep-onset association disorder (SOAD) |
| Food allergies | |
| Gastroesophageal reflux | |
| Colic in infants | |
| Excessive nighttime fluid intake | |
| Acute otitis media or other infectious diseases | |
| Chronic diseases | |
| 2–3 years | SOAD |
| Fear | |
| Parental separation anxiety | |
| Prolonged naps or at inappropriate times | |
| Acute infectious diseases | |
| Chronic diseases | |
| Preschoolers and school-aged children | Limit-setting sleep disorder |
| Fear | |
| Nightmares | |
| Acute infectious diseases | |
| Chronic diseases | |
| Adolescents | Sleep hygiene problems |
| Delayed sleep phase | |
| Psychiatric comorbidities (anxiety, depression, attention deficit hyperactivity disorder) | |
| Family, school pressure | |
| Sleep-disordered breathing | |
| Movement disorders | |
| Acute infectious diseases | |
| Chronic diseases | |
Clinical history is extremely important for the diagnosis of insomnia, in which the falling asleep routine, as well as sleep and wake characteristics should be investigated. The impact of sleep disturbance on the child's life and family structure should be evaluated. The physical examination also helps to exclude possible causes of secondary insomnia.2,5,16
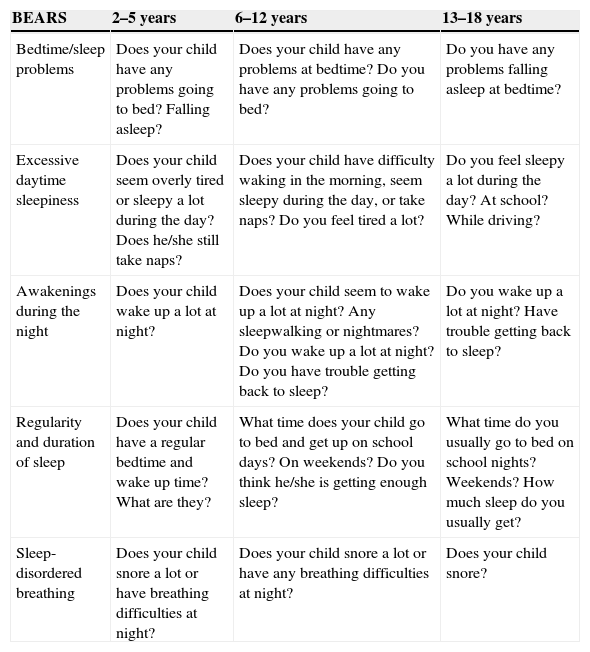
Early detection of SD is essential for the proper management to be established and for prognosis to be favorable. During the routine pediatric consultation, a tool that can assist in the screening is the Bedtime routines, Excessive daytime sleepiness, Awakenings during night, Regularity and duration of sleep, Sleep-disordered breathing; (BEARS) algorithm, consisting of five easy-to-apply questions that have good power to detect sleep alterations.17Table 4 shows the trigger questions for adequate sleep assessment.
BEARS algorithm.a
| BEARS | 2–5 years | 6–12 years | 13–18 years |
|---|---|---|---|
| Bedtime/sleep problems | Does your child have any problems going to bed? Falling asleep? | Does your child have any problems at bedtime? Do you have any problems going to bed? | Do you have any problems falling asleep at bedtime? |
| Excessive daytime sleepiness | Does your child seem overly tired or sleepy a lot during the day?Does he/she still take naps? | Does your child have difficulty waking in the morning, seem sleepy during the day, or take naps? Do you feel tired a lot? | Do you feel sleepy a lot during the day? At school? While driving? |
| Awakenings during the night | Does your child wake up a lot at night? | Does your child seem to wake up a lot at night? Any sleepwalking or nightmares? Do you wake up a lot at night? Do you have trouble getting back to sleep? | Do you wake up a lot at night? Have trouble getting back to sleep? |
| Regularity and duration of sleep | Does your child have a regular bedtime and wake up time? What are they? | What time does your child go to bed and get up on school days? On weekends? Do you think he/she is getting enough sleep? | What time do you usually go to bed on school nights? Weekends? How much sleep do you usually get? |
| Sleep-disordered breathing | Does your child snore a lot or have breathing difficulties at night? | Does your child snore a lot or have any breathing difficulties at night? | Does your child snore? |
Source: Modified from Mindell & Owens.17
BEARS, Bedtime routines, Excessive daytime sleepiness, Awakenings during night, Regularity and duration of sleep, Sleep-disordered breathing.
Another option that can help assess the dimension of insomnia is the use of sleep journals. These allow for the assessment of the circadian rhythm and time (amount of sleep). Some questions may be directed to assess sleep habits and routine. The journal should cover the 24-h period, and contain information related to a mean period of two weeks.
Additionally, validated questionnaires that assess sleep quality are also quite useful and should be used in association with interviews and the sleep journal.
For children aged between 0 and 3 years, the Brief Infant Sleep Questionnaire, created by Sadeh et al. and validated in Brazilian Portuguese should be used.18,19 For children older than 3 years, the Sleep Disturbance Scale for Children, proposed by Bruni et al. and also validated in Brazilian Portuguese, should be used.20,21 The Brazilian Portuguese version of this scale is available in the digital version of this article (Appendix 1).
Actigraphy is also a simple way to evaluate the sleep-wake rhythm. This device is shaped like a wristwatch and monitors body movements. The obtained signals can be analyzed through software and correlated with the child's condition, and can be used at any age.22
Polysomnography (PSG) is the gold standard exam for sleep evaluation. It consists in recording the electroencephalogram (EEG) with other physiological variables (eye movements, submental electromyogram, respiratory channels, ECG, oxygen saturation, leg movements, position sensor, snore sensor). It allows for a complete analysis of sleep architecture, respiratory events, and body movements. It assists in the assessment of sleep organization, time asleep, sleep latency, and in the differential diagnosis between epileptic and non-epileptic motor events.23
Comorbidities- 1)
Depression
Psychiatric disorders are usually associated with sleep problems such as hypersomnia, fatigue, irregular sleep-wake pattern, and nightmares, among others. Children with major depression have a high prevalence of insomnia (around 75%), and 30% have severe insomnia. The use of psychotropic medications can also negatively affect sleep. Conversely, there is new evidence suggesting that childhood insomnia itself is a risk factor for the development of psychiatric disorders in adolescence and adulthood.5
A population-based study conducted with Norwegian adolescents showed that depression leads to significant sleep time reduction, as well as longer latency to sleep onset and more episodes of nocturnal awakenings in both genders. Adolescents with insomnia had a four to five times higher risk of depression than those who sleep well. Sleep deprivation (sleeping fewer than 6h/night) results in an eight-fold higher risk of depression.24
- 2)
Attention-deficit disorder/hyperactivity disorder (ADHD)
It is estimated that around 25–50% of children with ADHD have sleep disorders. Miano et al. suggest different patterns, including hyperarousal, latency delay, association with respiratory disorders, RLS, and epilepsy.25 Children with the combined subtype of ADHD tend to have more sleep problems. Strategies related to better sleep hygiene and positive sleep routines are effective in these children. In selected cases, it may be necessary to use drugs to treat the insomnia, such as alpha agonists (clonidine), non-benzodiazepine sleep-inducers (zolpidem), or melatonin.26
- 3)
Autism spectrum disorder (ASD)
ASD consists of neurodevelopmental disturbances (pervasive diseases, Asperger's) characterized by significant social interaction and communication (language) impairment. SDs are common in this population and have severe effects on the affected child's and family's quality of life. Sleep restriction has been associated with increased frequency of stereotypies and worse severity scores. The complaint of insomnia characterized by long latency to sleep onset, resistance to sleep, reduced sleep efficiency, and nocturnal awakenings are of great concern to parents. In younger children, there is also increased prevalence of behavioral insomnia (SOAD and limit-setting SD).27
- 4)
Epilepsy
Patients with epilepsy have several changes in macro and micro sleep architecture, such as increased latency to sleep onset, reduced sleep efficiency, reduced REM sleep, and sleep fragmentation (especially those who have nocturnal seizures or refractory epilepsy). Complaints of excessive daytime sleepiness and poor sleep quality are also frequent.28–30
- 5)
Tourette syndrome
Patients with Tourette syndrome frequently have sleep and attention disorders. Insomnia is the most frequent SD and is usually associated with behavioral disorder during sleep.31
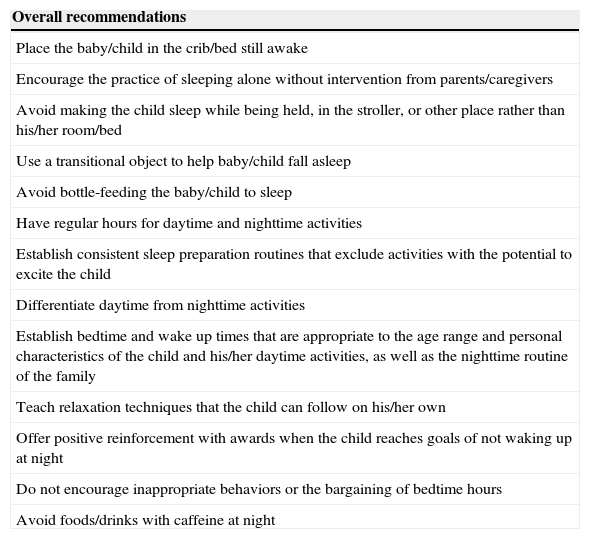
The treatment of insomnia starts with a detailed assessment of its causes and triggers. Parents should be educated about sleep hygiene and adequate sleep routines by the pediatrician during routine visits. Some of these recommendations are listed in Table 5.
Sleep routine recommendations.
| Overall recommendations |
|---|
| Place the baby/child in the crib/bed still awake |
| Encourage the practice of sleeping alone without intervention from parents/caregivers |
| Avoid making the child sleep while being held, in the stroller, or other place rather than his/her room/bed |
| Use a transitional object to help baby/child fall asleep |
| Avoid bottle-feeding the baby/child to sleep |
| Have regular hours for daytime and nighttime activities |
| Establish consistent sleep preparation routines that exclude activities with the potential to excite the child |
| Differentiate daytime from nighttime activities |
| Establish bedtime and wake up times that are appropriate to the age range and personal characteristics of the child and his/her daytime activities, as well as the nighttime routine of the family |
| Teach relaxation techniques that the child can follow on his/her own |
| Offer positive reinforcement with awards when the child reaches goals of not waking up at night |
| Do not encourage inappropriate behaviors or the bargaining of bedtime hours |
| Avoid foods/drinks with caffeine at night |
Strategies for the treatment of primary insomnia involve sleep hygiene routines, behavioral techniques, and/or pharmacological treatment.
- 1)
Sleep hygiene routines
Parents’ education regarding what is adequate sleep hygiene is the start of the treatment, noting that these procedures start during the day. Diet is an important factor, and high intake of caffeine (chocolate, teas, soft drinks) should be avoided during the day and especially at night. Another daytime aspect is physical activity, which, when moderate, has a beneficial effect on sleep. At least 3h before the child's established bedtime, he/she should be involved in relaxing activities; overstimulation should be avoided. Activities involving electronic media (TV, computer, tablet, and mobile phone) should also be restricted and avoided at least 1h before bedtime. The bedroom environment is also a sleep hygiene factor. It should be well ventilated, quiet and dark, at an adequate temperature, and have a comfortable bed. It is advisable not to use the bedroom for punishments (“time-outs”) applied during the day to prevent negative associations with the place of sleep.26
Positive routines can also help the child learn appropriate sleep behaviors and reduce stress. In addition to defining bedtime, consistent routines (activities that help prepare for sleep) should be established and repeated every night. As an example, let the child know that is almost time to go to bed, brush the teeth, perform other hygiene routines, put on pajamas, read a story or spend some time with the parents, turn off the lights. It is important to make sure that the time set for these routines is sufficient, so that they can be conducted calmly, without harming (reducing) total sleep time.26
In brief, adequate sleep hygiene consists of (1) regular/consistent bedtime that is appropriate for the age group; (2) avoiding high caffeine consumption; (3) welcoming nocturnal atmosphere; (4) bedtime routines; and 5) consistent and regular wake-up time, regardless of what occurred during the night (to maintain internal clock synchronization).17
- 2)
Behavioral therapy
The main objective of the behavioral approach is to eliminate the negative associations that lead to insomnia. It is possible to start this type of therapy after six months of life. Several studies have demonstrated the effectiveness of this approach in most cases, with clear benefits to the child's daytime routine, as well as to that of the family.32,33
There are several behavioral techniques that have been developed or adapted for the management of children with behavioral insomnia. These techniques have proven efficacy and safety and are widely used, especially in Anglo-Saxon countries. The technique should be decided by the pediatrician together with the parents, so that they can define the most appropriate one according to the child's age and the parents’ circumstances regarding treatment adherence.34
The following briefly describes the most often used techniques.2,16,17,34
Extinction: consists in putting the child to sleep safely and ignoring the nocturnal behavior (crying, tantrums, calling the parents) until the following morning. This procedure can also be performed with a parent in the bedroom, who will not interact until the predetermined time.
Gradual extinction: consists in putting the child to sleep safely and ignore the nocturnal behavior (crying, tantrums, calling the parents) for periods of time that increase during the night (starting with 5min and gradually increasing the waiting time by 5min each time). The purpose of this technique is to encourage the child to learn to self-comfort and return to sleep alone.
Positive routines: consists of developing a series of activities/calm routines that the child enjoys to prepare for bedtime, trying to disconnect the act of going to bed from a stressful routine. It is also possible to establish rewards to be given on the next day for those who manage to stay in bed until the next morning without going to the parents’ room or calling them.
Planned bedtime: consists of removing the child from bed if he/she cannot fall asleep within the pre-established time interval (15–30min) and letting him/her perform some calming activity to get sleepy; the parents should delay bedtime, so that the child goes to bed when feeling sleepy. After establishing the time when the child goes to sleep spontaneously, put the child to bed 15–30min earlier every day, until the appropriate time is achieved.
Programmed awakening: consists of waking up the child at night, between 15 and 30min before the usual time of spontaneous awakening, and after that, increasing the interval between episodes.
Cognitive restructuring: consists of using cognitive-behavioral techniques, in which the patient is taught to control his/her negative thoughts about sleep and bedtime. For instance, instead of thinking “I won’t sleep tonight”, the child should think “tonight I will relax and rest in my bed.”
Relaxation techniques: consists of meditation, muscle relaxation, taking deep breaths, visualizing positive images.
Sleep restriction: consists of restricting the time in bed, so that the child will only lie in bed when he/she is almost asleep; it helps to disconnect the idea of staying in bed without feeling sleepy and helps to consolidate the connection between bed and sleep.
Stimulus control: consists of avoiding performing activities that are not sleep-inducing when the child/adolescent is already in bed (TV, social media, worries, etc.).
Gradual extinction and extinction techniques, which have been used for several decades, still generate discussion and debate, and parents have difficulty adhering to them, especially in Latin culture countries. Controlled studies have shown that the use of behavioral interventions in children with insomnia not only improves their daily functions (sense of well-being and less crying), but also the mood, sleep, and parental marital satisfaction.34
More recent studies support and confirm these findings, demonstrating that, at school age, children with insomnia who received behavioral intervention had better performance at social skills when compared to children who did not receive it.35 Additionally, another study also reported improvements in maternal sleep and mood.36
During the literature review for the preparation of this article, the authors did not retrieve any studies that associated the use of behavioral interventions in children with insomnia to deleterious effects on mental health or on the emotional connection with parents. On the contrary, several studies that consistently demonstrated the benefits of this intervention were retrieved.37,38 It is also important to mention two studies in which children who received early behavioral interventions for insomnia were reassessed at the follow-up and the authors did not detect any changes in emotional function or internalizing and externalizing behaviors.37,39
- 3)
Pharmacological therapy
Pharmacological therapy indication in childhood insomnia should occur when the parents cannot adapt to behavioral therapies due to objective difficulties or when the therapy does not show adequate results. The indication must be made before the problem becomes chronic, and must be conducted in association with behavioral therapy and for a limited period of time. It is important to emphasize that there are no drugs for insomnia approved for use in children with such an indication, which already limits this strategy.2,17 Indications are empirical, based more on clinical experience than on evidence. In most children, sleep problems can be solved using a sleep hygiene approach and behavioral techniques; however, if there is drug indication, it is recommended to follow these guidelines when choosing it:
- a)
The medication should act on the target symptom (pain, anxiety);
- b)
Primary SDs (e.g., apnea, RLS) should be treated before insomnia medication is indicated;
- c)
The choice of medication must be appropriate for the age and neurodevelopmental level, always weighing the benefits against the side effects.
- a)
3.1) Antihistaminic agents:
They are the most frequently prescribed drugs for insomnia therapy at the level of primary care (e.g., hydroxyzine, diphenhydramine, promethazine). They assist in the acute phase, leading to a decrease in latency and awakenings, and must be used in combination with a behavioral intervention program. Daytime sedation, dizziness, or paradoxical hyperactivity can occur as side effects.40
3.2) Alpha-agonists (clonidine)
They are used for the treatment of insomnia in children due to their sedative effect. Their duration of action is 3–h and the half-life is 12–6h. They should be administered at bedtime, orally. Hypotension and weight loss have been described as side effects. Rapid withdrawal can lead to unwanted symptoms, such as shortness of breath, high blood pressure, and tachycardia.26
3.3) Melatonin
It is a hormone (N-acetyl-5-methoxytryptamine) synthesized by the pineal gland, whose secretion is controlled by the suprachiasmatic nucleus of the hypothalamus, with a peak between 2 and 4am. It reduces latency to sleep onset and number of awakenings, as well as improving mood and daytime behavior. Its efficacy in children with ADHD and ASD has been reported in several studies. The recommended dose is 0.5–3mg in children and 3–5mg in adolescents. At the usual doses, the side effects are irrelevant. The medication does not interfere with antiepileptic drug action, endogenous melatonin production, or pubertal development, and does not cause addiction.41
3.4) L5-hydroxytryptophan
It is a serotonin precursor. It has shown to be effective in episodes of certain types of parasomnia, such as night terrors, at a dose of 1–2mg/kg/day at bedtime. It appears to have a sleep stabilizing function, being effective in some patients. It can be used as an alternative treatment, as it has practically no side effects.40
3.5) Iron
The association between reduced iron levels and motor activity during sleep has been widely discussed in recent years. Iron deficiency in the substantia nigra can reduce dopaminergic function, as this element has a modulatory function. Iron-deficiency anemia may be associated with nocturnal motor hyperactivity, with reduced sleep time and increase in the number of awakenings. As this hyperactivity can be a precursor of RLS, oral iron replacement is indicated when ferritin levels are low.42
3.6) Benzodiazepines
These are the most often prescribed psychotropic drugs for children with neurological and/or psychiatric problems. They reduce the latency to sleep onset and improve sleep efficiency. Side effects may occur and vary from daytime sedation, changes in behavior, paradoxical hyperactivity, and memory deficits. They are contraindicated in suspected sleep-disordered breathing.41
3.7) Tricyclic antidepressants
Imipramine at a dose of 0.5mg/kg/day at bedtime appears to have some efficacy in insomnia; however, it is not widely used due to the risk of severe side effects.41
3.8) Non-benzodiazepine sleep inducers (imidazopyridine)
Their use in children younger than 12 years is contraindicated. Zolpidem and zaleplon are the most often used; as they have few side effects, they can be administered in children aged 12 years and older at a dose of 5–0mg at bedtime.41
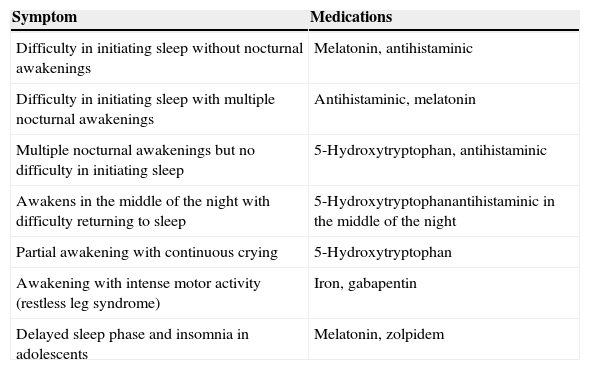
Table 6 summarizes drug indications for insomnia according to the nocturnal complaint.
Pharmacotherapy of insomnia according to the type of nocturnal symptoms.
| Symptom | Medications |
|---|---|
| Difficulty in initiating sleep without nocturnal awakenings | Melatonin, antihistaminic |
| Difficulty in initiating sleep with multiple nocturnal awakenings | Antihistaminic, melatonin |
| Multiple nocturnal awakenings but no difficulty in initiating sleep | 5-Hydroxytryptophan, antihistaminic |
| Awakens in the middle of the night with difficulty returning to sleep | 5-Hydroxytryptophanantihistaminic in the middle of the night |
| Partial awakening with continuous crying | 5-Hydroxytryptophan |
| Awakening with intense motor activity (restless leg syndrome) | Iron, gabapentin |
| Delayed sleep phase and insomnia in adolescents | Melatonin, zolpidem |
Source: Modified from Bruni & Angriman.2
In conclusion, insomnia complaints in children and adolescents should be taken into account and properly investigated by the pediatrician, considering its association with several comorbidities, which must also be diagnosed. The main causes of insomnia and its triggers vary according to the age and level of development. The therapeutic approach should include sleep hygiene measures, behavioral techniques, and, in individual cases, pharmacological treatment.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Nunes ML, Bruni O. Insomnia in childhood and adolescence: clinical aspects, diagnosis, and therapeutic approach. J Pediatr (Rio J). 2015;91:S26–35.