The purpose of this study was to analyze the factors that influence of the time between birth and the beginning of breastfeeding, especially at the moment of the rapid HIV test results at hospital admission for delivery.
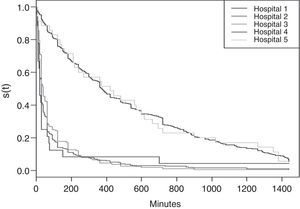
MethodsCohort study of 932 pregnant women who underwent rapid HIV test admitted in the hospital for delivery in Baby-Friendly Hospitals. The survival curves of time from birth to the first feeding were estimated by the Kaplan–Meier method and the joint effect of independent variables by the Cox model with a hierarchical analysis. As the survival curves were not homogeneous among the five hospitals, hindering the principle of proportionality of risks, the data were divided into two groups according to the median time of onset of breastfeeding at birth in women undergoing rapid HIV testing.
ResultsHospitals with median time to breastfeeding onset at birth of up to 60min were considered as early breastfeeding onset and those with higher medians were considered as late breastfeeding onset at birth. Risk factors common to hospitals considered to be with early and late breastfeeding onset at birth were: cesarean section (RR=1.75 [95% CI: 1.38–2.22]; RR=3.83 [95% CI: 3.03–4.85]) and rapid test result after birth (RR=1.45 [95% CI: 1.12–1.89]; RR=1.65 [95% CI: 1.35–2.02]), respectively; and hospitals with late onset: starting prenatal care in the third trimester (RR=1.86 [95% CI: 1.16–2.97]).
ConclusionsThe onset of breastfeeding is postponed, even in Baby-Friendly Hospitals, when the results of the rapid HIV test requested in the maternity are not available at the time of delivery.
Identificar os fatores associados ao tempo entre o nascimento e o início da amamentação em mães, especialmente o momento do resultado do teste rápido anti-HIV, na internação para o parto.
MetodologiaEstudo de coorte com 932 parturientes que realizaram teste rápido anti-HIV na internação para o parto em Hospitais Amigos da Criança. As curvas de sobrevida do tempo do nascimento até a 1ª mamada foram estimadas pelo método Kaplan–Meier, e o efeito conjunto das variáveis independentes pelo modelo de Cox, com análise hierarquizada. Como as curvas de sobrevida não foram homogêneas entre os 5 hospitais, ferindo o princípio de proporcionalidade de riscos, os dados foram desmembrados em dois grupos segundo o tempo mediano de início de aleitamento materno ao nascer em mulheres submetidas ao teste rápido anti-HIV.
ResultadosHospitais com tempo mediano de até 60 minutos foram considerados como hospitais de início precoce do aleitamento materno e hospitais com tempo mediano superior foram considerados como hospitais de início tardio do aleitamento materno ao nascer. Foram fatores de risco comuns aos hospitais com início precoce e tardio do aleitamento materno ao nascer: parto cesáreo [RR=1.75 (IC95%:1,38–2,22); RR=3,83 (IC95%:3,03–4,85)] e resultado do teste rápido após o parto [RR=1,45 (IC95%:1,12–1,89); RR=1,65 (IC95%:1,35–2,02)], respectivamente; e nos hospitais com início tardio de aleitamento materno ao nascer: iniciar o pré-natal no 3° trimestre [RR=1,86 (IC95%:1,16–2,97)].
ConclusõesO início do aleitamento materno vem sendo postergado, mesmo em Hospitais Amigos da Criança, quando os resultados do teste rápido anti-HIV solicitados na maternidade não estão disponíveis no momento do parto.
Breastfeeding at birth is essential to establish mother–baby bonding and contributes to the continuation of breastfeeding and the reduction of neonatal mortality.1,2 Newborns are more responsive to the mother's smell, touch, and warmth; when the skin-to-skin contact is initiated soon after birth, the newborn has the capacity to seek out the nipple–areola region and latch on during the first hour of life. Three to four hours after birth, newborns enter the sleep phase, which complicates the onset of breastfeeding.3
The Baby-Friendly Hospital Initiative (BFHI) recommends “putting babies in direct contact with the mother immediately after birth for at least an hour and encourage the mother to verify whether the baby is ready to be breastfed and offer help if necessary” as the Step 4 of the “Ten Steps to Successful Breastfeeding”.4
There are situations, however, when breastfeeding should not be practiced. In Brazil, breastfeeding by human immunodeficiency virus (HIV)-infected mothers is contraindicated due to the risk of vertical transmission through breast milk.5 However, the Ministry of Health (MOH) recommends that health professionals should not prohibit breastfeeding to mothers who, although submitted to the anti-HIV test, do not have the result available, as the contraindication should be based on an HIV-reagent test, stressing that it is the responsibility of the service to establish the logistics so that the result is available in a timely manner.6 With this purpose, the MOH has regularized rapid HIV tests in hospitals for pregnant women not tested for HIV during prenatal care, in time for establishing vertical transmission prophylactic measures.7
Additionally, since 2006 the MOH has recommended repeating anti-HIV serology, with the pregnant woman's consent, near the 38th week of pregnancy8 whenever possible. Thus, rapid HIV tests are currently often requested in maternity wards, but often without following any criteria or standards, even for women who already had a diagnosis at the last trimester of pregnancy. This increased demand for rapid tests and the professionals’ work overload has hindered how promptly results are obtained.9
Therefore, this study aimed to analyze the factors associated with the period between birth and the onset of breastfeeding in mothers submitted to rapid HIV test at hospital admission for delivery, especially at the moment of the rapid HIV test results.
MethodsThis was a cohort study, whose initial event was delivery and whose outcome was the onset of breastfeeding. The database from the research “Gender, Power and Citizenship: is the woman a subject in decision-making regarding breastfeeding at birth when HIV status is unknown to the service?”10 was used. The target population of the study was all women submitted to rapid HIV test at hospital admission for delivery in the five Baby-Friendly hospitals belonging to the High-Risk Pregnancy System in the city of Rio de Janeiro between September 11 and December 11, 2006.
The pilot study was performed in two hospitals of the High-Risk Pregnancy System in the same city, which had agreed to become Baby-Friendly hospitals. The study indicated a prevalence of non-breastfeeding at birth of 50% among seronegative women submitted to the rapid HIV test. Based on this parameter, a sample of 700 mothers was estimated, with a statistical power of 99% and 95% confidence level.
Women included in the study were those submitted to rapid HIV test at delivery, whose children were born alive and remained in rooming-in care. The women excluded from the study were those whose infants were born with 5-min Apgar value <7 (critically low state of vitality), who were referred to the intensive care unit (ICU; or neonatal ICU [NICU]) when the mother was referred to the ICU or showed HIV seropositivity.
The interviews were performed by nurses or nursing students trained and supervised weekly by a researcher, after the informed consent had been signed, which contained details of the research and ensured confidentiality of information. The project was approved by the Health Secretariat Ethics Committee of Rio de Janeiro (Statement 82A of 31/07/2006).
A daily survey was carried out in the laboratory of each hospital to identify the pregnant women submitted to rapid HIV test and the name of these women was transcribed to a data collection form. The form was compared daily with the list of rooming-in admissions, the chart was checked, delivery data were entered into a daily plan, and eligible mothers were interviewed. The interviews were performed using a structured questionnaire, administered at least 2h after the child's birth. If during the interview the newborn had not been breastfed yet, the interviewer returned to interview that mother again at the end of the day to collect data on the time between birth and the first feeding.
The study endpoint was obtained through the question “How long after birth was your baby breastfed for the first time?”, and in an attempt to improve the mother's answer accuracy, it was sought to make her recall the time of this event based on the schedule of hospital routines. The answer was given in hours and minutes, and the first breastfeeding was considered as the moment of contact between the baby's mouth and the mother's nipple–areola region, with either the occurrence of suction or licking.
The variables were organized in a hierarchical model, with socioeconomic and demographic (distal), reproductive and prenatal care (intermediate), and hospital characteristics (proximal). The distal variables were age, educational level, ethnicity, marital status, maternal employment, and income.
The intermediate variables were: parity; prenatal care; trimester when prenatal care started; number of prenatal visits; HIV test performed during prenatal care; trimester when the pregnant woman was tested; and results of HIV testing in prenatal care.
Finally, the proximal variables were: hospital; type of delivery; gender of the baby; mother wanted to breastfeed; professional heard what the mother had to say about her and the infant; mother knew about performing rapid HIV test at the hospital; mother received explanation about the test; mother received the test result; and moment when the mother knew the test result.
Survival analysis11 was used, in which time zero was birth and the first feeding was the final event. The analysis considered the mothers that started breastfeeding within the first 24h. Cases where the follow-up until the outcome was not possible and those in which the occurrence of start of breast-feeding time was more than 24h were omitted.
Survival curves, overall and by stratum, estimated by the nonparametric Kaplan–Meier method,12 were used as an exploratory tool in the univariate analysis.
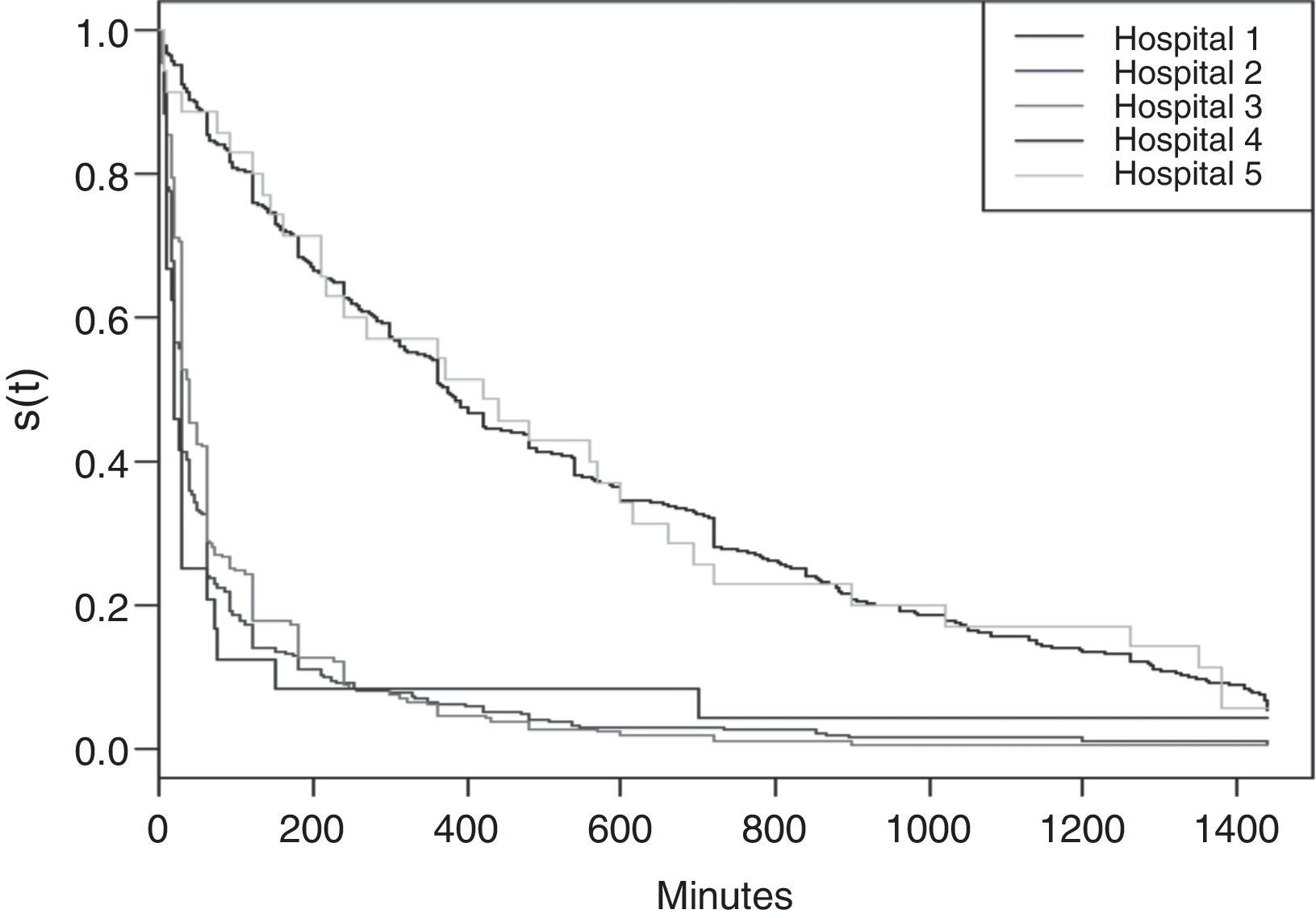
It was observed that survival curves were not homogenous in the five hospitals, affecting the principle of risk proportionality. Therefore, it was decided to divide the data into two groups, according to the median time to onset of breastfeeding at birth: hospitals with median time of up to 60min were considered as early onset of breastfeeding at birth and those with higher median time were considered as late onset of breastfeeding at birth.
After the initial analysis, the variables that showed statistical significance of 10% at the Peto test12 or epidemiological significance test were considered for construction of the hierarchical model. The Wald test was used to compare the different Cox regression models. The R2 of the saturated model was used to evaluate the quality of adjustment, based on the proportion of explained variance.
In the hierarchical modeling, the block of variables in the distal level was introduced. Variables with statistical significance at the 10% level were kept in the model and incorporated into the analysis of the intermediate block. The same procedure was repeated for the analysis of the proximal block variables, resulting in a final model with three levels.13,14
The Schoenfeld and Martingale tests12 were applied to the analysis of residues. The database was built using Epi Info (Epi Info™ Centers for Disease Control and Prevention, GA, USA) software and the statistical modeling, charts, and residue analysis were performed using the R statistical package15 (R Core Team (2012). R: a language and environment for statistical computing. Vienna, Austria).
ResultsDuring the study period there were 4895 births in selected hospitals and 1396 (28.5%) women underwent rapid HIV test. Of these, 322 women were excluded due to the presence of criteria that could impair or prevent breastfeeding at birth. Of the 1074 eligible women, 42 refused to participate (3.9%) and there was loss of 77 (7.2%) due to early discharge or other reasons. It was not possible to obtain the time until the first feeding in 23 mothers (2.1%), thus totaling 932 women for the analysis. Of these, 27 cases were omitted, who had time until onset of breastfeeding longer than 24h, and thus the number of events was restricted to 905.
The median time until the onset of breastfeeding was 90min (95% CI: 63–120), with a probability of 48% to breastfeed within the first hour after delivery.
The median time to the onset of breastfeeding for white mothers (60min; 95% CI: 40–65), with 1–4 years of schooling (60min; 95% CI: 36–120) and maternal income >1 minimum wage (60min; IC 95%: 40–110) was lower than their corresponding matches, with statistical significance in the Peto Test (p<0.001, p=0.046, p=0.089, respectively). Maternal age showed no statistical significance when analyzed by categories in the Kaplan–Meier test (p=0.313), but it did when analyzed continuously (p=0.049), and showed a linear association with time when a spline was performed, with a p-value of the linearity of p=0.051, vs. p=0.470 in the non-linear association.
The prenatal variables did not show survival curves with a statistically significant difference in the Peto test, but in relation to hospital variables, the following factors postponed the start of breastfeeding: hospital length of stay (p<0.001); mother knew about the performance of the rapid HIV test (120min; 95% CI: 90–135); mother received explanation about the test (120min; 95% CI: 105–180); mother knew the test result (180min; 95% CI: 120–210); mother knew the test result after delivery (240min; 95% CI: 180–348); mother was submitted to a cesarean section (110min; 95% CI: 120–360); mother did not want to put the baby at the breast at birth (120min; 95% CI: 95–174); and mother reported that the hospital staff had not listened to her (136min; 95% CI: 110–189).
In the survival curves stratified by hospital, as shown in Fig. 1, it is seen that the time until the first feeding showed distinct patterns. Hospitals 2, 3, and 4 had an early onset of breastfeeding at birth in the case of women submitted to the rapid HIV test, whereas hospitals 1 and 5 had a late onset of breastfeeding, leading to the division of the database according to the median time. The median time was analyzed for these two groups of hospitals (Table 1).
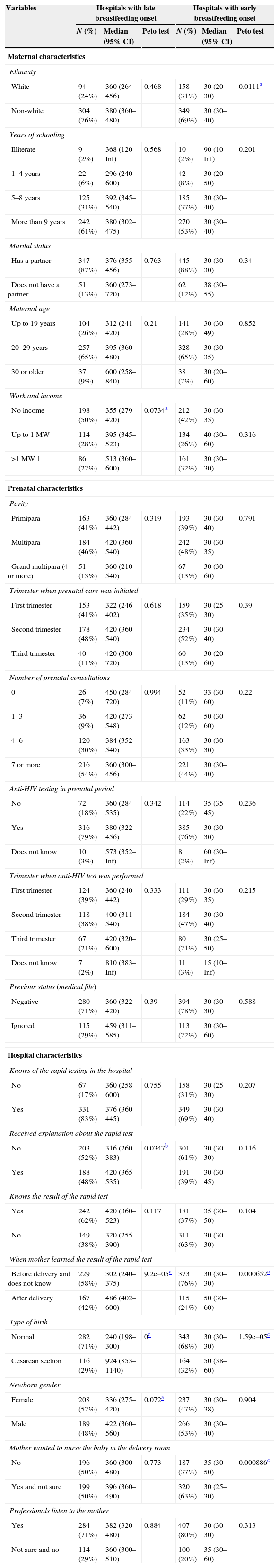
Median time from birth to breastfeeding onset, per type of hospital conduct. Rio de Janeiro, Brazil, 2006.
| Variables | Hospitals with late breastfeeding onset | Hospitals with early breastfeeding onset | ||||
|---|---|---|---|---|---|---|
| N (%) | Median (95% CI) | Peto test | N (%) | Median (95% CI) | Peto test | |
| Maternal characteristics | ||||||
| Ethnicity | ||||||
| White | 94 (24%) | 360 (264–456) | 0.468 | 158 (31%) | 30 (20–30) | 0.0111a |
| Non-white | 304 (76%) | 380 (360–480) | 349 (69%) | 30 (30–40) | ||
| Years of schooling | ||||||
| Illiterate | 9 (2%) | 368 (120–Inf) | 0.568 | 10 (2%) | 90 (10–Inf) | 0.201 |
| 1–4 years | 22 (6%) | 296 (240–600) | 42 (8%) | 30 (20–50) | ||
| 5–8 years | 125 (31%) | 392 (345–540) | 185 (37%) | 30 (30–40) | ||
| More than 9 years | 242 (61%) | 380 (302–475) | 270 (53%) | 30 (30–40) | ||
| Marital status | ||||||
| Has a partner | 347 (87%) | 376 (355–456) | 0.763 | 445 (88%) | 30 (30–30) | 0.34 |
| Does not have a partner | 51 (13%) | 360 (273–720) | 62 (12%) | 38 (30–55) | ||
| Maternal age | ||||||
| Up to 19 years | 104 (26%) | 312 (241–420) | 0.21 | 141 (28%) | 30 (30–49) | 0.852 |
| 20–29 years | 257 (65%) | 395 (360–480) | 328 (65%) | 30 (30–35) | ||
| 30 or older | 37 (9%) | 600 (258–840) | 38 (7%) | 30 (20–60) | ||
| Work and income | ||||||
| No income | 198 (50%) | 355 (279–420) | 0.0734a | 212 (42%) | 30 (30–35) | |
| Up to 1MW | 114 (28%) | 395 (345–523) | 134 (26%) | 40 (30–60) | 0.316 | |
| >1MW 1 | 86 (22%) | 513 (360–600) | 161 (32%) | 30 (30–30) | ||
| Prenatal characteristics | ||||||
| Parity | ||||||
| Primipara | 163 (41%) | 360 (284–442) | 0.319 | 193 (39%) | 30 (30–40) | 0.791 |
| Multipara | 184 (46%) | 420 (360–540) | 242 (48%) | 30 (30–35) | ||
| Grand multipara (4 or more) | 51 (13%) | 360 (210–540) | 67 (13%) | 30 (30–60) | ||
| Trimester when prenatal care was initiated | ||||||
| First trimester | 153 (41%) | 322 (246–402) | 0.618 | 159 (35%) | 30 (25–30) | 0.39 |
| Second trimester | 178 (48%) | 420 (360–540) | 234 (52%) | 30 (30–40) | ||
| Third trimester | 40 (11%) | 420 (300–720) | 60 (13%) | 30 (20–60) | ||
| Number of prenatal consultations | ||||||
| 0 | 26 (7%) | 450 (284–720) | 0.994 | 52 (11%) | 33 (30–60) | 0.22 |
| 1–3 | 36 (9%) | 420 (273–548) | 62 (12%) | 50 (30–60) | ||
| 4–6 | 120 (30%) | 384 (352–540) | 163 (33%) | 30 (30–30) | ||
| 7 or more | 216 (54%) | 360 (300–456) | 221 (44%) | 30 (30–40) | ||
| Anti-HIV testing in prenatal period | ||||||
| No | 72 (18%) | 360 (284–535) | 0.342 | 114 (22%) | 35 (35–45) | 0.236 |
| Yes | 316 (79%) | 380 (322–456) | 385 (76%) | 30 (30–30) | ||
| Does not know | 10 (3%) | 573 (352–Inf) | 8 (2%) | 60 (30–Inf) | ||
| Trimester when anti-HIV test was performed | ||||||
| First trimester | 124 (39%) | 360 (240–442) | 0.333 | 111 (29%) | 30 (30–35) | 0.215 |
| Second trimester | 118 (38%) | 400 (311–540) | 184 (47%) | 30 (30–40) | ||
| Third trimester | 67 (21%) | 420 (320–600) | 80 (21%) | 30 (25–50) | ||
| Does not know | 7 (2%) | 810 (383–Inf) | 11 (3%) | 15 (10–Inf) | ||
| Previous status (medical file) | ||||||
| Negative | 280 (71%) | 360 (322–420) | 0.39 | 394 (78%) | 30 (30–30) | 0.588 |
| Ignored | 115 (29%) | 459 (311–585) | 113 (22%) | 30 (30–60) | ||
| Hospital characteristics | ||||||
| Knows of the rapid testing in the hospital | ||||||
| No | 67 (17%) | 360 (258–600) | 0.755 | 158 (31%) | 30 (25–30) | 0.207 |
| Yes | 331 (83%) | 376 (360–445) | 349 (69%) | 30 (30–40) | ||
| Received explanation about the rapid test | ||||||
| No | 203 (52%) | 316 (260–383) | 0.0347b | 301 (61%) | 30 (30–30) | 0.116 |
| Yes | 188 (48%) | 420 (365–535) | 191 (39%) | 30 (30–45) | ||
| Knows the result of the rapid test | ||||||
| Yes | 242 (62%) | 420 (360–523) | 0.117 | 181 (37%) | 35 (30–50) | 0.104 |
| No | 149 (38%) | 320 (255–390) | 311 (63%) | 30 (30–30) | ||
| When mother learned the result of the rapid test | ||||||
| Before delivery and does not know | 229 (58%) | 302 (240–375) | 9.2e−05c | 373 (76%) | 30 (30–30) | 0.000652c |
| After delivery | 167 (42%) | 486 (402–600) | 115 (24%) | 50 (30–60) | ||
| Type of birth | ||||||
| Normal | 282 (71%) | 240 (198–300) | 0c | 343 (68%) | 30 (30–30) | 1.59e−05c |
| Cesarean section | 116 (29%) | 924 (853–1140) | 164 (32%) | 50 (38–60) | ||
| Newborn gender | ||||||
| Female | 208 (52%) | 336 (275–420) | 0.072a | 237 (47%) | 30 (30–38) | 0.904 |
| Male | 189 (48%) | 422 (360–560) | 266 (53%) | 30 (30–40) | ||
| Mother wanted to nurse the baby in the delivery room | ||||||
| No | 196 (50%) | 360 (300–480) | 0.773 | 187 (37%) | 35 (30–50) | 0.000886c |
| Yes and not sure | 199 (50%) | 396 (360–490) | 320 (63%) | 30 (25–30) | ||
| Professionals listen to the mother | ||||||
| Yes | 284 (71%) | 382 (320–480) | 0.884 | 407 (80%) | 30 (30–30) | 0.313 |
| Not sure and no | 114 (29%) | 360 (300–510) | 100 (20%) | 35 (30–60) | ||
CI: confidence interval.
For hospitals with late onset of breastfeeding at birth the median time was 375min. In hospitals with early onset of breastfeeding the median time was 30min, representing a period more than 10-fold shorter.
Based on the univariate analysis using the Kaplan–Meier method and epidemiological criteria, variables were analyzed using the proposed hierarchical model.
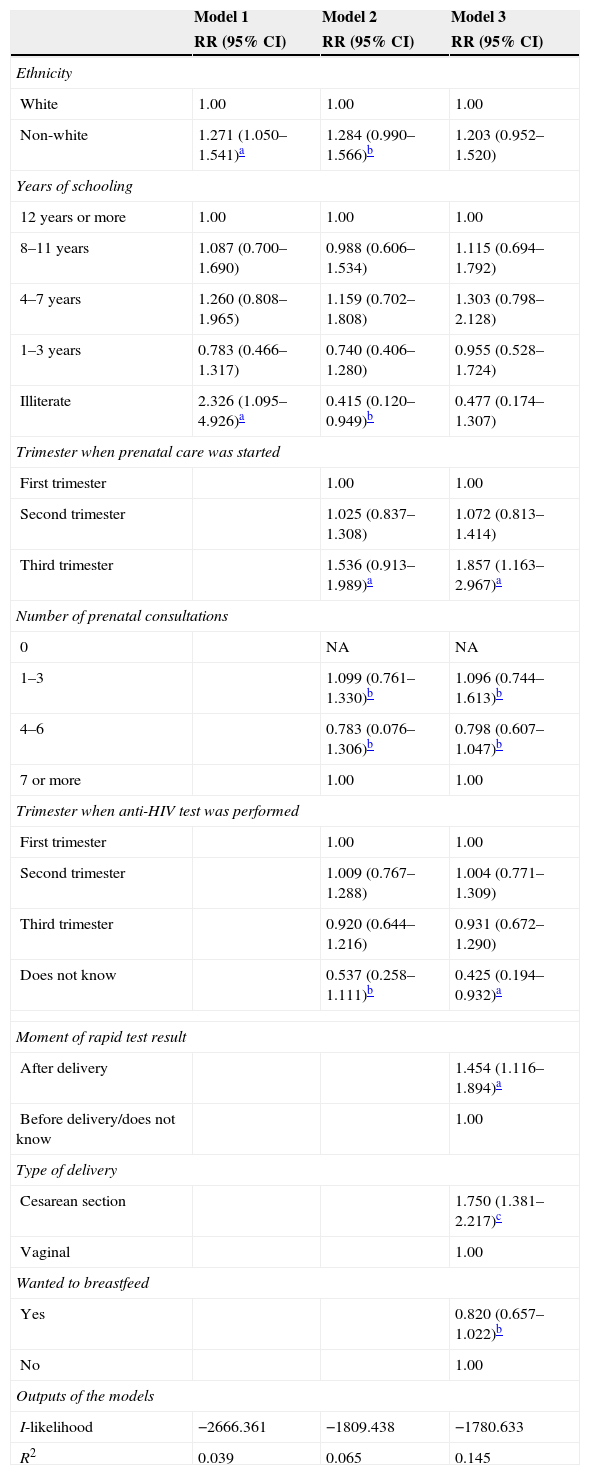
Model 3, after adjustment by the hierarchical model of factors related to the time of breastfeeding start in hospitals with early onset of breastfeeding, had a covariance explanation power of 14.5%.
In this sense, factors that postponed the start of breastfeeding were: starting prenatal care in the third quarter; knowledge after delivery of the result of the rapid HIV test in the hospital; and cesarean delivery.
In the hierarchical model for hospitals with late onset of breastfeeding, when the proximal level variables were introduced, the variables in the distal level lost statistical significance and, therefore, their effect appeared to be mediated by the variables in that level (Table 2).
Hierarchical model of factors associated with time to breastfeeding onset in hospitals with early-onset breastfeeding at birth. Rio de Janeiro, Brazil, 2006.
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Ethnicity | |||
| White | 1.00 | 1.00 | 1.00 |
| Non-white | 1.271 (1.050–1.541)a | 1.284 (0.990–1.566)b | 1.203 (0.952–1.520) |
| Years of schooling | |||
| 12 years or more | 1.00 | 1.00 | 1.00 |
| 8–11 years | 1.087 (0.700–1.690) | 0.988 (0.606–1.534) | 1.115 (0.694–1.792) |
| 4–7 years | 1.260 (0.808–1.965) | 1.159 (0.702–1.808) | 1.303 (0.798–2.128) |
| 1–3 years | 0.783 (0.466–1.317) | 0.740 (0.406–1.280) | 0.955 (0.528–1.724) |
| Illiterate | 2.326 (1.095–4.926)a | 0.415 (0.120–0.949)b | 0.477 (0.174–1.307) |
| Trimester when prenatal care was started | |||
| First trimester | 1.00 | 1.00 | |
| Second trimester | 1.025 (0.837–1.308) | 1.072 (0.813–1.414) | |
| Third trimester | 1.536 (0.913–1.989)a | 1.857 (1.163–2.967)a | |
| Number of prenatal consultations | |||
| 0 | NA | NA | |
| 1–3 | 1.099 (0.761–1.330)b | 1.096 (0.744–1.613)b | |
| 4–6 | 0.783 (0.076–1.306)b | 0.798 (0.607–1.047)b | |
| 7 or more | 1.00 | 1.00 | |
| Trimester when anti-HIV test was performed | |||
| First trimester | 1.00 | 1.00 | |
| Second trimester | 1.009 (0.767–1.288) | 1.004 (0.771–1.309) | |
| Third trimester | 0.920 (0.644–1.216) | 0.931 (0.672–1.290) | |
| Does not know | 0.537 (0.258–1.111)b | 0.425 (0.194–0.932)a | |
| Moment of rapid test result | |||
| After delivery | 1.454 (1.116–1.894)a | ||
| Before delivery/does not know | 1.00 | ||
| Type of delivery | |||
| Cesarean section | 1.750 (1.381–2.217)c | ||
| Vaginal | 1.00 | ||
| Wanted to breastfeed | |||
| Yes | 0.820 (0.657–1.022)b | ||
| No | 1.00 | ||
| Outputs of the models | |||
| I-likelihood | −2666.361 | −1809.438 | −1780.633 |
| R2 | 0.039 | 0.065 | 0.145 |
CI, confidence interval; RR, relative risk.
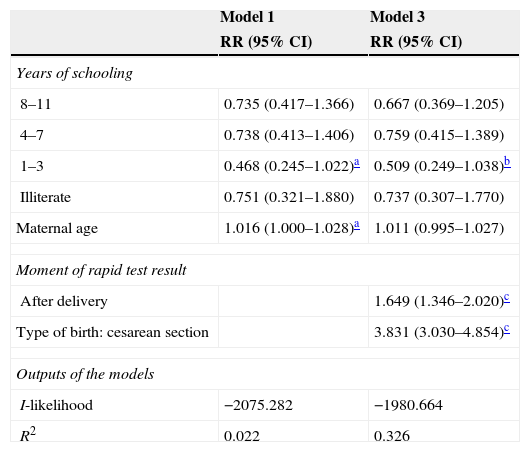
In the final model for hospitals with late onset of breastfeeding at birth, factors that negatively interfered with the outcome were: having received the result of the rapid test performed in the maternity after birth; and cesarean delivery. The inclusion of variables in the proximal level improved the model fit by 30% (Table 3).
Hierarchical model of factors associated with time to breastfeeding onset in hospitals with late-onset breastfeeding at birth. Rio de Janeiro, Brazil, 2006.
| Model 1 | Model 3 | |
|---|---|---|
| RR (95% CI) | RR (95% CI) | |
| Years of schooling | ||
| 8–11 | 0.735 (0.417–1.366) | 0.667 (0.369–1.205) |
| 4–7 | 0.738 (0.413–1.406) | 0.759 (0.415–1.389) |
| 1–3 | 0.468 (0.245–1.022)a | 0.509 (0.249–1.038)b |
| Illiterate | 0.751 (0.321–1.880) | 0.737 (0.307–1.770) |
| Maternal age | 1.016 (1.000–1.028)a | 1.011 (0.995–1.027) |
| Moment of rapid test result | ||
| After delivery | 1.649 (1.346–2.020)c | |
| Type of birth: cesarean section | 3.831 (3.030–4.854)c | |
| Outputs of the models | ||
| I-likelihood | −2075.282 | −1980.664 |
| R2 | 0.022 | 0.326 |
CI: confidence interval; RR: relative risk.
Risk factors for the outcome in hospitals with early onset of breastfeeding at birth were: starting prenatal care in the third trimester; moment of rapid test result after delivery; and cesarean delivery. For hospitals with late onset of breastfeeding the risk factors were: moment of rapid test result after delivery; and cesarean delivery.
DiscussionThe variable “moment of anti-HIV rapid test result after delivery” showed similar consistency and magnitude in both models, regardless of the hospital characteristic of early or late onset of breastfeeding at birth. This fact shows the delay in the test result has similar impact and same-intensity influence on breastfeeding postponement at birth.
In a study that dichotomized breastfeeding onset (first hour of life and after the first hour), not knowing whether the rapid HIV test was performed at the hospital and not knowing the results also showed to be factors that delayed breastfeeding at birth.9
In a recently published systematic review,15 it was observed that the only study that investigated the rapid HIV test in relation to breastfeeding is the result of the same database that gave origin to this article.
Cesarean delivery was negatively associated with the onset of breastfeeding and, thus, persisted as a barrier to breastfeeding at birth.16–18 Some authors consider cesarean section a risk factor for the continuation of breastfeeding at one and 3 months after birth.19
The median time to onset of breastfeeding in vaginal birth was 60min, and for cesarean section, the median time was 210min. According to hospital conduct, the median time to the onset of breastfeeding for a vaginal delivery in hospitals with early onset is 30min, whereas in hospitals with late onset of breastfeeding this time is 240min, an 8-fold longer period.
The median time to the first feeding for cesarean delivery also showed differences by hospital conduct. In hospitals with late onset, the median was 924min and in hospitals with early onset, the median was 50min, an almost 18-fold shorter period.
The variable “intention to breastfeed in the delivery room” was significantly associated with the outcome only in hospitals with early onset of breastfeeding at birth, suggesting that the mother's decision to breastfeed is weakened even in Baby-Friendly Hospitals, where the lack of staff awareness still persists in the autonomy of the woman regarding the hospital institution.
Based on the final models, it was verified that there are common factors, regardless of the pattern of median time until the onset of breastfeeding, such as the moment of the rapid test result and the type of delivery.
In hospitals with late onset of breastfeeding, the analyses suggest that almost 30% of the time variation is predictable by hospital variables. In hospitals with early onset of breastfeeding at birth, a small portion of data variability is explained by the model (R2=0.145), but the proximal variables still showed greater weight regarding the outcome. Residual analysis of the final models showed good fit of the models.
In hospitals with early onset of breastfeeding, 74% of women were able to start breastfeeding within the newborn's first hour of life, whereas in hospitals with late onset, only 15% started breastfeeding within 1h of birth. Therefore, the postponement of the onset of breastfeeding becomes evident as established practice, even in Baby-Friendly Hospitals, and hospital protocols are described in the literature as a barrier to the onset of breastfeeding.20
In spite of the characteristics of these hospitals, which in essence are breastfeeding supporters, the postponement of breastfeeding is supported by knowledge not reported in the literature. Thus, although they are Baby-Friendly Hospitals, they can be classified as having early- or late-onset of breastfeeding at birth.
The study has limitations, as it was not possible to analyze factors that, according to a systematic review on the theme,15 can influence the onset of breastfeeding, such as: area of residence, information on breastfeeding during prenatal care, home birth, and prematurity. Moreover, as all assessed mothers were submitted to the rapid test, it was not possible to investigate the influence of the test alone, which would add more information to the analysis.
Despite these limitations, this study is an important tool to improve vertical transmission prevention strategies and the Baby-Friendly Hospital Initiative, as well as humanization strategies in care and the establishment of these policies.
The only prenatal care variable associated with the time to onset of breastfeeding was the beginning of prenatal care in the third trimester, in hospitals with early onset of breastfeeding at birth. Women who started a late prenatal appear to constitute a risk clientele for the practice of breastfeeding, even in hospitals with practices that promote early onset of breastfeeding. Therefore, it can be observed that greater efforts are needed to carry out good-quality prenatal care, with early identification of pregnant women and a more thorough assessment for cesarean delivery.
It is crucial to define standards regarding the practice of breastfeeding for unknown HIV status, counseling practices and consent, and definition of responsibilities for providing results in a timely manner.
A more recent study conducted in 15 maternity hospitals in Rio de Janeiro in 2009 showed that the proportion of mothers submitted to the rapid test when admitted at the hospital for delivery was still high, and that not knowing the results of the HIV testing before delivery increased by more than 2-fold the chance of late onset of breastfeeding,21 showing that this scenario has not shown a positive evolution with time.
After the implementation of the Baby-Friendly Hospital Initiative, there were significant advances in breastfeeding practices. Thus, the proposed challenge is the establishment of guarantees to evaluate interventions that may be related to the postponement of breastfeeding, such as inadequate operationalization of the rapid HIV test.
FundingGlaucia Talita Possolli received a Master's Degree grant from CAPES.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Possolli GT, de Carvalho ML, de Oliveira MI. HIV testing in the maternity ward and the start of breastfeeding: a survival analysis. J Pediatr (Rio J). 2015;91:397–404.
Study conducted at Escola Nacional de Saúde Pública (ENSP), Fundação Oswaldo Cruz (FIOCRUZ), Rio de Janeiro, RJ, Brazil.