To assess the level of agreement in health-related quality of life between children with Post-infectious Bronchiolitis Obliterans and their parent (so-called proxy).
MethodsParticipants aged between 8and 17 years who had been previously diagnosed with Post-infectious Bronchiolitis Obliterans were regularly followed up at a pediatric pulmonology outpatient clinic. Parents or legal guardians (caregivers) of these patients were also recruited for the study. A validated and age-appropriate version of the Pediatric Quality of Life Inventory 4.0 was used for the assessment of health-related quality of life. Caregivers completed the corresponding proxy versions of the questionnaire. The correlation between self and proxy reports of health-related quality of life was determined by intra-class correlation coefficient and dependent t-tests.
ResultsThe majority of participants were males (79.4%), and the average age was 11.8 years. Intra-class correlations between each of the Pediatric Quality of Life Inventory 4.0 domains and the total score were all lower than 0.6, with a range between 0.267 (poor) and 0.530 (fair). When the means of each domain and the total score of the questionnaires were compared, caregivers were observed to have a significantly lower health-related quality of life score than children, with the exception of the social domain in which the difference was not significant. However, the differences in score exceeded the critical threshold difference of four points in all other domains.
ConclusionProxies of children and adolescents with Post-infectious Bronchiolitis Obliterans appear to consistently perceive their children as having lower health-related quality of life than how the patients perceive themselves.
Avaliar o nível de concordância a respeito da qualidade de vida relacionada à saúde entre crianças com bronquiolite obliterante pós-infecciosa e seus pais (responsáveis).
MétodosOs participantes entre 8–17 anos, anteriormente diagnosticados com bronquiolite obliterante pós-infecciosa, foram acompanhados regularmente no ambulatório de pneumologia pediátrica. Os pais ou responsáveis legais (cuidadores) desses pacientes também foram convidados a participar do estudo. Uma versão validada e adequada para a idade do Inventário Pediátrico de Qualidade de Vida, versão 4.0, foi utilizada para a avaliação da qualidade de vida relacionada à saúde. Os cuidadores concluíram as versões do questionário correspondentes aos responsáveis. A correlação entre os autorrelatos e os relatos dos responsáveis da qualidade de vida relacionada à saúde foi determinada pelo coeficiente de correlação intraclasse e pelos testes t dependentes.
ResultadosA maior parte dos participantes era do sexo masculino (79,4%) e a idade média foi 11,8 anos. As correlações intraclasse entre cada um dos domínios do Inventário Pediátrico de Qualidade de Vida e o escore total foram todas inferiores a 0,6, com intervalo entre 0,267 (baixo) e 0,530 (justo). Quando as médias de cada domínio e o escore total dos questionários foram comparados, observamos que os cuidadores apresentaram qualidade de vida relacionada à saúde significativamente menor em comparação com as crianças, com exceção do domínio social, no qual a diferença não foi significativa. Contudo, as diferenças no escore ultrapassaram o limite de diferença essencial de 4 pontos em todos os outros domínios.
ConclusãoOs responsáveis pelas crianças e adolescentes com bronquiolite obliterante pós-infecciosa parecem perceber de forma consistente que suas crianças possuem qualidade de vida relacionada à saúde menor que os próprios pacientes.
Post-infectious Bronchiolitis Obliterans (PIBO) is an uncommon and severe respiratory disease characterized by chronic obstruction of the small airways.1–9 As a result, it has a predictable negative impact on daily-life functions and overall quality of life.
In an attempt to understand the extent of this impact, we recently reported that children and adolescents with PIBO had lower scores of health-related quality of life (HRQoL) than healthy individuals in both physical and school domains.10 An important part of managing chronic pediatric conditions is controlling symptoms and promoting the proper psycho-social development of patients.11 Assessment of the latter, by measuring the objective outcome, is more complex than the former. Therefore, the use of subjective measures such as patient-reported outcomes (PROs) should be encouraged in clinical practice as key complementary tools for the care of both adult and pediatric patients with chronic disease.
When a patient is not able to respond to questions or express his/her own opinion due to cognitive limitations, a person familiar with the patient, having knowledge of the health problem that the patient has, can be an appropriate source of information. This individual is known as a proxy and is typically the spouse or a close family member who knows the patient well. Proxy assessments are generally used in research or clinical care of individuals who are very young, very old, and/or severely ill.12 The use of proxies, however, is also common in children with chronic conditions, raising some questions and debate over how parents and their children should agree on the assessment of the children's HRQoL by both of them.
In an ideal scenario, children and proxies participate together in the decision-making process regarding the management of the disease. As differences in perception of patients’ HRQoL could influence intervention, it would be vital for clinicians to understand the basis and importance of such differences while counseling families. Differences in HRQoL between groups could be attributed to interventions when in fact they were due to reporting differences.13
Despite the severity of PIBO and its effect on the patient's quality of life, studies evaluating the agreement in the assessment of health-related quality of life (HRQoL) between children and their proxies have not yet been published.14 Thus, the objective of this study was to evaluate the agreement between self-reports and proxy reports of HRQoL in children with PIBO.
MethodsWe included both children and adolescent patients with PIBO aged 8–17 years in follow-up at a pediatric pulmonology clinic in southern Brazil, as well as their parents or legal guardians (proxy). The criteria for the diagnosis of PIBO has been previously described.15 It was essentially based on the association of the following clinical, radiological, and functional criteria: (1) history of acute lung infection in a previously healthy child; (2) chronic breathing problems beyond four weeks since the initial event; (3) high-resolution computed tomography with common findings in PIBO, such as mosaic pattern, bronchiectasis, and atelectasis; (4) lung function tests indicating significant airflow limitation; and (5) exclusion of other chronic lung diseases, such as severe asthma, cystic fibrosis, primary ciliary dyskinesia, and immune deficiencies.
Lung functionIn order to categorize the functional impairment lung function was assessed by spirometry according to the American Thoracic Society criteria for acceptability and reproducibility.2 Spirometry was performed using Master-Screen equipment (Jaeger, Germany) and results were expressed as percentages of predicted values from Knudson's reference values.16
HRQoL was assessed using the Pediatric Quality of Life Inventory version 4.0 (PedsQL) generic core scale, which had been validated in Brazil in earlier studies.17,18 The instrument included 23 items comprising the following domains: physical (eight items), emotional (five items), social (five items), and scholar (five items). We used both patient and proxy versions for children and their parents, respectively, with age-appropriate options for children aged 8–12 and 13–18 years. The items in each of the versions were essentially similar and only differed in terms of age-adjusted language and the use by either the patients themselves or their proxies. The scale and its domains referred to the perception of events and feelings in the previous month. Survey respondents answered using a five-point Likert scale, ranging from 0 (never a problem) to 4 (almost always a problem). To eliminate discrepancy due to potential reading difficulties, the PedsQL was applied through interview.18 Following the scale's instructions, items were scored inversely and transposed linearly on a scale of 0–100 (0=100, 1=75, 2=50, 3=25, 4=0). Thus, higher scores indicated better HRQoL. Two previously trained interviewers applied all questionnaires. Children and their proxies were interviewed separately.
Sample sizeWith one observation for child and the parent, and assuming the probability of a type 1 error of 5%, the probability of a type 2 (1-beta) error of 10%, an intraclass correlation coefficient of 0.7, 95% confidence interval, and required lower limit of no less than 0.3, the required sample size was 29 participants in each group (child and parent).
Statistical analysisVariable distribution was assessed using the Kolmogorov–Smirnov test. The values of mean and standard deviations represented the continuous variables, while absolute and relative frequencies represented the categorical measures. The agreement between self- and proxy report was determined with intra-class correlation coefficient (ICC) and dependent t-test. The level of significance was set at 5% (P<0.05). For the evaluation of the critical threshold difference the means of the groups were compared using the t-test. The critical threshold difference was considered at 4 points.18
Data analyses were performed using SPSS software version 17.0 (SPSS Inc, EUA). The use of the research instrument PedsQL had been previously authorized by the author of the questionnaire.19 The project was approved by the Institutional Research Ethics Committee, and participants provided written consent prior to participation.
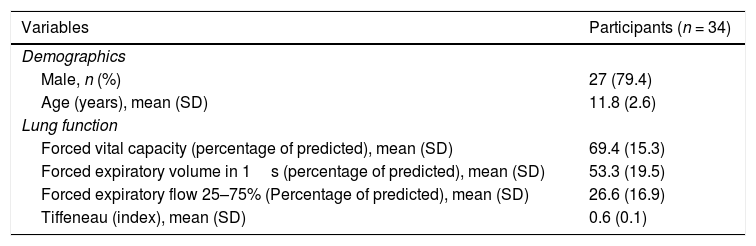
ResultsThe mean age of the patients was 11.8±2.6 years and most participants were males (79.4%). Lung function showed patterns of a moderate to severe obstructive airway disease, typical in children with PIBO (Table 1).
Characterization of children and adolescents diagnosed with BOPI.
| Variables | Participants (n = 34) |
|---|---|
| Demographics | |
| Male, n (%) | 27 (79.4) |
| Age (years), mean (SD) | 11.8 (2.6) |
| Lung function | |
| Forced vital capacity (percentage of predicted), mean (SD) | 69.4 (15.3) |
| Forced expiratory volume in 1s (percentage of predicted), mean (SD) | 53.3 (19.5) |
| Forced expiratory flow 25–75% (Percentage of predicted), mean (SD) | 26.6 (16.9) |
| Tiffeneau (index), mean (SD) | 0.6 (0.1) |
SD, standard deviation.
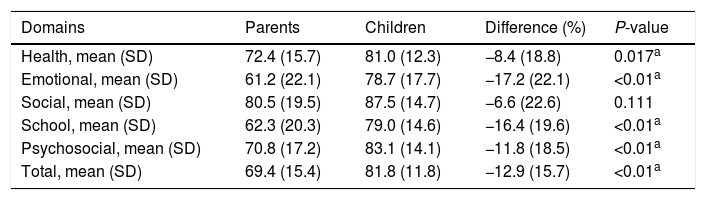
When PedsQL results from the children were compared with those of their proxy children generally scored significantly better than their parents, both in terms of the total score and individually on most domains of the scale. In other words, parents considered their children to have a lower HRQoL than that evaluated by the patients themselves. The only exception was the social domain of the scale, where differences between patients and proxy were not significant (Table 2). However, all the differences were clinically relevant (>4 points).
Differences in the domains and the total self-reported score by children and parents.
| Domains | Parents | Children | Difference (%) | P-value |
|---|---|---|---|---|
| Health, mean (SD) | 72.4 (15.7) | 81.0 (12.3) | −8.4 (18.8) | 0.017a |
| Emotional, mean (SD) | 61.2 (22.1) | 78.7 (17.7) | −17.2 (22.1) | <0.01a |
| Social, mean (SD) | 80.5 (19.5) | 87.5 (14.7) | −6.6 (22.6) | 0.111 |
| School, mean (SD) | 62.3 (20.3) | 79.0 (14.6) | −16.4 (19.6) | <0.01a |
| Psychosocial, mean (SD) | 70.8 (17.2) | 83.1 (14.1) | −11.8 (18.5) | <0.01a |
| Total, mean (SD) | 69.4 (15.4) | 81.8 (11.8) | −12.9 (15.7) | <0.01a |
SD, standard deviation.
Intra-class correlations between each of the PedsQL domains and the total score were all lower than 0.6, with a range between 0.267 and 0.530.
DiscussionThis study showed that patients with PIBO reported having a better quality of life than what their proxies perceived. As in other cases, particularly in chronic diseases, parents tend to assume a worse quality of life in their children than how patients assess themselves.13,20,21
A possible explanation for the lack of agreement, from a more conservative point of view, is that a child's cognitive internal structure is different from that of the adult.22 Children, therefore, could have a different understanding of the disease, its causes, expected natural history, and expected efficacy of the treatment. Another possible explanation is resilience and adaptation of children with PIBO; they have lived with the disease since very early in life, and they may have learned to adapt and carry out their daily activities despite their limitations. This inevitable situation probably led the children to accept the disease as a natural part of their being and influenced their perception (a much more optimistic one) of what is considered to be “normal”, compared to their parents. This is in line with the mismatch hypothesis, which states that individuals who experience adverse situations early in life trigger adaptive processes, thereby rendering an individual better adapted to challenges later in life.23 Another crucial factor worth mentioning is that being a caregiver (or proxy) of a child with a chronic and severe disease like PIBO often leads to high levels of anxiety and feelings of hopelessness, which in turn affects the parents’ own quality of life.24-26 A causal relation between interpretation bias and anxiety has been documented,27 and it can predispose parents to negatively distort their perceptions about their children.
One limitation of our study could be that we neither assessed the parents’ own HRQoL nor the emotional impact of their children's chronic disease on them. High emotional impact and/or low HRQoL could negatively influence their responses to how they perceived their children's HRQoL.
In conclusion, our study found that the assessment of HRQoL in children with PIBO differs between children with PIBO and their proxies. The disagreement, more than a contradiction, reflects two different visions that should be considered when caring for these patients.
FundingWe thank the Conselho Nacional de Desenvolvimento Científico e Tecnológico – CNPq and the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) for their support with graduates’ fellowships. Rita Mattiello and Ricardo Stein hold CNPq fellowships.
Conflicts of interestThe authors declare no conflicts of interest.
We thank the parents and patients for participating in this study.
Please cite this article as: Sarria EE, Mundstock E, Mocelin HT, Fischer GB, Torres RR, Garbin JG, et al. Health-related quality of life in post-infectious bronchiolitis obliterans: agreement between children and their proxy. J Pediatr (Rio J). 2019;95:614–8.