To characterize the lingual frenulum of full-term newborns using two different protocols and to assess the association of the lingual frenulum with breastfeeding.
MethodsThis non-probabilistic sample consisted of 449 mother/baby binomials. For the anatomo-functional evaluation of the frenulum, the Neonatal Tongue Screening Test and the Bristol Tongue Assessment Tool were used for the evaluation of the lingual frenulum. Breastfeeding was evaluated using the protocol proposed by UNICEF. Scores were created (good, fair, poor) to evaluate every aspect of the breastfeeding to be observed. The results were analyzed through descriptive and inferential statistics and association tests (Pearson's chi-squared and Fisher's exact test).
ResultsThe study showed that 14 babies had a lingual frenulum alteration, of whom three had difficulties during suction, requiring frenotomy in the first week of life, whereas 11 had no difficulties during breastfeeding. Regarding the breastfeeding evaluation, 410mother/baby binomials had good, 36 regular, and three had bad scores. There was a statistically significant association between the tongue-tie test protocol and breastfeeding (p=0.028) and between the Bristol Tongue Assessment Tool protocol and breastfeeding (p=0.028).
ConclusionAlterations in the lingual frenulum are associated with interferences in the quality of breastfeeding and thus, evaluation of the lingual frenulum in newborns is important.
Caracterizar o frênulo lingual de recém-nascidos a termo, utilizando dois protocolos diferentes e verificar a relação do frênulo lingual com o aleitamento materno.
MétodoA amostra não probabilística foi constituída por 449 binômios mãe/bebê. Para a avaliação anatomofuncional do frênulo, utilizou-se o protocolo de avaliação do frênulo lingual para bebês “Teste da Linguinha” e o Bristol Tongue Assessment Tool. A mamada foi avaliada com o protocolo proposto pelo UNICEF. Foram criados escores (bom, regular, ruim) para avaliar cada aspecto da mamada a ser observada. Os resultados foram analisados através de estatísticas descritivas e inferenciais e testes de associação (Qui-quadrado de Pearson e Exato de Fisher).
ResultadosO estudo mostrou que 14 bebês apresentaram alteração de frênulo lingual, nos quais três com dificuldade durante a sucção, necessitando de frenotomia na primeira semana de vida e 11 sem dificuldades durante a amamentação. Quanto à avaliação da mamada, 410 binômios mãe/bebê apresentaram o escore bom, 36 regular e 3 ruim. Houve associação estatisticamente significativa entre o protocolo “Teste da Linguinha” e amamentação (p=0,028) e entre o protocolo Bristol Tongue Assessment Tool e amamentação (p=0,028).
ConclusãoAlterações no frênulo lingual estão associadas a interferências na qualidade da amamentação, sendo importante a avaliação do frênulo lingual em recém-nascidos.
In the first six months of life, breastmilk should be the exclusive source of nutrition. Theoretically, every newborn without functional limitations has the capacity for breastfeeding.1
There are three oral reflexes of the newborn (NB) that will guarantee feeding in the initial phase of development: rooting, whose function is to locate the breast; suction, which is the withdrawal of milk from the nipple ducts; and swallowing.2
Breastfeeding is directly related to the sucking and swallowing functions, which are coordinated with breathing. The participation of the tongue movements is fundamental, since it functions to produce the anterior seal, adhered around the nipple, and the posterior seal, adhered to the soft palate and pharynx.3 Therefore, any restriction to the free movement of the tongue can result in function impairment, thus making breastfeeding difficult.4
The lingual frenulum alteration or ankyloglossia, popularly known as tongue-tie, is a congenital anomaly in which a small portion of tissue, which should have undergone apoptosis during embryonic development, remains in the sublingual surface.5
Ankyloglossia in children can lead to several problems, such as difficulties in breastfeeding, speech disorders, poor oral hygiene, and bullying by peers during childhood and adolescence. The effect of ankyloglossia on breastfeeding has been discussed in the medical literature.6 The functional impact of “tongue tie” on breastfeeding is a controversial point, since for some authors there is a tendency for the functional limitation to decrease with increasing age,7 while for other researchers it is necessary to identify the changes in the lingual frenulum in the first months of life, to prevent early weaning and, subsequently, speech alterations.8,9
The lack of standardized criteria for the diagnosis and classification of the lingual frenulum is one of the main criticisms of the Canadian Paediatric Research Society,10 and evaluation proposals based on visual clinical inspection have been found, which justify the great variation in the prevalence of ankyloglossia, between 0.88% and 12.7%.11–13
On June 20, 2014, Law No. 13,002 was approved, which requires lingual frenulum evaluation in newborns in all Brazilian hospitals and maternity wards, allowing the identification of lingual frenulum alterations and tongue movement limitations, which are important for sucking, chewing, swallowing, and speaking.14
Studies that associate the suction and swallowing functions to the anatomical variations of the frenulum are scarce. Therefore, this study aimed to characterize the lingual frenulum in full-term newborns, using two different protocols, as well as to verify the association between the lingual frenulum and breastfeeding.
MethodsThis is a cross-sectional, descriptive study of a population consisting of mother/baby binomials cared for at the rooming-in setting of Instituto de Medicina Integral Prof. Fernando Figueira (IMIP), Recife, state of Pernambuco, Brazil, in the months of March to May of 2016. A non-probabilistic sample was obtained, since all the babies born during this period (spontaneous demand) participated in the study, respecting the inclusion and exclusion criteria. The sample size was calculated based on an infinite population size. The EPI-INFO program (Centers for Disease Control and Prevention, EPI-INFO, version 7.2.2.2, GA, USA) was used to determine the sample size. A 5% error was established, with a reliability of 95% and an expected proportion of 50%, since the prevalence of ankyloglossia is unknown. Thus, 384 binomials were obtained, plus 15% so that any losses would not compromise the sample representativeness, therefore totaling a minimum sample of 442, albeit 449 were effectively collected. Newborns receiving infant formula (born to mothers carrying viruses transmitted through breast milk or using medication that made breastfeeding impossible), preterm infants with perinatal complications such as craniofacial anomalies, neurological diseases, and genetic syndromes visible at the time of assessment were excluded.
The infant lingual frenulum evaluation was performed during the data collection, followed by the observation of the baby's performance during breastfeeding at the mother's breast. The collection was performed by a researcher, and when an alteration was identified in the lingual frenulum or during the breastfeeding, a second researcher re-evaluated the infant together with the first researcher, aiming at reaching a consensus. The two researchers (dental surgeons) were previously trained and calibrated.
To evaluate the lingual frenulum, the Lingual Frenulum Evaluation Protocol for Infants was applied, which allows verifying the anatomical characteristics of the lingual frenulum and the suction and swallowing functions in infants. This protocol is divided into clinical history, anatomo-functional evaluation, and evaluation of non-nutritive and nutritive suction. It has independent scores and can be applied in parts until the 6th month of life.15 As the present study was carried out in newborns during their stay in the rooming-in setting, it was decided to apply the protocol in its neonatal screening modality16 (booklet), which consisted in applying only part I of the Protocol (anatomo-functional assessment). The following was observed in the anatomo-functional assessment: resting lip posture; tendency of tongue positioning during crying; shape of the tongue tip when elevated during crying; and lingual frenulum (thickness, fixation on the sublingual surface, fixation on the floor of the mouth). For data analysis, a score greater than or equal to 7 was considered as interference of the lingual frenulum in the tongue movements.15,16
Another protocol used to evaluate the lingual frenulum was the Bristol Tongue Assessment Tool (BTAT), a simple tool that shows scores and the classification of tongue function reduction severity. It evaluates four aspects to the frenulum, as follows: appearance of the tip of the tongue; fixation of the frenulum to the lower alveolus; elevation of tongue during open-mouth crying; and protrusion of the tongue over the gingiva. The scores for the four items are added and can range from 0 to 8; a score of 0–3 indicates severe reduction in tongue function.17
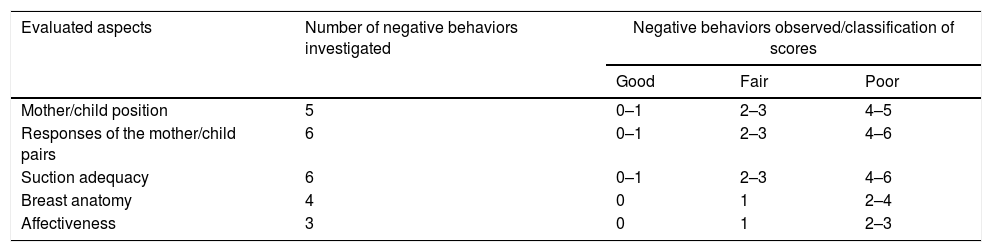
Subsequently, the UNICEF Breastfeeding Assessment and Observation Protocol18 was chosen to evaluate the performance of the mother/baby binomial at the time of breastfeeding. It consists of five categories, indicating favorable behaviors and behaviors indicating difficulties in breastfeeding, addressing aspects related to the position, responses, affection bonding, anatomy, and suction. In this study, the frequency of unfavorable behaviors for each aspect of breastfeeding was investigated and, according to the number of negative behaviors observed, were classified into scores (good, fair, and poor), according to a study by Carvalhaes et al. performed in 2003, as shown in Table 1.19
Criteria for classification of the scores used in the breastfeeding evaluation according to each evaluated aspect (Carvalhaes et al.).19
| Evaluated aspects | Number of negative behaviors investigated | Negative behaviors observed/classification of scores | ||
|---|---|---|---|---|
| Good | Fair | Poor | ||
| Mother/child position | 5 | 0–1 | 2–3 | 4–5 |
| Responses of the mother/child pairs | 6 | 0–1 | 2–3 | 4–6 |
| Suction adequacy | 6 | 0–1 | 2–3 | 4–6 |
| Breast anatomy | 4 | 0 | 1 | 2–4 |
| Affectiveness | 3 | 0 | 1 | 2–3 |
Infants that showed lingual frenulum alterations and difficulty during suction were submitted to frenotomy in the first week of life, returning to the service within one week and after 30 days for re-evaluation. Infants who had lingual frenulum alterations without difficulty in breastfeeding returned to the service within 30 days and were reassessed by the researcher. When they returned, all mothers answered the following questions: Are you breastfeeding your baby? Have you offered any complementary food to your child? What is the reason for the complementation?
The results were statistically analyzed using the SPSS program (SPSS Statistics for Windows, Version 17.0, Chicago, USA), with descriptive and inferential statistical analyses. To verify the association between the lingual frenulum variables and the newborn's performance at breastfeeding, Pearson's chi-squared test and Fisher's exact test were used. A significance level of 5% was considered in all analyses.
The study was approved by the Ethics Committee of Human Research of Instituto de Medicina Integral Prof. Fernando Figueira – IMIP, according to Opinion No. 1,066,444, of May 13, 2015. It should be clarified that only babies whose mothers and/or guardians accepted to participate were included in the study, after signing the informed consent. The confidentiality of their identities and the use of information exclusively for research purposes were guaranteed.
Twenty-nine babies were re-examined by the two researchers to assess the inter-examiner agreement; the Kappa statistical test was used for the analysis, in which the obtained values ranged between 0.70 and 1.0, considered an indication of excellent agreement.
ResultsOf the 449mother/baby binomials, 240 (46.5%) newborns were females, but the higher prevalence (64.28%) of frenulum alterations was found in the male gender. The mean maternal age was 26 years. Most reported having completed high school (42.5%) and 245 (54.6%) mothers self-declared their ethnicity as mixed-race, 279 (62.1%) came from other cities in the state of Pernambuco; and 173 (38.5%) had a minimum-wage income.
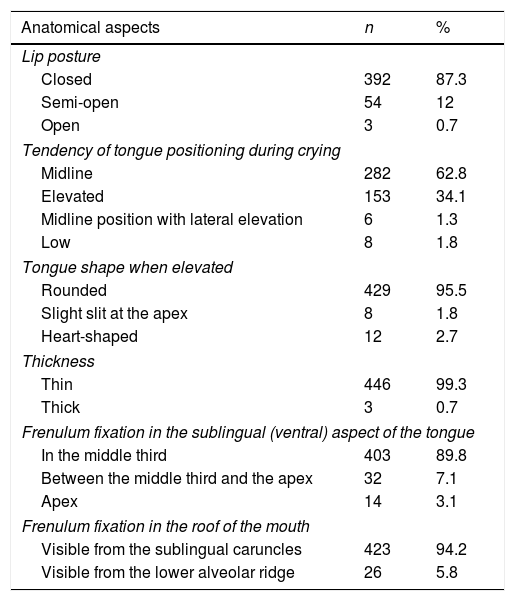
A correlation was identified regarding the lingual frenulum characterization between the two protocols in the same babies. According to them, 14 (3.11%) babies had lingual frenulum alterations. The results obtained regarding the anatomical aspects, when the anatomo-functional evaluation of the Lingual Frenulum Evaluation Protocol was used, are described in Table 2.
Anatomical aspects related to infants and lingual frenulum, according to the Protocol of the Lingual Frenulum Assessment with Scores for Infants – Instituto de Medicina Integral Prof. Fernando Figueira, Pernambuco, Brazil, 2016.
| Anatomical aspects | n | % |
|---|---|---|
| Lip posture | ||
| Closed | 392 | 87.3 |
| Semi-open | 54 | 12 |
| Open | 3 | 0.7 |
| Tendency of tongue positioning during crying | ||
| Midline | 282 | 62.8 |
| Elevated | 153 | 34.1 |
| Midline position with lateral elevation | 6 | 1.3 |
| Low | 8 | 1.8 |
| Tongue shape when elevated | ||
| Rounded | 429 | 95.5 |
| Slight slit at the apex | 8 | 1.8 |
| Heart-shaped | 12 | 2.7 |
| Thickness | ||
| Thin | 446 | 99.3 |
| Thick | 3 | 0.7 |
| Frenulum fixation in the sublingual (ventral) aspect of the tongue | ||
| In the middle third | 403 | 89.8 |
| Between the middle third and the apex | 32 | 7.1 |
| Apex | 14 | 3.1 |
| Frenulum fixation in the roof of the mouth | ||
| Visible from the sublingual caruncles | 423 | 94.2 |
| Visible from the lower alveolar ridge | 26 | 5.8 |
Total of 449 assessed infants.
The data obtained showed that most of the newborns had a resting closed lip posture, tendency of tongue positioning in the midline, and rounded tongue shape. As for the visualization of the lingual frenulum, it was possible in 233 (51.9%) of the newborns.
Most infants had a thin lingual frenulum attached to the middle third of the tongue and visible from the sublingual caruncles on the mouth floor.
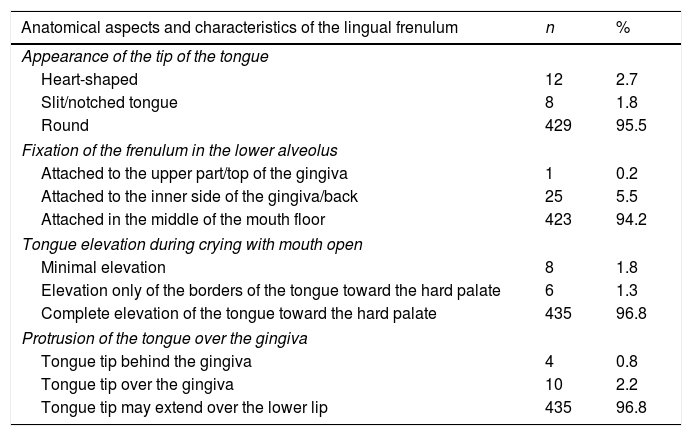
The results obtained with the BTAT protocol application are shown in Table 3. According to the protocol, most infants had round appearance of the tongue tip, complete elevation of the tongue toward the hard palate during crying, and the tongue could protrude over the lower lip. As for the lingual frenulum fixation, most had the frenulum attached to the middle of the mouth floor.
Anatomical aspects and characteristic of the lingual frenulum, according to the protocol applied to evaluate the lingual frenulum – BTAT – Instituto de Medicina Integral Prof. Fernando Figueira, Pernambuco, Brazil, 2016
| Anatomical aspects and characteristics of the lingual frenulum | n | % |
|---|---|---|
| Appearance of the tip of the tongue | ||
| Heart-shaped | 12 | 2.7 |
| Slit/notched tongue | 8 | 1.8 |
| Round | 429 | 95.5 |
| Fixation of the frenulum in the lower alveolus | ||
| Attached to the upper part/top of the gingiva | 1 | 0.2 |
| Attached to the inner side of the gingiva/back | 25 | 5.5 |
| Attached in the middle of the mouth floor | 423 | 94.2 |
| Tongue elevation during crying with mouth open | ||
| Minimal elevation | 8 | 1.8 |
| Elevation only of the borders of the tongue toward the hard palate | 6 | 1.3 |
| Complete elevation of the tongue toward the hard palate | 435 | 96.8 |
| Protrusion of the tongue over the gingiva | ||
| Tongue tip behind the gingiva | 4 | 0.8 |
| Tongue tip over the gingiva | 10 | 2.2 |
| Tongue tip may extend over the lower lip | 435 | 96.8 |
BTAT, Bristol Tongue Assessment Tool.
Total of 449 assessed infants.
Regarding the breastfeeding evaluation, also performed during the initial screening in the maternity, 409 (91%) infants showed a good score. The main cause of difficulties during breastfeeding was the anatomy of the mother's breasts (51.3%). Among the 14 newborns who had a lingual frenulum alteration, three had difficulties during suction, requiring frenotomy in the first week of life. These babies returned to the service after one week, as well as after 30 days for re-evaluation. Those who did not undergo the frenotomy returned after 30 days and were reassessed by the researcher. When they returned, all babies were being exclusively breastfed and had an average weight gain of 1100kg.
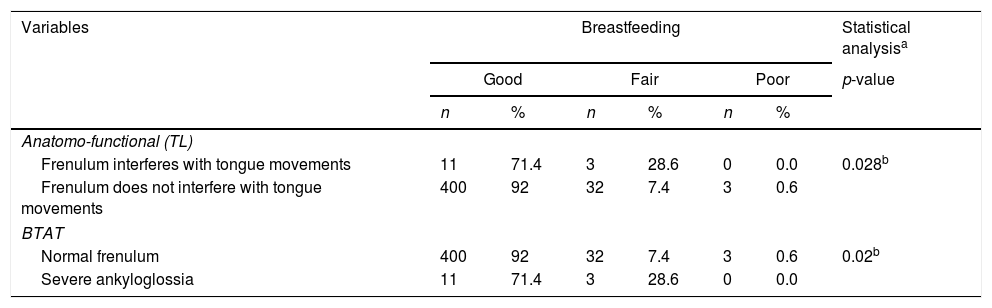
There was a statistically significant association between the Neonatal Tongue Screening Test protocol and the quality of breastfeeding (p=0.028) and between the BTAT protocol and the quality of breastfeeding (p=0.028) (Table 4).
Association between the protocols used to evaluate the lingual frenulum and breastfeeding Instituto de Medicina Integral Prof. Fernando Figueira, Pernambuco, Brazil, 2016.
| Variables | Breastfeeding | Statistical analysisa | |||||
|---|---|---|---|---|---|---|---|
| Good | Fair | Poor | p-value | ||||
| n | % | n | % | n | % | ||
| Anatomo-functional (TL) | |||||||
| Frenulum interferes with tongue movements | 11 | 71.4 | 3 | 28.6 | 0 | 0.0 | 0.028b |
| Frenulum does not interfere with tongue movements | 400 | 92 | 32 | 7.4 | 3 | 0.6 | |
| BTAT | |||||||
| Normal frenulum | 400 | 92 | 32 | 7.4 | 3 | 0.6 | 0.02b |
| Severe ankyloglossia | 11 | 71.4 | 3 | 28.6 | 0 | 0.0 | |
BTAT, Bristol Tongue Assessment Tool.
Total of 449 mother/infant binomials.
The present study identified a rate of frenulum alteration prevalence within the variation range found in the literature, of 0.8–12.7%.11–13,20
As described in the literature, boys seem to be more often affected than girls, as evidenced in the assessed sample, in which male gender was predominant.21
According to the technical-scientific opinion of the Instituto de Saúde da Criança in São Paulo, there is not enough scientific evidence to diagnose frenulum alterations and their association with breastfeeding, as proposed in the Lingual Frenulum Evaluation Protocol for Infants.22 The opinion also states that there is no gold standard for the ankyloglossia diagnostic test. The authors, using the Bristol Tongue Assessment Tool (BTAT), concluded that it does not provide reliable results to ascertain whether children with tongue-tie had difficulties in breastfeeding.23 In this study, the two tools used, the Lingual Frenulum Assessment Protocol with Scores for Babies and the BTAT were effective in correlating breastfeeding with the lingual frenulum characteristics (p=0.028).
It is possible to find divergences in the literature regarding the association between the lingual frenulum and breastfeeding. In a literature review, in which diagnostic and treatment criteria for ankyloglossia were assessed in 64 analyzed articles, it was demonstrated that breastfeeding problems in newborns were associated with tongue-tie, similar to what was found in this research; however, more controlled trials need to be performed to identify an ideal treatment option.8
Most infants had a good score regarding the breastfeeding evaluation; this can be justified by the fact that IMIP is a baby-friendly hospital, where the mothers are advised by the Neonatology, the Human Milk Bank, and Breastfeeding Incentive Center teams of IMIP (BLH/CIAMA/IMIP) from birth, so that breastfeeding is established and maintained.
Ankyloglossia is a recognized cause of breastfeeding difficulty and, if untreated, can result in nipple pain and trauma, ineffective feeding, and low infant weight gain. In some cases, this condition can result in poor breastmilk production. The problem usually occurs in the first week after birth, but its effect on feeding is difficult to measure.24 In this study, of the 14 babies diagnosed with ankyloglossia, 11 had no breastfeeding difficulties at the 30-day follow-up and were monitored. Only three showed negative behaviors during the feeding evaluation, affecting the success of breastfeeding; weight loss was verified in these infants and thus, in the presence of these difficulties, frenotomies were performed in the 1st week of life.
It is worth mentioning in this study the importance of the frenulum evaluation together with the feeding assessment, and the occurrence of interference with breastfeeding, as well as weight loss to justify the surgical intervention in the first weeks of life. These interventions, when performed, resulted in the infant's nutritive sucking improvement and the mother's report of greater comfort at the time of breastfeeding.
The authors concluded in their research that frenotomy is a safe and fast procedure, with low morbidity, and it improves the results of breastfeeding. Additionally, when the frenotomy is performed at an early age, it results in better breastfeeding outcomes.25 In a systematic review, a small body of evidence suggests that the frenotomy may be associated with improvements reported by the mother regarding breastfeeding and, potentially, nipple pain, but with small short-term studies with inconsistent methodology, the strength of evidence is low and insufficient.26 In another systematic review, consisting of five randomized clinical trials and eight case studies, the authors concluded that frenotomy favors long-term breastfeeding in more than 50% of cases.27
There is no consensus yet in the literature regarding the efficacy of the frenotomy for the treatment of Ankyloglossia in infants.22 The work of the multidisciplinary team in this process is of the utmost importance, contributing to the diagnosis of possible alterations in the frenulum, in breastfeeding, and in decision-making, preventing early weaning and possible changes in the stomatognathic system.
According to the study, it was possible to conclude that alterations in the lingual frenulum are associated with interferences in the quality of breastfeeding, making the evaluation of the lingual frenulum in newborns an important matter. Longitudinal studies are suggested for the improvement of scientific evidence that will contribute to the reinforcement and encouragement of exclusive breastfeeding in the first six months of life.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Araujo MC, Freitas RL, Lima MG, Kozmhinsky VM, Guerra CA, Lima GM, et al. Evaluation of the lingual frenulum in newborns using two protocols and its association with breastfeeding. J Pediatr (Rio J). 2020;96:379–85.