To assess the efficacy of the Baby's Mouth early dental care prevention and promotion program in preventing oral diseases (caries, gingivitis, or malocclusions) in children attended since 2010.
MethodsThis was a cross-sectional and cohort study that assessed 252 children between 36 and 60 months of age in both sexes. The children were divided into three groups: G1: effective participants of the program from birth; G2: children who have stopped participating for more than 24 months, and G3: children who have never attended a prevention program. The evaluation was carried out in two stages: first, an interview with the mothers and, afterwards, a clinical children examination to assess the presence of caries, gingivitis, and malocclusion. The chi-squared test was used for statistical analysis between groups (p<0.05).
ResultsThe diseases assessed were: caries (G1: 5.9%, G2: 54.7%, G3: 70%), gingivitis (G1: 8.3%, G2: 17.9%, G3: 40.5%), and malocclusion (G1: 22.6%; G2: 28.6%; G3: 50%). For gingivitis, there was no significant difference when comparing G1 and G2 (p=0.107), but it was significant between G1 and G3 (p<0.001). Regarding malocclusion, a statistically significant relationship was observed (p=0.004) among all groups.
ConclusionThe prevention and promotion program in public oral health was effective in preventing caries disease, gingivitis, and malocclusion in children under 5 years of age.
Avaliar a eficácia do programa de prevenção e promoção de cuidados dentários precoce da boca do bebê, a fim de prevenir doenças bucais (cáries, gengivite ou má oclusões) em crianças atendidas desde 2010.
MétodosEstudo transversal e de coorte com avaliação de 252 crianças entre 36 e 60 meses de idade de ambos os sexos. As crianças foram divididas em dois grupos: G1: participantes efetivos do programa a partir do nascimento; G2: crianças que pararam de participar por mais de 24 meses do programa; e G3: crianças que nunca participaram de um programa de prevenção. A avaliação foi feita em dois estágios: entrevista com as mães e, depois, um exame clínico nas crianças para analisar cáries, gengivite e oclusão. Foi utilizado o teste qui-quadrado para análise estatística entre os grupos (p<0,05).
ResultadosAs doenças analisadas foram: cáries (G1: 5,9%, G2: 54,7%, G3: 70%), gengivite (G1: 8,3%, G2: 17,9%, G3: 40,5%) e má oclusão (G1: 22,6%; G2: 28,6%; G3: 50%). Para gengivite, não houve diferença significativa ao comparar G1 e G2 (p=0,107), porém a diferença foi extremamente significativa entre G1 e G3 (p<0,001). Nas oclusões, houve uma relação estatisticamente significativa (p=0,004) entre todos os grupos.
ConclusãoO programa de prevenção e promoção de saúde bucal pública foi efetivo na prevenção de cáries, gengivite e má oclusão em crianças com menos de cinco anos de idade.
Oral health is part of general health and should be accessible to all people regardless of age, race, creed, color, sex, or socioeconomic status.1 Dentistry has sought to change the curative approach of oral problems to a broader work aiming to identify and reach the determinants of the health disease process. These changes promote awareness for maintaining health with early initiation of dental care, thus avoiding and/or reducing the sequelae of the main problems that affect the oral health of the population.2 Dentistry for babies has been gaining great attention worldwide and has become an alternative in the prevention and control of oral diseases in early childhood.3
Early childhood is a fundamental period in the psycho-social development of the individual; oral health promotion measures for children under 5 years are essential for maintaining health and proper development of digestion, phonation, and respiration.1 The age at the first preventive dental visit has a positive and significant effect on oral health costs, which are, on average, lower for children who received early preventive treatment.4
A local study5 demonstrated the great demand for dental care of children 2–5 years of age with presence of pain and sequelae of oral diseases in the city of Gurupi, Tocantins State, northern region of Brazil. The public program for the promotion of oral health in children (POHC), called Baby's Mouth, was implemented in 2010 in partnership with the City Hall and Centro Universitário UnirG (University Center of Gurupi). This program encompasses the period from gestation until 5 years of age. The children have been enrolled in this public program since birth. The professionals treated edentulous children, and all of them received clinical examination, oral cleaning, and quarterly control. The project also provided orientation to mothers regarding diet, and they received a returning card. The professionals followed-up the child's dental eruption, occlusion stabilization, and monitored them up to 5 years of age; if any changes were detected during this period, the staff intervened according to the dental standards of the American Academy of Pediatric Dentistry.6
The aim of this study was to assess the efficacy of the Baby's Mouth early dental care prevention and promotion program in preventing oral diseases (caries, gingivitis, or malocclusions) in children attended since 2010.
MethodsThis was a cross-sectional and cohort study carried out in the Legal Amazon region, covering the micro-region of Bananal Island, within the scope of the public health network of Gurupi (TO), with an area of 1,836,091km2 and a total population of 76,755 individuals, approved by the Human Research Ethics Committee of the Centro Universitário UnirG, under protocol number 19895713.0.0000.5518.
Inclusion and exclusion criteriaFor all groups, patients aged 36–60 months of both sexes and who were assisted at one of the ten primary care units (PCU) of the municipality were included. The age of 3–5 years was selected to allow evaluation of the effect of the activities performed by this oral health program; it was stipulated that the study would assess the results of the program with a minimum of 30 months of attendance for G1 and 12 months for G2.
In 2015, of the 1303 enrolled in the program from 0 to 6 months in the period from 2010 to 2014, 423 children (52%) were lost to follow-up after the first consultation, 171 (21%) after the second consultation, and 89 (11%) after the third consultation; the other losses occurred after the fourth consultation. Thus, during the 2015 study period, there were 488 completed records of children aged 0–5 years who were effective participants in the program.
For sample homogeneity in the groups, the number established was the quantity of Group 1.
Group 1 (G1): Of the 488 children from the 0 to 5-year-old total sample, who regularly participated in the POHC, children with semester frequency and enrolled in the program from birth (0–3 months) were chosen for the cohort study. This sample consisted of 106 children aged 3–5 years, using a sample calculation with an error possibility of 5%, a confidence level of 95%.
In Group 2 (G2), children who attended the program from birth (0–3 months) for at least 18 months and dropped out for more than 24 months were included. A total of 145 telephone records were obtained, from which 84 were randomly invited to participate in the study.
Group 3 (G3) consisted of a similar number of children with spontaneous demand who were vaccinated in the PCU and who had never participated in any oral health promotion program.
The exclusion criteria for G1 were incomplete records; for G2, lack of telephone contact or if the child had migrated to another prevention program; and for G3, if these children did not live in the region studied.
A total of 252 children aged 3–5 years were evaluated from February 2015 to March 2016. The G1 and G2 children were randomly selected by drawing of the patient's chart number. Patients in G1 were attended in the routine consultations, those in G2 were scheduled for attendance at the health clinic, and those G3 were selected when attending the PCU for vaccination, carrying out the study at this time. In the follow-up, three children from G1 were lost to follow-up, but three others were selected, thus the number of 84 participants remained. In G2, 14 children did not attend the appointment and new inclusions were performed until reaching the number of 84. In G3, the first 84 authorizations of examinations were reached for the study, with a weekly visit to each of the ten PCU.
The legal guardians received information about the methodology and the objectives of the research, having the right of non-participation without any harm to the dental care. In addition, legal guardians signed a term agreeing to participate in the research.
All exams and interviews were held in an appropriate PCU room intended for the care of the children of the program. The research was divided into two stages; the first one consisted of an interview with the mothers, containing 12 closed questions about their knowledge and attitudes regarding the oral health of their child. The mother was questioned about age, family income, schooling, employment, marital status, number of children, and knowledge about the children's oral health. The child was questioned about the habits, oral hygiene, and also related to the frequency of the program. During the interview, the program staff provided guidance and reinforcement of the necessary aspects pertinent to the child's age group. G2 and G3 children with oral alterations (caries, gingivitis, or malocclusion) detected during the study were referred to the public pediatric dentistry service at the PCU.
In the second stage, the child's oral cavity was assessed by a single, previously trained and qualified examiner (Kappa intra-rater index=0.86). During the data collection, 10% of the sample was reexamined (Kappa=0.89). This examiner was responsible for all the examinations of the children in the dental office, after brushing and under the light of the reflector, using instruments such as a periodontal probe, dental mirror, and gauze.
Dental caries were recorded based on the World Health Organization (WHO)7 oral health survey criteria and methods, using the decayed, extracted, and filled teeth (deft) index for primary dentition. Deft values higher than 6.5 indicate a very high prevalence; values between 4.5 and 6.5, high; between 2.7 and 4.4, moderate; between 1.2 and 2.6, low; and values lower than 1.2, very low prevalence.
The indicator used to measure changes in the gingival mucosa was the modified gingival index (GI) proposed by Lobene et al.,8 with following values for the observation criteria: 0 – absence of inflammation; 1 – mild inflammation (when slight color change and slight changes in the texture of any portion of the marginal gingiva or gingival papilla are observed); 2 – mild inflammation (same criteria as above, but completely involving or almost every portion of the marginal gingiva and the gingival papilla); 3 – moderate inflammation (marginal gingiva and bright, reddish, swollen, and/or hypertrophic gingival papillae); and 4 – severe inflammation (redness, edema and/or hypertrophy of the marginal gingiva or gingival papillae, spontaneous bleeding, congestion, and/or ulcerations).
Tests were performed to detect signs of malocclusion such as overjet, overbite, and crossbite.9 Overjet was analyzed by measuring the horizontal distance between the upper and lower incisors with the teeth in occlusion. The distance between the incisal edge of the prominent upper incisors and the vestibular face of the corresponding lower incisor was measured with the periodontal probe parallel to the occlusal plane. This distance was considered as normal, when up to 3mm; overjet, for values greater than 3mm; and as anterior crossbite, when the incisors were in negative occlusion distance from the lower incisal edge of the vestibular to the upper incisal border. Overbite was obtained by measuring the vertical distance between the edges of the upper and lower central incisors with the teeth in occlusion. This distance was considered normal when the upper incisors covered the lower incisors by up to 3mm; overbite, when this coverage was greater than 3mm; and open bite, when there was no overlap between the upper and lower incisors with a minimum space of 1mm between both incisal edges. Posterior crossbite was considered present when, in occlusion, the buccal cusps of the lower molars were displaced to the buccal on the buccal cusps of the maxillary molars. Only its presence or absence was considered, regardless of the side.
The clinical data and the information obtained through the questionnaires were described and the variables were assessed using Fisher's exact test and chi-squared test (p<0.05).
ResultsIn the present study, the mean family income of 1–2 minimum wages, and the mean age of the groups was 3.662±0.753 years in G1, 3.698±0.711 years in G2, and 3.714±0.744 years in G3. In all groups, most mothers had completed secondary education.
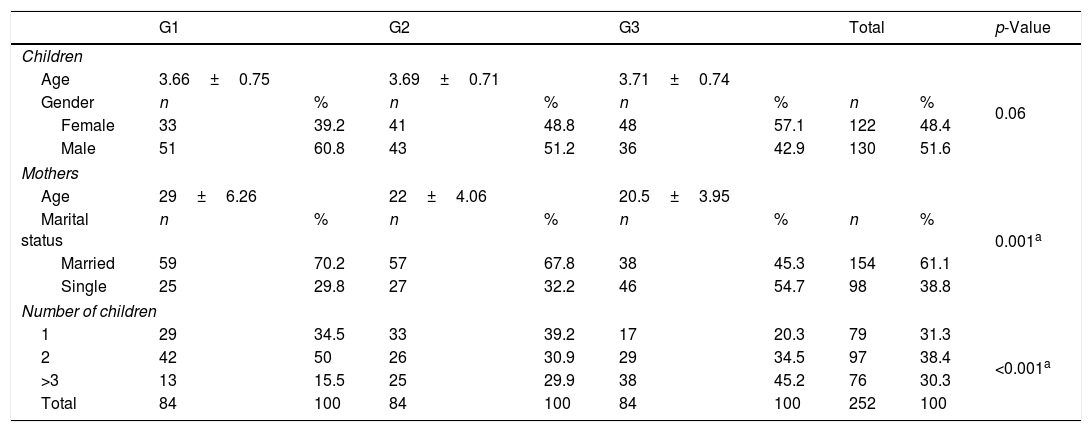
When analyzing the percentage components of the program in Table 1, a statistical significance was observed among the groups regarding the presence of partners; in G1 and G2, the majority were married. The mean number of children per mother was two children in G1, one child in G2, and three or more children in G3; this difference was statistically significant.
Sample profile (mothers and children).
| G1 | G2 | G3 | Total | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|
| Children | |||||||||
| Age | 3.66±0.75 | 3.69±0.71 | 3.71±0.74 | 0.06 | |||||
| Gender | n | % | n | % | n | % | n | % | |
| Female | 33 | 39.2 | 41 | 48.8 | 48 | 57.1 | 122 | 48.4 | |
| Male | 51 | 60.8 | 43 | 51.2 | 36 | 42.9 | 130 | 51.6 | |
| Mothers | |||||||||
| Age | 29±6.26 | 22±4.06 | 20.5±3.95 | 0.001a | |||||
| Marital status | n | % | n | % | n | % | n | % | |
| Married | 59 | 70.2 | 57 | 67.8 | 38 | 45.3 | 154 | 61.1 | |
| Single | 25 | 29.8 | 27 | 32.2 | 46 | 54.7 | 98 | 38.8 | |
| Number of children | |||||||||
| 1 | 29 | 34.5 | 33 | 39.2 | 17 | 20.3 | 79 | 31.3 | <0.001a |
| 2 | 42 | 50 | 26 | 30.9 | 29 | 34.5 | 97 | 38.4 | |
| >3 | 13 | 15.5 | 25 | 29.9 | 38 | 45.2 | 76 | 30.3 | |
| Total | 84 | 100 | 84 | 100 | 84 | 100 | 252 | 100 | |
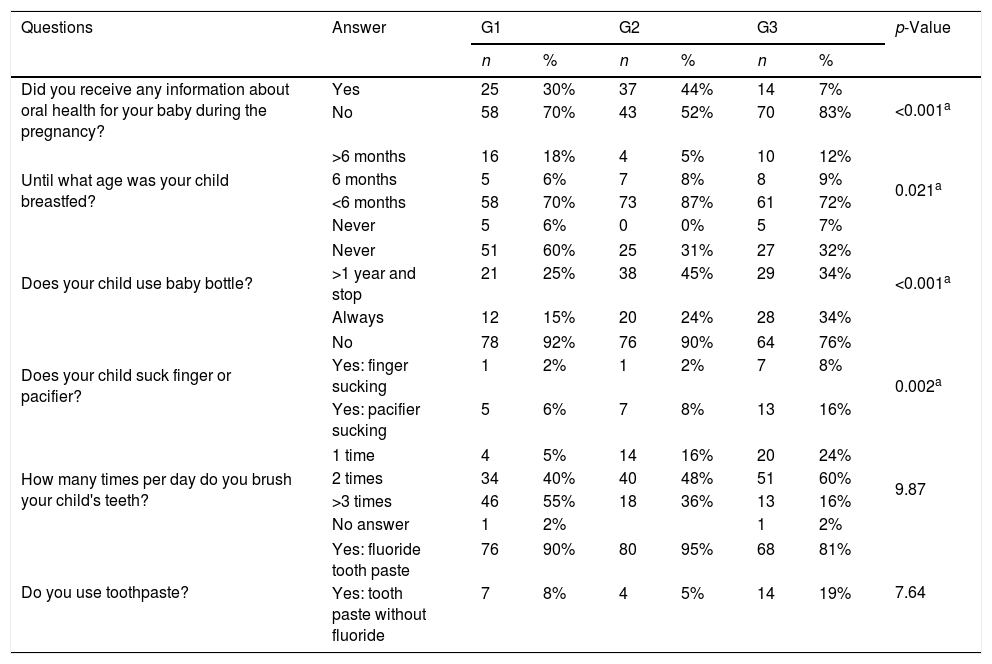
Table 2 indicated that, although several mothers reported not having received information about oral health in prenatal care, those in G3 had received practically no information; this difference was significant between the groups.
Maternal perceptions and knowledge about oral health care in early childhood in all groups.
| Questions | Answer | G1 | G2 | G3 | p-Value | |||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| Did you receive any information about oral health for your baby during the pregnancy? | Yes | 25 | 30% | 37 | 44% | 14 | 7% | <0.001a |
| No | 58 | 70% | 43 | 52% | 70 | 83% | ||
| Until what age was your child breastfed? | >6 months | 16 | 18% | 4 | 5% | 10 | 12% | 0.021a |
| 6 months | 5 | 6% | 7 | 8% | 8 | 9% | ||
| <6 months | 58 | 70% | 73 | 87% | 61 | 72% | ||
| Never | 5 | 6% | 0 | 0% | 5 | 7% | ||
| Does your child use baby bottle? | Never | 51 | 60% | 25 | 31% | 27 | 32% | <0.001a |
| >1 year and stop | 21 | 25% | 38 | 45% | 29 | 34% | ||
| Always | 12 | 15% | 20 | 24% | 28 | 34% | ||
| Does your child suck finger or pacifier? | No | 78 | 92% | 76 | 90% | 64 | 76% | 0.002a |
| Yes: finger sucking | 1 | 2% | 1 | 2% | 7 | 8% | ||
| Yes: pacifier sucking | 5 | 6% | 7 | 8% | 13 | 16% | ||
| How many times per day do you brush your child's teeth? | 1 time | 4 | 5% | 14 | 16% | 20 | 24% | 9.87 |
| 2 times | 34 | 40% | 40 | 48% | 51 | 60% | ||
| >3 times | 46 | 55% | 18 | 36% | 13 | 16% | ||
| No answer | 1 | 2% | 1 | 2% | ||||
| Do you use toothpaste? | Yes: fluoride tooth paste | 76 | 90% | 80 | 95% | 68 | 81% | 7.64 |
| Yes: tooth paste without fluoride | 7 | 8% | 4 | 5% | 14 | 19% | ||
G1 and G2 mothers enrolled their children in the program for prevention, while G3 mothers intended to take their child to dentist dental appointment only when treatment for caries or pain was needed. Patients in G2, the loss to follow-up was due to the fact that most mothers (54%) forgot the time of the consultation in the PCU; and 25% of the mothers claimed that they could not attend because they started to work.
Regarding the mothers’ knowledge about the question “when should the child be taken for the first visit to the dentist?,” mothers in G1 (69%) and G2 (74%) answered “before the first tooth erupted,” while 49% of the mothers in G3 answered “when the first tooth erupted” and 29%, “when the child presents some discomfort or pain.”
The deft index varied among the groups: G1, 0.05; G2, 1.96; and G3, 3.3.
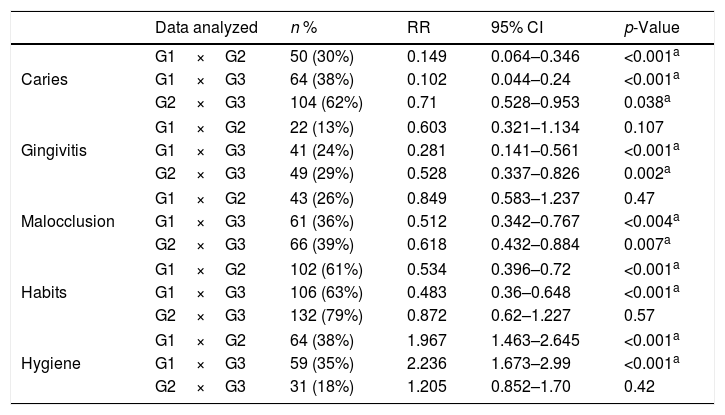
Regarding caries (Table 3), a linear relationship was observed between variables, in which all groups presented a significant difference. For gingivitis, no significant differences were observed when comparing G1 and G2, but significant differences were observed between G1 and G3. In the occlusions, a statistically significant relationship was observed among the three groups relating the lack of attendance in the program and the presence of malocclusion. In G2 and G3, the prevalence of these alterations was increased, since the patients participated partially or did not participate in the program.
Submission of data analyzed by comparing group to group.
| Data analyzed | n % | RR | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Caries | G1×G2 | 50 (30%) | 0.149 | 0.064–0.346 | <0.001a |
| G1×G3 | 64 (38%) | 0.102 | 0.044–0.24 | <0.001a | |
| G2×G3 | 104 (62%) | 0.71 | 0.528–0.953 | 0.038a | |
| Gingivitis | G1×G2 | 22 (13%) | 0.603 | 0.321–1.134 | 0.107 |
| G1×G3 | 41 (24%) | 0.281 | 0.141–0.561 | <0.001a | |
| G2×G3 | 49 (29%) | 0.528 | 0.337–0.826 | 0.002a | |
| Malocclusion | G1×G2 | 43 (26%) | 0.849 | 0.583–1.237 | 0.47 |
| G1×G3 | 61 (36%) | 0.512 | 0.342–0.767 | <0.004a | |
| G2×G3 | 66 (39%) | 0.618 | 0.432–0.884 | 0.007a | |
| Habits | G1×G2 | 102 (61%) | 0.534 | 0.396–0.72 | <0.001a |
| G1×G3 | 106 (63%) | 0.483 | 0.36–0.648 | <0.001a | |
| G2×G3 | 132 (79%) | 0.872 | 0.62–1.227 | 0.57 | |
| Hygiene | G1×G2 | 64 (38%) | 1.967 | 1.463–2.645 | <0.001a |
| G1×G3 | 59 (35%) | 2.236 | 1.673–2.99 | <0.001a | |
| G2×G3 | 31 (18%) | 1.205 | 0.852–1.70 | 0.42 | |
RR, relative risk; 95% CI, confidence interval.
Of the malocclusions, the most prevalent was open bite, followed by the anterior and posterior crossbite; the group that never attended the program (G3) presented a statistical difference in this oral alteration as much as G1.
No difference between G2 and G3 regarding hygiene and habits was observed.
DiscussionInfant care programs are more effective than spontaneous demand, fulfilling the goal of maintaining oral health in the child population. Nonetheless, to prove the success and effectiveness of a program, the results achieved should be clinically evaluated after a certain period.10 Therefore, this project was evaluated, in order to outline the profile of the participant community, to obtain a diagnosis of the results obtained, to identify the major obstacles that interfere with the program, and to seek solutions to achieve the goal of the proposal in primary health.
Several authors11–13 agree with the implementation of preventive programs for infants, as they state that oral health education to those responsible for the children have led to great benefits. Information on oral health care should be provided to mothers during pregnancy, to increase their knowledge about gestational care, its general and oral implications, and to prevent problems that may occur both in the mothers themselves and in their children.14 Pregnant women who receive this information become health promoters in the family, as well as multiplying agents of oral health education. During the gestational period, the emotional system of the woman is more sensitive, making them more receptive; therefore, this is an ideal phase for implanting new ideas and concepts regarding oral health.15 The present study found that children who started participating in the program, and women who have received pertinent information since pregnancy, presented fewer oral diseases than those who never participated in the program.
In the present study, the marital status of the parents was significant, the mothers in G3 had more children and were, on average, ten years younger than G1. According to Moimaz et al.,16 the presence of caries in children and the maternal history of caries were associated with maternal level education, low family economic status, and number of dental appointments. However, the marital status of the parents was not significant (0.695), but the number of children in the house was strongly associated with dental caries (p<0.0001).
Although the G1 and G2 mothers received a card with program enrollment and information about the date of the scheduled return, many abandoned the program (G2). These mothers claimed several reasons that led them to miss the consultations, from lack of time, returning to work, and also forgetting. When they believed that all was well in the first visits to the dentist, they became less vigilant and began to seek health professionals only when a disease manifested, demonstrating the difficulty of accepting new paradigms in promoting and maintaining health.17 The mothers’ profile may interfere in the participation and collaboration in preventive actions, taking considering the socio-economic status,18 the age of the mothers, the number of children, and the presence of a partner.19
A significant association was observed between sucrose consumption and caries prevalence in children.20 It is known that approaching pregnant woman and the baby, even in the first months of life, is extremely important for the introduction of educational and preventive diet, allowing increased parental involvement in breastfeeding, solid and liquid diet after six months of life, and the motivation of infant oral hygiene. Oral diseases related to the type of child's diet should be directed to those responsible.21
Although children are not able to care for their oral hygiene at ages 0–5 years, most G3 mothers allowed their child to perform oral hygiene. In a study where 71% of the mothers reported being aware of the need for supervised daily brushing, only 40% of them helped their children, i.e., when interviewed, they seem to recognize the importance of oral hygiene and presented knowledge in giving satisfactory answers.22 The caries and gingivitis prevalence observed in G2 and G3 indicate that the epidemiological approach with a questionnaire does not always reflect the reality of family habits and attitudes, but rather often shows only the theoretical knowledge of these questions.
In Brazil, an epidemiological study conducted in 2010 showed a 13.6% reduction in malocclusion at the age of 12 years. Even though there is a drop in the prevalence of malocclusions at this age, this occlusal alteration can still be considered a public health problem.23 In the present study, the G1 results of malocclusion was not as high as expected; however, two important factors, genetic inheritance and persistent oral habits, must be taken into account. The genetic factor can be attenuated by avoiding deleterious habits that can stimulate greater deformities and sequelae in these children.24 The open bite was the most prevalent occlusion in the groups of the present study, which, despite knowing the possible genetic/hereditary etiological factors present in the child, may also have been acquired by the non-nutritive habits of pacifier and finger suction.
Even for children of G1 and G2 who were enrolled at up to 6 months of age, some had sucking habits such as bottle and pacifier, the program staff worked to discontinue them. The non-nutritive pacifier sucking habit was the most frequent among all infant habits in the present study. Pacifier sucking is a damaging habit for occlusion and maxillary bones, causing imbalance of the stomatognathic apparatus.25 A major obstacle to the success of preventive programs has been the lack of adherence of families to the guidelines, since in addition to the increasingly early insertion of inappropriate habits that lead to oral diseases, the lack of attendance at consultations can compromise control and encouragement of guidance by the team.26
Dental caries is a multi-factorial disease that involves tooth structure, biofilm dysbiosis adhered to the dental surface, and dietary carbohydrates, which can result in the dissolution of the mineral of the teeth.27 However, the simple removal of microorganisms is not enough to manage the progression of a carious lesion; it is necessary to control the etiological factors. Some strategies have been proven to be effective in reducing the incidence of caries in children, such as counseling for early adoption of oral health-promoting dietary practices, daily brushing with 1000ppm fluoride toothpaste concentration.28 In a study with children aged from 0 to 5 years old, 40% (589/1487) had dental caries; the highest prevalence and severity of caries was observed between the ages of 1 and 2 years.8 Caries affects a higher number of children due to inadequate diet habits (high sugar consumption) and poor oral hygiene.28
The data from the present study demonstrated that the program was efficient in preventing caries, even in those children who did not continue in the prevention program, when compared with those who never participated. According to the WHO oral health classification,7 the deft index in G1 was considered very low; in G2, low; and in G3, average. It demonstrates that the program was effective in controlling caries disease in the first 5 years of age.
The present study demonstrated that children most protected from caries and periodontal disease were those who participated effectively in the program (G1). Oral diseases were not prevented in those who received counseling but left the program (G2). Thus, regular visits reinforce and motivate correct prevention procedures and, consequently, reduce oral diseases.16
According to Lee et al.,29 the first visits of this program focus on oral hygiene in children, dietary counseling, information on oral habits, and prevention of dental injuries, which lead to a reduction dental treatment costs. In this sense, it is necessary that public policies periodically evaluate their health programs, with longitudinal studies, searching for ideal samples and considering them as important indicators for health promotion. This will bring a direct return to the population studied, as it allows a reduction in treatment costs and attendance of the sequelae of the main oral problems that affect children. Such actions reach positive results will be reflexes in improving the quality of life of this community.
The group of children aged 3–5 years who actually attended the Baby's Mouth oral health program presented a lower number of individuals with caries, gingivitis, occlusion, and less harmful habits than those who dropped out or never attended the program. In order to promote children's oral health, parents should follow the guidelines for healthy habits as early as possible.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Alves AP, Rank RC, Vilela JE, Rank MS, Ogawa WN, Molina OF. Efficacy of a public promotion program on children's oral health. J Pediatr (Rio J). 2018;94:518–24.