To investigate the effects of multidisciplinary treatment with and without psychological counseling on obese adolescents’ self-reported quality of life.
MethodsSeventy-six obese adolescents (15.87±1.53 y) were allocated into psychological counseling group (PCG; n=36) or control group (CG; n=40) for 12 weeks. All participants received the same supervised exercise training, nutritional and clinical counseling. Participants in PCG also received psychological counseling. QOL was measured before and after 12 weeks of intervention by Generic Questionnaire for the Evaluation of Quality of Life (SF-36).
ResultsThe dropout rate was higher in GC (22.5%) when compared with PCG (0.0%) (p<0.001). After 12 weeks, participants from PCG presents lower body weight, relative fat mass and higher free fat mass (p<0.001 for all) compared to GC. QOL improved among adolescents from both groups (p<0.05), however, a better QOL was reported from those adolescents enrolled in PCG.
ConclusionThe inclusion of a psychological counseling component in multidisciplinary treatment for adolescent obesity appears to provide benefits observed for improved QOL as compared with treatment without psychological counseling.
Para investigar os efeitos do tratamento multidisciplinar com e sem aconselhamento psicológico voltado à qualidade de vida de adolescentes obesos.
Métodos76 adolescentes obesos (15,87±1,53 ano) foram alocados em um grupo de aconselhamento psicológico e (GAP; n=36) ou grupo de controle (GC; n=40) por 12 semanas. Todos os participantes receberam o mesmo treinamento físico supervisionado e aconselhamento nutricional e clínico. Os participantes no GAP também receberam aconselhamento psicológico. A qualidade de vida foi avaliada antes e depois das 12 semanas de intervenção por meio de um Questionário Genérico de Avaliação da Qualidade de Vida (SF-36).
ResultadosO abandono do tratamento foi maior no GC (22,5%), em comparação ao GAP (0,0%) (p<0,001). Após 12 semanas, os participantes do GAP apresentam menor peso corporal, massa gorda relativa e maior massa livre de gordura (p<0,001 para todos) em comparação ao GC. A qualidade de vida melhorou entre os adolescentes de ambos os grupos (p<0,05); contudo, uma melhor qualidade de vida foi relatada pelos adolescentes incluídos no GAP.
ConclusãoA inclusão de aconselhamento psicológico no tratamento multidisciplinar dos adolescentes obesos parece proporcionar benefícios observados na melhoria da qualidade de vida, em comparação ao tratamento sem aconselhamento psicológico.
Obesity and its associated risk factors have become a major public health concern.1–4 The worldwide prevalence of overweight among children and adolescents (aged 5–17 years) is estimated at 21.4% for girls and 22.9% for boys.5 In Brazil, the prevalence of childhood and adolescent overweight/obesity ranges from 4% to 37% in the different regions of the country.6
Studies show that adolescence obesity is associated with an increased likelihood of depression, anxiety, and eating disorders, which may affect quality of life (QOL).7–9 Studies have demonstrated lower QOL in the physical, psychosocial, emotional, and school functioning domains among obese children and adolescents when compared with their normal weight peers10–12; a multidisciplinary behavioral treatment positively impacts QOL in this population.13 In fact, multidisciplinary behavioral interventions composed by regular physical activity, nutrition, and psychological counseling have been widely acclaimed as the most effective approach for treating obesity.14,15 Moreover, such interventions appear to be more effective with children/adolescents than adults.16
Improvements in weight and body composition are common as a result of a multidisciplinary behavioral treatment for obesity.10 Improvements in psychological well-being and quality of life are common as well.8,9,17–19 Better psychological outcomes may result from changes in weight status and body composition following an increase in participants’ physical activity levels and improvements in eating behavior. These psychological outcomes may also be directly related to a treatment including psychological counseling; however, to the best of the authors’ knowledge, none of the previous researches were conducted to verify the contribution of psychological counseling on QOL in obese adolescents submitted to a multidisciplinary therapy. Psychological counseling targets a broad variety of factors, such as physical, psychosocial, emotional, and school functioning in the context of changing health-related behaviors. As such, psychological counseling per se could be affecting changes in psychological outcomes and adolescents’ QOL beyond the effects observed as a result of changes in weight status or body composition. Thus, the main purpose of this study was to investigate the effects of a multidisciplinary treatment for adolescent obesity with and without psychological counseling on participants’ self-reported quality of life. Secondary outcomes included therapy adherence, and anthropometric and body composition measures.
MethodsSampleStudy participants from both genders were recruited between 2011 and 2012 through advertisements in local media (newspaper, radio, and television) in the urban area of Recife, Brazil. The study was approved by the Ethics Committee of the University of Pernambuco (No. 154/09); parents or guardians signed an informed consent, and participants signed an assent form. The inclusion criteria were: age range 13–18 years; pubertal stage: Tanner 3–420,21; obesity: BMI>95th percentile22; and no pre-existing conditions that would restrict participation in an exercise program. Additional exclusion criteria included pregnancy, presence of hypertension and/or another metabolic condition (such as diabetes type II diabetes and hyperlipidemia), and use of weight loss medications.
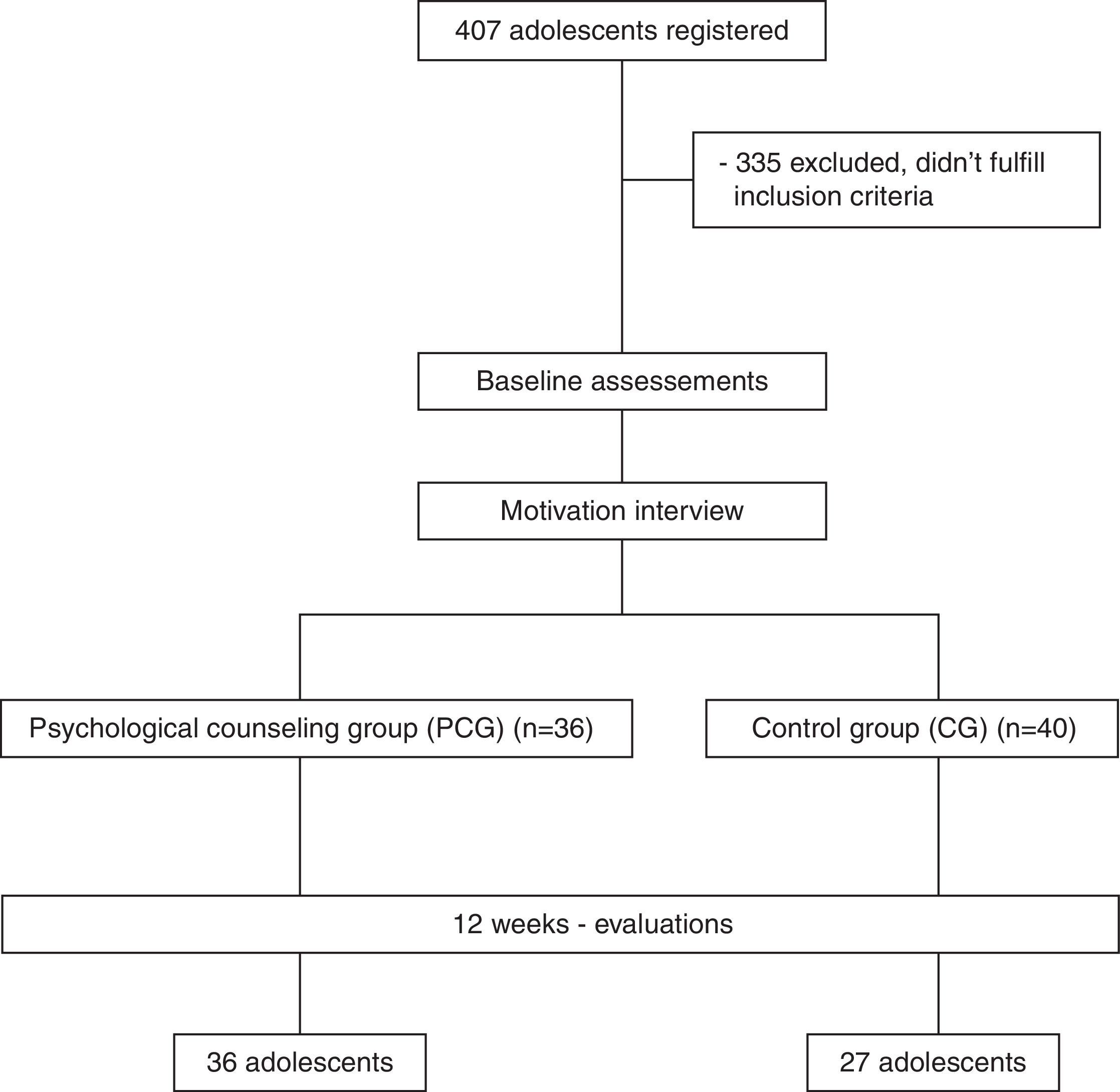
Study protocolA total of 407 adolescents were screened for the study. During the first laboratory visit, potential participants were instructed to self-assess and report their perceived pubertal stage; height and weight was measured. At the second visit, an individual, semi-structured interview containing eight questions was conducted by a psychologist. The interview assessed motives for seeking weight loss treatment and barriers to losing weight. During a third visit, the adolescents underwent a medical screening and resting ECG's were performed. Three hundred thirty-two adolescents did not meet inclusion criteria based on the screening results. A total of 76 obese adolescents (27 boys and 49 girls) who met all inclusion criteria were enrolled in the study. Following baseline testing, participants were allocated into either psychological counseling group (PCG; n=36) or control group (CG; n=40) for 12 weeks of a multidisciplinary intervention that included supervised exercise training sessions, nutritional, and clinical counseling (Fig. 1). Participants enrolled in PCG also received psychological counseling. Fig. 1 presents the flow of participants through the study process.
Multidisciplinary treatmentClinical counselingMedical follow-up was performed once a month by an endocrinologist. This included a physical examination to monitor clinical parameters and to facilitate overall compliance with the study.
Nutrition educationNutritional counseling was conducted by a trained dietitian for one hour each week in small groups (approximately nine participants). Lessons focused on healthy eating behavior, weight loss diets, diet vs. light products, macro and micronutrients function, and nutritional facts. Although no specific prescription for energy intake was recommended, the participants were encouraged to reduce overall calorie intake and to follow a balanced diet as recommended by the Brazilian Ministry of Health. The dietitian was blinded for group allocation.
Supervised aerobic exercise trainingThe adolescents underwent an exercise program administered on a treadmill and supervised by physical educators three times per week (36 sessions total). The intensity of the exercise training (50–60% of the maximum oxygen uptake [VO2max]) was individualized, based on each adolescents’ ventilatory threshold 1 (VT1) obtained from an incremental test on a treadmill with a fixed inclination of 1%.23 All exercise sessions had a set caloric expenditure at 350kcal (1050kcalweek−1) and duration was determined as:
Psychological counselingPsychological counseling was conducted for one hour each week in small groups (approximately nine adolescents) by a clinical psychologist. Along with the psychological motivation for compliance, themes related to body image, eating disorders (symptoms and consequences), the relationship between food and feelings, family and social problems, mood, anxiety, and depression were included.
MeasurementsAll participants underwent the same assessment protocol, at the beginning and at the end of the 12-week treatment. Assessments were performed during a similar time of day to avoid circadian influence. The same evaluator conducted the assessments for both cohorts.
Pubertal maturationEach participant was given drawings of the five stages of breast, genital, and pubic hair development. They were instructed to look at the drawings, read the accompanying descriptions, think about their own physical development and appearance in comparison to the drawings, and pick the one that most closely resembled their own stage of physical maturity.
Anthropometry and body compositionParticipants were weighed barefoot and wearing light clothing on a Filizola scale (model 160/300, Brazil) to the nearest 0.1kg. Stature was measured to nearest 0.5cm using a wall-mounted stadiometer (Filizola scale, model 160/300, Brazil). Body mass index (BMI) was calculated in kgm−2.22 Triceps, subscapular, and medial calf skinfolds were measured in triplicate with a caliper (Lange, CA, USA) with constant pressure (10gmm−2) and resolution of 1mm, on the right hemisphere; the mean value was used. Body composition was estimated by gender-specific equations.24
Generic Questionnaire for the Evaluation of Quality of Life: ‘Medical Outcomes Study SF-36’.
The SF-36, translated into Portuguese and validated for the Brazilian population,25 was used to assess the adolescents’ quality of life (QOL). The instrument is multidimensional. It consists of 36 items, and is intended to generically evaluate QOL. The questionnaire has eight multi-item subscales: physical functioning, role-physical, pain, general health perception, vitality, social functioning, role-emotional, mental health, plus a one-item measure of self-evaluated change in health status over the past year.
Statistical proceduresAll analyses were performed using the software Statistica® 7.0 for Windows®. Normality was verified by the Shapiro–Wilk test and data were presented as means±SD; differences in outcomes between times (baseline and 12 weeks) and groups were analyzed using two-way ANOVA with a Duncan post hoc test. Due to baseline differences between groups for %FM, physical functioning, general health perception, and mean of dimensions of QOL, additional analyses were performed with ANCOVA, where the baseline values were included as covariates. The significance level was set at p<0.05.
ResultsOf the 76 adolescents who participated in the study, 100% from PGC (n=36) and 67.5% from GC (n=27) completed the 12-week of multidisciplinary therapy (p<0.001). At baseline, differences in height and relative fat mass (%FM) were observed between groups (p<0.05 for both).
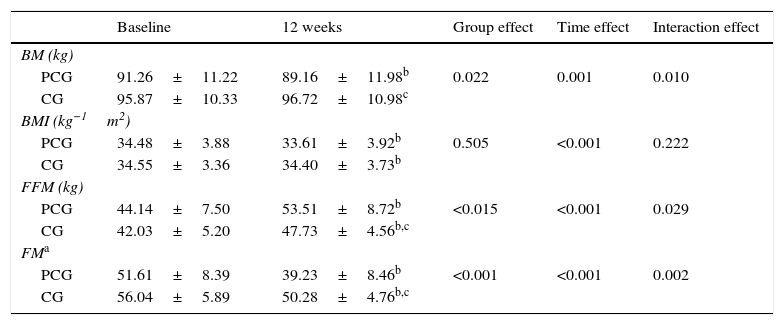
Multidisciplinary therapy was effective in reducing BMI (PCG=2.6% and CG=0.5%; F1,61= 37.05; p<0.001), fat mass (PCG=24% and CG=10.3%; F1,59= 12.78; p<0.001) and to increase FFM (PCG=21.2% and CG=13.5%; F1,60= 55.34; p<0.001). At the end of 12 weeks, participants from PCG presented lower body weight (2.3%, F1,61=7.03; p<0.001), %FM (PCG=13.7%, F1,59=12.78; p<0.001) and higher FFM (PCG=7.7%, F1,60=55.34; p<0.001) when compared GC (Table 1).
Effects of multidisciplinary therapy with and without psychological counseling on anthropometry and body composition in obese adolescents.
| Baseline | 12 weeks | Group effect | Time effect | Interaction effect | |
|---|---|---|---|---|---|
| BM (kg) | |||||
| PCG | 91.26±11.22 | 89.16±11.98b | 0.022 | 0.001 | 0.010 |
| CG | 95.87±10.33 | 96.72±10.98c | |||
| BMI (kg−1m2) | |||||
| PCG | 34.48±3.88 | 33.61±3.92b | 0.505 | <0.001 | 0.222 |
| CG | 34.55±3.36 | 34.40±3.73b | |||
| FFM (kg) | |||||
| PCG | 44.14±7.50 | 53.51±8.72b | <0.015 | <0.001 | 0.029 |
| CG | 42.03±5.20 | 47.73±4.56b,c | |||
| FMa | |||||
| PCG | 51.61±8.39 | 39.23±8.46b | <0.001 | <0.001 | 0.002 |
| CG | 56.04±5.89 | 50.28±4.76b,c | |||
BM, body mass; BMI, body mass index; FFM, fat free mass; %FM, relative fat mass; PCG, psychological counseling group; CG, control group.
p≤0.05.
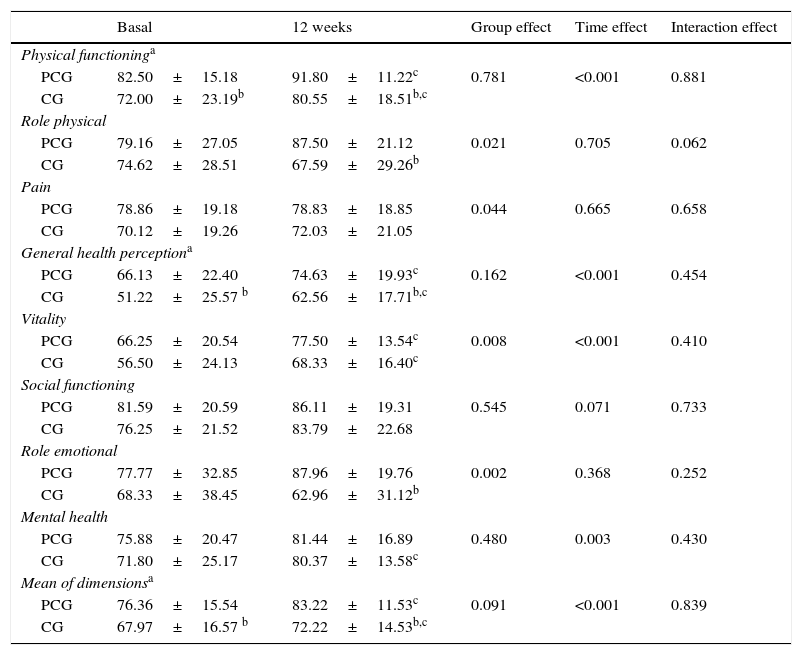
As shown in Table 2, adolescents from both PCG and CG presented an overall improvement on the dimensions of QOL, such as physical functioning, general health perception, vitality, and mean of dimensions. However, high values of self-reported QOL were observed in adolescents enrolled in the PGC.
Effects of multidisciplinary therapy with and without psychological counseling on quality of life in obese adolescents.
| Basal | 12 weeks | Group effect | Time effect | Interaction effect | |
|---|---|---|---|---|---|
| Physical functioninga | |||||
| PCG | 82.50±15.18 | 91.80±11.22c | 0.781 | <0.001 | 0.881 |
| CG | 72.00±23.19b | 80.55±18.51b,c | |||
| Role physical | |||||
| PCG | 79.16±27.05 | 87.50±21.12 | 0.021 | 0.705 | 0.062 |
| CG | 74.62±28.51 | 67.59±29.26b | |||
| Pain | |||||
| PCG | 78.86±19.18 | 78.83±18.85 | 0.044 | 0.665 | 0.658 |
| CG | 70.12±19.26 | 72.03±21.05 | |||
| General health perceptiona | |||||
| PCG | 66.13±22.40 | 74.63±19.93c | 0.162 | <0.001 | 0.454 |
| CG | 51.22±25.57 b | 62.56±17.71b,c | |||
| Vitality | |||||
| PCG | 66.25±20.54 | 77.50±13.54c | 0.008 | <0.001 | 0.410 |
| CG | 56.50±24.13 | 68.33±16.40c | |||
| Social functioning | |||||
| PCG | 81.59±20.59 | 86.11±19.31 | 0.545 | 0.071 | 0.733 |
| CG | 76.25±21.52 | 83.79±22.68 | |||
| Role emotional | |||||
| PCG | 77.77±32.85 | 87.96±19.76 | 0.002 | 0.368 | 0.252 |
| CG | 68.33±38.45 | 62.96±31.12b | |||
| Mental health | |||||
| PCG | 75.88±20.47 | 81.44±16.89 | 0.480 | 0.003 | 0.430 |
| CG | 71.80±25.17 | 80.37±13.58c | |||
| Mean of dimensionsa | |||||
| PCG | 76.36±15.54 | 83.22±11.53c | 0.091 | <0.001 | 0.839 |
| CG | 67.97±16.57 b | 72.22±14.53b,c | |||
PCG, Psychological Counseling Group; CG, Control Group.
p≤0.05.
The data from the present study provided evidence that including psychological counseling in a multidisciplinary treatment is more effective for improving QOL when compared with a treatment that does not include it. Furthermore, psychological counseling may reduce dropout rate.
The discussions of topics such as social acceptance and self-motivation may have encouraged adolescents to further modify their lifestyle, making them more aware of the importance of physical activity and nutrition,10,11,26–29 leading to positive changes on body composition, as observed in the present study, which has been identified as a protective factor against disease development (e.g., hypertension, diabetes, dyslipidemia, and cardiovascular problems)1,2,4,26–29 and as such may also improve the QOL of individuals.30
On average, published studies from programs addressing lifestyle changes report that 50% of patients dropout early or do not complete the treatment. In the current study, psychological counseling appeared to have been important for treatment completion; the reasons for early dropout or treatment completion were not investigated, but future studies should consider the reasons for early dropout and factors contributing to treatment completion.
Although it is known that engaging in regular physical exercise improves QOL,7,9,27 recent studies have suggested that the addition of a behavioral component and a nutritional intervention provides the most changes in QOL among obese individuals.3,10,12,13 In those studies, overweight adolescents reported lower QOL when compared with their normal weight peers. This was observed not only on their total score, but also on the physical, social, psychosocial, and school domains as assessed by the PedsQL 4.0, suggesting that lower QOL affects adolescents on a daily basis.8 Obese individuals are more vulnerable to social injustices (e.g., bullying, discrimination in school, social isolation) and are likely to face prejudice, which may result in poorer QOL.
Behavioral interventions that aim to promote lifestyle changes (increasing physical activity and improving diet quality) are identified as effective for improving QOL, among both adolescents and adults. It is noteworthy that, while comparing the groups of this study, those who received psychological counseling reported a higher QOL on some domains (physical functioning, role physical, general health perception, mean of dimensions). The results from the present study are consistent with other studies that demonstrated that obesity treatment should focus on changes in lifestyle and be conducted by a multidisciplinary team.7–9 However, to date, this was the first study to evaluate the effect of adding psychological counseling in such a multidisciplinary intervention.
A limitation of this study was the use of a generic QOL questionnaire, which may be less sensitive than a specific questionnaire. Another limitation is the fact that, of the participants who started out in CG, only 67.5% completed the intervention, which reduced the generalizability of the conclusions drawn from this study. However, the dropout rate observed in this study was not any higher than what is expected in intervention studies.
In conclusion, multidisciplinary treatment improves quality of life among obese adolescents; the outcomes are improved when psychological counseling is included. Moreover, the inclusion of a psychological counseling component may reduce the dropout ratio commonly observed in the obesity treatment in adolescents.
FundingAll phases of this study were supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ). Data collection was performed at the University of Pernambuco.
Conflicts of interestThe authors declare no conflicts of interest.
All phases of this study were supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico [CNPQ). Data collection was performed by the Grupo de Estudos em Nutrição e Exercício (GENE).
Please cite this article as: Freitas CR, Gunnarsdottir T, Fidelix YL, Tenório TR, Lofrano-Prado MC, Hill JO, et al. Effects of a psychological intervention on the quality of life of obese adolescents under a multidisciplinary treatment. J Pediatr (Rio J). 2017;93:185–91.