The present study aimed to evaluate the effects of hydrotherapy and tactile-kinesthetic stimulation on the birth weight of preterm infants admitted in the Neonatal Intensive Care Unit.
MethodIt was a randomized controlled trial, without blinding, in which 44 preterm infants of both sexes with gestational age between 32 and 34 weeks were included into two groups: hydrotherapy group (n = = 22) and tactile-kinesthetic stimulation group (n = 22). Weight gain was the parameter assessed daily.
ResultsIn the tactile-kinesthetic stimulation group there was a variation in weight gain, but without significant difference (p = 0,43). However, in the hydrotherapy group, it was observed that increased weight gain started from the 2nd day (p < 0,001).
ConclusionsHydrotherapy group presented significantly increased weight after the interventions, indicating that this technique can interfere with weight gain in preterm infants.
The association of preterm infants with low birth weight is the primary mortality and morbidity cause of the neonatal period.1 Due to complications, preterm infants need specialized assistance in a neonatal intensive care unit (NICU), remaining in this environment for a long time.2
This permanency of preterm infants in NICUs favors the exposure to a series of external factors such as noise, illumination, excessive handling, and invasive procedures that can cause pain and discomfort, which could have an impact on neuropsychomotor development.3-6 Therefore, neonatal care has become a significant challenge to decrease the risks of harm to this population.1
Considering the care complexity to preterm infants, techniques and therapeutic measures based on humanized assistance are required, which can reduce the negative impacts of prematurity and prolonged stay in a NICU.7-9 Some stimulations have been used in clinical practice such as tactile-kinesthetic stimulation (TKS) and hydrotherapy.10,11
TKS is a therapy in which touch is used in a systematic approach.12,13 It is a procedure used to stimulate preterm infant's growth and development, based on the forward upgrowth of the tactile system, present from the seven and a half weeks of gestation.14 The therapeutic proposal is given by a tactile, systematic and kinesthetic system.15 Furthermore, TKS is beneficial as it consists of a non-invasive technique, with low cost and safety to preterm infants.14
Hydrotherapy is a therapeutic procedure applied to preterm infants since the '70s in several clinical conditions aiming pain and stress reduction as well as sleep therapy.11 “The use of water as a cure has been described since Greek civilization (around 500 BCE). Medical schools were created close to the stations' bath and thus developing aquatic techniques for use in specific physical treatment. Hippocrates already used hydrotherapy for patients with rheumatic, neurological diseases, as well as immersion treatment for muscle spasms and joint diseases (460-375 BCE)”. Thishis technique is still applied in different people, from when they are babies up until adulthood.16 This study aimed to evaluate the effects of hydrotherapy and TKS on preterm infants' weight (Fig. 1).
Materials and methodsThe research was approved by the Human Research Ethics Committee (CAAE 71355317.1.0000.0096), and it was registered in the Brazilian Registry of Clinical Trials (ReBEC). This study was a randomized controlled clinical trial without blinding, conducted in Rocio's Hospital, at Campo Largo city, in Paraná state. Preterm infants hospitalized at the Neonatal Intensive Care Unit (NICU) were included, with gestational age between 32 and 34 weeks, from 8 to 28 days of life, clinically stables, in use of hydrolyzed milk without addition of fortifier, with full enteral diet via nasogastric or orogastric tube, with a fractionated diet every three hours. The authors excluded preterm infants transferred to intermediate intensive care unit; with food intolerance in the 72 h before the interventions; in use of invasive ventilatory support, non-invasive or oxygen therapy; with neurological impairment or genetic syndromes; small or big for gestational age; gastrointestinal disorders; in fasting; in oral diet or on breastfeeding; child of diabetic mothers; congenital infectious diseases; receiving phototherapy; with central or peripheral venous access.
Some variables could change the research outcome, such as sensory overload, emesis episodes, diarrhea, and signs of food intolerance. In order to control the sensory overload, the whole team was trained and monitored daily by the researcher. Emesis episodes, diarrhea and signs of food intolerance could not be controlled, so the presence of any of these signs resulted in the exclusion of the preterm infant from the study.
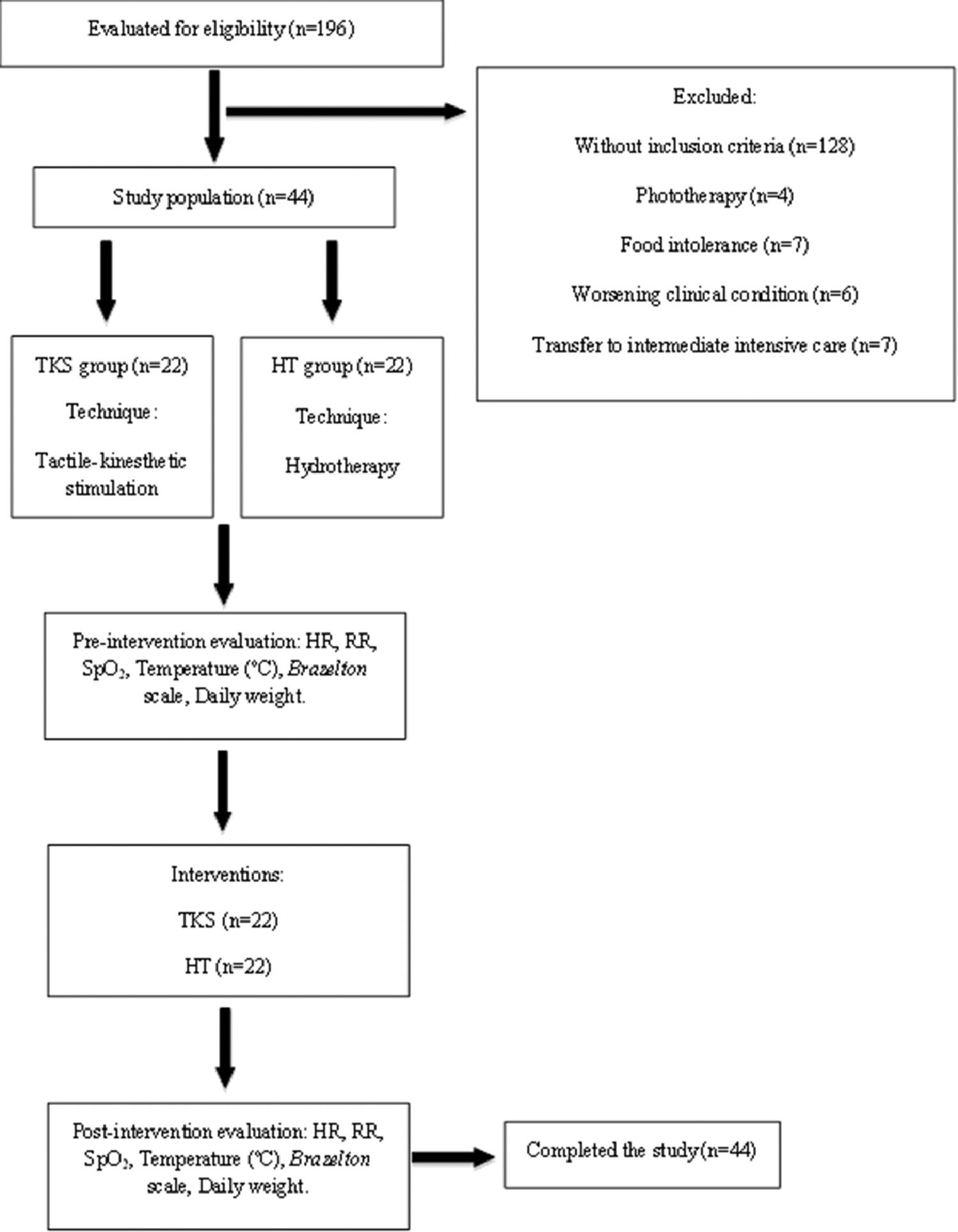
To estimate the minimum sample size, the authors applied the formula for comparing two groups according to paired quantitative variables, considering the significance level of 5%, type II error of 5%, the magnitude of the effect was of 0.01 points, a standard deviation of 0.01 points, with an indication of 22 pairs of participants, granting a 95% test power. It was eligible 196 preterm infants, of which 128 did not attend to the inclusion criteria, and 24 were excluded during the study. Hence, 44 preterm infants composed the study population, which were randomized for allocation on tactile-kinesthetic stimulation group (TKSG) and hydrotherapy group (HG) using a randomization software (http://<www.randomizer.com>). The flowchart of the data collected is presented in Fig. 1.
The interventions were performed on five consecutive days and were performed by the same researcher. The techniques were applied once a day on fifteen minutes sessions to TKSG and eight-minute sessions to HG. At first, the groups were evaluated according to clinical safety and stability, such as heart rate (HR), respiratory rate (RR), peripheral oxygen saturation (SpO2), axillary temperature, and behavioral state based on the Neonatal Assessment Scale adapted from Brazelton17 for sleep and awakeness.
The TKS method consisted of three steps, two of them tactile and one kinesthetic. The first phase was performed on the newborn in a prone position, and tactile stimulation (massage) was performed with moderate pressure with the following order: from the anterior fontanelle to the neck, returning the fontanelle; from neck to shoulder, returning to the neck; from the neck to the sacral region, returning to the neck; from thigh to foot, returning to the thigh (on each leg); from shoulder to hand, returning to the shoulder (on each arm). Each complete slide lasted ten seconds, five seconds to perform the proximal/distal slide (forward), and five seconds to perform the distal/proximal slide (backward), with six sliding movements in each segment, totalizing five minutes. In the second phase (kinesthetic stimulation), the newborn was positioned in the supine position. The technique followed the sequence: a) arm flexion/extension, with five seconds for flexion and five seconds for an extension, six repetitions were performed; b) leg flexion/extension, with five seconds for flexion and five seconds for an extension, performing six repetitions; c) flexion/extension of the legs together, with five seconds for flexion and five seconds for an extension, six repetitions were performed. In the third phase, the first sequence was repeated. Therefore, the three phases of this technique totalized fifteen minutes and were performed without the use of oil or lotion. The original protocol by Field et al.10 consists of applying TKS three times a day for fifteen minutes during each intervention, for five consecutive days with moderate pressure. In the present study, an adaptation of the protocol was made referring to the number of daily interventions. After each intervention, the preterm infants were held in a prone position and re-evaluated after five minutes.
After the evaluation, the patients of the HG were submitted to a hydrotherapy session which took place in a private room with the environment and water temperature control. Then, the patients were covered in a sheet and taken to a heated hydrotherapy room, with a temperature from 28ºC to 30ºC, controlled by a thermometer. The pool was 62 cm long by 43 cm wide and 40 cm deep, with water heated ranging 36 ºC to 37 ºC. The hydrotherapy protocol consisted of light and slow movements of trunk rotation, scapular, and pelvic girdle dissociation, intending to promote tactile and kinesthetic stimulation, flexing posture, and body organization performed by the upthrust force. When finished, the preterm infants were withdrawn from the pool, covered in a towel and taken to the incubator, and then re-evaluated after five minutes.
In both groups, at the end of interventions, the preterm infants were monitored by the researcher for hemodynamic stability and were not handled for the next three hours.
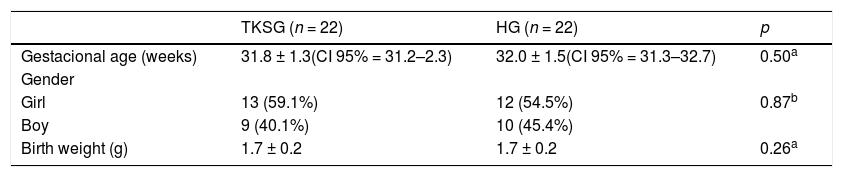
ResultsDuring the study period, a total of 44 premature infants, randomized in two study groups, composed the sample. The Tactile/Kinesthetic Stimulation Group (TKSG) (n = 22) and Hydrotherapy Group (HG) (n = 22). Table 1 shows the distribution of GA, birth weight and gender in both groups. There was homogeneity in the sample characteristics.
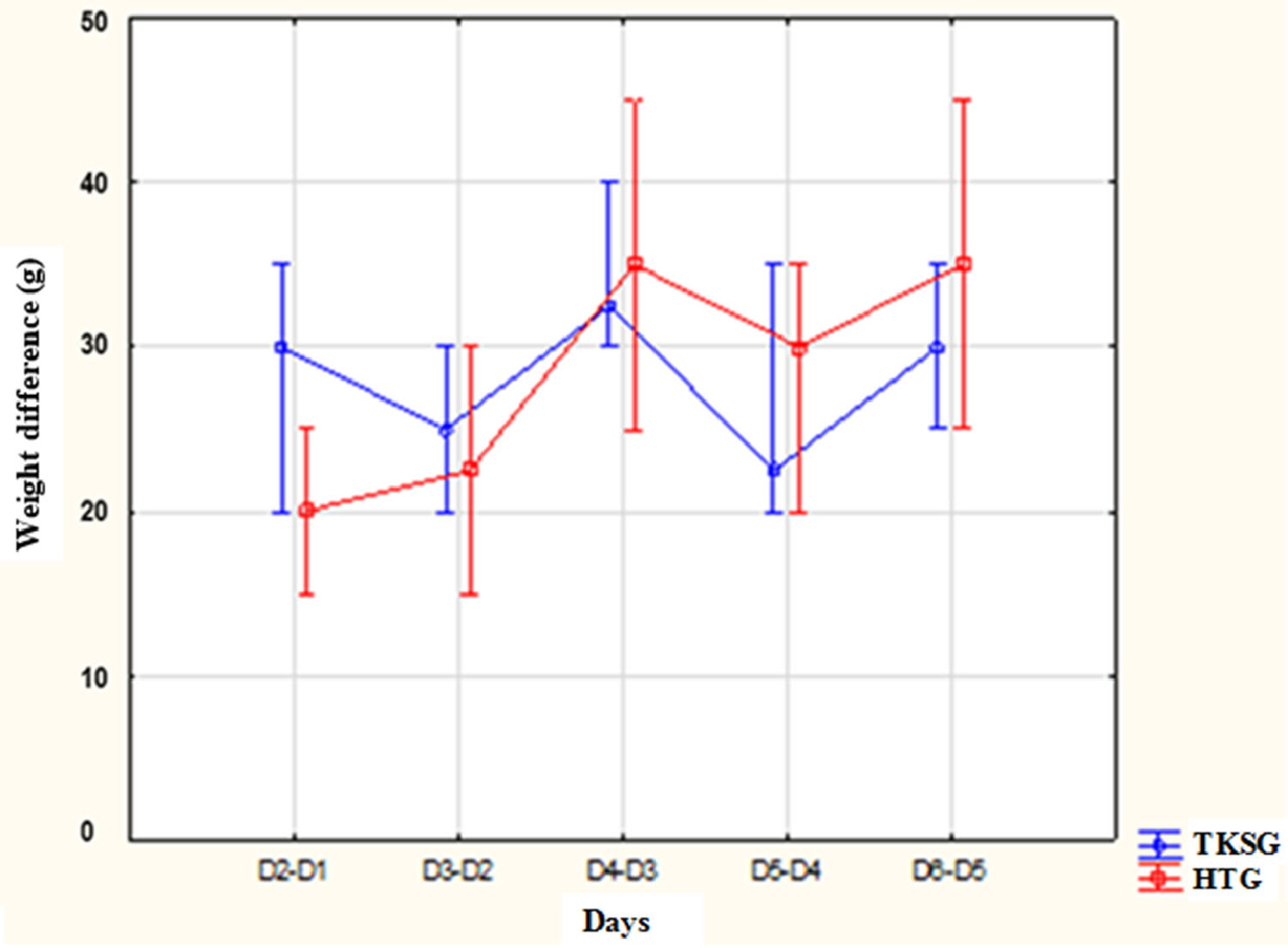
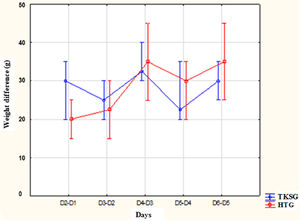
The median of the days of life at the beginner of the intervention was 13.5 (8 - 26) days in the TKSG and 11 (8 - 20) days in the HG (p = 0.10). The evaluation of the weight gain rate, in grams, from the 1st day, the authors found median variation between 25 and 32 g in TKSG and 20 to 35 g in HG. In the TKSG, during the days of evaluation, there was a variation in the weight rate with increase and decrease, but without significant difference (p = 0.43). In HG, the authors observed a higher rate of weight gain after the 2nd day (p < 0.001) (Fig. 2).
Distribution of weight gain rates between the assessment times according to the study groups.
Note: Kruskal–Wallis ANOVA, Mann–Whitney post-hoc test - comparison between groups: D2-D1: p = 0.22; D3-D2: p = 0.41; D4-D3: p = 0.78; D5-D4: p = 0.34; D6-D5 = 0.21 Friedman's ANOVA: GETC: p = 0.43; GH: p < 0.001.
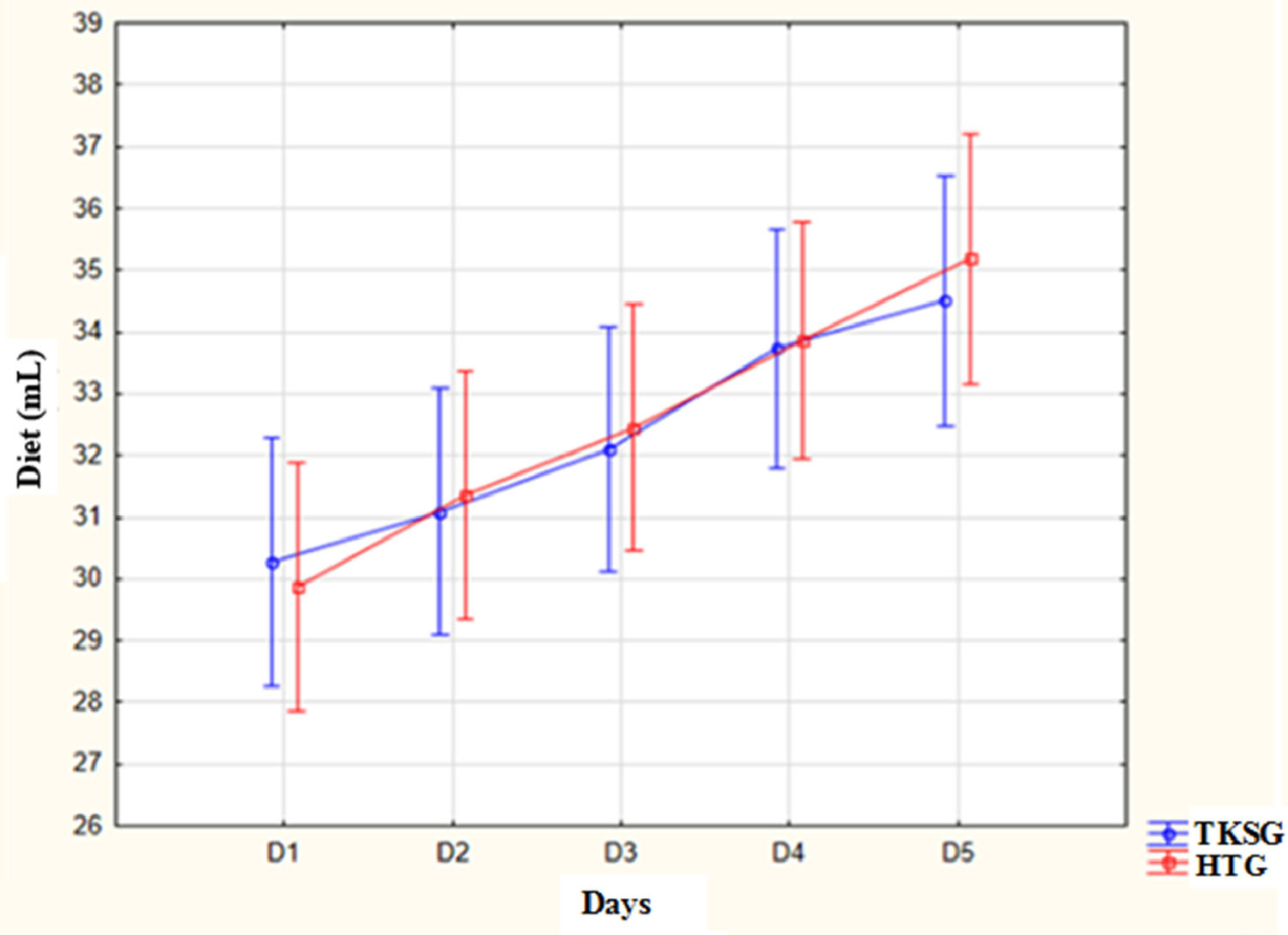
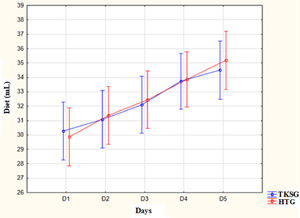
Fig. 3 illustrates the distribution of the daily food intake in milliliters for each administration in both groups. There was no significant difference between the study groups. However, when observing the intragroup values, both in TKSG and in HG, there was a statistical difference between days D1 to D5 intervention (p < 0.001), and the food intake was significantly higher on D5 when compared to D1. This increase refers to the normal daily diet progression expected for GA and weight.
Distribution of mean values of newborns' diets according to study groups.
Note: ANOVA for repeated measures: comparison between groups - At birth: p = 0.89; D1: p = 0.77; D2: p = 0.84; D3: p = 0.79; D4: p = 0.92; D5: p = 0.62. Comparison between measurements in the same group: TKSG - D1 to D6: p < 0.001; HG: D1 to D6: p < 0.001.
In this study, the authors evaluated comparatively the impact of hydrotherapy and TKSG on weight gain in premature infants. As a safety measure, physiological signs such as heart rate, breathing frequency, oxygen saturation, body temperature, and behavioral status (sleep and wakefulness) were evaluated before and after the interventions.
There are differences in the literature about the descriptions and implementations of aquatic therapy techniques. Scientific evidence has been presented, based on techniques such as immersion bath and ofuro in plastic bucket. The immersion bath is characterized by a high level of manipulation with the newborn and its objective is to cleanse the body. In addition, it can cause thermal and cardiorespiratory changes.18,19 While the ofuro in plastic bucket seeks to simulate sensations experienced inside the maternal uterus, providing relaxation, security and body limit to the premature infant.19
The immersion bath and the ofuro in plastic bucket should not be confused with hydrotherapy, which is the application of water with movements for therapeutic purposes. The difference between the techniques of immersion bath and ofuro in plastic bucket with hydrotherapy occurs from its objectives and the execution of the techniques. For hydrotherapy is necessary enough space for wider movements and without established body limits, for all the benefits and effects generated by the technique can be used. However, no studies have been found on how the hydrotherapy technique has been applied.
In the present study, it was possible to observe that the hydrotherapy technique has a positive effect on the weight gain variable in premature infants. However, the mechanism of weight gain related to hydrotherapy is still unknown. According to Silva et al.20 and Tobinaga et al.21 the hydrotherapy age to decrease hormone levels related to stress and consequently to decrease the activation of the sympathetic nervous system, promoting a state of relaxation, characterized by regular breathing, decreased muscle tone, and improved sleep in premature infants.
It is possible to consider that weight gain in HG can be related to maintaining clinical stability and improving the quality of sleep. Leading to a decrease in sensory overload and relaxation, which can be associated with a possible reduction in cortisol levels, and it was not evaluated in this study, but described in previous researches20,21 so there is lower energy expenditure, essential in this stage of development.
The TKS is one of the alternative therapies most used in premature infants.22 The therapeutic proposal occurs in a tactile, systematic and kinesthetic form. The weight gain is one of the results commonly evaluated in premature infants submitted to TKSG.7,23,24 Field et al.23 assessed weight gain in 68 premature infants, with a mean of GA of 30 weeks, which were randomly allocated into two groups. Group 1 received the original protocol from Field et al.10 for 5 consecutive days. While group 2 received the same protocol, but with light pressure. The results showed that group 1, which received the original protocol, gained more weight than those who received the modified protocol (p ≤ 0.02). These findings are different from the results found in this study since the TKSG did not show significant weight gain. Ang et al.7 assessed weight gain in stable premature infants, with GA, a mean of 30 weeks, using the TKS protocol applied by Field et al.,10 from 5 days. The study was a placebo-controlled clinical trial and the sample consisted of 120 premature infants, 58 from the TKSG group and 62 from the control group. The results showed that the experimental group gained more weight daily, when compared to the control group. Another randomized clinical study24 compared weight gain in 60 preterm infants divided into three groups of 20 preterm infants with a mean GA of 30 to 32 weeks, with the first group receiving TKS protocol, the second only tactile stimulation and the third no receiving intervention specifies, following the service routines. The interventions were applied twice a day and as outcome, they concluded that the group who received TKS protocol gained more weight when compared to the other groups.
Mendes and Procianoy25 showed in their randomized study, the application of TKS, carried out by the mother, in 104 premature infants, with gestational age less than 32 weeks, with birth weight between 750 and 1.500g, divided into two groups, one experimental group, and another control. This study concluded that maternal therapeutic massage in premature infants with low birth weight reduced the length of hospital stay and the incidence of delayed sepsis. This same study showed that the weight did not have significant differences between the groups, and these results were similar to the present study, but with the difference, because it was in low birth weight premature infants.
The present study used the TKS technique adapted from Field et al.10 The authors choose to perform it only once a day because they believe that excessive handling could interfere in the results since premature infants are subjected to several interventions during the permanence in the NICU. In addition, the authors suggest a similar intervention protocol between the TKSG and HG, related to the time of application of the technique.
The adaptation of the Field et al.10 protocol used in this study could justify the fact that there was not an increase in weight in the population studied. The data from the present study corroborate the findings by Ho et al.15 who applied the TKS technique only once a day and they did not obtain results on weight gain. Thus, the number of TKS interventions per day can influence weight gain.
It is important to note that premature infants receive varied levels of stress and painful processes inside the NICU environment.26 Due to these factors, premature infants can evolve with discomfort signs, that result in physiological response changes, such as the increase in blood pressure, HR and RR.27 The interventions that can reduce these changes caused by the NICU environment, provide beneficial effects to premature infants.
Field et al.23 and Vignochi et al.11 found that TKS and Hydrotherapy respectively reduce the signs of stress after the interventions due to the relaxation that the techniques promote to the newborn. It is difficult to quantify the degree of relaxation generated in each intervention since the sleep state after both techniques was similar. Thus, it cannot claim that one technique was able to promote greater relaxation than the other. It is important to remember that even when premature infants are in clinical stability conditions, the physiological demands created by the interventions could cause an increase in energy expenditure, leading to weight loss. This effect did not occur, so these results highlight showed the influence of the techniques applied in the maintenance and weight gain in premature infants.
This study had limitations related to the target sample because even stable premature infants can evolve with clinical changes that excluded some babies, with sample loss. In addition, the adaptation of the TKS protocol, the total number of the sample, and the non-blinding of the research were limiting factors.
ConclusionComparing the impact of hydrotherapy and TKS techniques on weight gain, the results showed that HG has a significant increase in weight at the end of the fifth day of intervention, indicating to be a good technique that can interfere with the weight gain in premature infants. Thus, both hydrotherapy and TKS are safe interventions, and their indications can contribute to the improvement of the general condition and the development of premature infants.
The short interventional time was a limitation of the present study, although there is not a consensus related to the total duration of the intervention days, most studies suggest that the TKS performed for 5 consecutive days is sufficient to increase significantly the weight gain in preterm infants. Another limitation was the hydrotherapy technique. There is not much information in the literature, most articles are about the use of the ofuro in plastic bucket technique. The studies using the ofuro in plastic bucket did not have as the main objective the gain weight, so the authors decided to use the same number of days already used in the TKS, 5 days. The authors suggest that other studies apply this technique and follow the weight gain for more time.
The authors thank the Fundação Araucária, Secretaria de Estado da Ciência, Tecnologia e Ensino Superior do Paraná (SETI), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Universidade Federal do Paraná, Pontifícia Universidade Católica do Paraná and the Hospital do Rocio directy for allowing the study to be performed on the NICU's premises.