To evaluate the demographics, genotype, and clinical presentation of pediatric patients presenting with distal intestinal obstruction syndrome (DIOS), and factors associated with DIOS recurrence.
MethodsCase series of ten patients (median age 13.2 years), followed-up in a reference center, retrospectively assessed. Data analyzed included age, gender, cystic fibrosis genotype, meconium ileus at birth, hydration status, pulmonary exacerbation, Pseudomonas aeruginosa colonization, pancreatic insufficiency (PI), body mass index (BMI) at the episodes, clinical manifestations of DIOS, imaging studies performed, acute management of DIOS, maintenance therapy, and recurrence on follow-up.
ResultsAll patients had two positive sweat chloride tests, and nine of ten also had genotype study. The most common genotype identified was homozygosis for the delta F508 mutation. In seven cases, a previous history of meconium ileus was reported. All patients had pancreatic insufficiency. Diagnosis of DIOS was based on clinical and imaging findings. Of the total number of episodes, 85% were successfully managed with oral osmotic laxatives and/or rectal therapy (glycerin enema or saline irrigation). Recurrence was observed in five of ten patients.
ConclusionIn this first report of pediatric DIOS in South America, the presence of two risk factors for DIOS occurrence was universal: pancreatic insufficiency and severe genotype. Medical history of meconium ileus at birth was present in most patients, as well as in the subgroup with DIOS recurrence. The diagnosis relied mainly on the clinical presentation and on abdominal imaging. The practices in the management of episodes varied, likely reflecting changes in the management of this syndrome throughout time.
Avaliar os dados demográficos, o genótipo e o quadro clínico de pacientes pediátricos que apresentam síndrome da obstrução intestinal distal (DIOS) e os fatores associados à recidiva da DIOS.
MétodosCasuística de 10 pacientes (média de 13,2 anos) monitorados em um centro de referência e avaliados de forma retroativa. Os dados analisados incluíram idade, sexo, genótipo da fibrose cística, íleo meconial no nascimento, estado de hidratação, exacerbação pulmonar, colonização por Pseudomonas aeruginosa, insuficiência pancreática (IP), IMC nos episódios, manifestações clínicas da DIOS, estudos de diagnóstico por imagem realizados, manejo agudo da DIOS, terapia de manutenção e recidiva no acompanhamento.
ResultadosTodos os pacientes apresentaram dois exames de cloreto no suor positivos e 09/10 também apresentaram estudo do genótipo. O genótipo mais comum identificado foi a homozigose da mutação delta F508. Em sete casos foi mencionado um histórico de íleo meconial. Todos os pacientes apresentaram insuficiência pancreática. O diagnóstico da DIOS teve como base achados clínicos e de imagem; 85% do número total de episódios foram tratados com sucesso com laxantes osmóticos orais e/ou terapia retal (enema de glicerina ou irrigação salina). A recidiva foi observada em 5 de 10 pacientes.
ConclusãoNeste primeiro relatório da DIOS pediátrica na América do Sul, a presença de dois fatores de risco na ocorrência da DIOS foi universal: insuficiência pancreática e genótipo associado a doença grave. O histórico de íleo meconial no nascimento esteve presente na maioria dos pacientes, bem como no subgrupo com recidiva da DIOS. O diagnóstico dependeu principalmente do quadro clínico e do diagnóstico por imagem abdominal. As práticas de manejo de episódios variaram, provavelmente refletiram as mudanças no tratamento dessa síndrome ao longo do tempo.
Cystic fibrosis (CF) is a monogenic autosomal recessive disease that presents with wide phenotypic variability – around 300 pathogenic cystic fibrosis transmembrane regulator (CFTR) variants cause the disease – and it is the most prevalent fatal genetic disease in humans. The absence of functional CFTRs affects multiple organ systems, with the highest morbidity and mortality in CF being secondary to respiratory diseases – as CF is among the main causes of chronic obstructive pulmonary diseases in children.1 With the increasing average life expectancy of CF patients, gastrointestinal manifestations are becoming more prevalent, as this is the second organ system mainly affected in CF.2 Given the burden and the complexity of this disease, early diagnosis and specialized care are mandatory. In Brazil, the neonatal screening program includes CF with broad national coverage, and the majority of states have referral centers for the follow-up of these patients.3
Distal intestinal obstruction syndrome (DIOS) is a gastrointestinal complication that is specific to CF. It was first described as syndrome of post-neonatal distal small bowel obstruction caused by meconium-like stool plugs, in 1945.4 It is characterized by accumulation of viscous fecal material, combined with sticky mucous secretions typically located in the distal ileum and cecum, which may adhere to the intestinal wall, causing subtotal or total obstruction. Since its initial description as “meconium-ileus equivalent,” not only has the denomination changed to DIOS,5 but also its definition has been reviewed6 – and thus the epidemiology, recurrence, and burden of this complication have been better described and understood.7
In 2010, the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) CF/Pancreas Working Group tackled the issue of the various definitions being used for DIOS by publishing a consensus document that defined DIOS as an acute complete or incomplete fecal ileocecal obstruction, clearly differentiated from constipation – defined as gradual fecal impaction in the colon. Complete DIOS (C-DIOS) was defined by the triad of complete intestinal obstruction (evidenced clinically by bilious vomiting and/or radiographically by fluid levels in the small intestine), presence of an ileocecal fecal mass, and abdominal pain or distension; whereas incomplete/impending DIOS (I-DIOS) was characterized by the presence of a short history of abdominal pain and/or distension (days) in association with an ileocecal fecal mass, in the absence of signs of complete intestinal obstruction.6 Initial reports of DIOS incidence found it to be frequent in adults and teenagers, but after the revision of diagnostic criteria, a recent international and prospective study reported a similar incidence in adults and children with CF.7
The present study reviewed patients with CF who were diagnosed with DIOS over a 16-year period in a Brazilian CF reference center. Evaluating demographics, genotype, clinical presentation, acute phase, and maintenance therapy, this study aims to characterize the clinical presentation, management, and factors associated with the occurrence and recurrence of this CF complication.
MethodsA retrospective case series study was conducted at a tertiary hospital and reference center for CF. The study was approved by the Research Ethics Committee of the Hospital. All the data gathered for this study was obtained from medical records, filed at the Medical Archive Service.
For the purposes of this study, it was decided to include only patients who had been admitted for DIOS management, since the patients managed in an outpatient basis could not always be identified and could lack a meticulous description of diagnosis, management, and resolution, which would impair the study analysis.
At this center, 250 patients per year are seen in a pediatric multidisciplinary outpatient CF clinic. Initially, 16 patients who had been admitted with the diagnosis of DIOS were identified, four patients were excluded from the present analysis since they did not fulfill diagnostic criteria or presented alternative diagnoses, and two patients were older than 20 years at diagnosis of the first DIOS episode. Therefore, ten children and teenagers up to 20 years old, admitted from May 2001 to March 2017, were included in this series.
Two investigators (NSS and LHPM) collected data from the medical records, including the following: age, gender, date of birth, history of meconium ileus at birth, date of occurrence of DIOS episode(s), genotype, patient hydration status at events, presence or absence of pulmonary exacerbation during the events, Pseudomonas aeruginosa colonization, diagnosis of pancreatic insufficiency (PI) and other CF-related morbidities, lipase dosage, body mass index (BMI), clinical symptoms of DIOS, test(s) performed to the diagnosis, acute management and maintenance therapy, recurrence, and total number of episodes in the study period.
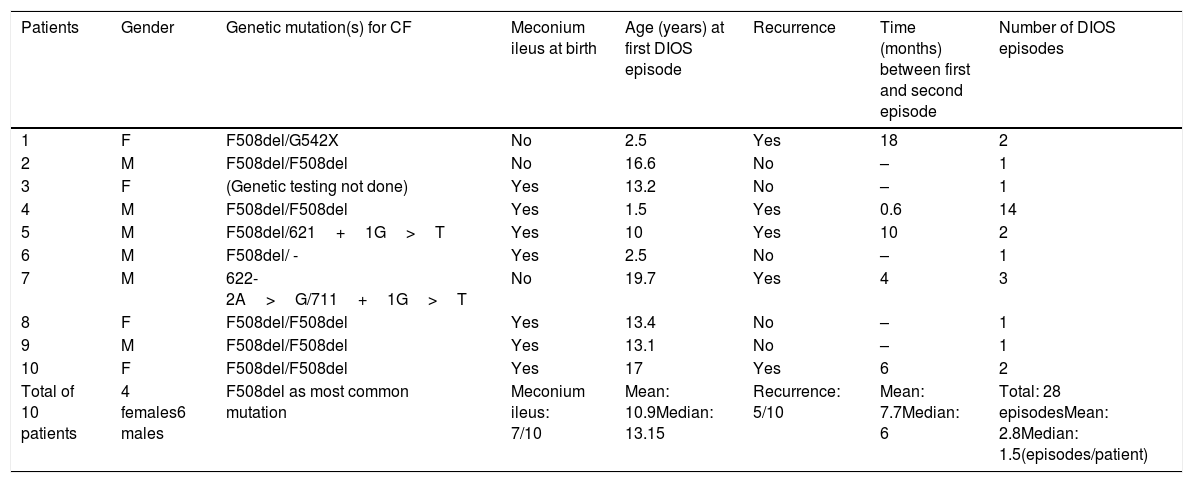
ResultsThe patients’ baseline characteristics are summarized in Table 1. Age at the first episode varied from 2.5 to 19.7 years (median: 13.2). All patients had two abnormal sweat chloride tests, assuring CF diagnosis. Genetic testing was not available in one out of the ten patients. Eight out of nine patients tested had two disease-causing mutations, with five being homozygous for delF508. DIOS recurrence was observed in five patients, three male. 28 DIOS episodes were recorded, with the total number of episodes per patient ranging from one (five out of ten patients) to 14. In patients with recurrent DIOS, the time between the first and second episodes ranged from 18 days to 18 months. Meconium ileus was present at birth in seven out of ten patients, and, proportionally, in three out of five of those who presented DIOS recurrence.
Baseline characteristics of patients’ gender, genotype, recurrence, and total number of episodes.
| Patients | Gender | Genetic mutation(s) for CF | Meconium ileus at birth | Age (years) at first DIOS episode | Recurrence | Time (months) between first and second episode | Number of DIOS episodes |
|---|---|---|---|---|---|---|---|
| 1 | F | F508del/G542X | No | 2.5 | Yes | 18 | 2 |
| 2 | M | F508del/F508del | No | 16.6 | No | – | 1 |
| 3 | F | (Genetic testing not done) | Yes | 13.2 | No | – | 1 |
| 4 | M | F508del/F508del | Yes | 1.5 | Yes | 0.6 | 14 |
| 5 | M | F508del/621+1G>T | Yes | 10 | Yes | 10 | 2 |
| 6 | M | F508del/ - | Yes | 2.5 | No | – | 1 |
| 7 | M | 622-2A>G/711+1G>T | No | 19.7 | Yes | 4 | 3 |
| 8 | F | F508del/F508del | Yes | 13.4 | No | – | 1 |
| 9 | M | F508del/F508del | Yes | 13.1 | No | – | 1 |
| 10 | F | F508del/F508del | Yes | 17 | Yes | 6 | 2 |
| Total of 10 patients | 4 females6 males | F508del as most common mutation | Meconium ileus: 7/10 | Mean: 10.9Median: 13.15 | Recurrence: 5/10 | Mean: 7.7Median: 6 | Total: 28 episodesMean: 2.8Median: 1.5(episodes/patient) |
CF, cystic fibrosis; DIOS, distal intestinal obstruction syndrome.
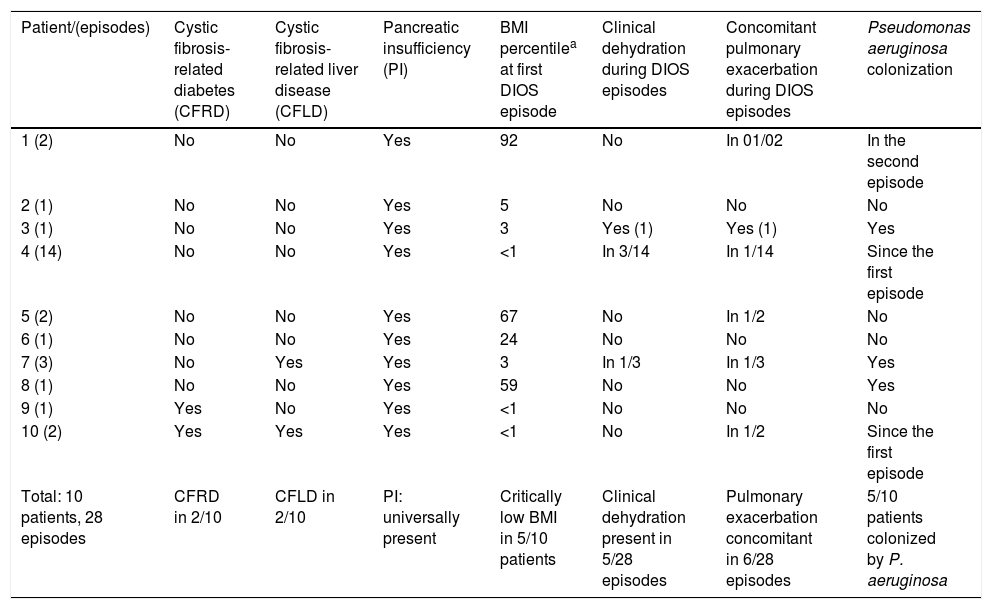
CF-related diabetes and CF-related liver disease were observed in two of the ten patients. PI was universally present, confirmed by fecal elastase <100μg/g – furthermore, all patients were on enzymatic supplementation since the first year of life. At the time of DIOS episode, lipase dosage ranged from 4,000 to 17,900 units/kg/day; median: 7,200units/kg/day. BMI percentile at the first DIOS episode ranged from <1 to 92, with five out of ten patients presenting a percentile that was equal or below 3. Dehydration was reported in five out of 28 episodes. There was concomitant pulmonary exacerbation in six out of 28 episodes. Half of the patients were colonized by Pseudomonas aeruginosa. Environmental and patient-related factors at the time of DIOS episodes are outlined in Table 2.
Environmental and patient-related factor at the time of DIOS episodes.
| Patient/(episodes) | Cystic fibrosis-related diabetes (CFRD) | Cystic fibrosis-related liver disease (CFLD) | Pancreatic insufficiency (PI) | BMI percentilea at first DIOS episode | Clinical dehydration during DIOS episodes | Concomitant pulmonary exacerbation during DIOS episodes | Pseudomonas aeruginosa colonization |
|---|---|---|---|---|---|---|---|
| 1 (2) | No | No | Yes | 92 | No | In 01/02 | In the second episode |
| 2 (1) | No | No | Yes | 5 | No | No | No |
| 3 (1) | No | No | Yes | 3 | Yes (1) | Yes (1) | Yes |
| 4 (14) | No | No | Yes | <1 | In 3/14 | In 1/14 | Since the first episode |
| 5 (2) | No | No | Yes | 67 | No | In 1/2 | No |
| 6 (1) | No | No | Yes | 24 | No | No | No |
| 7 (3) | No | Yes | Yes | 3 | In 1/3 | In 1/3 | Yes |
| 8 (1) | No | No | Yes | 59 | No | No | Yes |
| 9 (1) | Yes | No | Yes | <1 | No | No | No |
| 10 (2) | Yes | Yes | Yes | <1 | No | In 1/2 | Since the first episode |
| Total: 10 patients, 28 episodes | CFRD in 2/10 | CFLD in 2/10 | PI: universally present | Critically low BMI in 5/10 patients | Clinical dehydration present in 5/28 episodes | Pulmonary exacerbation concomitant in 6/28 episodes | 5/10 patients colonized by P. aeruginosa |
BMI, body mass index; DIOS, distal intestinal obstruction syndrome.
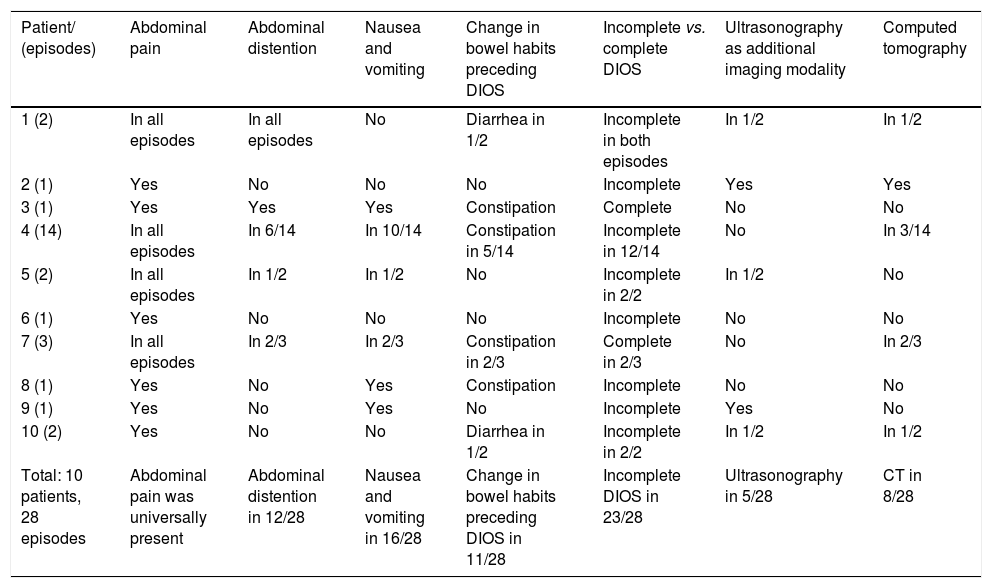
The diagnosis of DIOS was based on clinical and imaging findings. Abdominal pain, recent weight loss, vomiting, and decreased number of bowel movements were the most common clinical manifestations reported. In many cases, however, no change in bowel habits was observed. The obstruction was complete in five out of 28 episodes. All patients had at least an abdominal radiography performed in all episodes of DIOS, whereas ultrasound and computed tomography (CT) were performed only in selected cases. The clinical characteristics and the imaging work-up are summarized in Table 3.
Clinical manifestations in the DIOS episodes and imaging tests.
| Patient/ (episodes) | Abdominal pain | Abdominal distention | Nausea and vomiting | Change in bowel habits preceding DIOS | Incomplete vs. complete DIOS | Ultrasonography as additional imaging modality | Computed tomography |
|---|---|---|---|---|---|---|---|
| 1 (2) | In all episodes | In all episodes | No | Diarrhea in 1/2 | Incomplete in both episodes | In 1/2 | In 1/2 |
| 2 (1) | Yes | No | No | No | Incomplete | Yes | Yes |
| 3 (1) | Yes | Yes | Yes | Constipation | Complete | No | No |
| 4 (14) | In all episodes | In 6/14 | In 10/14 | Constipation in 5/14 | Incomplete in 12/14 | No | In 3/14 |
| 5 (2) | In all episodes | In 1/2 | In 1/2 | No | Incomplete in 2/2 | In 1/2 | No |
| 6 (1) | Yes | No | No | No | Incomplete | No | No |
| 7 (3) | In all episodes | In 2/3 | In 2/3 | Constipation in 2/3 | Complete in 2/3 | No | In 2/3 |
| 8 (1) | Yes | No | Yes | Constipation | Incomplete | No | No |
| 9 (1) | Yes | No | Yes | No | Incomplete | Yes | No |
| 10 (2) | Yes | No | No | Diarrhea in 1/2 | Incomplete in 2/2 | In 1/2 | In 1/2 |
| Total: 10 patients, 28 episodes | Abdominal pain was universally present | Abdominal distention in 12/28 | Nausea and vomiting in 16/28 | Change in bowel habits preceding DIOS in 11/28 | Incomplete DIOS in 23/28 | Ultrasonography in 5/28 | CT in 8/28 |
CT, computed tomography; DIOS, distal intestinal obstruction syndrome.
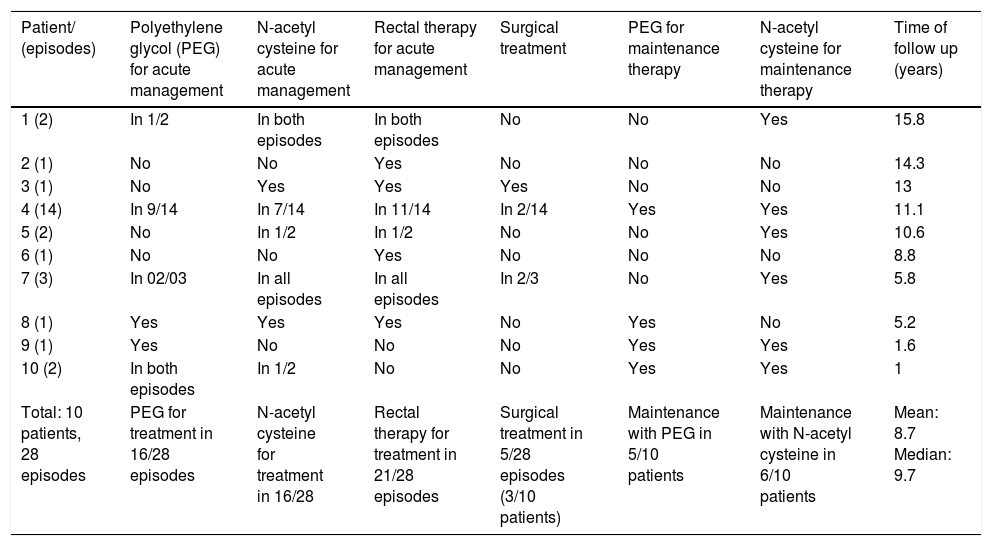
Of the DIOS episodes, 82% were treated clinically, sparing surgical approach. Polyethylene glycol (PEG) and/or N-acetyl cysteine delivered orally or through a nasogastric tube were administered in 16 out of 28 episodes, and rectal enema with glycerin or normal saline irrigation was performed in 21 out of 27 events. One patient presented DIOS complicated by intussusception that failed to respond to medical management and was managed endoscopically.8 Among the ten patients followed, three received maintenance therapy with both oral PEG and N-acetyl cysteine, three with N-acetyl cysteine only, and one with PEG only. The median follow-up time was 9.7 years, with a mean of 8.1 years. Data on acute management, maintenance therapy, and follow-up time are summarized in Table 4.
Treatment modalities in acute management, maintenance, and follow-up time after the first event.
| Patient/ (episodes) | Polyethylene glycol (PEG) for acute management | N-acetyl cysteine for acute management | Rectal therapy for acute management | Surgical treatment | PEG for maintenance therapy | N-acetyl cysteine for maintenance therapy | Time of follow up (years) |
|---|---|---|---|---|---|---|---|
| 1 (2) | In 1/2 | In both episodes | In both episodes | No | No | Yes | 15.8 |
| 2 (1) | No | No | Yes | No | No | No | 14.3 |
| 3 (1) | No | Yes | Yes | Yes | No | No | 13 |
| 4 (14) | In 9/14 | In 7/14 | In 11/14 | In 2/14 | Yes | Yes | 11.1 |
| 5 (2) | No | In 1/2 | In 1/2 | No | No | Yes | 10.6 |
| 6 (1) | No | No | Yes | No | No | No | 8.8 |
| 7 (3) | In 02/03 | In all episodes | In all episodes | In 2/3 | No | Yes | 5.8 |
| 8 (1) | Yes | Yes | Yes | No | Yes | No | 5.2 |
| 9 (1) | Yes | No | No | No | Yes | Yes | 1.6 |
| 10 (2) | In both episodes | In 1/2 | No | No | Yes | Yes | 1 |
| Total: 10 patients, 28 episodes | PEG for treatment in 16/28 episodes | N-acetyl cysteine for treatment in 16/28 | Rectal therapy for treatment in 21/28 episodes | Surgical treatment in 5/28 episodes (3/10 patients) | Maintenance with PEG in 5/10 patients | Maintenance with N-acetyl cysteine in 6/10 patients | Mean: 8.7 Median: 9.7 |
To the best of the authors’ knowledge, this is the first DIOS case series reported in Brazil and South America. Even in international and multi-centric studies, the number of reported pediatric cases of DIOS is relatively limited, with the DIOS incidence varying from 2.3 to 11.2 episodes/1,000 patient-years7 – so the number of pediatric cases described in this study is relevant. In the present series, there was a predominance of severe CFTR genotypes, which is in agreement with the observation that the occurrence of DIOS is related to the severity of the CF genotype.6,9 Among a number of factors identified as predisposing to DIOS, past medical history of meconium ileus at birth has been consistently reported and also associated with recurrence,7 and this was observed in the majority patients in this series (seven out of ten), as well as in a significant share of those who had recurrence of DIOS (three out of five), and also among patients who required surgical treatment (two out of three). Other factors reported as associated with the occurrence of DIOS – such as dehydration, hot seasons/weather, CF pulmonary exacerbation,10 colonization by Pseudomonas aeruginosa, diabetes mellitus related to cystic fibrosis,7,11 CF-related liver disease, and post-operatory lung transplant12,13 – were not consistently present in this series.
As reported in the pertinent literature, in the vast majority of episodes, the diagnosis was based on the combination of history, clinical examination, and simple abdominal radiography. Other imaging modalities, which can aid in differential diagnosis, were performed only in selected cases. In regards to the medical management of DIOS, there have been changes in the preferred therapies over time, and there is still great variability in practice among different centers, with no high quality evidence to guide the practice, which was reflected in the present series. Currently, the preferred first line therapy for the management of incomplete DIOS is the use of oral osmotic laxatives,7 mainly polyethylene glycol (PEG) – which is used for this purpose in doses that are much higher than standard dosing −2g/kg, up to a maximum 80–100g/day, or iso-osmotic PEG solution, 20–40mL/kg/h, up to a maximum of 1L/h, for a period of up to 8h.14 In the present case series, rectal therapy was more often used – which somewhat reflects the practices regarding the timing of the events, while the use of PEG was preferred in later patients/episodes. Clinical treatment was successful in 82% of the episodes, so the need of surgical management for complete DIOS was higher than the 8% reported in the first multi-centric prospective DIOS cohort (European).7
The use of maintenance therapy to prevent recurrence is recommended based on the fact that the occurrence of a DIOS is associated with a ten-fold higher risk of a second event.6 In this regard, the practice of this center resembled what is reported by European centers: the majority of patients received some form of long-term maintenance therapy – PEG and/or N-acetyl cysteine.
This study has a few limitations. Primarily, the data were obtained retrospectively, reflecting the practice of almost two decades – so the review of the treatments given through the years was likely affected by different practices/tendencies throughout time, and even the ability to promptly recognize DIOS has probably changed over this time. Nonetheless, despite the above mentioned limitations, the authors believe that these results constitute a very important first step in the still incipient discussion on DIOS in South America, as the current literature mainly reflects North American and European experiences and practices. Secondly, this case series may not resemble patients recruited from general registries, which may include milder phenotypes. And finally, when including CF-related morbidities, it is important to keep in mind that the definition and recognition of these have also changed over the past decades. A prospective study would be the best approach to evaluate DIOS-associated factors, as well as different treatment strategies. Finally, it must be acknowledged that part of the patients being followed at this center are sometimes either managed as outpatients or admitted at other institutions to treat acute conditions, but given that 85% to 96% of patients with DIOS are hospitalized,7 and considering the complexity of the cases reported, the authors do believe that the majority of the DIOS episodes that required hospitalization were captured.
In conclusion, this is first DIOS case series in South America, in which a wide spectrum of DIOS presentations have been reported. Two known risk factors were relevant to these DIOS cases: pancreatic insufficiency and genotype associated with severe disease. Past medical history of meconium ileus at birth as a risk factor for occurrence, recurrence, or need for surgical treatment remains controversial, and it was present in the majority of cases, as well as in the subgroup of patients who had recurrence of DIOS. The early recognition and medical management of DIOS is important to avoid poor outcomes, such as complications or need for surgical treatment. In Brazil and South America, better knowledge of DIOS-associated epidemiology is required, since the previous studies on this syndrome are mainly North American and European, and environmental conditions, such as warmer climate conditions, may influence the incidence and prevalence of this severe CF complication.15 Local prospective studies in which DIOS diagnosis can be systematically assessed and performed according to the ESPGHAN guidelines14 are needed, as early recognition of DIOS by pediatricians involved in the care of CF patients is fundamental.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Sandy NS, Massabki LH, Gonçalves AC, Ribeiro AF, Ribeiro JD, Servidoni MF, et al. Distal intestinal obstruction syndrome: a diagnostic and therapeutic challenge in cystic fibrosis. J Pediatr (Rio J). 2020;96:732–40.
Study conducted at Universidade Estadual de Campinas (Unicamp), Faculdade de Ciências Médicas, Campinas, SP, Brazil.