To analyze the scientific literature on dietary changes in preterm children during the first years of life.
Data sourceThe PubMed database was used for article selection. The texts were analyzed according to their objectives, research design, and research group characteristics. The following were selected to comprise the criteria: (1) publications in the period from 1996 to 2014; (2) participation of infants and children from birth to 10 years of age; (3) development of oral motor skills necessary for feeding; (4) development of the feeding process; and (5) feeding difficulties during childhood.
Summary of the findingsThere were 282 studies identified, of which 17 were used in the review, and five more articles were identified through the reference list of selected articles, totaling 22 references.
ConclusionVery low birth weight preterm newborns are more likely to have feeding problems in early postnatal stages and during childhood when compared with full-term infants. Monitoring the feeding of these infants after hospital discharge is strictly recommended in an early intervention program aiming at better development of feeding skills.
Analisar a literatura científica sobre alterações alimentares em crianças prematuras durante os primeiros anos de vida.
Fonte dos dadosA base de dados do Pubmed foi a percursora para a seleção dos artigos. Os textos foram analisados quanto aos seus objetivos; desenhos da pesquisa; características do grupo pesquisa e foram selecionados os seguintes temas para compor os critérios: (1) publicações no período de 1996 a 2014; (2) participação de bebês e crianças, do nascimento até os 10 anos de idade; (3) desenvolvimento das habilidades motoras orais necessárias para a alimentação; (4) desenvolvimento do processo de alimentação e (5) dificuldades alimentares durante a infância.
Síntese dos dadosforam identificados 282 estudos, destes 17 foram utilizados e 5 artigos foram identificados por meio da lista de referência bibliográfica dos artigos selecionados, totalizando 22 referências bibliográficas.
ConclusãoA revisão permitiu concluir que recém-nascidos pré-termo muito baixo peso (RNPTMBP) são mais propensos a apresentarem problemas de alimentação nos estágios iniciais pós-natal e durante a infância quando comparados com crianças a termo. O monitoramento da alimentação após a alta hospitalar é estritamente recomendado em um programa de intervenção precoce com vistas ao melhor desenvolvimento das habilidades alimentares.
Prematurity is considered a risk factor, because the infant's anatomical and physiological immaturity predisposes to a number of adaptation and evolution difficulties in post-natal life.1 The reduction of neonatal morbidity and mortality and, consequently, the significant increase in survival of very low birth weight (VLBW) preterm newborns, i.e., those with gestational age (GA) <37 weeks and birth weight (BW) <1500g,2–5 has led many authors to identify this group of children as prone to develop important dietary-related problems.
The initial difficulties with sucking and swallowing patterns in VLBW preterm newborns during the hospitalization period are described in the literature6–9 as immature oral reflexes, reduced sucking effort, small number of sucks due to pauses, incoordination of sucking, swallowing and breathing, choking, and difficulty accepting full volume by oral route (OR).10 The morbidities associated with prematurity, such as lower GA at birth, presence of clinical instability of the breathing pattern, prolonged intubation time, and gastrointestinal system immaturity11 make these infants unable to initially receive oral feeding exclusively. Thus, the use of alternative feeding routes, through a nasogastric (NG) or orogastric tube, becomes strictly necessary.12,13
Studies have indicated that feeding problems can persist in these children after hospital discharge, and this can have consequences in the long term.12–16 Understanding the development of the feeding process in this population, as well as identifying the factors that may contribute to the onset of eating disorders in childhood are essential to determine, in this group of children, which would be more likely to develop problems, and to identify which stages of feeding development can be altered.17,18 This literature review aimed to assess international and Brazilian articles on feeding development of preterm children and feeding problems during the first years of life.
MethodsData sourceArticles were selected from the PubMed database using the following descriptors: feeding problems, development of feeding skills, and preterm infants, in the period from 1996 to 2014.
Article selectionThe study titles and abstracts were identified by two independent researchers, and disagreements were resolved by consensus-based discussion. All potentially relevant studies and those whose abstracts did not provide sufficient information for inclusion or exclusion were recovered as full articles. After the literature review and selection of articles according to their objectives, an analysis of potentially relevant full texts was carried out based on the pre-established criteria, characterizing it as not single-blinded.
Inclusion criteria for article selection were: (1) publications in the period 1996–2014; (2) participation of infants and children from birth up to 10 years of age; (3) inclusion of necessary oral motor skills (OMS) for feeding; (4) development of the feeding process; and (5) inclusion of feeding difficulties during childhood.
Articles whose full texts were not accessible [obtained from the CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior) Journal Portal] were excluded from the selection, as well as those related to case studies, letters to the editor, and studies published in languages other than English, Spanish, and Portuguese. Articles whose topics were not related to the focus of this review, such as maternal diseases, children's severe illnesses, nutritional aspects of breast milk or artificial formula, specific assessments of time of dietary transition from gavage to oral feeding, and specific results of the treatment of non-nutritive sucking were also excluded.
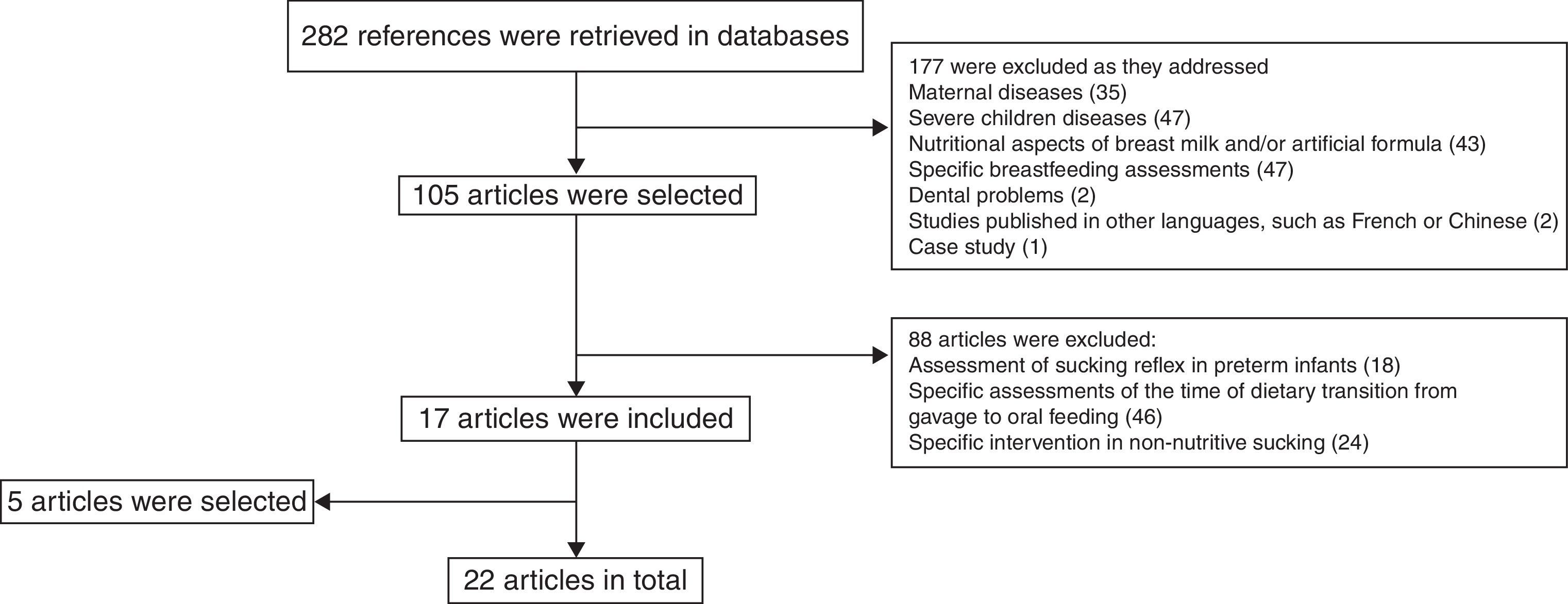
ResultsA total of 282 references were retrieved in the literature search. Of these, 177 studies were excluded, as they addressed maternal diseases (35), children's severe illnesses (47), nutritional aspects of breast milk or artificial formula (43), specific breastfeeding assessments (47), and dental problems (two). Two other reasons were also cause for exclusion: two studies published in other languages, such as French and Chinese, and one case study.
Of the remaining 105 studies, after they were read as full texts, 88 were excluded, as they addressed topics that were not relevant for the main purpose of the research, namely: (18) reviews on sucking in preterm infants in the neonatal intensive care unit environment, (46) on specific assessments of time of dietary transition from gavage to oral feeding, and (24) on specific interventions in non-nutritive sucking of infants during hospitalization. Five literature review articles were identified through the reference list of the selected articles, and were included because they addressed topics that were relevant for this research. Thus, 22 articles were included in this review. The flowchart representing article search and selection method is shown in Fig. 1.
Start of the initial feeding difficultiesFrequent exposures to harmful sensory stimuli to which VLBW preterm infants are submitted as a result of prematurity – such as intubation, upper airway aspiration, and use of feeding tubes – result in a negative experience, and consequently, aversion to oral stimuli can be observed in that population.19,20 The initial experience of the feeding process using the NG tube at birth can be a precursor to difficulties in this process, such as changes in facial and oral sensitivity, mainly in preterm infants that have used it for a period longer than three weeks.21
However, the necessary OMS for feeding continue to develop, and the literature has emphasized that eating disorders in preterm newborns may persist even after hospital discharge.19,22
Jonsson et al.,16 in a cohort study, applied a questionnaire to parents concerning the development of feeding skills during the first three years of life of 27 preterm infants (born with GA between 28 and 32 weeks, mean BW 1698g) and 29 children in the control group (CG). Children were excluded if they had congenital abnormalities or chronic diseases. The questionnaire was initially applied in the neonatal period after hospital discharge, at the time when solid foods were introduced, and at 36 months of age. The authors found that 48% of preterm children had feeding difficulties soon after hospital discharge, followed by extended feeding time (25%), vomiting (22%), poor weight gain (19%), and food refusal (15%).
Feeding difficulties in infancyThe description of the feeding difficulties in preterm infants in the first year of life is known in the literature and is made notable by the presence of oral motor dysfunction (OMD), vomiting, gastroesophageal reflux (GER), choking, aspiration, preference for only one food consistency, significant leaking of food, food refusal, reduced feeding time due to lack of attention/involvement with the feeding situation, difficulty during the food consistency transition according to the age range, difficulty chewing solid food, poor weight gain, and low volume of food intake.4,5,17,18,23–39
Norris et al.,21 through an observational study, interviewed the parents of 253 preterm infants up to 12 months of corrected age (CA) on feeding practices. The authors found that the mean age for introduction of complementary foods was 17 weeks of postnatal GA for 50% of preterm infants; however, when adjusting for the chronological age, these infants started receiving complementary foods at 11.5 weeks. Difficulties implementing the necessary OMS to swallow this new food consistency were reported by parents. One study found that food introduction occurred early in preterm infants born between 28 and 32 weeks, with mean CA of 3.2 and 4.5 months when compared to the CG.16 Another study found that the introduction of complementary foods was initiated at 3.5 months in preterm infants with GA<32 weeks and at 4 months of age in children born at term.22
Törölä et al.23 performed a longitudinal follow-up of preterm infants with CA of 1.5 to 4 months of age born with GA of 27 weeks and BW<1000g, to evaluate the development of feeding skills in these infants when compared to full-term infants. The authors observed that the sucking reflex was present with the use of a spoon when introducing complementary feeding in most preterm infants. Children exhibiting this alteration had significant leaking of food, making the feeding process long and exhausting, both for the children and their caregivers. Preterm infants needed six weeks to learn how to deal with this new food consistency, while full-term infants learned instantly.
Castro et al.,24 in an exploratory study, observed the association between GA and global motor development and the presence of early signs of alterations in the development of the orofacial myofunctional system (OMFS) in 55 preterm infants at 4 and 5 months of CA, with 29–34 weeks GA, and BW of 1500–2000g. Children with a history of neurological alterations, genetic syndromes, and congenital malformations were excluded. The authors found an association with lower GA at birth (<34 weeks) and alterations in the OMFS assessment, when compared with the group of infants that had a higher GA, between 35 and 36 weeks. The most frequent alterations were the presence of primitive oral reflexes (rooting, sucking, and phasic bite), absence of lip closure, absence of tongue activity in the frontal plane, and absence of symmetrical activity of the buccinator muscles. The authors concluded that the difficulties found in the global motor development of preterm infants were important factors for the deficits of OMFS development gain due to lack of stretching, symmetry, and synergy of the muscles that constitute the trunk, shoulder girdle, and cervical region.
Ruedell et al.,25 through a longitudinal and prospective study, investigated the OMS of preterm infants with GA between 29 and 35 weeks and mean BW of 1556g, at 4 and 6 months of CA. The presence of genetic syndromes, major congenital malformations, and children submitted to speech therapy were excluded. At 4 months old, sucking the bottle was the most affected OMS in 14 preterm children. At 6 months, 57.1% of these children did not adequately sip liquid from the cup.
Hawdon et al.4 prospectively evaluated the incidence of feeding-related problems in 35 preterm infants (mean GA of 34 weeks) in the NICU environment and described the characteristics of these children diagnosed with feeding problems at 6 and 12 months of age. Children who remained hospitalized for a period of less than five days were excluded. The authors found that 40% of preterm babies who remained hospitalized in the NICU for three months had feeding disorders, with nine of them showing important alterations, such as neurological disorders (cerebral palsy and neuromuscular disorder). At 6 months of age, parents reported that episodes of choking and vomiting were common during the feeding routine of these infants; at 12 months of age these children also had feeding difficulties, and refusal to eat was one of the main causes of stress for the family.
Mathisen et al.,26 in a cross-sectional study using video analysis, assessed the OMS and eating behaviors in 20 preterm infants, GA of 27 weeks and VLBW (<1000g), at 6 months of CA. Children diagnosed with intraventricular hemorrhage, bronchopulmonary dysplasia, or chromosomal abnormalities were excluded. The authors found that 80% of children had immaturity of the oral motor functions, such as incoordination between sucking, swallowing, and breathing, lack of head orientation in the presence of food, lip closure after swallowing, difficulty swallowing liquids, and leakage of saliva and food.
In a prospective study, Kamita et al.27 investigated the parental experience of the feeding behavior problems in 40 preterm infants up to 12 months of CA. Children with syndromes and congenital malformations and those born to adolescent parents were excluded. A small percentage of children (22.7%) born with GA<29 weeks were identified with feeding problems, such as leakage of saliva, poor weight gain, ingestion of small food volume, difficulties ingesting new consistencies, and difficulties with independent feeding. The authors found that food difficulties were significantly associated with complications of prematurity, as well as gastrointestinal and pulmonary problems.
Pridham et al.28 assessed the performance of feeding skills in 45 preterm infants with BW<1250g in a longitudinal descriptive study during the first year of life. The authors found that, at 8 and 12 months of age, regarding feeding skills, the minority of preterm infants showed delay and lack of opportunity to ingest new food consistencies, such as solid foods and drinking from a cup.
Boer and Schipper29 carried out a direct analysis of feeding skills in 47 preterm infants born with mean GA<30 weeks and BW<1286g, at 9 months of CA and CG. The authors found the occurrence of significant feeding difficulties in preterm infants when compared with the CG infants, such as episodes of asphyxia (45%), choking (55%), and accepting crusty bread (71%).
DeMauro et al.,30 in a cohort study, analyzed the feeding skills in the first year of life in 319 extremely preterm infants (born with GA of 25–33 weeks) and 571 late preterm infants (born at 34–36 weeks of GA) through a specific questionnaire applied to parents. Children with chromosomal or congenital anomalies were excluded. The authors found that the extremely preterm children had more feeding difficulties, characterized by OMD, when compared with late preterm infants at 3 months. Difficulties such as choking and food refusal resolved at 6 months of age in both groups. At 12 months, OMD and discomfort during feeding were still evident in preterm infants.
Buswell et al.31 evaluated the OMS through the analysis of videos in a small group of 15 preterm infants at 10 months of GA during feeding with different food consistencies. Children that had birth defects, heart disease, or gastrointestinal abnormalities, intraventricular hemorrhage or leukomalacia and food aspiration risk were excluded. In the present study, a small proportion of 20% of preterm children with OMD was observed. There was no association between OMD and neonatal history variables, such as GA at birth, number of days with oxygen support, and number of days from birth to feeding stabilization through OR.
Dodril et al.18 prospectively assessed the differences between oral sensitivity in preterm infants, born after 32 weeks of GA and CG in the NICU environment and the development of feeding, from 11 to 17 months of CA. Children were excluded if they had a history of structural lesions that affected the swallowing mechanism and heart, respiratory, gastrointestinal, or neurological diseases. The authors found that preterm children showed immaturity in both the incapacity to ingest liquids from a cup, as well as to eat from a spoon, when compared with children from the CG. Preterm children consumed less food during the meal; the duration of the feeding was longer; lip activity when removing the food from the spoon was lower. When compared to children in the CG, they showed higher tongue protrusion, food loss for semi-solid swallowing, and reduced sucking when swallowing liquids. The authors also found that the preterm children who used NG feeding for a period longer than three weeks tended to be weaker, having immature movements of jaw when chewing and biting into solid foods when compared with children that used NG feeding for a shorter period of time.
Douglas and Bryon20 carried out a descriptive analysis in 201 children younger than seven to investigate the risk factors that could be associated with severe chronic feeding difficulties. The authors verified that 22% of preterm infants (GA between 30 and 36 weeks) showed a high incidence of nutritional problems, from 0 to 3 months and the difficulties persisted between 3 and 6 months of age, followed by behaviors such as food spitting when urged to feed themselves, as well as choking, suffocation, GER, vomiting, and refusal to eat. The authors found that the risk factors associated with severe feeding problems in the pediatric population were underweight, stunted global development, early-onset eating disorders in the first months, and frequent vomiting history. It was pointed out that 90% of the parents reported that their children's food problems constituted one of their main stressors.
Cerro et al.22 investigated the perception of parents, through a pre-established questionnaire in relation to feeding behavior in 95 preterm children (GA<32 weeks and BW<1.5kg), aged 1.5–3.5 years, who were followed at a neonatal follow-up program and a CG. Children with severe neurological problems were excluded. The authors found significant data in relation to the rate of feeding problems, corresponding to 73% of preterm infants when compared to the CG. The most common problems were vomiting (73%), GER (33%), and failure to thrive (32%).
Crapnell et al.,32 in a longitudinal study of 127 preterm infants, GA<30 weeks, investigated the association between neonatal clinical factors and feeding problems at age 2 years through a questionnaire applied to parents. Children with congenital complications were excluded. The authors observed that 23% of children had feeding problems, 44 (55%) did not feed adequately, 24 (30%) did not accept the food immediately, 22 (28%) were selective for food, 18 (23%) spat out food, 12 (15%) refused to eat some type of food, nine (11%) refused food, eight (10%) accumulated the food between the cheeks, seven (9%) refused food that required chewing, five (6%) choked. One child was identified as having a gastrostomy and 22% had sensory alterations. The presence of these eating disorders at 2 years of age was associated with general hypotonia in the children and low socio-economic status of the parents.
Sweet et al.33 prospectively analyzed the survival and neurological development of preterm infants with BW≤600g, after 2 years of CA. A total of 104 children were identified, of which 23% survived after hospital discharge. The authors found that the diagnosis of cerebral palsy was present in 16 (76%), while three children had hemiplegia, eight children had diplegia, and five children had quadriplegia. The diagnosis of eating disorders was identified in 62% (13) of children, and 28% (six) were fed through a gastrostomy. The growth of these children was significantly impaired, and 55% of them had scores below the 10th percentile for the weight, height, and head circumference.
Wood et al.34 prospectively studied 283 preterm infants with GA<25 weeks to verify the associations between growth and feeding problems at 30 months of CA. The authors found that 33% of the parents of these children reported feeding difficulties, and 34 children had swallowing problems, 66 children had food refusal; both problems were observed in 19 of them. The differences in standard deviation for weight showed worse results in children with swallowing difficulties than in those who refused food.
Samara et al.35 conducted a descriptive study on feeding behaviors in 223 extremely preterm children, at 6 years of age, with GA<24 weeks and mean BW of 749g and in a CG, through a questionnaire applied to parents. The presence of behavioral problems, OMD, refusal to eat, and hypersensitivity showed significant associations in preterm infants, in both genders, when compared with children from the CG. The problems reported were: leakage of liquids while swallowing and difficulty biting into solid foods, found in 49 (23%) boys and 23 (10.6%) girls; hypersensitivity, found in 35 (16.4%) boys and 15 (7.04%) girls. Feeding problems were significantly associated with an inadequate growth pattern in these children, assessed at 6 years old, in addition to predictive factors such as GA, BW, and feeding difficulties in the early stages of life.
Rommel et al.5 characterized the etiologies of feeding difficulties in 700 preterm infants (GA<34 weeks) younger than 10 years. The authors showed that feeding problems in these children showed significant associations with low birth weight and GER, corresponding to 53% of children.
DiscussionThis literature review included publications that investigated feeding difficulties in preterm infants during the first years of life. Nine publications described the occurrence of feeding disorders through interviews with parents4,16,21,22,27,30,32,34,35; eight publications included direct feeding assessments18,23–26,28,29,31; two studies performed descriptive analyses to characterize the children's feeding problems5,20; and one article included the assessment of neuropsychomotor development, but the diagnoses of feeding disorders were also evidenced.33 Ten articles analyzed the associations of the variables motor development delay, GER, vomiting, pulmonary complications, lower GA and BW at birth, prolonged oxygen use, use of NG feeding, presence of hypotonia in the children, and low socio-economic status of parents as predictors for the occurrence of feeding disorders in children during infancy.4,5,21,23,26,28,31,34,36,38 Of these ten articles, seven analyzed these associations through structured interviews with parents,4,23,26,31,34,36,38 and three5,21,28 made objective assessments of feeding dynamics. The longitudinal follow-up of these children was observed in 12 articles,4,16,21,25–29,31,32,34,36 and in seven of them4,16,25,26,31,34,36 data were obtained by relying on the parents’ perceptions of their children's feeding. However, few studies have been performed to monitor feeding development, comprising the steps of dietary transition according to the age range of these children. The difficulties in conducting longitudinal studies, which depict the reality of children's feeding patterns performed through direct assessments of feeding skills by specialized professionals and comprising a small sample number, can confirm this issue. These qualitative analyses of feeding carried out through interviews with parents and retrospectively collected data may not represent an accurate assessment of these children's status.
Feeding difficulties in preterm infants have been estimated to range between 25% and 45%; for children with developmental delay, the mean increases to 33% to 80%. The proportion may increase due to the survival of extreme preterm infants and those diagnosed with neurological problems, such as cerebral palsy.33,36
The association between feeding difficulties and growth deficits has been reported with significant associations in preterm infants’ development. Failure to thrive during the first year of life has shown severe long-term problems and implications, as nutrition and growth can have an impact on the motor, cognitive, and psychological development of these children. Feeding difficulties predispose children to recurrent respiratory infections, gastrointestinal disorders, and behavioral and language problems.5,22,33,36–43
Another group of factors that can influence the performance of preterm infants’ feeding are medical complications associated with prematurity. Gastrointestinal problems, such as GER, are a major factor related to feeding difficulties in childhood. The incidence of GER is also increased by reduced respiratory capacity and the presence of feeding tubes.36,39 Evident signs, such as frequent episodes of crying, irritability, body stretching, nausea, vomiting, and refusal to eat are often reported by parents and have a negative impact on the children's feeding, appetite, and growth.5,20,22,26 GER is frequently associated with OMD and oral hypersensitivity, factors that contribute to episodes of pulmonary aspiration and pulmonary chronic diseases, considered one of the main reasons for the increase in hospital length of stay.39 The constant acid irritation in the esophagus makes children lose the desire to eat and associate food with something that causes displeasure and pain. Some children who have oral hypersensitivity usually react excessively to changes in food flavor and consistency, with episodes of nausea. This factor may explain difficulties children have when dealing with solid foods that require chewing and, consequently, episodes of refusal to eat certain foods are common during the feeding routine.40
Diseases that affect the respiratory pattern, such as bronchopulmonary dysplasia, also cause feeding difficulties. The lack of coordination between sucking, swallowing, and breathing, as well as long apnea periods, result in disturbance of the lip and jaw movements during feeding.2,41 Due to this factor, these children cannot achieve complete recovery during respiratory pauses of sucking, becoming fatigued and tired before the end of feeding, and are thus unable to ingest the entire food volume. The respiratory effort also results in high energy expenditure, which often leads to growth deficits, when aggravated by the decrease in daily energy consumption.36
The understanding that successful feeding of VLBW preterm newborns should occur during hospitalization only to attain hospital discharge is a mistake, as children's feeding skills continues to develop concomitantly with other development milestones, such as motor development and communication skills.12,19
The acquisition of the necessary OMS for each food consistency is closely related to the children's motor development.36 Preterm children who have a delay in global motor development when considering the CA may also have delays in OMS, when compared with normal children. Unfavorable feeding results in the short- and long-term are attributed not only to preterm infants’ development failures, but also to the fact they are forced to feed at an early stage, when not all of the OMS have been reached.13
The studies included in this review showed that early introduction of complementary feeding, at 3 and 4 months of CA, contributed to the occurrence of major problems, such as irritability, stress, choking, nausea, and vomiting. The preterm children's neurological immaturity prevents them from using all necessary OMS to deal with this new food consistency and the spoon utensil.12,27
Due to these initial difficulties, parents, as they do not have the knowledge and strategies needed to help their children acquire better skills and involvement in the feeding process, choose to further facilitate the latter. Situations such as inadequate positioning of these children (inclined position) in order to avoid leakage of food and help swallowing with the aid of gravity, as well as offering preferably semi-solid foods for better acceptance, result in the lack of development of adequate feeding skills.20 These aspects can result in significant alterations in oral motor development,36 making them more prone to swallowing disorders with foods of different textures and consistencies and, as a result, making them more prone to difficulties with solid food mastication.30
The introduction of complementary foods at 6 months of CA can increase the chances of achieving successful feeding, as these infants are neurologically more organized and have more sensory experience, which are essential for better food acceptance. Giving these children opportunities to play with and orally explore objects of different textures will prepare them for a better feeding performance with the spoon and, consequently, lead to pleasure in this new feeding phase.40
Problems with the start of the process of chewing different food textures are also demonstrated in preterm infants, such as vomiting, refusal to eat, and choking.19 Concurrently with such difficulties, the parents do not perform the adequate food consistency progression according to the age group, and offer a limited number of consistencies.4,5,15,27–31 This has been explained, in part, due to the initial aversive oral experiences during hospitalization in the NICU, with prolonged use of NG feeding, mechanical ventilation, aspiration of upper and lower respiratory tract, and gastrointestinal problems, such as occurrence of GER. These factors can contribute to an increase in oral sensitivity, which results in aversion to new food textures.5,18,20,22,27,40 Immaturity and neurological disorganization may also explain this issue, due to the lack of control and organization of the oral muscles, necessary for chewing.40
Offering opportunities for preterm children to acquire the appropriate learning experiences in the early stages of feeding actually contributes to prevent feeding disorders. Children who are more stimulated with the environment and able to interact with their parents can more easily fit the developmental changes in skills required for successful feeding.42,43
The follow-up of preterm infants aiming at monitoring all stages of dietary transition, with objective and direct assessments of feeding skills carried out by a qualified audiologist, is strictly recommended. Such conduct leads to appropriate guidance to mothers, regarding appropriate eating utensils and consistencies according to the child's age, in order to favor the correct way to offer food, making them able to use all necessary OMS when feeding. Consequently, the child will receive learning experiences, which will contribute to the successful and adequate development of OMFS and the mother–child bond. The earlier the child's eating disorders are diagnosed, the better the chances to perform successful interventions.12,13,19,21,40,42,43
ConclusionBased on the articles assessed in this literature review, it can be affirmed that preterm infants, especially those born with VLBW, are more prone to feeding problems in the early stages of life and during childhood, when compared with children born at term. The monitoring of these children's nutritional status is strictly recommended in an early intervention program with specialized professionals, aiming to promote adequate nutritional development, as well as to ensure adequate growth.
FundingThis research received funding subsidized by FAPESP 2013/13734-2.
Conflicts of interestThe authors declare no conflicts of interest.
We thank Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP), for funding this research.
Please cite this article as: Pagliaro CL, Bühler KE, Ibidi SM, Limongi SC. Dietary transition difficulties in preterm infants: critical literature review. J Pediatr (Rio J). 2016;92:7–14.