To evaluate the impact of a curricular intervention concerning the knowledge about asthma among adolescents from a public school.
MethodsThis was a randomized, controlled trial study on a curricular intervention in asthma, carried out with asthmatic and non-asthmatic adolescents. The study participants were divided into a curricular intervention group for asthma (IG), and a control group with traditional curriculum (CG). Topics related to asthma were included in the curriculum, such as the disease concept, triggering factors, treatment, symptoms, action plan, and beliefs in popular myths about the disease. These topics were evaluated through a questionnaire with scores ranging from 0 to 20 points, expressed by the mean score. The acquisition of knowledge was evaluated 90 days and 540 days after the start of the intervention (baseline), by applying the mixed linear model for analysis of associations.
Results181 students participated in the study (IG=101 and CG=80). As shown by their scores before the intervention; the students were unaware about asthma (IG: x¯=10.7±2.9vs. CG: x¯=11.5±2.7 points), its treatment (IG: x¯=1.6±0.9vs. CG: x¯=1.6±0.8 points), and reported beliefs in popular myths about the disease (IG: x¯=1.5±1.1vs. CG: x¯=1.7±1.1 points). After the intervention, the IG showed higher overall knowledge (GI: x¯=15.5±3.1 points), as well as knowledge about the treatment (GI: x¯=2.5±1.0 points), and two times more knowledge in the field “beliefs in popular myths about the disease” when compared to the CG. A greater probability of achieving satisfactory knowledge about asthma was noted in the IG (RR=3.5), with NTT=2.0.
ConclusionThe inclusion of the asthma topic in the curriculum improved knowledge about the disease in a subgroup of students.
Avaliar o impacto de uma intervenção curricular sobre o conhecimento em asma dos adolescentes de um colégio público.
MétodosEnsaio controlado e randomizado de uma intervenção curricular em asma, conduzido com adolescentes, asmáticos e não asmáticos, alocados em: grupo intervenção curricular em asma (GI) e grupo controle com currículo tradicional (GC). Foram inseridos no currículo tópicos relacionados à asma tais como o conceito, fatores desencadeantes, tratamento, sintomas, plano de ação e crenças em mitos populares sobre a doença, avaliados por meio de um questionário com escore de 0-20, expressos em média de acertos. Avaliou-se a apreensão do conhecimento 90 dias e 540 dias após o início da intervenção (baseline), aplicou-se o modelo linear misto para análise das associações.
Resultados181 estudantes participaram do estudo (GI=101 e GC=80). Os estudantes desconheciam a asma, como revelam os seus escores anteriores à intervenção (GI: x¯=10,7±2,9vs. GC: x¯=11,5±2,7 acertos), seu tratamento (GI: x¯=1,6±0,9vs. GC: x¯=1,6±0,8 acertos) e relataram crenças em mitos populares sobre a doença (GI: x¯=1,5±1,1vs. GC: x¯=1,7±1,1 acertos). Após a intervenção, o GI apresentou maior conhecimento geral (GI: x¯=15,5±3,1 acertos); sobre o tratamento (GI: x¯=2,5±1,0 acertos) e duas vezes mais conhecimento no domínio “crenças em mitos populares sobre a doença” comparado ao GC. Maior probabilidade de alcançar conhecimento satisfatório sobre a asma foi observado no GI (RR=3,5), com NNT=2,0.
ConclusãoA inserção do tema asma no currículo é capaz de elevar o conhecimento sobre a doença em um subgrupo de estudantes.
Asthma is the most common chronic disease among children and adolescents, with a worldwide prevalence of 14%.1 In Brazil, it is estimated that 23.2% of adolescents have symptoms suggestive of the disease, one of the highest worldwide prevalence rates.2 At this age range, asthma is the third cause of hospitalization and death among respiratory diseases3 in Brazil.
Education is one of the pillars for asthma management, and has been recommended by national and international guidelines.4 Despite these recommendations, patients and relatives of asthmatic individuals have a low level of knowledge about the disease, which contributes to undertreatment and lack of symptom control,5–7 high morbidity, social isolation, future working inability,7 and early death8 at school-age.9
The school environment is favorable to asthma guidelines, primarily for adolescents.10–16 School educational actions have been developed by health professionals and have contributed to the reduction of underdiagnosis,11 morbimortality, and the emotional burden caused by asthma in countries such as the USA and Australia.9,11,14 Despite the successful results in high-income countries, there are few initiatives in economically-disadvantaged countries.11
In middle-income countries, such as Brazil, educational interventions on asthma carried out in schools can also be an effective strategy for health promotion, and for control of asthma and other chronic respiratory diseases. Despite this, there are no standardized actions in Brazil that include guidelines on asthma in schools’ curricular activities. In the city of Salvador, state of Bahia, Brazil, despite the existence of a successful program for asthma control, in which health education is one of the pillars for the disease management,17 the authors did not identify educational actions aimed at adolescents in the school environment.
An alternative for the development of educational actions aimed at prevention and promotion of health in schools is the inclusion of health-related themes into the school curriculum.18,19 The inclusion of these themes into the curriculum allows for health issues such as asthma to be studied during school hours on a permanent basis, integrated into the curricular content, not fragmented or isolated from other school activities, and associated with the students’ reality.18,19
The aim of this study was to evaluate the impact of a curricular intervention in asthma on the knowledge about the disease among the adolescents from a public school in Salvador, Bahia.
MethodsStudy design, site, and participantsA controlled, single-blinded, randomized trial of an educational intervention in asthma with adolescents from a public school, located in Salvador, Bahia, Northeastern Brazil, was carried out. The study was conducted in a medium-sized school, considered a model school in the region's public network.
The study was approved by the Research Ethics Committee of Universidade Federal da Bahia (Opinion no. 046/2011). Registration number at clinicaltrials.gov: NCT02142179.
Sample characteristicsAll 511 students enrolled in elementary school were invited to participate in the study. A total of 212/511 (41.5%) adolescents, asthmatics or non-asthmatics, aged 10–19 years old, who signed the Informed Consent Form and Term of Assent were included. Subjects who did not complete all follow-up visits or who did not fill out the questionnaires in full were excluded from the study.
Group allocationParticipants were divided into two groups: curricular intervention in asthma (IG) and traditional curriculum – control (CG). The allocation criterion was defined according to the enrollment system. Students attending the afternoon shift were drawn by lots to be allocated to the IG and those attending the morning shift, the CG.
Sample size calculationThe sample size was calculated using the WinPepi program (PEPI-for-Windows: computer programs for epidemiologists, version 11.6), obtained through a pilot study, with a 95% chance of detecting elevation of the primary outcome – the asthma knowledge score (scale of 0–20 correct answers). The mean number of correct answers adopted for the IG was 15.5±3.1 and in the CG, 10.4±3.9, with a magnitude of effect of 5.1 points in the mean of correct answers and a 5% level of significance. A sample of 26 individuals was estimated.
Curricular interventionPreviously trained elementary school teachers carried out the curricular intervention. All staff members underwent a 240-min training on topics related to the respiratory system, asthma concepts, triggering factors, symptoms, treatment, action plan, and popular beliefs about the disease. Additionally, 12 pedagogical plans were developed with the teachers, in partnership with professors in the field of health of Universidade Federal da Bahia (UFBA).
The aim was to include health and asthma content in the school curriculum to provide the school community with training in citizenship for health and the possibility of recognizing aspects related to asthma, such as prevention and control measures. This intervention was based on legislation that institute health18 and asthma education at schools.14,19
Subjects on health and asthma were included in different curricular components, such as sciences, Portuguese language, writing, and history, with a total duration of ten hours per month. The teachers presented to the students concepts about (i) the anatomy and physiology of the respiratory system; (ii) the influence of air pollution, environmental factors, and smoking on respiratory diseases; (iii) asthma as a respiratory system disease; (iv) asthma symptoms; (v) treatment; and (vi) clarification of beliefs in popular myths related to asthma and inhalation treatment.
Pedagogical resources and techniques were used, such as artificial anatomical models, an educational booklet (www.ginanobrasil.org.br), cultural scavenger hunts, and didactic texts on the subject.
Data collection toolsA questionnaire was applied to evaluate the knowledge about asthma in the baseline period (V0), 90 days (V90), and 540 days after the baseline period (V540). A subgroup of 88 students (50% of the sample), obtained through a simple drawing of lots using Microsoft Excel (Microsoft®, version 2011, WA, USA), was evaluated in the V540 as verification of asthma knowledge maintenance.
The frequency of individuals with symptoms suggestive of asthma was obtained through the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire.20 Sociodemographic information, self-report of asthma diagnosed by a physician, and learning difficulties were collected through a structured questionnaire.
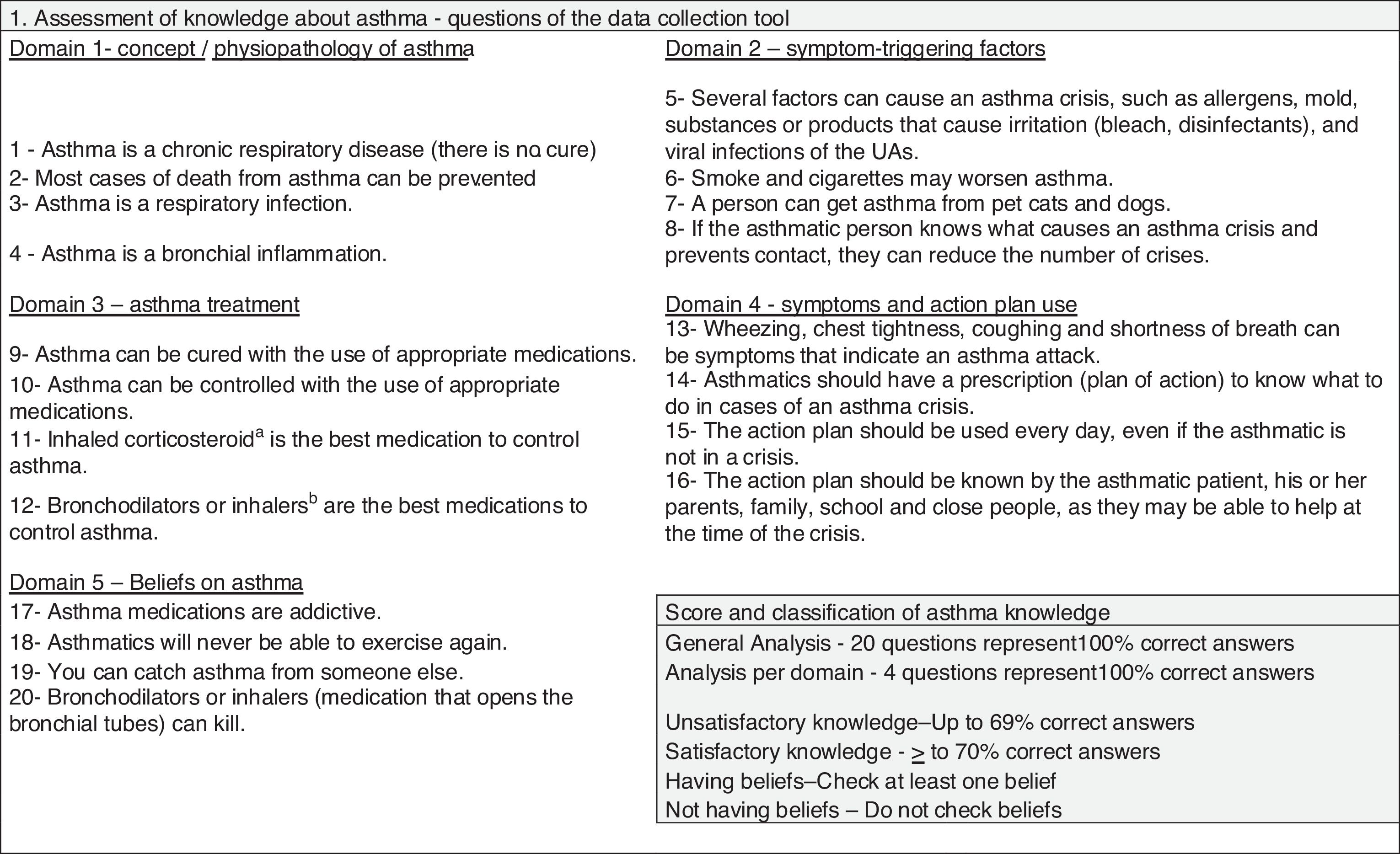
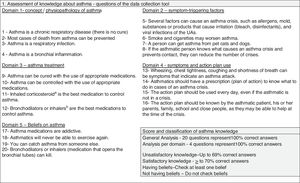
Asthma knowledge assessmentThe knowledge about asthma was assessed through a self-administered questionnaire with 20 questions and five domains: (i) concept, (ii) triggering factors, (iii) treatment, (iv) symptoms/action plan, and (v) beliefs in popular myths about asthma. All items of the tool had the alternatives “yes,” “no,” and “do not know,” and were analyzed considering the number and proportion of correct answers in the general score and for each domain. Increases in the scores indicated increase in knowledge. The knowledge was stratified as unsatisfactory (up to 69% correct answers) or satisfactory (≥70% of correct answers; Fig. 1).
Statistical analysisKnowledge about asthma was used as the primary outcome. Data were analyzed using SPSS (IBM SPSS Statistics for Windows, Version 21.0. NY, USA). Analysis by protocol of the clinical trial and intention to treat were performed. As there were no significant differences between the two, it was decided to perform the analysis by protocol. The variables showed a normal distribution, verified by the Kolmogorov–Smirnov test. Means and standard deviations were calculated for age, years of study, and knowledge score. Simple frequency and proportions were calculated for the variables gender, school repetition, years of study, history of allergy, family history of asthma/allergy, previous asthma, wheezing in the last year, and the presence of beliefs in popular myths.
In V0, clinical and sociodemographic differences among students were analyzed using the chi-squared test and Student's t-test. In V90, knowledge on asthma was analyzed by the t-test for independent samples and by analysis of variance (ANOVA). Modifications in the outcome means were evaluated using the paired Student's t-test.
In V540, knowledge maintenance was analyzed using the paired Student's t-test. The increments obtained in the knowledge score were calculated based on the difference of means observed before and after the intervention, expressed in proportions. In all the study periods, a subgroup analysis was performed to compare knowledge about asthma between asthmatic and non-asthmatic students.
The estimate of the treatment effect size was calculated through Cohen's d index (Cohen's d index=x¯IG−x¯CG/SDCOMBINED). For the interpretation of the effect size values, Cohen's classification was used (insignificant (<0.19), small (0.20–0.49), medium (0.50–0.79), large (0.80–1.29), very large (>1.30).21
The relative risk (RR) was calculated for the outcome satisfactory knowledge about asthma, as well as the NNT – number needed to treat. Multinomial logistic regression was used to identify whether age, gender, school repetition, years of study, history of allergy, family history of asthma/allergy, previous asthma, wheezing in the last year, and the presence of beliefs in popular myths were associated with knowledge about asthma. Analysis of covariance (ANCOVA) was used with the same variables tested in the multinomial regression, aiming to verify the possible co-variances. Significant associations (p<0.05) were selected to be tested in the mixed linear models.
ResultsClinical and sociodemographic characteristics of the IG and CGA total of 181/212 students completed all the evaluation steps (85.4%; 101 in the IG and 80 in the CG), considering a loss of 13.2% in the IG (n=28) and 1.4% in the CG (n=3).
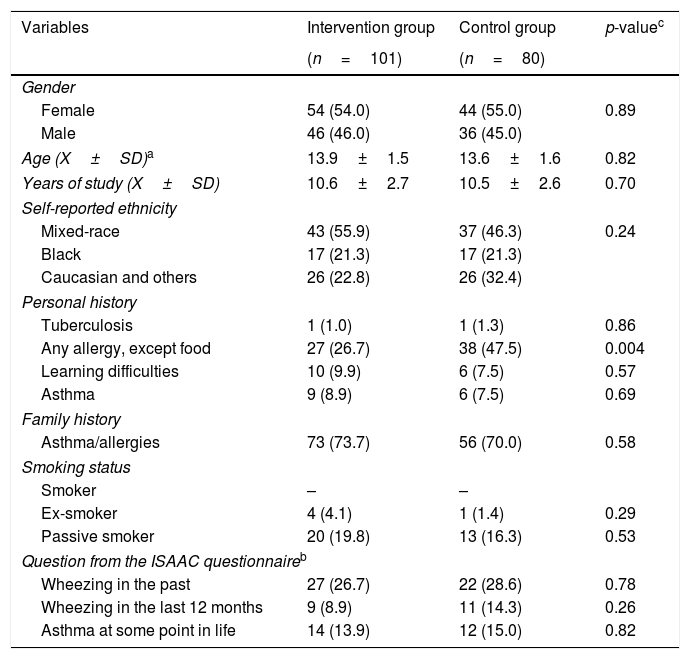
The mean age (±SD) of the participants was 13.9±1.5 (IG) and 13.6±1.6 (CG). Female gender and self-reported mixed-race ethnicity predominated in both groups. The report of asthma diagnosis was observed in nine (8.9%) and six (7.5%) individuals in the IG and CG groups, respectively. At baseline, clinical and sociodemographic characteristics were similar between groups; history of allergy was more often observed in the CG (Table 1).
Clinical and sociodemographic characteristics of the adolescents participating in the intervention and in the control group at baseline, in a public school in Salvador, Bahia, Brazil, 2017.
| Variables | Intervention group | Control group | p-valuec |
|---|---|---|---|
| (n=101) | (n=80) | ||
| Gender | |||
| Female | 54 (54.0) | 44 (55.0) | 0.89 |
| Male | 46 (46.0) | 36 (45.0) | |
| Age (X±SD)a | 13.9±1.5 | 13.6±1.6 | 0.82 |
| Years of study (X±SD) | 10.6±2.7 | 10.5±2.6 | 0.70 |
| Self-reported ethnicity | |||
| Mixed-race | 43 (55.9) | 37 (46.3) | 0.24 |
| Black | 17 (21.3) | 17 (21.3) | |
| Caucasian and others | 26 (22.8) | 26 (32.4) | |
| Personal history | |||
| Tuberculosis | 1 (1.0) | 1 (1.3) | 0.86 |
| Any allergy, except food | 27 (26.7) | 38 (47.5) | 0.004 |
| Learning difficulties | 10 (9.9) | 6 (7.5) | 0.57 |
| Asthma | 9 (8.9) | 6 (7.5) | 0.69 |
| Family history | |||
| Asthma/allergies | 73 (73.7) | 56 (70.0) | 0.58 |
| Smoking status | |||
| Smoker | – | – | |
| Ex-smoker | 4 (4.1) | 1 (1.4) | 0.29 |
| Passive smoker | 20 (19.8) | 13 (16.3) | 0.53 |
| Question from the ISAAC questionnaireb | |||
| Wheezing in the past | 27 (26.7) | 22 (28.6) | 0.78 |
| Wheezing in the last 12 months | 9 (8.9) | 11 (14.3) | 0.26 |
| Asthma at some point in life | 14 (13.9) | 12 (15.0) | 0.82 |
Continuous variables expressed as mean and standard deviation. Student's t-test was used to analyze the differences of the variables age and years of study. The differences between the other variables were analyzed using the chi-squared test.
In V0, it was observed that 89% of the IG students (x¯=10.7±2.9 of correct answers) and 85% of the CG students (x¯=11.5±2.7 correct answers) had unsatisfactory knowledge about asthma. Treatment was the most unknown item in both groups (IG=1.6±0.9 correct answers vs. CG=1.6±0.8) (Tables 2 and 3), including in the subgroup of asthmatic students (x¯=1.7±1.0 correct answers). 80.6% of the students (n=146) could not differentiate when the relief or maintenance medication should be used and 89.5% were not aware of the indication for short-acting bronchodilator use.
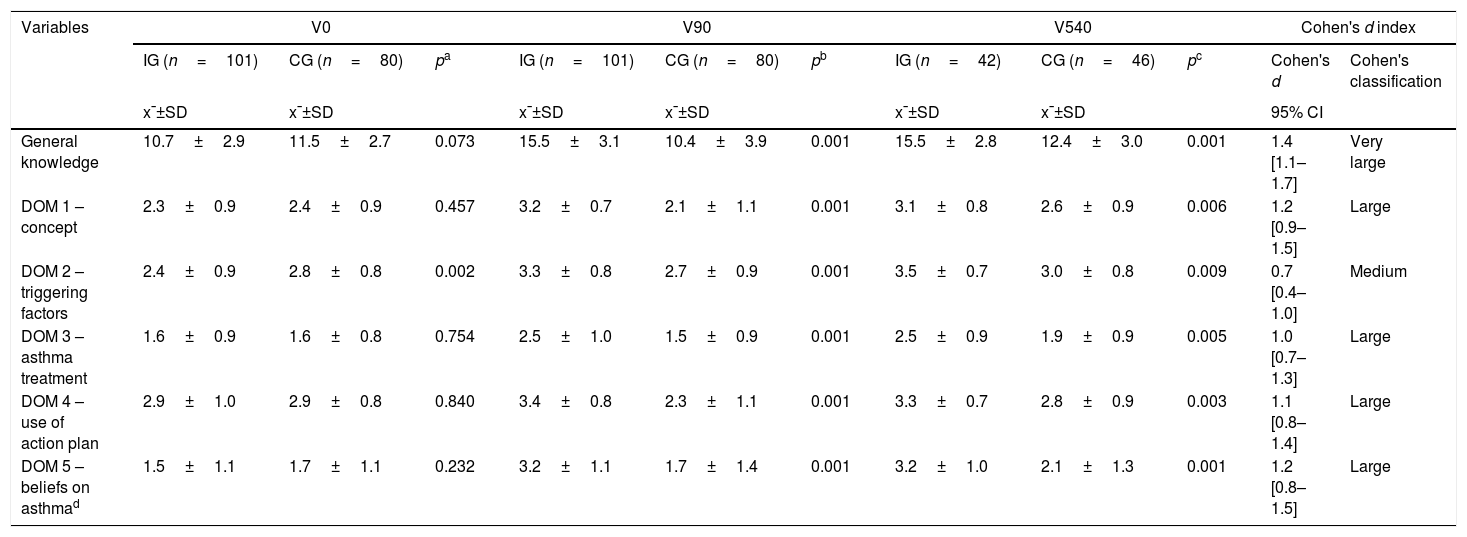
Comparison of the degree of knowledge of the adolescents from the intervention group vs. the control group on asthma in the general analysis and by domain, during the follow-up period in a public school in Salvador, Bahia, Brazil. 2017.
| Variables | V0 | V90 | V540 | Cohen's d index | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| IG (n=101) | CG (n=80) | pa | IG (n=101) | CG (n=80) | pb | IG (n=42) | CG (n=46) | pc | Cohen's d | Cohen's classification | |
| x¯±SD | x¯±SD | x¯±SD | x¯±SD | x¯±SD | x¯±SD | 95% CI | |||||
| General knowledge | 10.7±2.9 | 11.5±2.7 | 0.073 | 15.5±3.1 | 10.4±3.9 | 0.001 | 15.5±2.8 | 12.4±3.0 | 0.001 | 1.4 [1.1–1.7] | Very large |
| DOM 1 – concept | 2.3±0.9 | 2.4±0.9 | 0.457 | 3.2±0.7 | 2.1±1.1 | 0.001 | 3.1±0.8 | 2.6±0.9 | 0.006 | 1.2 [0.9–1.5] | Large |
| DOM 2 – triggering factors | 2.4±0.9 | 2.8±0.8 | 0.002 | 3.3±0.8 | 2.7±0.9 | 0.001 | 3.5±0.7 | 3.0±0.8 | 0.009 | 0.7 [0.4–1.0] | Medium |
| DOM 3 – asthma treatment | 1.6±0.9 | 1.6±0.8 | 0.754 | 2.5±1.0 | 1.5±0.9 | 0.001 | 2.5±0.9 | 1.9±0.9 | 0.005 | 1.0 [0.7–1.3] | Large |
| DOM 4 – use of action plan | 2.9±1.0 | 2.9±0.8 | 0.840 | 3.4±0.8 | 2.3±1.1 | 0.001 | 3.3±0.7 | 2.8±0.9 | 0.003 | 1.1 [0.8–1.4] | Large |
| DOM 5 – beliefs on asthmad | 1.5±1.1 | 1.7±1.1 | 0.232 | 3.2±1.1 | 1.7±1.4 | 0.001 | 3.2±1.0 | 2.1±1.3 | 0.001 | 1.2 [0.8–1.5] | Large |
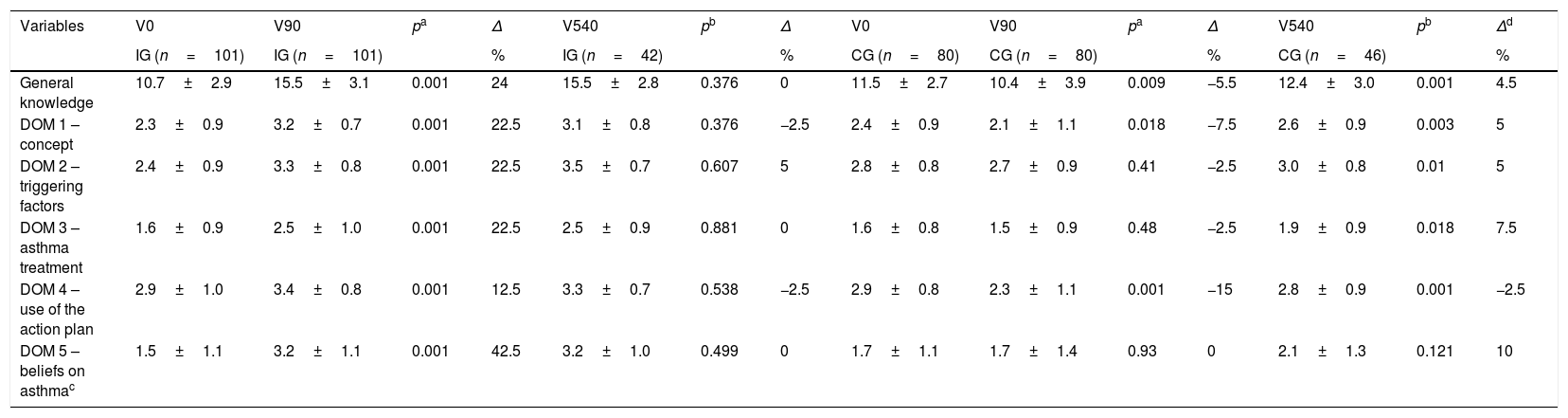
Comparison of the means and percentage variation (Δ) of the intervention group vs. intervention group and the control group vs. control group, regarding the knowledge of adolescents about asthma in the general analysis and by domain during the entire follow-up period in a public high school in Salvador, Bahia, Brazil, 2017.
| Variables | V0 | V90 | pa | Δ | V540 | pb | Δ | V0 | V90 | pa | Δ | V540 | pb | Δd |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| IG (n=101) | IG (n=101) | % | IG (n=42) | % | CG (n=80) | CG (n=80) | % | CG (n=46) | % | |||||
| General knowledge | 10.7±2.9 | 15.5±3.1 | 0.001 | 24 | 15.5±2.8 | 0.376 | 0 | 11.5±2.7 | 10.4±3.9 | 0.009 | −5.5 | 12.4±3.0 | 0.001 | 4.5 |
| DOM 1 – concept | 2.3±0.9 | 3.2±0.7 | 0.001 | 22.5 | 3.1±0.8 | 0.376 | −2.5 | 2.4±0.9 | 2.1±1.1 | 0.018 | −7.5 | 2.6±0.9 | 0.003 | 5 |
| DOM 2 – triggering factors | 2.4±0.9 | 3.3±0.8 | 0.001 | 22.5 | 3.5±0.7 | 0.607 | 5 | 2.8±0.8 | 2.7±0.9 | 0.41 | −2.5 | 3.0±0.8 | 0.01 | 5 |
| DOM 3 – asthma treatment | 1.6±0.9 | 2.5±1.0 | 0.001 | 22.5 | 2.5±0.9 | 0.881 | 0 | 1.6±0.8 | 1.5±0.9 | 0.48 | −2.5 | 1.9±0.9 | 0.018 | 7.5 |
| DOM 4 – use of the action plan | 2.9±1.0 | 3.4±0.8 | 0.001 | 12.5 | 3.3±0.7 | 0.538 | −2.5 | 2.9±0.8 | 2.3±1.1 | 0.001 | −15 | 2.8±0.9 | 0.001 | −2.5 |
| DOM 5 – beliefs on asthmac | 1.5±1.1 | 3.2±1.1 | 0.001 | 42.5 | 3.2±1.0 | 0.499 | 0 | 1.7±1.1 | 1.7±1.4 | 0.93 | 0 | 2.1±1.3 | 0.121 | 10 |
Note: Data shown as mean±SD.
Ninety percent of the students reported beliefs in popular myths about the disease. The most frequently reported beliefs in popular myths were: (i) deleterious effect of medications to control asthma exacerbation (84.5%); (ii) addiction caused by the use of relief medications (64.6%); and (iii) harmful effect of physical activities on the disease (49.7%).
Post-intervention assessment of knowledge at 90 and 540 daysNinety days after the intervention, 92% of the IG students had higher scores of knowledge when compared to the CG (IG=15.5±3.1 vs. CG=10.4±3.9, p=0.001), representing a “very large” effect size (d=1.4, 95% CI=1.1–1.7). The IG also obtained a 24% increase in the total score of general knowledge about asthma, compared to the baseline period.
After 90 days, the knowledge about asthma treatment and concepts increased at the same rate, 22.5%, for the IG. When comparing the groups, 84% of the IG students showed higher knowledge scores in the “concept” and “treatment” domains when compared to the CG means (concept score: IG=3.2±0.7 vs. CG=2.1±1.1, p=0.001; treatment score: IG=2.5±1.0 vs. CG=1.5±0.9, p=0.001). In these domains, large effect magnitudes were observed (concept: d=1.2, 95% CI=0.90–1.5 and treatment: d=1.0, 95% CI=0.7–1.3).
In V90, beliefs in popular myths reported in the baseline period were overcome by participants in the intervention, since the IG students showed approximately a two-fold increase in the score of the “asthma-related beliefs” domain (IG=3.2±1.1 vs. CG=1.7±1.4, p=0.001). In this domain, the increase in the scores is related to the clarification of the beliefs in asthma-related popular myths. Furthermore, it was observed that 88% of the IG participants had higher scores in this domain than the CG means.
In V540, knowledge about asthma and all domains was maintained in the IG (Tables 2 and 3).
Comparison of knowledge about asthma between asthmatic and non-asthmatic students participating in the curricular interventionIn the subgroup analysis, only family history of asthma/allergy (86.7%) and self-report of learning difficulties (3.3%) were more frequent in asthmatics. Differences were not found between asthmatic and non-asthmatic individuals regarding clinical and sociodemographic characteristics.
In the baseline period, greater knowledge about the treatment was observed among asthmatic (47.5% of correct answers), compared to non-asthmatic individuals (40% of correct answers). In V90, there was an improvement in knowledge about asthma in both groups.
In V540, maintenance of the knowledge about asthma in both groups was demonstrated. After the intervention (V90), no significant changes were observed in the morbidity indicators among asthmatic students. The IG showed higher rates of maintenance medication use and physician-prescribed action plans, a behavior not observed in the CG.
Factors associated with satisfactory knowledge about asthmaThe variables age, gender, school repetition, years of study, history of allergy, family history of asthma/allergy, wheezing in the previous year, and previous asthma were tested. Only “wheezing in the previous year” was associated with a satisfactory knowledge about asthma. It was observed that having beliefs in popular myths related to the disease can modify the educational intervention effect, worsening the understanding of the disease (p<0.05).
In V90, it was observed that students submitted to the educational intervention had a 3.5-fold higher probability of achieving satisfactory general knowledge about asthma. (95% CI=2.1–5.6). Similarly, higher probabilities of having knowledge related to the “disease concept” (RR=4.9, 95% CI=2.9–8.4), “treatment” (RR=3.2; 95% CI=1.7–5.7), and “beliefs in popular myths related to asthma” domains (RR=2.0; 95% CI=1.5–2.7) were observed. A similar behavior was observed in V540. An NNT of 2.0 (95% CI=2–3) was identified for this subgroup.
DiscussionThe present study identified that 87% of the students had previously unsatisfactory knowledge about asthma. The relief and maintenance treatment were the most unknown topics in this sample. Also observed was an intense presence of beliefs in popular myths that interfered with disease understanding. The intervention used, through health education measures incorporated into a public-school curriculum, promoted a great improvement in adolescents’ knowledge of asthma. Knowledge apprehension was evaluated early at 90 days and late at 540 days, suggesting that curricular interventions promote long-lasting knowledge apprehension.
In the sample, the students did not have knowledge of asthma in general, with the concept and treatment of asthma being the least known subjects. After training, significant improvement in knowledge on the subject was observed in the IG compared to the CG at V90, which was maintained up to V540. This acquired knowledge about asthma concepts and treatment may promote adequate subject dissemination among asthmatic and non-asthmatic adolescents, the recognition of individuals with disease symptoms at school, and the use/recommendation of the maintenance medication for asthma control, as well as for relief in situations of disease exacerbation, by the school community,14–16 contributing to a safer school environment.
The strong presence of beliefs in popular myths about asthma among adolescents interfered with disease understanding, but were overcome after the intervention in 82% of the IG sample. The clarification of concepts about the disease nature and treatment can influence safer actions in cases of asthma exacerbation and daily control22 by the students. Additionally, overcoming beliefs in popular myths may reduce social discrimination by non-asthmatic peers,23,24 reduce the occurrence of depression and anxiety among adolescents with asthma,23,24 and increase the participation of asthmatics in physical education activities at school.24
Furthermore, it was identified that disease-related beliefs in popular myths can modify the educational intervention effect, worsening the final result on asthma knowledge. The presence of beliefs in health is a behavior predictor and they should be clarified to the population.25 Popular myths observed among adolescents regarding the concept of asthma, the physical limitations caused by the disease, and inhalation treatment should be demystified,26 even before an educational intervention is started and reviewed during the entire educational program.14–16
Asthma education, when applied alone, can be a viable alternative for increasing knowledge about the disease that may have a medium- and long-term impact on morbidity indicators.9–12 For the short-term impact on morbidity indicators, education must be associated with clinical follow-up. In the present study, for instance, it was observed among the asthmatics, there was greater report of maintenance medication use and action plans after the intervention. However, there were no reductions in visits to emergency services and nocturnal awakenings, probably because of the small number of asthmatics in the sample, the low frequency of symptoms, and the intervention model aimed at disseminating knowledge about asthma to the entire community rather than the teaching of self-management skills.
In parallel, the results found in this study demonstrate that school interventions on asthma can be extended to the entire school community instead of only asthmatics. The broad and articulated discussion of a public health problem such as asthma, adding it to the conventional curricular components, can (i) train multipliers of knowledge on aspects related to health and asthma, extrapolating this theme to out of the school environment27; (ii) promote civil empowerment and promote the search for better health conditions for students28; (iii) decrease the stigma associated with chronic diseases, such as asthma23; (iv) to consolidate behaviors that prevent the progression of chronic diseases29; and (v) to enable students to assist their peers in acute asthma episodes.29
In this study, the authors used asthma as one of the curricular subjects, but they suggest that this intervention can be applied to other chronic respiratory diseases and health conditions, such as healthy eating and smoking.26,30 It is hypothesized that this model can be reproduced in different regions of Brazil because it is simple and has low cost; does not require additional professionals in the school environment27,30; is carried out by teachers trained27 by health professors; and allows students from low-income families, with restricted access to health services, to acquire lasting knowledge about a serious public health problem.
Among the study limitations, the following should be mentioned: the lack of recording of school absenteeism due to asthma; the self-report of diagnosed asthma; the lack of disease severity evaluation; and the intentional construction of a subgroup with 50% of the initial sample in V540. A cost-effectiveness analysis of the intervention was not performed. However, this is considered a low-cost intervention, as it was carried out by trained teachers who worked at the school, which favors its feasibility.
To summarize, inclusion of asthma-related topics to the school curriculum is capable of increasing knowledge about asthma in a satisfactory and lasting manner among asthmatic and non-asthmatic elementary school students. It is a simple model that can be applied to the entire school community; it can be reproduced for other chronic respiratory diseases, and can be developed in different regions and countries, respecting the cultural and political diversities of each region.
FundingFundação de Amparo à Pesquisa do Estado da Bahia (FAPESB).
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Coelho AC, de Souza-Machado C, Oliveira TS, Santos TN, Cruz ÁA, Souza-Machado A. Curricular intervention increases adolescents’ knowledge about asthma: a randomized trial. J Pediatr (Rio J). 2018;94:325–34.