to evaluate the frequency of respiratory viral infections in hospitalized infants with clinical suspicion of pertussis, and to analyze their characteristics at hospital admission and clinical outcomes.
Methodsa historical cohort study was performed in a reference service for pertussis, in which the research of respiratory viruses was also a routine for infants hospitalized with respiratory problems. All infants reported as suspected cases of pertussis were included. Tests for Bordetella pertussis (BP) (polymerase chain reaction/culture) and for respiratory viruses (RVs) (immunofluorescence) were performed. Patients who received macrolides before hospitalization were excluded. Clinical data were obtained from medical records.
ResultsAmong the 67 patients studied, BP tests were positive in 44%, and 26% were positive for RV. There was no etiological identification in 35%, and RV combined with BP was identified in 5%. All patients had similar demographic characteristics. Cough followed by inspiratory stridor or cyanosis was a strong predictor of pertussis, as well as prominent leukocytosis and lymphocytosis. Rhinorrhea and dyspnea were more frequent in viral infections. Macrolides were discontinued in 40% of patients who tested positive for RV and negative for BP.
Conclusionthe results suggest that viral infection can be present in hospitalized infants with clinical suspicion of pertussis, and etiological tests may enable a reduction in the use of macrolides in some cases. However, the etiological diagnosis of respiratory virus infection, by itself, does not exclude the possibility of infection with BP.
avaliar a frequência das infecções por vírus respiratórios em lactentes hospitalizados com suspeita clínica de coqueluche e analisar suas características admissionais e evolutivas.
Métodosfoi realizado um estudo de coorte histórica, em um serviço sentinela para coqueluche, no qual a pesquisa de vírus respiratórios também foi rotineira para os lactentes hospitalizados com problemas respiratórios. Foram incluídos todos os lactentes submetidos à notificação compulsória de suspeita de coqueluche. Foram realizadas pesquisas para Bordetela pertussis – BP (PCR/cultura) e vírus respiratórios – VR (imunofluorescência). Foram excluídos os pacientes que haviam recebido macrolídeos previamente à internação. Os dados clínicos foram obtidos dos prontuários.
Resultadosdentre os 67 pacientes analisados, a pesquisa para BP foi positiva em 44% e para VR em 26%. Não houve identificação etiológica em 35% e em 5% houve codetecção de VR e BP. Todos os pacientes apresentaram características demográficas semelhantes. A presença de tosse seguida de guincho inspiratório ou cianose foi um forte preditor de coqueluche, assim como, leucocitose e linfocitose evidentes. Coriza e dispneia foram mais frequentes nas infecções virais. Houve suspensão do uso de macrolídeos em 40% dos pacientes com pesquisa positiva para VR e negativa para BP.
Conclusãoos resultados sugerem que lactentes hospitalizados com suspeita de coqueluche podem apresentar infecção viral e a pesquisa etiológica pode possibilitar a redução do uso de macrolídeos em alguns casos. No entanto, salienta-se que o diagnóstico etiológico de infecção por vírus respiratórios, por si só, não exclui a possibilidade de infecção por Bordetella pertussis.
Acute respiratory infections are prevalent in pediatric patients, particularly in infants.1 The clinical manifestations depend on the etiological agent, patient-related factors, and environmental interactions.1,2 Often, the etiological diagnosis of respiratory infections in infants cannot be based on clinical parameters, as symptoms caused by different microorganisms may be similar.2
Pertussis is an acute respiratory disease caused by Bordetella pertussis (BP), whose clinical presentation, unlike other respiratory infections, generally has characteristics that differentiate it from other etiologies. Most often, the diagnosis is made during the paroxysmal phase, when coughing spells occur, which may be accompanied by vomiting, cyanosis, and apnea lasting from one to six weeks.3,4 More severe clinical presentations are observed in young infants not yet fully immunized, in whom infections by respiratory viruses are frequent and constitute an important differential diagnosis in hospitalized patients.2
Identifying patients with respiratory virus (RV) infection among those with clinical suspicion of pertussis may contribute to minimize the use of macrolides, adjust measures to prevent in-hospital transmission of respiratory infections, and elucidate the impact of co-detection of BP and VR.2–4
The objectives of this study were to evaluate the frequency of RV infections in hospitalized infants with clinically suspected pertussis, and to analyze their characteristics at hospital admission and evolution during hospitalization.
MethodsA historical cohort study was conducted in the Division of Pediatric Clinic of the Hospital Universitário da Universidade de São Paulo (HU-USP), which during the study period was a pertussis surveillance service and had respiratory virus research as a routine procedure for all infants hospitalized with respiratory illness.
Infants admitted to the pediatric ward between April 2009 and June 2012, who were submitted to compulsory notification as “suspected” case of pertussis, according to the guidelines of the Department of Health of the State of São Paulo (which considers as “suspected cases” those who, regardless of vaccination status and age, present dry cough for at least two weeks accompanied by inspiratory stridor, paroxysmal cough, or vomiting after coughing), were included in the study.4
Patients were selected from the electronic database of the HU-USP. RV investigation was conducted by indirect immunofluorescence assay (IFA) in nasopharyngeal aspirates, collected during the first 24hours of hospitalization. For this laboratory test, a standardized kit (Biotrin International Ltd. – Dublin, Ireland) was used for the identification of seven respiratory viruses (RSV, Adenovirus, Influenza A and B, and Parainfluenza 1, 2, and 3). The tests were performed at the clinical laboratory of the HU-USP. BP investigation was performed in a material obtained by nasopharyngeal swab using polymerase chain reaction (PCR) and culture in Regan-Lowe (RL) semisolid medium.
BP investigation was performed at the Laboratory of Immunology of Instituto Adolfo Lutz de São Paulo (IAL), as recommended by the “Manual of Laboratory Diagnosis, Instituto Adolfo Lutz São Paulo”.5 The patients’ clinical and evolution data were collected from their medical files by completing the protocol, performed by one of the authors (AEF). Patients who had received macrolides during the two weeks prior to admission were excluded. The study was approved by the Research Ethics Committee of the HU-USP.
Statistical analysisContinuous variables were described as means and medians, and categorical variables were described as proportions. The chi-squared test was used for comparison of categorical variables. Interquartile ranges of continuous variables were evaluated, and the Kruskal-Wallis test was used for nonparametric statistical analysis when comparing values in both groups. Statistical significance was set at p < 0.05. Positive and negative predictive values were calculated for the diagnostic variables that presented statistical significance.
For sample size calculation, assuming a probability of alpha error of 5% and an 80% power of study, frequency of RSV among infants hospitalized due to acute respiratory disease was considered to be approximately 30%;6 among reported cases of suspected pertussis, the possibility of infection by respiratory viruses is not usually considered, being estimated at no more than 2%. Thus, considering a ratio of exposed/non-exposed individuals of 1.0, 52 subjects would be needed.
ResultsDuring the study period, 67 children with clinically suspected pertussis were hospitalized in the pediatric ward of the HU-USP. One patient was excluded for being on the fifth day of erythromycin at admission. There were nine losses (13.6% – one inconclusive PCR result, two transfers before discharge, three laboratory result misplacements, and three files were not located).
The medical records of 57 patients were completely analyzed. Of these, 25 (43.8%) were positive for BP investigation performed by PCR, and six of them, also, by culture in a specific medium. RV investigation was positive in 15 patients (26.3%). The following viruses were identified: respiratory syncytial virus (RSV) in 12 patients (21%), and Parainfluenza-3 in two patients; in one patient, adenovirus and Influenza-A were co-detected. There was co-detection of BP and RV in three patients (12% of patients with BP positive). No etiological agent was identified in 20 patients (35%).
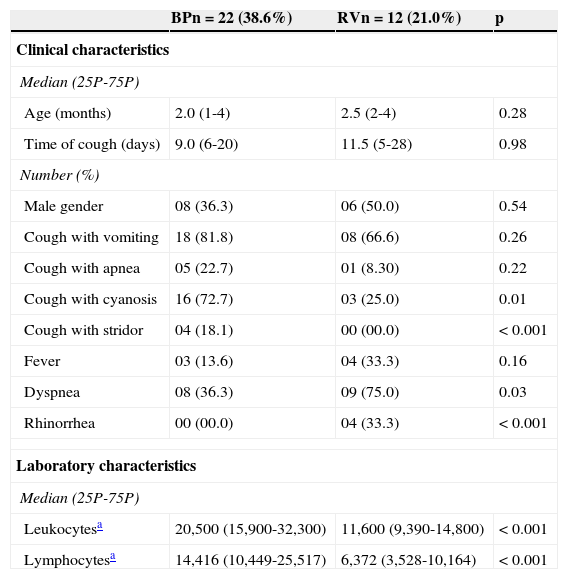
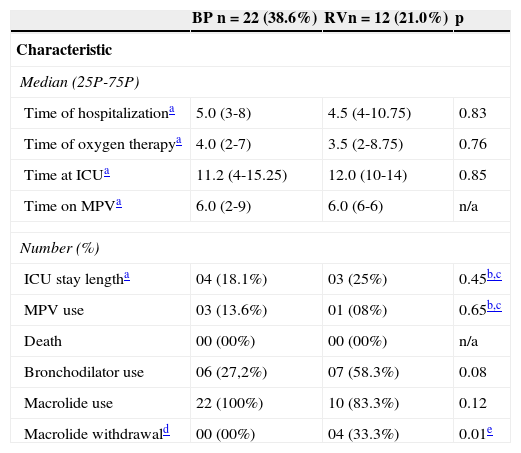
The clinical and laboratory characteristics on admission and evolution during hospitalization were compared between patients with positive BP and RV results as single agents, as shown respectively in Tables 1 and 2. Cough followed by inspiratory stridor and cough accompanied by cyanosis were significant predictors of pertussis (positive predictive values of 100% and 84%, respectively). Leukocyte count > 20,000 cells/mm3 and lymphocyte count > 10,000 cells/mm3 showed predictive values of 92% and 85%, respectively. However, these variables showed low negative predictive values for the diagnosis of pertussis (40%, 60%, 52% and 64%, respectively). Fifty-three patients (93%) received macrolides at admission. Macrolide withdrawal during hospitalization was more frequent in patients with positive results for viral testing and negative results for BP, as shown in Table 2.
Clinical and laboratory characteristics on admission of 34 patients with positive results for Bordetella pertussis and respiratory virus investigation, as single agents.
| BPn=22 (38.6%) | RVn=12 (21.0%) | p | |
|---|---|---|---|
| Clinical characteristics | |||
| Median (25P-75P) | |||
| Age (months) | 2.0 (1-4) | 2.5 (2-4) | 0.28 |
| Time of cough (days) | 9.0 (6-20) | 11.5 (5-28) | 0.98 |
| Number (%) | |||
| Male gender | 08 (36.3) | 06 (50.0) | 0.54 |
| Cough with vomiting | 18 (81.8) | 08 (66.6) | 0.26 |
| Cough with apnea | 05 (22.7) | 01 (8.30) | 0.22 |
| Cough with cyanosis | 16 (72.7) | 03 (25.0) | 0.01 |
| Cough with stridor | 04 (18.1) | 00 (00.0) | < 0.001 |
| Fever | 03 (13.6) | 04 (33.3) | 0.16 |
| Dyspnea | 08 (36.3) | 09 (75.0) | 0.03 |
| Rhinorrhea | 00 (00.0) | 04 (33.3) | < 0.001 |
| Laboratory characteristics | |||
| Median (25P-75P) | |||
| Leukocytesa | 20,500 (15,900-32,300) | 11,600 (9,390-14,800) | < 0.001 |
| Lymphocytesa | 14,416 (10,449-25,517) | 6,372 (3,528-10,164) | < 0.001 |
BP, Bordetella pertussis; RV, respiratory virus.
Evolution characteristics of the 34 patients with positive results for Bordetella pertussis and respiratory virus investigation as single agents.
| BP n=22 (38.6%) | RVn=12 (21.0%) | p | |
|---|---|---|---|
| Characteristic | |||
| Median (25P-75P) | |||
| Time of hospitalizationa | 5.0 (3-8) | 4.5 (4-10.75) | 0.83 |
| Time of oxygen therapya | 4.0 (2-7) | 3.5 (2-8.75) | 0.76 |
| Time at ICUa | 11.2 (4-15.25) | 12.0 (10-14) | 0.85 |
| Time on MPVa | 6.0 (2-9) | 6.0 (6-6) | n/a |
| Number (%) | |||
| ICU stay lengtha | 04 (18.1%) | 03 (25%) | 0.45b,c |
| MPV use | 03 (13.6%) | 01 (08%) | 0.65b,c |
| Death | 00 (00%) | 00 (00%) | n/a |
| Bronchodilator use | 06 (27,2%) | 07 (58.3%) | 0.08 |
| Macrolide use | 22 (100%) | 10 (83.3%) | 0.12 |
| Macrolide withdrawald | 00 (00%) | 04 (33.3%) | 0.01e |
BP, Bordetelle pertussis; ICU, intensive care unit; MPV, mechanical pulmonary ventilation; n/a, not applicable; RV, respiratory virus.
There was co-detection of BP and RV in three patients aged between 4 and 5 months and cough duration between one and ten days. All presented vomiting after coughing, and two of these patients had apnea and cyanosis. The identified viruses were RSV and Parainfluenza 3, and one patient had co-detection of adenovirus and Influenza A virus. Leukocytosis ranged from 16,000 to 86,000, and lymphocytosis ranged from 12,640 to 32,718. Two patients required admission to the intensive care unit and mechanical pulmonary ventilation. One of these patients died on the eighth day of hospitalization.
DiscussionRV infections were common in this cohort of infants with clinically suspected pertussis on admission. The routine investigation for RV enabled the reduction of the macrolide use in patients with viral infections.
The high frequency of RV infections in infants is observed worldwide. In the past decades, an increase in the occurrence of RV infections in European countries and the Americas has been reported. RSV is the most frequently identified agent in hospitalized infants, as observed in the present study.2,7,8 The co-circulation of BP and RVs during the viral season months emphasizes the importance of the differential diagnosis between the two respiratory tract infections.9,10
In the present study, the etiological confirmation of suspected cases (44%) was higher than that reported in the state of São Paulo in 2011 (29.2% of 1,540 suspected cases up to the 43rd epidemiological week).4 The molecular methods used have 90% sensitivity for the diagnosis of pertussis. The high rates of etiological confirmation possibly resulted from the use of these tests in a group of children stringently selected according to the clinical criteria for suspected pertussis. Infants analyzed in this study had paroxysmal cough and inspiratory stridor or vomiting after cough lasting 14 days or more, and were included regardless of their vaccination status.4,11
The results of this study suggest that the RV investigation was important in infants with suspected pertussis, especially those with less typical clinical presentation. Patients with etiological diagnosis of BP infection showed a prevalence of signs and symptoms of the disease, such as cough with inspiratory stridor and cyanosis, which had high positive predictive values for the diagnosis of pertussis. However, in less typical cases, the infection coursed with cough not accompanied by vomiting (18%), apnea (77%), cyanosis (30%), and inspiratory stridor (83%). These findings are consistent with the low negative predictive values of these clinical variables.
Conversely, in 21% of cases of suspected pertussis, RVs were detected as single agents. In these viral infections, the expected clinical characteristics were predominant, such as higher frequency of rhinorrhea (p < 0.001) and dyspnea (p = 0.03), and absence of inspiratory stridor (p < 0.001).
Similarly, the leucocyte count was useful in differentiating pertussis and RV cases; however, there were five children with leukocytosis < 10,000 cells/mm3 among those with diagnostic confirmation for BP. Leukocytosis up to 16,000 cells/mm3 were observed in the group of children with RV.
Similar to the results found in this study, infants hospitalized with a clinical diagnosis of pertussis are usually treated with macrolides, even before the etiological confirmation. Clinical suspicion justifies the use of this therapy, which reduces BP transmission time.4 This aspect is relevant, since pertussis is highly contagious and, although preventable by immunization, it represents a frequent cause of hospitalization in infants.3.4,12,13
Macrolide withdrawal in most children with RV infection without BP detection (40%) strongly suggests that the viral investigation outcome may have induced the review of clinical aspects and evolution of suspected pertussis cases, allowing for the reduction of antibiotic use. A similar impact was observed by the authors in a previous study that evaluated the influence of RSV investigation on antibiotic use in patients with a clinical diagnosis of bronchiolitis, which showed withdrawal in 32% of cases after viral test results.14
The present study has some limitations. The retrospective data collection from medical files can contain inaccuracies regarding clinical information, but objective parameters were analyzed in order to reduce the possibility of bias. All enrolled patients were evaluated for bacterial infection through blood cultures collected on admission, which has low sensitivity, but the absence of clinical relapses after discontinuation of antibiotics in patients with RV infections confirms the absence of bacterial coinfection.
The identified respiratory viruses followed the expected distribution, with predominance of RSV (80%), Parainfluenza (13%), and a case of adenovirus-Influenza A co-detection. Although the IFA method has a high sensitivity (approximately 90%) for RSV and Parainfluenza virus, and is thus used in routine practice, the non-performance of molecular methods for RV may have limited the diagnosis of infections by other respiratory viruses, such as rhinovirus and metapneumovirus. The use of these methods could reduce the number of children with undetermined etiology in this study (35%). Despite this limitation, the possibility of a greater number of identified viruses reinforces the main conclusion that it is necessary to consider respiratory viral infections, not just BP, in patients with suspected pertussis.15
It was not possible to assess the importance of BP and RV co-detection due to the limited number of cases. In the current literature, there is no evidence that co-detection has an impact on infection severity.16 Previous studies showed that the identification of BP in patients hospitalized with bronchiolitis did not alter the clinical course.8,10 However, patients with BP and RV co-detection reported in the present study had a severe outcome, one of whom died. In all three cases, there was a predominance of the clinical presentation characteristic of BP. Further studies are needed to elucidate this etiological aspect.
Conversely, the co-detection of BP and RV stresses the importance of investigating both etiologies, as the detection of the viral agent should not exclude the possibility of co-detection in cases with suspected pertussis.16 Studies that have analyzed the occurrence of BP infections in children with viral infections found co-detection of RSV and BP at higher rates than that of the present study.17,18 In infants younger than four months, Cosnes-Lambe et al. found a 16% co-detection rate.18 The co-detection rate of 5% observed in the present study is below that reported in the literature, which can be explained by the difference in design among the studies, as the present study investigated the viral etiology in children with suspected pertussis and the others analyzed a sample of children diagnosed with viral infections.
The results of the present study suggest that lower respiratory tract infections in infants hospitalized with suspected pertussis may have a viral etiology, and that etiological investigation may enable a reduction in macrolide use in some cases. However, it was observed that the etiological diagnosis of RV infection, by itself, does not exclude the possibility of infection by BP.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Ferronato AE, Gilio AE, Vieira SE. Respiratory viral infections in infants with clinically suspected pertussis. J Pediatr (Rio J). 2013;89:549–553.