To analyze the association between child exposure to intimate partner violence (CEIPV) committed against their mother and functional gastrointestinal disorders (FGIDs) in school-age children.
MethodsA prospective cohort study was carried out that evaluated 626 mother-child pairs living in a poor urban area in the Northeast of Brazil. The mothers were asked about their children's exposure to intimate partner violence. Holden's classification was used, which investigates ten types of CEIPV from prenatal care. The number of exposures, age of onset, and the perpetrator of the exposure were also verified. The FGIDs in children were identified from the mother's responses to the questionnaire about pediatric gastrointestinal symptoms, Roma III version parent-report, translated and cross-culturally adapted into Brazilian Portuguese.
ResultsFGIDs were more frequent among children exposed to violence than those not exposed (OR: 1.64; 95% CI: 1.04–2.58; p = 0.03). Likewise, in children who suffered four or more types of exposure (OR: 1.81; 95% CI: 1.10–2.96; p = 0.01), in which the exposure started in the first two years of life (OR: 1.93; 95% CI: 1.08–3.47; p = 0.02) and in those whose biological father was the perpetrator of the violence (OR; 1.62; 95% CI: 1, 05–2.48; p = 0.02).
ConclusionCorroborating the proposal of the biopsychosocial model, CEIPV increases the chance of occurrence of FGIDs in school-age children. Therefore, early identification and proposals for appropriate interventions are suggested both for the prevention of CEIPV and for the prevention and follow-up of FGIDs.
Functional gastrointestinal disorders (FGIDs) are a group of clinical entities diagnosed when the symptoms reported by patients are not related to organic disease.1 They are highly frequent worldwide among children and adolescents,2 with impacts on health and quality of life.3
Although the etiology and pathophysiology of FGIDs are not fully understood, there is consensus that they are complex phenomena resulting from the interaction of multiple factors - biological, psychological, and social - represented in the biopsychosocial model proposed by Drossman et al.4 In this model, it is proposed that the occurrence of traumatic events early in life could trigger a stressful situation that would influence the brain-gut interaction and the physiology of the digestive system: motility, sensitivity, immune dysfunction (leading to inflammation) and alteration in gut microbiota.4
When stress occurs in a prolonged, frequent, or intense way, it is called toxic stress, a condition that alters the functioning of the nervous, endocrine, and immune systems with several short-term and/or long-term health repercussions.5 Violence, as a stressful event, constitutes a risk factor for the manifestation of FGIDs,4–6 according to the biopsychosocial model proposed by Engel7 and adapted by Drossman.4
Among the traumatic events, also called adverse childhood experiences (ACE), the child's exposure to intimate partner violence (CEIPV) committed against their mother draws attention to the damage it can cause to the offspring. CEIPV is characterized as child maltreatment8 and often presents itself as a chronic situation.9 Intimate partner violence (IPV) is a worldwide problem with several consequences for the physical and mental health of women and their children,10 even if the child is not the target of violence.11
Despite the growing number of studies on CEIPV, researchers face the problem of the lack of uniform terms and definitions that cover all the diversity of experienced situations by children in the context of IPV.12 The terms 'witnesses', 'observers', and 'exposed' have been used as if they were synonymous. Some authors8,11 argue that the term “exposed” is more inclusive because it encompasses several types of experience and reveals exposure to violence as a much more complex construct than just seeing and hearing, as the most common forms cited in studies.13 Therefore, exposure includes all direct and indirect ways of experiencing violent events.
From this perspective and in an effort to create a taxonomy of children's exposure to IPV, Holden8 proposes a theoretical classification, which has been cited by some studies14–16 and includes direct and indirect exposures. Also points out that the violence that happens within homes is not a homogeneous phenomenon and highlights some dimensions: type of violence, nature of specific acts, the severity of injuries, timing or chronicity of violence, escalation, type of perpetrator, perpetrator's relation to the child, victim's role in the assault, and resolution when examining the impact of exposition.
Although FGIDs and CEIPV are frequent problems, few studies have analyzed the repercussions of CEIPV on physical health, especially the relationship between CEIPV and FGIDs.17–19 Hence arose the objective of analyzing the association between children's exposure to intimate partner violence and FGIDs in school-age children in a cohort study.
MethodsStudy design and populationA prospective cohort study was carried out with women enrolled in the Family Health Program of the Sanitary District II in the city of Recife, Northeastern Brazil. The target population of the study is mostly composed of low-income women.
In the first stage, 1120 pregnant women with at least 31 weeks of pregnancy were interviewed. In the second stage, 1057 women were interviewed again during the postpartum period. In the third stage, conducted between July 2013 and December 2014, 644 (61%) women were re-interviewed and answered questions about themselves, about CEIPV, and about symptoms suggestive of FGIDs when their children were of school age (6 to 9 years). In relation to the initial sample, 391 women were excluded due to a change of address, 17 did not want to continue in the survey and 5 had died. In addition, 18 mother-child pairs were lost: 4 children died, 2 were donated to other families, 2 did not live with their mother, 5 pairs of twins, and 5 without complete information in the questionnaire. Thus, the final sample analyzed had information reported by the mothers of 626 children. After analyzing characteristics such as age, race/skin color, marital status, education, and exposure to IPV, no statistically significant differences were found between the women who remained and those who left the study.20 All interviews were conducted by women researchers, with experience in research on IPV and violence against children, without the partner or any child aged two years and older being present.
VariablesChildren exposed to intimate partner violenceThe CEIPV was defined based on Holden's classification,8 which describes ten types of exposure, six of which were direct (prenatal exposure, seeing, hearing, intervening, participating, and being a victim) and four indirect (observing the initial effects, experiencing the consequences, listening to adult comments and apparently not knowing). The questionnaire used showed good internal consistency (α Cronbach = 0.81).
The mother reported the child's exposure to IPV. In addition to answering about the types of exposure, the mother was also asked if the child was exposed to IPV in the periods of 0–11 months of age, 1–2 years old, 3–5 years old, and ≥6 years old. For this study, the age of exposure was categorized as “no exposure”, “prenatal exposure” (the authors already had the data from the 1st stage), “0–2 years old” and “≥3 years old” (data collected in the third stage of the cohort). Answers about types of exposure were categorized into: “no exposure”, “1 to 3 types” and “four or more types”. The child, whose mother replied “yes” to at least one of the 10 types of exposure questioned, was considered exposed. In relation to the perpetrator of the exposure the categories used were: the child's biological father and another intimate partner of the mother (Supplementary material).
Functional gastrointestinal disordersThe dependent variable studied was the FGIDs, based on the set of symptoms presented by the children, considering the Roma III definitions and criteria.21 They were identified based on the mother's responses to the questionnaire about pediatric gastrointestinal symptoms, Roma III, version parent-report for children aged four and over, translated and cross-culturally adapted into Brazilian Portuguese. The diagnoses included in Roma III were investigated,21 with the exception of “adolescent rumination syndrome”, as it is a disorder that predominates in an age group not included in this study.
CovariablesThe general characteristics of the mother, partner, and child were verified. Regarding the mother and partner: age (<28 and ≥28 years); mother's marital status (with or without a partner); current or most recent partner being the child's biological father (yes or no). Concerning children: age (6–7 and 8–9 years); sex (male and female); the number of siblings (none, one to two and ≥ three siblings); a position of the child in the offspring (first or second position and ≥ third position).
Life habits and mental health variables were: use of alcohol by the mother and/or partner (yes or no); use of illicit drugs by the mother and/or partner (yes or no). The presence of maternal common mental disorders (yes or no) was investigated by the self reporting questionnaire (SRQ-20) and considered a case when the woman responded positively to eight or more questions, as validated in Brazil by Mari and Williams.22
Data collection procedureInterviews were carried out in a reserved place, guaranteeing the privacy and confidentiality of the answers, with written consent. In the first stage, the pregnant women were identified by community health agents and interviewed during the prenatal consultation. In the second stage, the women were contacted after scheduling the childcare consultation. When the women did not attend the consultations, the contact was made at home and the interviews were carried out in a place more convenient for the women. In the third stage, in order to locate the participants of the previous stages and to minimize losses in the follow-up of the cohort, the research team carried out an active search, based on information from family members, neighbors, and health professionals in the study area. They were interviewed about socioeconomic and demographic conditions, daily living habits, mental health, social support, and experiences of IPV. They also responded to a form on children's sociodemographic characteristics and exposure to IPV, in addition to the Questionnaire about Pediatric Gastrointestinal Symptoms, version parent-report, from Roma III.21 The women interviewed, regardless of the situation of violence, received a mini-guide containing information about support services for women and children who are victims of violence, available in the city of Recife. All steps were approved by the Research Ethics Committee of the Health Sciences Center of the Federal University of Pernambuco (report number 194.672 of 02/06/2013).
Statistical analysisStata version 13.0 for Windows was used in statistical analysis. Initially, the general characteristics of the sample were verified, estimating possible associations with the independent variable (CEIPV) and the dependent variable (FGIDs), using Pearson's chi-square test to identify possible confounding factors. The distribution of FGIDs between exposed and unexposed, their association with the different types of CEIPV, and their related characteristics (number of exposures, age of onset, and perpetrator of exposure) were identified. Finally, the associations that obtained a p < 0.10 were included in the multivariate analysis, using logistic regression, in order to estimate the association controlling for confounding variables. Crude and adjusted odds ratios (OR) were estimated, considering a confidence interval of 95% (95% CI) and p < 0.05.
ResultsTable 1 presents the general characteristics of the sample in relation to CEIPV and the occurrence of FGIDs. The CEIPV was more frequent in children whose mothers were ≤27 years old, without a partner, the partner was the child's father, and had common mental disorders; whose partners of mothers were aged ≤27 years old, had ≤9 years of schooling, and used illicit drugs; and both used alcohol. Furthermore, those women who had younger children and who studied in public schools. Only the child's age and the maternal common mental disorders were associated with FGIDs.
Family characteristics according to children's exposure to intimate partner violence and functional gastrointestinal disorders.
| Variables | Child exposure to intimate partner violence | Functional gastrointestinal disorders | |||||
|---|---|---|---|---|---|---|---|
| N = 626 | No | Yes | No | Yes | |||
| n (%) | n (%) | n (%) | p | n (%) | n (%) | p | |
| General characteristics of mothers | |||||||
| Age (years) | |||||||
| ≥28 | 544 (86.9) | 198 (36.4) | 346 (63.6) | 419 (77) | 125 (23) | ||
| ≤27 | 82 (13.1) | 15 (18.3) | 67 (81.7) | 0.002 | 69 (84.1) | 13 (15.9) | 0.15 |
| Schooling (years of schooling) | |||||||
| >9 | 316 (50.5) | 114 (36.1) | 202 (63.9) | 252 (79.7) | 64 (20.3) | ||
| ≤9 | 310 (49.5) | 99 (31.9) | 211(68.1) | 0.27 | 236 (76.1) | 74 (23.9) | 0.27 |
| Income | |||||||
| ≥1 minimum wage | 211 (33.7) | 66 (31.3) | 145 (68.7) | 163 (77.3) | 48 (22.7) | ||
| No income/<1 minimum wage | 415 (66.3) | 147(35.4) | 268 (64.6) | 0.30 | 325 (78.3) | 90 (21.7) | 0.76 |
| Marital status | |||||||
| Partner | 508 (81.1) | 190 (37.4) | 318 (62.6) | 401 (78.9) | 107 (21.1) | ||
| No partner | 118 (18.9) | 23 (19.5) | 95 (80.5) | <0.001 | 87 (73.7) | 31 (26.3) | 0.22 |
| Partner is father of child | |||||||
| Yes | 401 (64.1) | 183 (45.6) | 218 (54.4) | 311 (77.6) | 90 (22.4) | ||
| No | 225 (35.9) | 30 (13.3) | 195 (86.7) | <0.001 | 177 (78.7) | 48 (21.3) | 0.75 |
| General characteristics of partners | |||||||
| Age (years)a | |||||||
| ≥28 | 545 (89.9) | 200 (36.7) | 345 (63.3) | 420 (77.1) | 125 (22.9) | ||
| ≤27 | 61 (10.1) | 6 (8.8) | 55 (90.2) | <0.001 | 51 (83.6) | 10 (16.4) | 0.24 |
| Schooling (years of schooling)b | |||||||
| >9 | 283 (53.0) | 114 (40.3) | 169 (59.7) | 221 (78.1) | 62 (21.9) | ||
| ≤9 | 251 (47.0) | 69 (27.5) | 182 (72.5) | 0.002 | 193 (76.9) | 58 (23.1) | 0.74 |
| Incomec | |||||||
| ≥1 minimum wage | 398 (72.8) | 144 (36.2) | 254 (63.8) | 309 (77.6) | 89 (22.4) | ||
| No income/<1 minimum wage | 149 (27.2) | 53 (35.6) | 96 (64.4) | 0.89 | 121 (81.2) | 28 (18.8) | 0.36 |
| General characteristics of children | |||||||
| Age (years) | |||||||
| 8–9 | 320 (51.1) | 124 (38.8) | 196 (61.2) | 262 (81.9) | 58 (18.1) | ||
| 6–7 | 306 (48.9) | 89 (29.1) | 217 (70.9) | 0.01 | 226 (73.9) | 80 (26.1) | 0.01 |
| Sex | |||||||
| Male | 317 (50.6) | 109 (34.4) | 208 (65.6) | 243(76.7) | 74(23.3) | ||
| Female | 309 (49.4) | 104 (33.7) | 205 (66.3) | 0.84 | 245 (79.3) | 64 (20.7) | 0.42 |
| No. siblings | |||||||
| None | 132 (21.1) | 52 (39.4) | 80 (60.6) | 106 (80.3) | 26 (19.7) | ||
| 1 or 2 | 262 (41.8) | 95 (36.3) | 167 (63.7) | 194 (74.1) | 68 (25.9) | ||
| 3 or more | 232 (37.1) | 66 (28.5) | 166 (71.5) | 0.54 | 188 (81.0) | 44 (19.0) | 0.13 |
| Birth order | |||||||
| 1st or 2nd | 444 (70.9) | 153 (34.5) | 291 (65.5) | 346 (77.9) | 98 (22.1) | ||
| ≥3rd | 182 (29.1) | 60 (33.0) | 122 (67.0) | 0.72 | 142 (78.0) | 40(22.0) | 0.97 |
| School grade | |||||||
| ≥2nd grade | 401 (64.1) | 138 (34.4) | 263 (65.6) | 311 (77.6) | 90 (22.4) | ||
| Literacy/1st grade | 225 (35.9) | 75 (33.3) | 150 (66.7) | 0.78 | 177 (78.7) | 48 (21.3) | 0.74 |
| Type of schoold | |||||||
| Private | 298 (47.8) | 120 (40.3) | 178 (59.7) | 234(78.5) | 64 (21.5) | ||
| State | 326 (52.2) | 93 (28.5) | 233 (71.5) | 0.002 | 253 (77.6) | 73 (22.4) | 0.78 |
| Mother's lifestyle and mental health | |||||||
| Use of alcohol | |||||||
| No | 357(57.0) | 142 (39.8) | 215(60.2) | 269(75.3) | 88 (24.7) | ||
| Yes | 269(43.0) | 71 (26.4) | 198(73.6) | 0.001 | 219(81.4) | 50 (18.6) | 0.07 |
| Use of illicit drugs | |||||||
| No | 595(95.1) | 207(34.8) | 388(65.2) | 462(77.7) | 133(22.3) | ||
| Yes | 31 (4.9) | 6 (19.4) | 25 (80.6) | 0.08 | 26 (83.9) | 5 (16.1) | 0.41 |
| Common mental health disorder | |||||||
| No | 425(67.9) | 174(40.9) | 251(59.1) | 351(82.6) | 74 (17.4) | ||
| Yes | 201(32.1) | 39(19.4) | 162(80.6) | <0.001 | 137(68.2) | 64 (31.8) | <0.001 |
| Partner lifestyle | |||||||
| Use of alcohole | |||||||
| No | 208 (33.4) | 94 (45.2) | 114(54.8) | 160 (76.9) | 48 (23.1) | ||
| Yes | 414 (66.6) | 118(28.5) | 296(71.5) | <0.001 | 326 (78.7) | 88 (21.3) | 0.60 |
| Use of illicit drugsf | |||||||
| No | 567 (94.2) | 205(36.2) | 362(63.8) | 438 (77.2) | 129(22.8) | ||
| Yes | 35 (5.8) | 5 (14.3) | 30 (85.7) | 0.01 | 31 (88.6) | 4 (11.4) | 0.12 |
More than half of the children (66%) were exposed to IPV, while the frequency of FGIDs was 22%. Table 2 shows that most types of CEIPV have a statistically significant association with FGIDs, except in the categories: exposure in prenatal care, being a victim, and experiencing the consequences.
Distribution of types of child exposure to intimate partner violence, according to Holden's classification and association with functional gastrointestinal disorders.
| Functional gastrointestinal disorders | |||||||
|---|---|---|---|---|---|---|---|
| Variables | N = 626 | No | Yes | ||||
| n (%) | n (%) | n (%) | OR (CI 95%) | p | |||
| Exposed to IPV | |||||||
| No | 213(34) | 180 (84,5) | 33 (15,5) | 1 | 0,005 | ||
| Yes | 413 (66) | 308 (74,6) | 105 (25,4) | 1.85 (1,20–2.86) | |||
| Types of exposurea | |||||||
| Direct exposure | |||||||
| No | 342 (54.6) | 287 (83.9) | 55 (16.1) | 1 | |||
| Yes | 284 (45.4) | 201 (70.8) | 83 (29.2) | 2.15 (1.46–3.16) | <0.001 | ||
| Prenatal | |||||||
| No | 448 (71.6) | 356 (79.5) | 92 (20.5) | 1 | |||
| Yes | 178 (28.4) | 132 (74.2) | 46 (25.8) | 1.34(0.89–2.02) | 0.15 | ||
| Postnatal | Hearing | ||||||
| No | 369 (59.0) | 308 (83.5) | 61 (16.5) | 1 | |||
| Yes | 257(41.0) | 180 (70.0) | 77 (30.0) | 2.15(1.47–3.16) | <0.001 | ||
| Seeing | |||||||
| No | 410(65.5) | 337 (82.2) | 73 (17.8) | 1 | |||
| Yes | 216(34.5) | 151(69.9) | 65(30.1) | 1.98(1.35–2.92) | <0.001 | ||
| Intervening | |||||||
| No | 526(84.0) | 420 (79.8) | 106(20.2) | 1 | |||
| Yes | 100 (16) | 68(68.0) | 32 (32.0) | 1.86(1.16–2.98) | 0.01 | ||
| Participating | |||||||
| No | 607 (97.0) | 478 (78.7) | 129 (21.3) | 1 | |||
| Yes | 19 (3.0) | 10 (52.6) | 9 (47.4) | 3.33 (1.32–8.37) | 0.01 | ||
| Being victim | |||||||
| No | 541 (86.4) | 425 (78.6) | 116 (21.4) | 1 | |||
| Yes | 85 (13.6) | 63 (74.1) | 22(25.9) | 1.27 (0.75–2.16) | 0.35 | ||
| Indirect exposure | |||||||
| No | 321 (51.3) | 264 (82.2) | 57 (17.8) | 1 | |||
| Yes | 305 (48.7) | 224 (73.4) | 81 (26.6) | 1.67 (1.14–2.45) | 0.008 | ||
| Postnatal | Watch the initial effects | ||||||
| No | 466(74.4) | 378 (81.1) | 88 (18.9) | 1 | |||
| Yes | 160 (25.6) | 110(68.7) | 50 (31.3) | 1.95(1.29–2.93) | 0.001 | ||
| Experience consequences | |||||||
| No | 396 (63.3) | 315 (79.6) | 81 (20.4) | 1 | |||
| Yes | 230 (36.7) | 173(75.2) | 57 (24.8) | 1.28(0.87–1.88) | 0.20 | ||
| Listen to adult comments | |||||||
| No | 543 (86.7) | 431 (79.4) | 112 (20.6) | 1 | |||
| Yes | 83 (13.3) | 57 (68.7) | 26(31.3) | 1.75 (1.05–2.91) | 0.03 | ||
| Apparently unaware | |||||||
| No | 514 (82.1) | 413 (80.4) | 101 (19.6) | 1 | |||
| Yes | 112 (17.9) | 75 (67) | 37 (33) | 2.01(1.28–3.16) | 0.002 | ||
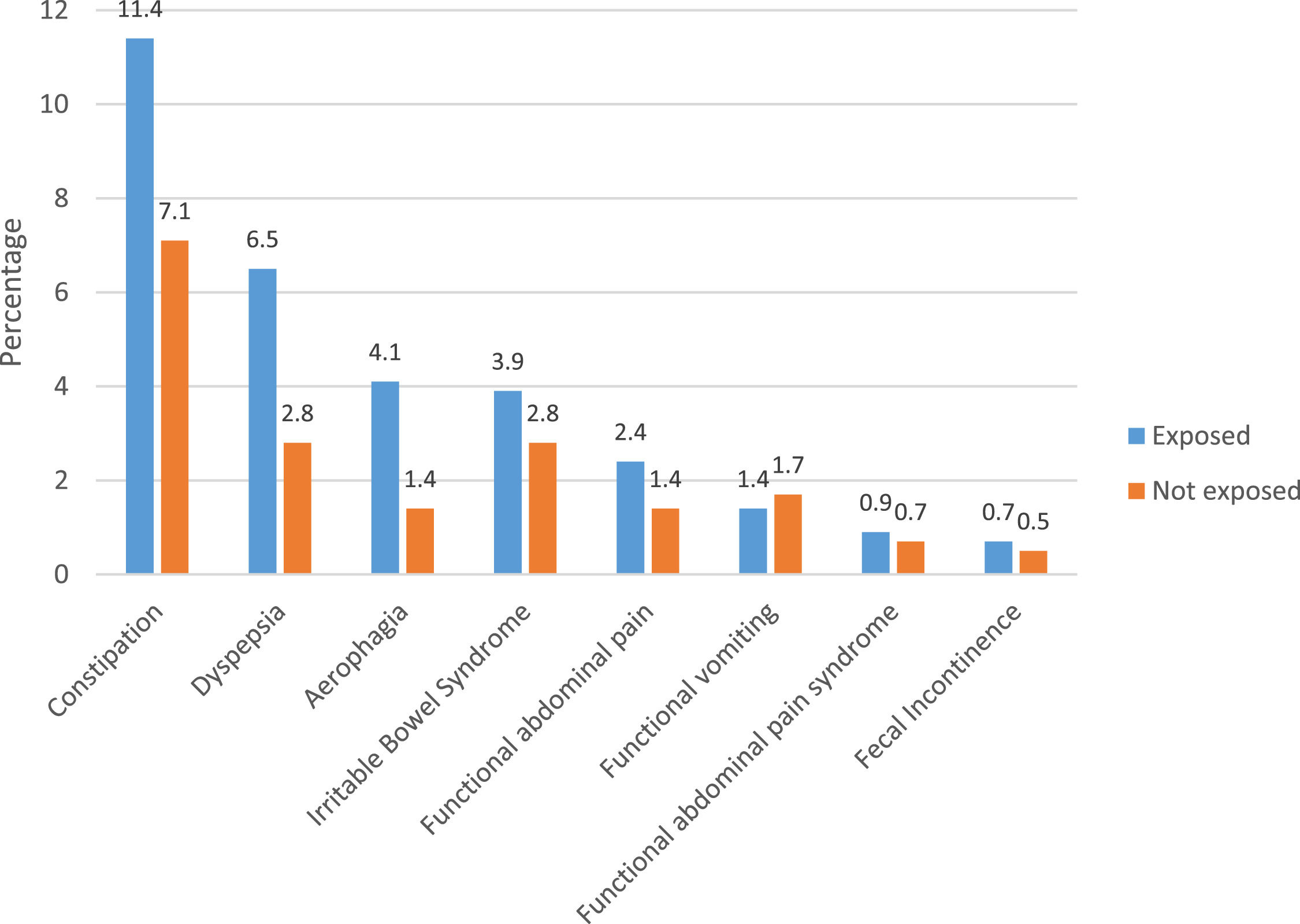
Analyzing each type of FGID separately, according to ROME III, with the exception of the category “cyclic vomiting”, higher frequencies of each disorder were identified when the child was exposed to IPV (Figure 1). No child met the criteria for abdominal migraine.
The multivariate analysis (Table 3) shows that, even after adjusting for confounding variables, CEIPV remained associated with FGIDs, increasing the chance of occurrence when the child was exposed to four or more types of IPV (OR = 1.81; 95% CI = 1.10–2.96), the exposure occurred in the first two years of life (OR = 1.93; 95% CI = 1.08–3.47) and IPV was perpetrated by the biological father of the child (OR = 1.62; 95% CI = 1.05–2.48).
Multivariate logistic analysis of the association between child exposure to intimate partner violence and functional gastrointestinal disorders.
| Functional gastrointestinal disorders (N = 626) | |||||
|---|---|---|---|---|---|
| Variables | N = 626n (%) | Non (%) | Yesn (%) | OR crude (CI95%) | OR adjusteda (CI 95%) |
| Children's exposure to intimate partner violence | |||||
| No | 213 (34.0) | 180 (84.5) | 33 (15.5) | 1 | 1 |
| Yes | 413 (66.0) | 308 (74.6) | 105(25.4) | 1.85(1.20–2.86) | 1.64 (1.04–2.58) |
| p | 0.005 | 0.03 | |||
| Number of exposure | |||||
| No exposure | 262 (41.8) | 219 (83.6) | 43 (16.4) | 1 | 1 |
| One to three types | 192 (30.7) | 149 (77.6) | 43 (22.4) | 1.46 (0.91–2.35) | 1.42 (0.87–2.31) |
| Four types or more | 172 (27.5) | 120 (69.8) | 52 (30.2) | 2.20(1.39–3.50) | 1.81 (1.10–2.96) |
| p | 0.003 | 0.01 | |||
| Exposure start age | |||||
| No exposure | 262(41.8) | 219 (83.6) | 43 (16.4) | 1 | 1 |
| Prenatal | 139 (22.2) | 100 (71.9) | 39 (28.1) | 1.98 (1.21–3.25) | 1.67 (0.99–2.82) |
| 0–2 years old | 88 (14.1) | 62 (70.5) | 26 (29.5) | 2.13 (1.21–3.75) | 1.93 (1.08–3.47) |
| ≥3 years old | 137 (21.9) | 107 (78.1) | 30 (21.9) | 1.42(0.84–2.40) | 1.33 (0.77–2.27) |
| p | 0.006 | 0.02 | |||
| Perpetrator of exposure | |||||
| No exposure | 262 (41.9) | 219 (83.6) | 43 (16.4) | 1 | 1 |
| Father | 338 (54.0) | 249 (73.7) | 89 (26.3) | 1.82 (1.21–2.73) | 1.62 (1.05–2.48) |
| Another partner | 26 (4.1) | 20 (76.9) | 6 (23.1) | 1.52 (0.57–4.02) | 1.29 (0.47–3.48) |
| p | 0.004 | 0.02 | |||
The results of this cohort show the distribution of FGIDs in a sample of children from a low-income community, exposed or not to IPV committed against their mother. The occurrence of CEIPV increased the chance of FGIDs, as identified in other international studies,17–19 even after controlling for confounding variables.
The greater chance of FGIDs when CEIPV started in the first two years of life, identified in the present study, corroborates the international literature that also shows harmful effects on the physical health of children exposed to violence early in life, despite verifying different ages from the one the authors analyzed.17–19 This occurrence can be explained due to the brain structures responsible for managing the stress response and emotional control are slow to develop early in life; therefore, the earlier the exposure, the more susceptible the child becomes to the damage caused by ACEs.23 Exposure to adversities in childhood increases the risk of health problems throughout life,17,18 due to the greater plasticity and vulnerability of the child's brain to environmental effects.5 CEIPV can also induce leading to the manifestation of diseases,23 as the FGIDs identified with high frequency in this study.
The frequency of FGIDs in the present study was similar to those identified in other South American countries,2 probably due to socioeconomic and cultural similarities linked to social inequality, which constitutes a risk factor for FDGIs.24 Practically all of them, according to the criteria established in ROME III,1 were more frequent among children exposed to IPV, similar to what was found in other studies with children who presented gastrointestinal symptoms, and whose mothers were also victims of IPV.17,18
According to Holden,8 children are likely to be exposed to different types of IPV, which was identified in this study. In this sense, the authors found the association of multiple exposures with FGIDs, highlighting the harmful consequences of the accumulation of adversities on the child's health25 and its role in the development of toxic stress with consequent effects on the digestive system,23 thus constituting a possible risk factor for the association with disorders found in this study.
Common mental disorders are frequent among them,26 a variable that, in this study, significantly increased the chance of FGIDs in children. In addition to this aspect, the mother's altered emotional state can be imitated by the child, leading to psychological changes capable of triggering symptoms suggestive of FGIDs.6
Exposure to IPV can change children's behavior, leading them to show reactions to confront violence, such as trying to intervene in order to stop the aggression16 or even to participate in situations of violence against the mother,27 as identified in the present study, whose situations increased the chances of FGIDs in the evaluated children. The child's participation in IPV may come from the fact that their coexistence in the violent environment leads to the naturalization and learning of aggression as something that is part of their daily life.25 Such situations require a level of skill not consistent with childhood, enhancing the child's level of stress, and even inducing the development of post-traumatic symptoms,27,28 which is also a risk factor for FGIDs.4 According to Carnevale et al.,27 the involvement of children participating in violence, especially as a result of the fear imposed by the perpetrator, or, on the other hand, by the coercion/encouragement by the perpetrator for the child to get involved in the aggressions, exposure that, in the present study, presented the greatest chance of occurrence of FGIDs.
In the context of IPV, the child is commonly considered an invisible victim.27 However, evidence of the consequences of CEIPV, even when they only see and/or hear the aggressions that occur in their home, shows that children are not passive to this experience,11 which was corroborated in this study.
On the other hand, the category “unknown apparently” was one of those with the highest chance of disorders. However, what mothers report may reflect a denial of knowledge or the illusion that children do not know about the situation of violence, or an underestimate of the magnitude of their children's exposure because they do not know where the children were or if they were sleeping in the moment of aggression.8
Regarding the association of the exposed child's age with the outcome, the authors analyzed schoolchildren, that is, all children were at the same stage of development, limiting the understanding of other variables that could be associated. There is evidence that younger children faced with a situation of violence have a lower capacity for self-regulation than older children due to less autonomy and degree of development.29 Furthermore, may develop a feeling of guilt due to their lower capacity for understanding,11 being, therefore, a possible source of greater stress, and consequently, increasing the chance of FGIDs.
The biological father's influence on the child's well-being is noticed when the authors evidence the association in the occurrence of FGIDs when he was the perpetrator. A possible explanation is that the stress levels of a child exposed to IPV perpetrated by the father may be higher due to the paternity being negatively affected, leading to an effectively insecure relationship.11,27 In addition, social support is an important element to establish resilience and mitigate the effects of toxic stress on the individual's health.23 In this situation of paternal involvement, this support may be weakened, contributing to the exacerbation of stress in the child. In summary, the present study found associations between most types of CEIPV with the occurrence of FGIDs, highlighting the impact of stress caused by violence on children's health.
This study has some advantages. One of them is that it is a population-based cohort, with the possibility of generalizing the results to a similar population. Another advantage was the use of Holden's classification,8 which consists of ten categories to investigate CEIPV, allowing the identification of various types of violence to which a child may have been exposed, since prenatal care. In general, studies cite that children saw or heard events of violence,13 perhaps because they are the easiest types to report; or only report that the child witnessed IPV,28 or analyze the repercussions for the child when the mother was exposed to IPV.30 However, there is a growing interest in expanding knowledge and systematizing the assessment of the child's exposure to IPV.13
Holden's classification (2003)8 contributes to this systematization. Population-based studies,14,31 with samples of 2184 and 49,953 children respectively, used some categories proposed by Holden. Qualitative studies have also cited this classification and used some of its categories.15,32 In a recent review Haselschwerdt, Savasuk-Luxton, and Hlavaty33 cite that: “Holden's taxonomy provides an excellent template to guide future studies”. The authors highlight that, until now, we did not identify any studies that evaluated Holden's ten categories, like ours, that is, no study has evaluated the CEIPV encompassing so many direct, indirect, active, and passive aspects of experiencing violent events.
Some limitations are also mentioned: the loss of participants from the first to the last stage, especially due to change of address, a common condition in low-income communities in Brazil; possible underestimation of data related to issues of violence, due to fear and/or embarrassment of victims in dealing with the matter; the CEIPV having been investigated only by the mothers' answers, which can lead to memory bias; there was no diagnostic confirmation of the FGIDs with medical evaluation, but based on the mothers' reports, which may have implications for memory or doubt in the answers. The explanatory model of FGIDs is complex and draws attention to the multicausality that can make it difficult to model studies by limiting the analysis of the various factors that may be involved in their occurrence, and possibly influencing the results found.
In addressing this, it is recommended that more research be carried out in order to increase the visibility of the problem and to provide knowledge to managers, researchers, and health professionals for early identification and proposals for appropriate interventions. It is also suggested that health professionals be trained to identify signs of exposure to violence in pregnant and non-pregnant women and children, as well as support them with conflict resolution strategies and security and empowerment measures. Professionals who work with children with FGIDs should also be aware of violence as a possible associated factor.