To evaluate the correlation between hemoglobin levels of mothers and their children on exclusive breastfeeding in the first six months of life.
MethodsCross-sectional study with 221 binomials (mother–child) enrolled in a breastfeeding support program, who were stratified into six groups according to the children's age group. The sample consisted of children born at term with normal weight, with no neonatal complications and whose mothers did not have anemia or infectious disease at the time of data collection. Interviews were carried out with the mothers, blood was collected by peripheral venipuncture from mothers and children, and children's anthropometric data were assessed. Pearson's correlation coefficients between the hemoglobin levels of mothers and children were calculated. Six multiple linear regression models were adjusted with regression coefficient estimates, considering as statistically significant associations with p≤0.05.
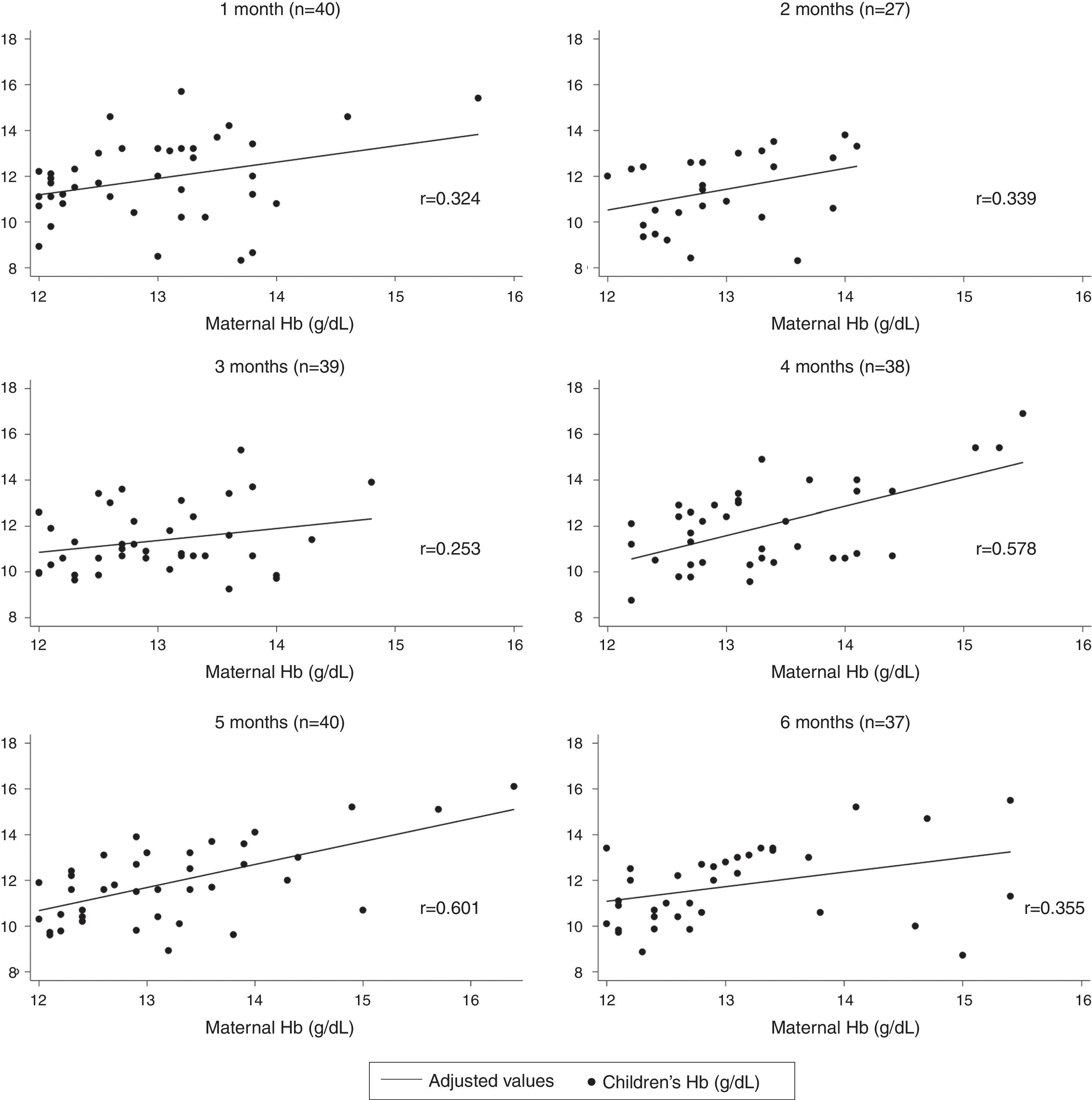
ResultsThe correlation coefficients of hemoglobin levels of mothers and children ranged from 0.253, at three months, to 0.601, at five months. The hemoglobin level of mothers was correlated with the hemoglobin level of their children at four months (r=0.578) and at five months (r=0.601). In the adjusted multiple linear regression, the regression coefficients were higher at four months (β=1.134; p=0.002) and at five months (β=0.845; p<0.001).
ConclusionThese findings allow for the conclusion that there is a correlation between the hemoglobin of mothers and the hemoglobin of their children on exclusive breastfeeding in the first six months of life.
Avaliar a correlação entre os níveis de hemoglobina de mães e de seus filhos em aleitamento materno exclusivo, no primeiro semestre de vida.
MétodosEstudo transversal com 221 binômios (mãe-filho) matriculados em programa de incentivo ao aleitamento materno, que foram estratificados em seis grupos de acordo com a faixa etária das crianças. A amostra consistiu de crianças nascidas a termo, com peso normal, sem intercorrências neonatais e cujas mães não apresentavam doença infecciosa e anemia na época da coleta de dados. Foram realizadas entrevistas com as mães, coleta de sangue por punção de veia periférica das mães e das crianças e antropometria das crianças. Foram calculados os coeficientes de correlação de Pearson entre os níveis de hemoglobina das mães e das crianças. Foram ajustados seis modelos de regressão linear múltiplos com estimativas de coeficientes de regressão, considerando-se estatisticamente significantes associações com p≤0,05.
ResultadosOs coeficientes de correlação dos níveis de hemoglobina das mães e das crianças variaram entre 0,253, aos três meses, e 0,601, aos cinco meses. O nível de hemoglobina das mães esteve mais correlacionado com o das crianças aos quatro meses (r=0,578) e aos cinco meses (r=0,601). Na regressão linear múltipla ajustada, os coeficientes de regressão foram maiores aos quatro meses (β=1,134; p=0,002) e aos cinco meses (β=0,845; p<0,001).
ConclusãoEsses achados permitem concluir que há correlação entre a hemoglobina de mães e a hemoglobina de seus filhos em aleitamento materno exclusivo no primeiro semestre de vida.
In the first year of life, iron-deficiency anemia is associated with psychomotor and cognitive development problems, which may be irreversible even after appropriate treatment.1 Therefore, knowledge of the risk factors, which may be already present in early life, is essential to support control and prevention strategies. In Brazil, the best estimates of the prevalence of anemia in infants and mothers are respectively 24.1% and 29.4%, highlighting the importance of the subject.2–4 Specifically, healthcare researchers have been discussing the influence of the nutritional status of maternal iron on the hemoglobin (Hb) levels of their children for several decades. As the concentrations of iron and lactoferrin in breast milk are needed to maintain body iron levels in the first months of life, maternal anemia could affect these concentrations in breast milk. However, two studies carried out by the same group of researchers in India, which evaluated the concentrations of iron and lactoferrin in anemic and nonanemic mothers’ milk who breastfed exclusively for the first six months of life, concluded that both iron and lactoferrin concentrations had no association with the mothers’ iron status.5,6
The results of studies that evaluated the association between anemia in infants and maternal anemia remain controversial. While some studies suggest no association,7–10 others show evidence that children born to anemic or iron-deficient mothers more frequently develop iron-deficiency anemia in the first year of life, when compared to children of non-anemic mothers.11–14 However, none of these studies investigated the influence of serum levels of maternal hemoglobin (Hb) on the children's Hb profile in a sample of exclusively breastfed infants, which affects the validity of their findings, as other sources of iron in the children's diets can be responsible for dissimilar findings, generating the controversy in the literature.
In this context, this study aimed to evaluate the correlation between Hb levels of mothers and their children on exclusive breastfeeding in the first six months of life.
MethodsThis was a cross-sectional study of the correlation between Hb levels of mothers and their children's Hb. Mothers and children were recruited from a primary health care unit in Belém (Brazil), from October 2006 to December 2008.
In this healthcare service, there is a care program for mothers and children that include regular consultations with a multidisciplinary team during the first six months of life. Its focus is on breastfeeding promotion and the effectiveness of childcare, so that mothers can successfully maintain exclusive breastfeeding in accordance with the recommendations of the Brazilian Ministry of Health, which follow the standards of the World Health Organization and the American Academy of Pediatrics.15,16
Initially, all infants enrolled in the unit who were near a full-month age (1, 2, 3, 4, 5, or 6 months) were considered. Thus, children were stratified into six groups according to age (age in months±5 days). Children whose age was out of this ten-day margin in the six strata were not included in the study.
In addition, the inclusion criteria comprised only infants who were exclusively breastfed from birth, born at term (gestational age between 37 and 42 weeks), who did not have low birth weight (birth weight<2500g), with no complications in the neonatal period and whose mothers had Hb levels<12g/dL at the time of data collection. Infants who had suspected infectious or inflammatory processes at the time of the blood sample collection (presence of morbid signs/symptoms and/or white blood cell count alterations) and the children of mothers who reported a history of malaria or had an infectious disease at the time of data collection were excluded.
The sample size was calculated based on the mean and standard deviation values of Hb from the pilot study conducted before the start of data collection. To meet the objective of the research, the estimate resulted in 40 children in each age group, considering a beta value=0.1 and bilateral alpha=0.05.
Children who received breast milk directly from the breast or expressed, or human milk from another source, with no other liquids or solids, with the exception of drops or syrups consisting of vitamins, oral rehydration salts, mineral supplements, or medications were considered to be on exclusive breastfeeding.16
Thus, 245 mothers whose children met the criteria for inclusion in the study were interviewed during the data collection. However, five children were excluded for presenting at least one of the exclusion criteria, resulting in 240 children. Later, 19 other children were excluded from the analysis due to insufficient material to carry out the laboratory tests, resulting in a sampling loss of 7.9%. Thus, the study included 221 binomials (mother–child), which were distributed in six groups according to age: 1 (n=40), 2 (n=27), 3 (n=39), 4 (n=38), 5 (n=40) and 6 (n=37) months. No binomial (mother–child) was included in more than one age group of the sample.
During the care activities provided to the selected children, the main investigator (RFVM) filled out, together with the mothers, a validated, structured, pre-coded questionnaire with information about the gestational history, delivery, and post-partum conditions, neonatal history, and the family's socioeconomic status.
The collection of blood samples from children and mothers were carried out after a medical consultation, through puncture of the radial or cubital peripheral vein on the anterior arm surface. The Cell-Dyn® 3.500 (ABBOTT, IL, USA) equipment was used for the determination of Hb concentration of mothers and children. Serum ferritin values were obtained by immunoenzymatic determination in serum or plasma using the enzyme linked fluorescent assay (ELFA) technique through the automated test VIDAS® Ferritin (Biomerieux, Paris, France) which allows the quantitative measurement of ferritin in serum or plasma.
Children were weighed in a pediatric scale certified by the National Institute of Metrology, Quality, and Technology (Instituto Nacional de Metrologia, Qualidade e Tecnologia [INMETRO]) with a maximum capacity of 16kg. An anthropometric ruler with a movable cursor was used to measure height. The anthropometric procedures used in the study were those recommended by the Ministry of Health.17
The anthropometric indicator chosen for nutritional assessment was the weight for age ratio and the criteria used to express it was the Z-score.18 The difference in the Z-score of the weight for age ratio between the time of data collection and the birth of the child was defined as the proportional weight gain indicator.19
Completed questionnaires were evaluated regarding their internal consistency. The information was transferred to databases with double entry and subsequently validated in order to correct input errors. The statistical package used was SPSS (SPSS Inc. Released 2007. SPSS for Windows, Version 16.0, IL, USA).20
Consistency analyses and univariate and bivariate descriptive statistics were performed. Analysis of variance (ANOVA) was used to compare means, and Pearson's correlation coefficients were calculated to quantify the correlation between Hb levels of mothers and children in the six age groups.21
For the control of confounding variables in the correlation between mothers’ Hb and children's Hb, a multiple linear regression model was adjusted with regression coefficient estimates.22
The criteria for the selection of control variables for the final model considered the situations with plausible effect on maternal Hb level (age, iron use at the time of data collection, and time of iron use during pregnancy) and Hb of children (weight gain, serum ferritin level, and gender). A maximum level of 0.05 was considered as a statistically significant association.
The study was approved by the Research Ethics Committee of the Escola Paulista de Medicina/Universidade Federal de São Paulo (UNIFESP/EPM) and authorized by the Health Unit of Belém do Pará. An informed consent form was signed by all mothers who agreed to participate in the study.
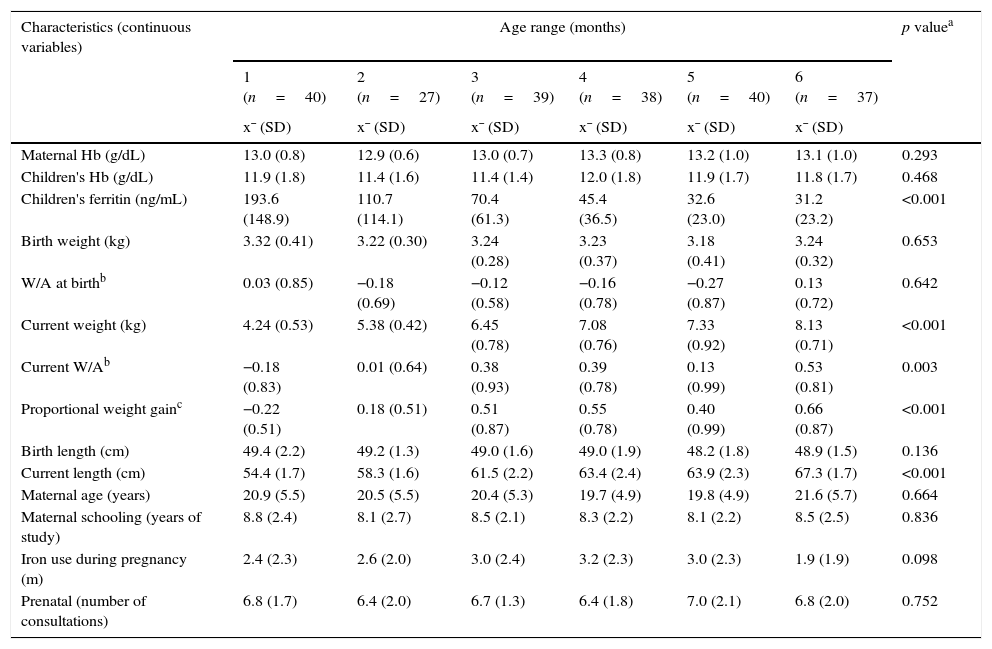
ResultsTable 1 shows the characteristics of the assessed mothers and children, according to the children's age groups. The mean Hb levels of mothers and children ranged, respectively, from 12.9 to 13.3g/dL and 11.4 to 12.0g/dL.
Comparison between the means with their respective standard deviations of the characteristics of mothers and children in exclusive breastfeeding, according to age group (2006–2008).
| Characteristics (continuous variables) | Age range (months) | p valuea | |||||
|---|---|---|---|---|---|---|---|
| 1 (n=40) | 2 (n=27) | 3 (n=39) | 4 (n=38) | 5 (n=40) | 6 (n=37) | ||
| x¯ (SD) | x¯ (SD) | x¯ (SD) | x¯ (SD) | x¯ (SD) | x¯ (SD) | ||
| Maternal Hb (g/dL) | 13.0 (0.8) | 12.9 (0.6) | 13.0 (0.7) | 13.3 (0.8) | 13.2 (1.0) | 13.1 (1.0) | 0.293 |
| Children's Hb (g/dL) | 11.9 (1.8) | 11.4 (1.6) | 11.4 (1.4) | 12.0 (1.8) | 11.9 (1.7) | 11.8 (1.7) | 0.468 |
| Children's ferritin (ng/mL) | 193.6 (148.9) | 110.7 (114.1) | 70.4 (61.3) | 45.4 (36.5) | 32.6 (23.0) | 31.2 (23.2) | <0.001 |
| Birth weight (kg) | 3.32 (0.41) | 3.22 (0.30) | 3.24 (0.28) | 3.23 (0.37) | 3.18 (0.41) | 3.24 (0.32) | 0.653 |
| W/A at birthb | 0.03 (0.85) | −0.18 (0.69) | −0.12 (0.58) | −0.16 (0.78) | −0.27 (0.87) | 0.13 (0.72) | 0.642 |
| Current weight (kg) | 4.24 (0.53) | 5.38 (0.42) | 6.45 (0.78) | 7.08 (0.76) | 7.33 (0.92) | 8.13 (0.71) | <0.001 |
| Current W/Ab | −0.18 (0.83) | 0.01 (0.64) | 0.38 (0.93) | 0.39 (0.78) | 0.13 (0.99) | 0.53 (0.81) | 0.003 |
| Proportional weight gainc | −0.22 (0.51) | 0.18 (0.51) | 0.51 (0.87) | 0.55 (0.78) | 0.40 (0.99) | 0.66 (0.87) | <0.001 |
| Birth length (cm) | 49.4 (2.2) | 49.2 (1.3) | 49.0 (1.6) | 49.0 (1.9) | 48.2 (1.8) | 48.9 (1.5) | 0.136 |
| Current length (cm) | 54.4 (1.7) | 58.3 (1.6) | 61.5 (2.2) | 63.4 (2.4) | 63.9 (2.3) | 67.3 (1.7) | <0.001 |
| Maternal age (years) | 20.9 (5.5) | 20.5 (5.5) | 20.4 (5.3) | 19.7 (4.9) | 19.8 (4.9) | 21.6 (5.7) | 0.664 |
| Maternal schooling (years of study) | 8.8 (2.4) | 8.1 (2.7) | 8.5 (2.1) | 8.3 (2.2) | 8.1 (2.2) | 8.5 (2.5) | 0.836 |
| Iron use during pregnancy (m) | 2.4 (2.3) | 2.6 (2.0) | 3.0 (2.4) | 3.2 (2.3) | 3.0 (2.3) | 1.9 (1.9) | 0.098 |
| Prenatal (number of consultations) | 6.8 (1.7) | 6.4 (2.0) | 6.7 (1.3) | 6.4 (1.8) | 7.0 (2.1) | 6.8 (2.0) | 0.752 |
x¯, mean; SD, standard deviation; Hb, hemoglobin; g/dL, gram per deciliter; ng/mL, nanogram per milliliter; kg, kilogram; cm, centimeter; m, months; W/A, weight for age ratio.
In the six age groups assessed, comparisons of the mean serum ferritin level (p<0.001) and the proportional weight gain (p<0.001) showed statistically significant differences between the age groups. Conversely, the characteristics of mothers and children, not entirely sensitive to the age difference (weight and length at birth, maternal age and education, iron use during pregnancy, and number of prenatal visits), were statistically similar (p>0.05).
Fig. 1 presents Pearson's correlation coefficients between Hb levels (g/dL) of mothers and children in each age group. The coefficients ranged from 0.253 at the age of 3 months to 0.601, at the age of 5 months. It can be observed that the Hb level of mothers was better correlated with the Hb of children at the age groups of 4 months (r=0.578) and 5 months (r=0.601).
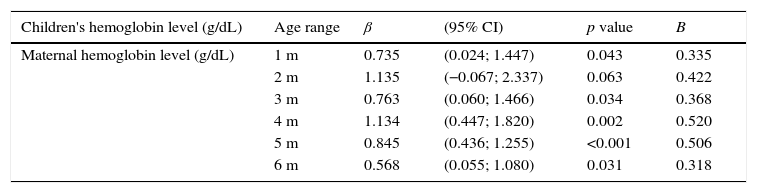
A multiple linear regression model was adjusted to each of the six age groups (Table 2). The regression coefficients were higher at the age groups of 4 months (β=1.134) and 5 months (β=0.845), meaning that for each increase of 1g/dLin maternal Hb, there was an estimated increase of approximately 1.1–0.8g/dL Hb in the children at these two age groups, respectively. These estimates were controlled in the models for three maternal variables (age, iron use at the time data collection, and time of iron use during pregnancy) and three variables of the children (weight gain, serum ferritin level, and gender).
Linear regression models between hemoglobin levels of mothers and children, according to the age range (2006–2008).
| Children's hemoglobin level (g/dL) | Age range | β | (95% CI) | p value | B |
|---|---|---|---|---|---|
| Maternal hemoglobin level (g/dL) | 1 m | 0.735 | (0.024; 1.447) | 0.043 | 0.335 |
| 2 m | 1.135 | (−0.067; 2.337) | 0.063 | 0.422 | |
| 3 m | 0.763 | (0.060; 1.466) | 0.034 | 0.368 | |
| 4 m | 1.134 | (0.447; 1.820) | 0.002 | 0.520 | |
| 5 m | 0.845 | (0.436; 1.255) | <0.001 | 0.506 | |
| 6 m | 0.568 | (0.055; 1.080) | 0.031 | 0.318 |
β, coefficient of regression; CI, confidence interval; B, standardized beta coefficient; m, month.
Models adjusted for maternal age, time of iron use during pregnancy, iron use at the time of data collection, weight gain, children's ferritin level, and gender.
The mean Hb levels of mothers and Hb and birth weight of the children in the six age groups were greater than 12.5g/dL, 11.0g/dL, and 3.0kg, respectively. Lower mean serum ferritin levels were observed month to month, from the first to the sixth month, and the distributions of Z scores of W/A ratio at birth and at the time of data collection were normal.
The highest correlation coefficients between Hb levels of mothers and children occurred in the age groups of 4 and 5 months. The six linear regression models resulted in positive regression coefficients and a statistically significant association at ages 1, 3, 4, 5, and 6 months, regardless of three characteristics of mothers (age and iron supplementation during pregnancy and at the time of data collection) and three characteristics of the children (weight gain, serum ferritin level, and gender).
There is no evidence in the literature of the association between maternal hemoglobin levels and those of their children after birth in humans. Findings from animal studies have contributed, to a limited extent, to the understanding of this association in humans, as the growth rate in experimental animals is significantly higher when compared to humans (i.e., in the first four weeks of life, a rabbit increases six times their body weight, while a human increases only a sixth of their birth weight in the same period). Furthermore, the proportion between the weight of the offspring and maternal weight is also much higher in experimental animals when compared with humans (e.g., ratio of 1:6 in rats and 1:16 in humans).7
A study in humans that evaluated iron concentrations in breast milk showed a decrease in mean iron levels during the duration of lactation from 0.6 to 0.3mg/L, but with great variability among the values, which potentially reflects the multifactorial nature of determining iron deficiency and its concentration in breast milk.23 In fact, Kumar et al.24 found lower iron levels in the breast milk of mothers with severe anemia, when compared to nonanemic mothers’ milk. However, the magnitude of the effect was approximately 2.6mmol/L, that is, a mean reduction of only 17% in iron concentration, which potentially does not result in differences in the iron status of their children.
Domellof et al.,25 when assessing breast milk samples collected from 191 mothers at nine months postpartum, found no association between levels of zinc, copper, and iron (hemoglobin, plasma ferritin, transferrin receptors, and zinc protoporphyrin) and the levels of these micronutrients in the mother's milk.
Even though there may be an association between Hb of mothers and children in the first months of life,13 the type of infant feeding, particularly exclusive breastfeeding, has been poorly considered in the analysis of the results of existing studies. The study by Kilbride et al.,12 which longitudinally evaluated children in the first 12 months of life and considered feeding practices in this period, found exclusive breastfeeding duration of only 2.3 months, which affects the interpretation of the findings as it does not constitute the ideal setting of the young infant nutrition.
The present study found a statistically significant correlation between hemoglobin levels of mothers and children in five of the six age groups analyzed, showing that maternal Hb status, as an indicator of body iron availability, influences the Hb status of children in the first six months of life, even with adequate iron stores, acquired by newborns at term and normal weight in late pregnancy.
The age groups shown here presented homogeneity between the assessed characteristics, minimizing misinterpretations related to factors that are determinants of serum Hb levels. Additionally, the adjustment in the multivariate analysis of mothers and children, which potentially interferes with iron status, reinforces this influence and therefore highlights the importance of exclusive breastfeeding in the first six months of life, even in children with good iron stores at birth.
Hay et al.26 concluded that serum ferritin levels in cord blood could be a predictor of iron status in the first two years of life. Although the time of clamping and the iron status in the umbilical cord blood may influence the hemoglobin levels of children, the correlation between ferritin values in cord blood and those in the infant's mother has not been demonstrated.12,24,27,28
It is worth mentioning that the iron status in the umbilical cord blood and time of clamping were not considered in this study, as these data were not available and the evaluation started with hemoglobin and ferritin levels in the children's first month of life. This may have influenced the results shown here.
In turn, the exclusion of mothers and children with infectious diseases during the data collection period ruled out the possibility that these conditions could interfere with the results. Although C-reactive protein was not measured, the mothers were asked about the presence of recent infections, and abnormalities in the levels of circulating leukocytes were verified.
Particularly, the exclusion of subjects with a history of malaria from the sample, as the present study was performed in an endemic area of the disease, prevented the influence of this infection on Hb levels, which has been demonstrated in women and infants.14
This study evaluated only mothers without anemia and their children on exclusive breastfeeding in the first six months of life, controlling, during the sample selection process, the effects of maternal anemia and different children's diets on the correlation between Hb levels of mothers and of their children. This inferential characteristic is unique in human studies.
It is noteworthy that the six age groups assessed here consisted of different binomials (mother–child), and follow-up was not conducted, but rather a separate assessment of six different age groups according to the adopted study design (cross-sectional). Even if the groups had similar characteristics, a longitudinal study would be closer to the ideal methodology to achieve the goal proposed herein. However, it is less feasible due to the need to collect repeated blood samples from healthy children and mothers, which is surely more uncomfortable and, consequently, results in sample loss.
In this context, regardless of the multifactorial nature of anemia assessment in childhood, the present findings indicate that there is a correlation between the mother's Hb levels and their children's on exclusive breastfeeding in the first six months of life. Despite the originality and methodological strength of this research, additional follow-up and ideally controlled studies appear to be necessary in order to confirm the results found here.
Finally, the authors recommend the adoption of three strategies to ensure the appropriate level of body iron in early life: effective iron supplementation of pregnant women during prenatal care, timely cord clamping (at least 1min after birth), and continuous support of exclusive breastfeeding in the first six months of life, which, combined with the good care at birth, provides the child enough iron quantity and quality to meet the demands of physical growth.24,29
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank the mothers who participated in the study, the Exclusive Breastfeeding Support Program team (Programa de Apoioao Aleitamento Materno Exclusivo [PROAME]) and those responsible for the Specialized Maternal-Child Reference Unit of the Department of Public Health of Pará (UREMIA-SESPA), where the study was performed.
Please cite this article as: Marques RF, Taddei JA, Konstantyner T, Marques AC, Braga JA. Correlation between hemoglobin levels of mothers and children on exclusive breastfeeding in the first six months of life. J Pediatr (Rio J). 2016;92:479–85.
Study conducted at the Department of Pediatrics, Escola Paulista de Medicina (EPM), Universidade Federal de São Paulo (UNIFESP), São Paulo, SP, Brazil.