In this systematic review (SR), the authors aimed to identify the possible impact of the social restriction imposed by the Coronavirus Disease-19 (COVID-19) pandemic on children/adolescents with Attention Deficit Hyperactivity Disorder (ADHD).
Data sourcesThis SR was registered on PROSPERO CRD42021255569. Eligible articles were selected from PubMed, Embase, and LILACS, according to the following characteristics: ADHD patients < 18 years old, exposed to the COVID-19 pandemic, and the outcomes, medications, relationships, sleep, media use, remote learning, and comorbidities such as depression/sadness, inattention, anxiety, and irritability/aggressiveness. Newcastle-Ottawa Scale (NOS) for cohort, cross-sectional and case-control studies was used to assess methodological quality and the risk of bias.
Summary of findingsOf the 222 articles identified, 27 were included, with information on 7,235 patients. Most studies (n = 22) were cross-sectional and received a mean NOS 4.63/10 followed by longitudinal (n = 4) with 3.75/8 points and case-control (n = 1), with 3/9 points. The pandemic affected patients’ access to treatment, behavior, and sleep. Difficulties in remote learning and increased use of social media were described, as well as significant and positive changes in relationships with family and peers.
ConclusionAlthough the studies were heterogeneous, they indicated that the pandemic-related issues experienced by patients with ADHD were mostly manifested affecting their behavior and sleep patterns.
The spread of the SARS-CoV-2 virus impacted the whole world leading to a pandemic named COVID-19, recognized by the World Health Organization on 11th March 2020.1 Social distancing, confinement, quarantine, and lockdown were among the measures implemented with the purpose of protecting the population from virus contamination.2 Although these measures were necessary, they have impacted lifestyle, habits, physical and mental health.3
Attention Deficit Hyperactivity Disorder (ADHD) is one of the most common behavioral disorders in childhood,4 with a prevalence of 2.2% worldwide among children and adolescents (up to 18 years old),5 and affecting more males than females.6,7 This neurodevelopmental disorder is characterized by a persistent pattern of inattention, disorganization, and/or hyperactivity-impulsivity that impacts the patient's life,8,9 interfering with their development8 and causing a direct negative impact on the patient's academic, occupational, or social functioning.9 Among the comorbidities associated with ADHD are the development of anxiety disorders, bipolar disorder, major depressive disorder, and substance-use disorders during lifetime.10
Previous studies have pointed toward the impact of environmental changes on children and adolescents with ADHD, showing that their symptomatology may relatively vary according to context dependency.11,12 Considering the pandemic, in general, children had milder forms of the COVID-19 disease,13 however, patients with ADHD were significantly more vulnerable to restrictions and measures of social distancing, showing consequences in their behavior.14
In this sense, the aim of this systematic review (SR) was to identify the potential impact of the social restriction imposed by the pandemic on children and adolescents with ADHD. Particularly, the authors aimed to identify whether there have been changes regarding the following domains, behavior, relationship with family and peers, sleep, inattention, and comorbidities such as anxiety, depression/sadness, irritability/aggressiveness. The hypothesis developed is that the pandemic, especially due to social isolation, worsened behavioral issues, ADHD symptoms, comorbidities, patients’ relationships, and sleep habits.
MethodsThis SR was performed following the Cochrane Handbook for Systematic Reviews (https://training.cochrane.org/handbook) and reported according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline. The review protocol is registered in the PROSPERO database (CRD42021255569).
Search strategyEligible articles were selected from PubMed, Embase, and Lilacs databases. The following PECO (Patient, Exposure, Comparison, Outcome) framework was implemented (1) Patient: children and adolescents with ADHD; (2) Exposure: COVID-19 pandemic; (3) Comparison: none; (4) Outcome: behavior, depression/sadness, inattention, anxiety, irritability/aggressiveness, relationships, and sleep. The outcomes selected were based on previous literature reports and on the domains affected by ADHD as reported in the Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM V).8 Exclusion criteria were, case series and case reports, paper reviews, debates, editorials, letters to the editor, experts' opinions, posters, meetings, seminars, and studies that did not respond to the PECO framework. Filters added to the search strategy were, language: English, Portuguese, and Spanish, and publication date: since December 2019.
The databases were queried as follows. Pubmed: ((“covid 19”[All Fields] OR “sars cov 2”[All Fields]) AND ((“English”[Language] OR “Portuguese”[Language] OR “Spanish”[Language]) AND (“infant”[MeSH Terms] OR “child”[MeSH Terms] OR “adolescent”[MeSH Terms])) AND “attention deficit disorder with hyperactivity”[All Fields]) AND ((english[Filter] OR portuguese[Filter] OR spanish[Filter]) AND (allchild[Filter])); Embase: 'attention deficit disorder' AND ('severe acute respiratory syndrome coronavirus 2′ OR 'coronavirus disease 2019′) AND ([adolescent]/lim OR [child]/lim OR [infant]/lim OR [preschool]/lim OR [school]/lim)); and, LILACS: (attention deficit disorder with hyperactivity) AND (severe acute respiratory syndrome coronavirus 2) OR (coronavirus disease 2019) AND (db:(“LILACS”) AND la:(“en” OR “es” OR “pt”)) AND (year_cluster:[2020 TO 2021]).
Screening and eligibilityAll articles resulting from the three database searches were imported into Rayyan (https:// rayyan.qcri.org). Searches were merged, and duplicates were selected by the software and excluded once the titles and authors were confirmed. In the second step, papers were screened based on their titles and abstracts. Any study that did not assess the consequences of the COVID-19 pandemic concerning children and adolescents with ADHD was excluded. In the third step, full-text articles were imported into the Mendeley bibliographic software package for full reading and data extraction. To maximize consistency, both selection phases were performed independently, by three pairs of two reviewers. Any disagreements about study inclusion or exclusion during this process were resolved in consensus discussions with a senior reviewer.
Data extractionThe same three pairs of reviewers extracted data from the included papers into an Excel spreadsheet. All extractions were discussed with a senior reviewer. The following data were extracted from every study: article characteristics (authors identification, publication year, journal name, DOI, title, objective, and study design); and, sample characteristics (sample size, gender, age, country of origin, comparison periods, and comparison between groups of participants, assessments performed and outcomes).
Methodological quality assessmentThe original version of the Newcastle-Ottawa Scale (NOS)15 for case-control studies and two adapted versions, for cross-sectional16 and longitudinal studies were used to assess the methodological quality and risk of bias of the included studies. The NOS for cross-sectional and longitudinal studies were adapted to our study needs, reaching a total of nine and eight stars each. The authors excluded the follow-up period since it is not known how long-term the patients with ADHD are expected to show differences in outcomes. The question concerning the adequacy of follow-up was graded according to sample loss. Studies were categorized as high quality when they met ≥ 90% of criteria, medium between 50 - 90%, and low when < 50%.17 The hypotheses were confirmed when articles with high- or medium-quality evidence showed worsened behavioral issues, ADHD symptoms, patients’ relationships, and/or sleep habits.
Variables studiedThe variables analyzed in this SR are related to the domains affected by ADHD, such as patients’ behavior (e.g., depression/sadness, inattention, anxiety, irritability/aggressiveness); relationship (e.g., family and peers); changes (e.g., sleep, medication treatment, media use, remote learning). Questions were dichotomic, multiple choices, or open-ended.
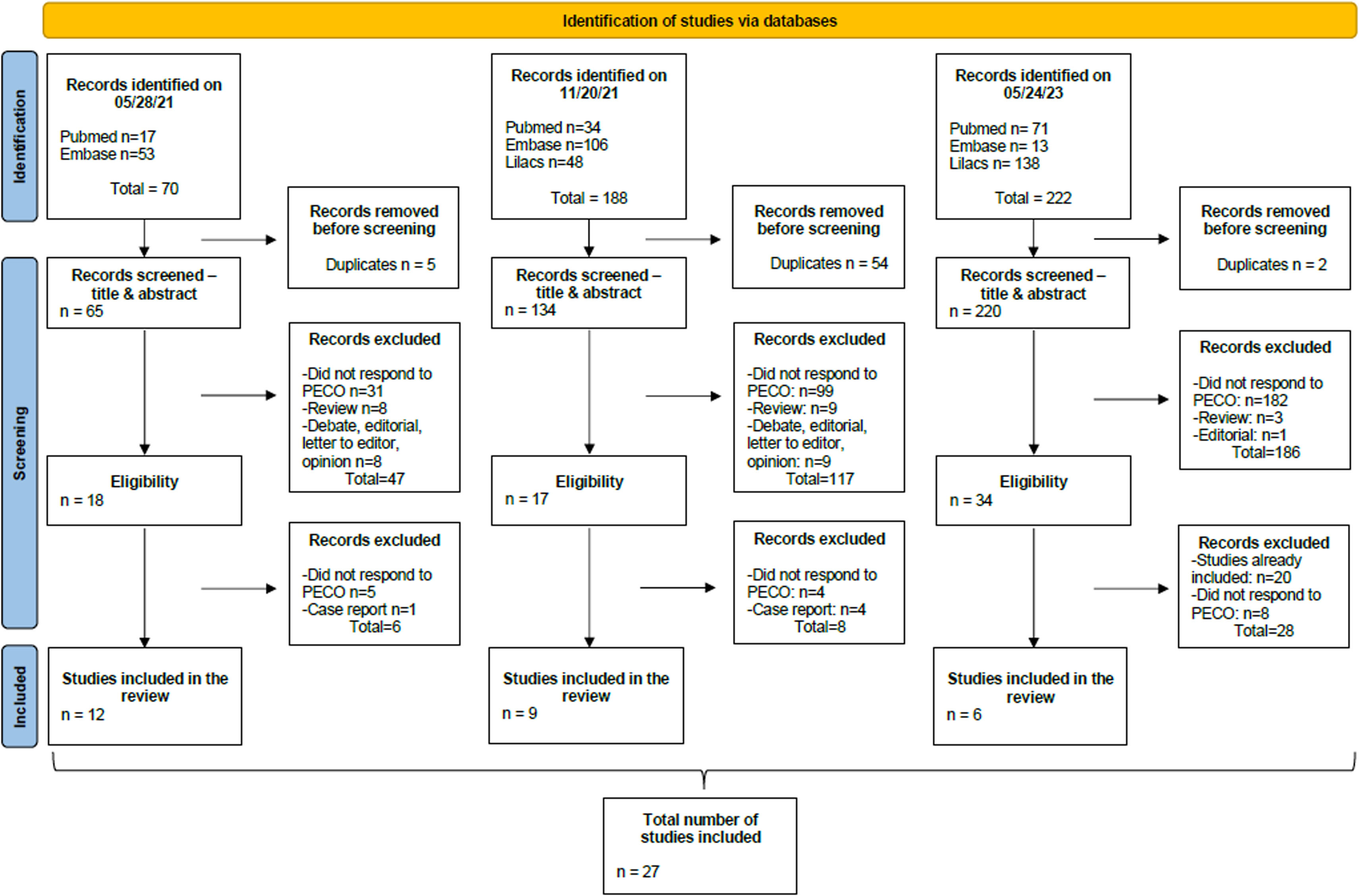
ResultsOur first search for papers was performed on PubMed and Embase databases in March 2021, where 70 studies were identified and 12 were included. A first update search made on December 2021, included the LILACS database. At this point, 9 articles of 188 observed were included. In May 2023, another update was performed, where a total of 222 papers were identified and 6 included. The total number of articles added to this SR was 27. The PRISMA flow chart below depicts the steps involved in the development of this SR (Figure 1).
Characteristics of studiesAll 27 articles included were published between 2020 and 2022. Twenty-two studies were cross-sectional, four longitudinal, and one case-control. According to NOS, 14 (52%) articles were low quality, and 13 (48%) were medium quality (see supplemental data).
Data from 7,235 patients with ADHD were analyzed, of whom 5477 (78%) were male - one study did not describe the gender. Six articles (28%) had a control group (n = 2640), of which 1027 (71%) were male - two studies did not describe gender among controls.
While one-third of articles (n: 8/27, 30%) addressed specifically the lockdown period during the COVID-19 pandemic,18-25 the other 70% (n: 19/27) compared the whole pandemic period.26-44 Only three papers did not compare before versus during lockdown 25 and before versus during the pandemic.43,44 General information from eligible papers is shown in Table 1.
The 27 eligible articles and data concerning the variables studied (behavioral issues, symptoms such as depression/sadness, inattention, anxiety, and irritability/aggressiveness) are presented in Table 2. The relationships with family and peers, sleep, medication treatment, media use, and remote learning, are described in Table 3.
General behavioral and symptomsOf the 27 articles added in this SR, 19 addressed behavioral issues of children and adolescents with ADHD.19-25,28,31,34,36-44 A medium level of evidence was reached in 10 papers and the hypothesis of worsening behavior was confirmed.20,25,31,34,36,37,40-43
In general, changes in behavior were significant when compared to before the pandemic28,31,34,36-42,44 or, specifically during lockdown period22-25 and were related to stress19,42 and school closure.21 During lockdown, a significant prevalence of stress-related behaviors (i.e. irritability/anger, COVID-19-fears) was observed.28
Concerning depression/sadness, 3 studies reached the medium quality of evidence, confirming the hypothesis of worsening of these symptoms.31,37,40 Depression during the pandemic was addressed by eight articles.22,27,28,31,37-40 A significant increase in depression was observed in the patients22,28,31,39 and in the controls.28 Regarding sadness, it was significantly associated with the COVID-19 pandemic in three studies.22,27,37
Inattention in children and adolescents with ADHD was addressed in 7 out of 27 papers.25,28,37,38,40,42,44 Medium level of evidence was observed in three papers, that confirmed the hypothesis of worsening in inattention.25,37,40,42 However, five out of seven papers found that inattention was better before the pandemic.28,37,38,40,42 Additionally, other studies observed that inattention was significantly associated with COVID-19 stress;37 it was significantly higher in patients than in controls;44 patients with problematic digital media use significantly worsened than those without it,38 and that significant cut-off on SNAP-IV was met for males when compared to females between 13 - 18 years.40
Nine studies addressed the subject anxiety,22,23,25,28,31,37,39,40,44 four of which reached a medium level of evidence and confirmed the hypothesis of anxiety worsening during the pandemic.25,31,37,40 Five articles described patients with lower symptoms of anxiety before the pandemic.25,28,31,37,40 A paper observed that 14.1% of children met the criteria for severe anxiety symptoms on the Generalized Anxiety Disorder test during the pandemic.40 Increased anxiety/nervousness was also significantly related to COVID-19 stress37 and had affected also controls.28
Twelve out of 27 articles approached irritability/aggressiveness.22-24,27,31,36,37,39,40,42-44 Six papers reached the medium quality of evidence31,36,37,40,42,43 but five addressed and confirmed the hypothesis of worsening of irritability/aggressiveness.31,36,37,40,42 Significant findings were observed and correlated the increase of irritability/aggressiveness with COVID-19 stress;43 more difficulties initiating and maintaining sleep and delayed sleep/wake behaviors;27 online distance learning for patients and controls (with more intensity in the first);44 and, finally, it was found to be significantly elevated in children with low and high ADHD degrees, and in adolescents of all ADHD degrees.22
Relationships with family and peersFive articles addressed relationship subjects during the pandemic,23,33,36,38,39 one of which reached the medium quality of evidence and confirmed the hypothesis of the relationship worsening 36. However, three papers indicated significant positive changes during the pandemic period.23,33,39 Papers also described an increase in home participation33 or in the time spent together with family.39 The authors observed that the reduction of cognitive and social demands associated with more readily available resources in the home environment had facilitated the positive changes observed.33
SleepEleven studies approached sleep during the pandemic.18,23,25,27,30,32,36,37,39,40,44 Of these, five had a medium quality of evidence and confirmed the hypothesis of worsening sleep habits.25,32,36,37,40 Four articles observed reduced sleep duration in patients with ADHD during the pandemic,18,27,30,40 which was associated with greater difficulty concentrating,27 greater hyperactivity/impulsivity and oppositional defiant disorder scores, depression, anxiety, and ADHD symptoms.40 Increased sleep difficulties were approached by three papers,18,27,30 in one there was an association with higher worry/afraid effect due to COVID-19.27
Use of medicationThe use of medication was investigated by seven papers,23,27,31,37,39,40 three of which reached a medium level of evidence.31,37,40 Two articles described that treatment was affected by the pandemic due to difficulties in accessing or purchasing and also due to medication being out of stock or difficulties in obtaining prescriptions.23,37 Modifications of dosage during the pandemic were evidenced in two studies,37,40 in one of which most patients needed increased dosage.37
Media useMedia use during the pandemic was approached by eleven articles,20,23,24,31,33,34,36-38,40,44 six reached medium quality of evidence.20,31,34,36,37,40 Six studies pointed toward an increase in the use of social media.20,24,31,34,37,38 One article associated an increase with COVID-19 stress which was also associated with a significant decrease in social media use in boys,37 while another observed higher social media time use in girls.24
An increase in video game use was observed,20,23,33,38,40,44 as well as in TV time.23,24,34,37,38 An increase in TV time use was significantly associated with COVID-19 stress37 while watching TV/playing videogames > 3.5 hours/day was significantly and positively correlated with reports of increased depression and mental health questionnaires total scores for depression, anxiety, inattention, and oppositional defiant disorder during the pandemic.40 The significant increase in total media time observed during the lockdown period (over 4h/day) significantly decreased after the easing of lockdown measures but remained significantly higher than pre-pandemic levels.24
Remote learningNine studies addressed remote learning23,26,29,31,35,36,38,39,44 and four reached medium quality of evidence.26,29,31,36 Patients’ difficulties with online learning were described only by four papers,26,36,39,44 one of these observed that remote learning difficulties were significantly higher for patients than controls even one year after the pandemic start.36 Difficulties in online learning were significantly associated with difficulties in concentrating because of COVID-19 in adolescents with ADHD, but not for their controls.26 Additionally, students with ADHD reported decreased grade point averages from 2019 - 2020 to 2020 - 2021 whereas controls did not.29 Two studies highlighted ADHD students’ performance.23,35 In the first, parents observed better performance in specific knowledge areas such as reading, writing, and mathematics,23 while in another the Wechsler Individual Achievement Test 3rd Edition (WIAT-III) was applied and a significant increase in scores for word, reading, and spelling subtests was observed.35
DiscussionIn this SR, the authors aimed to identify whether the social restriction imposed by the pandemic led to changes regarding domains such as behavior, inattention, comorbidities (depression/sadness, anxiety, and irritability/aggressiveness), relationship with family and peers, and sleep in children and adolescents with ADHD. The data obtained from the studies included in this review were heterogeneous and the results were often conflicting. All hypotheses raised in this work were supported, namely that the behavioral issues, depression/sadness, inattention, anxiety, irritability/aggressiveness, relationships, and sleep disturbances associated with ADHD worsened during the COVID-19 pandemic.
Corroborating with our findings, a study showed that children/adolescents (including ADHD) with and without pre-existing psychiatric diagnoses worsened between 47-52% in the domains of depression, irritability, attention, anxiety, and hyperactivity, while those without premorbid mental health worsened 37 - 40%.40 A more specific study with ADHD patients of all ages observed the negative effects of the COVID-19 pandemic on emotions such as sadness/depression, mood, anxiety, boredom, and loneliness.41 A study with German children and adolescents with mental disorders observed that one-third of them reached the cut-off for clinically significant pandemic-associated distress (as rated by their parents). In this group, 38.3% were patients with ADHD with and without conduct disorder and the result obtained was significantly higher when compared to healthy controls.42
Inattention was pointed out as one of the predominant new-onset psychological problems in children and adolescents during the COVID-19 pandemic.43 This finding goes toward ours, since the authors observed inattention worsened in patients and controls, however with higher significance in the firsts. This domain should receive special attention from parents, physicians, and educators, as it is essential for children's learning and the development of their skills.
Contributing to our findings of increased depression during the pandemic, a review article observed that depression occurs in youths with ADHD at a significantly higher rate than in controls of the same age.45 In healthy children, authors observed that depression was the second most prevalent mental health problem during the pandemic, with an incident rate of 19.7%.46 This symptom should be evaluated and treated in patients with ADHD that went through the pandemic, since patients with ADHD in childhood may have an increased risk of recurrent depression in the young-adulthood.47
Sleep was an issue during the pandemic for children and adolescents with ADHD, but also for children and adolescents with autism spectrum disorder,48 those with epilepsy,49 and healthy children and adolescents.46 A meta-analysis found that children and adolescents were the second most prevalent population with sleep problems (42.47%), behind only people with COVID-19.50 Additionally, this population showed sleep disturbances at a rate of around 46%, which is a matter of concern, once a meta-analysis developed pre-COVID-19 pandemic observed that this rate was 25% in healthy children and adolescents.51
Like this SR, an overall increase in media use in healthy children52 and adolescents was observed compared to the pre-pandemic period.53 Additionally, authors found significantly more stress and poorer mental health in adolescents.53
Some limitations were observed in this SR. Although eligible articles included addressed similar subjects concerning the ADHD universe, approaches differed among studies, providing a heterogeneous collection of information, limiting comparison and quantification of results. Adding to it, most articles are based on surveys responded to by parents or caregivers, therefore based on their perception toward their children, which potentially includes bias and reduces the quality of evidence.
In conclusion, this systematic review provides information regarding children and adolescents with ADHD who went through the COVID-19 pandemic. Taken together, the data available in the literature collectively support that patients with ADHD were affected by the pandemic and this had impacted their behavior, mood, and sleep quality.
FundingNo grant was provided for the development of this review.
JDP is a postdoc with a scholarship by Coordenação de Aperfeiçoamento de Pessoal de Nivel Superior- Brasil (CAPES), process number 88887.624940/2021-00.
MLN is a researcher 1D supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq)- Brazil, PQ306338/2017-3.