In this study, the authors aimed to evaluate the effectiveness of the vena cava distensibility index and pulse pressure variation as dynamic parameters for estimating intravascular volume in critically ill children.
MethodsPatients aged 1 month to 18 years, who were hospitalized in the present study's pediatric intensive care unit, were included in the study. The patients were divided into two groups according to central venous pressure: hypovolemic (< 8 mmHg) and non-hypovolemic (central venous pressure ≥ 8 mmHg) groups. In both groups, vena cava distensibility index was measured using bedside ultrasound and pulse pressure variation. Measurements were recorded and evaluated under arterial monitoring.
ResultsIn total, 19 (47.5%) of the 40 subjects included in the study were assigned to the central venous pressure ≥ 8 mmHg group, and 21 (52.5%) to the central venous pressure < 8 mmHg group. A moderate positive correlation was found between pulse pressure variation and vena cava distensibility index (r = 0.475, p < 0.01), while there were strong negative correlations of central venous pressure with pulse pressure variation and vena cava distensibility index (r = –0.628, p < 0.001 and r = –0.760, p < 0.001, respectively). In terms of predicting hypovolemia, the predictive power for vena cava distensibility index was > 16% (sensitivity, 90.5%; specificity, 94.7%) and that for pulse pressure variation was > 14% (sensitivity, 71.4%; specificity, 89.5%).
ConclusionVena cava distensibility index has higher sensitivity and specificity than pulse pressure variation for estimating intravascular volume, along with the advantage of non-invasive bedside application.
It is difficult to determine the optimal fluid treatment for a critically ill patient based on the intravascular volume alone, due to the influence of factors such as impaired myocardial function, mechanical ventilator therapy, and changes in distribution volume.1,2 Early diagnosis and treatment of tissue hypoperfusion are important to prevent the development of complications in critically ill patients, whose reserve is severely limited.1-3 Central venous pressure (CVP), one of the first invasive methods used to determine intravascular volume, may not provide clear results in patients undergoing mechanical ventilator therapy due to changes in intrathoracic pressure.4 The vena cava distensibility index (dIVC) is increasingly being used, as it reflects both cardiac and respiratory changes. Furthermore, it can be performed at the bedside using a non-invasive procedure.5,6 Pulse pressure variation (PPV) is another parameter reflecting changes in intrathoracic pressure; it can easily be performed in any patient undergoing arterial monitoring, making it useful for detecting changes in intravascular volume.7,8 No pediatric study to date has shown which of these assessments is more effective for determining intravascular volume in critically ill pediatric patients, and standards of care have not yet been established. Determining a diagnostic cutoff for intravascular volume in critically ill children should be of major benefit during resuscitation, especially in critical situations such as shock.
In this study, the authors aimed to evaluate the effectiveness of vena cava distensibility index and pulse pressure variation, which are dynamic parameters for determining intravascular volume in critically ill children.
Materials and methodsPatients aged 1 month to 18 years, who were hospitalized at the Erciyes University Faculty of Medicine pediatric intensive care unit, were enrolled in this study. This study was approved by the Institutional Review Board (Project code:2018/144). The patients were divided into two groups according to CVP: a hypovolemic group (CVP < 8 mmHg) and a non-hypovolemic (CVP ≥ 8 mmHg).9 In both groups, the effectiveness of the intravascular volume assessment was evaluated by simultaneously measuring dIVC using bedside ultrasound and PPV using arterial monitoring. The study was supported by an Erciyes University BAP grant awarded to the Scientific Research Project Coordinator; project code: TSA-2018–8279).
Exclusion criteriaTidal volume < 8 mL/kg
Presence of spontaneous respiration
Presence of pulmonary hypertension (Estimated mPAP = maximum PR velocity + mean RAP; pediatric pH defined as mPAP > 25 mmHg and PVRi > 3.0 WU m2)10
Right ventricular failure (echography evidence of paradoxical interventricular septal motion)11
Arrhythmia (Non-sinus rhythm in ECG)
Heart peak rate per number of breaths (min) ≤ 3.6
Intraabdominal pressure ≥ 16 mmHg
CVP measurement: CVP was recorded in patients undergoing central venous catheterization using a GE 560 monitor and appropriate kit.
dIVC measurement: Critically ill patients were placed in the supine position; the inferior vena cava was located using a probe and marked 1 cm from the hepatic vein. The dIVC was measured using M-mode. On a subcostal window, measure the maximum IVC diameter on inspiration (dI) and the minimum IVC diameter on expiration (dE).12 dIVC = [(maximum diameter on inspiration –minimum diameter on expiration)/ minimum diameter on expiration]
PPV measurement: PPV was recorded using the GE 560 monitor in cases where arterial catheterization was performed. PPV was defined as the relative variation between the highest (PPmax) and lowest (PPmin) pulse pressure divided by the mean of PPmax and PPmin.13
Statistical analysisThe normality of the parametric data was analyzed using the Shapiro–Wilk test. Numerical variables are expressed as mean ± SD or median (minimum, maximum), as appropriate. Comparison between groups was performed using Student's t-test and the Mann–Whitney U test for normal and non-normally distributed data, respectively. Pearson's or Spearman's correlation analysis was used to investigate the relationship between two numerical variables. Receiver operating characteristic (ROC) curve analysis was used to determine the predictive power of dIVC and PPV for hypovolemia. Kappa statistics were generated to assess the agreement of dIVC and PPV values with CVP values. All statistical analyses were performed using SPSS software (ver. 22.0; IBM Corp., Armonk, NY, USA), and statistical significance was set at P < 0.05.
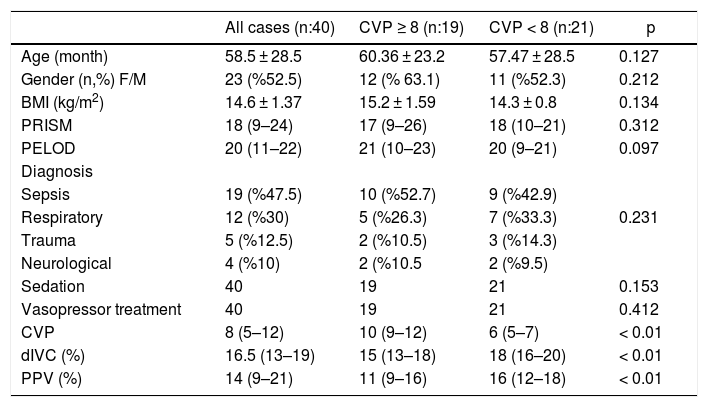
ResultsOf the 40 cases enrolled in the study, 23 were girls (57.5%), and 17 were boys (42.5%); their average age was 58.5 ± 28.5 months. For all cases, the mean CVP value was 8 ± 2.3 mmHg, while the mean PPV was 14% (9–21%) and the mean dIVC was 16.6 ± 2.9%. When cases were classified according to CVP, 19 patients (47.5%) were in the CVP ≥ 8 mmHg group, and the remaining 21 (52.5%) were in the CVP < 8 mmHg group. According to the admission diagnoses of the patients, 12 (30%) patients due to respiratory problems, 4 (10%) patients due to neurological problems, 19 (47.5%) patients due to sepsis, and 5 (12.5%) patients due to trauma were admitted to intensive care. The demographic data of all cases are presented in Table 1.
Demographic data of patients.
PELOD, pediatric logistic organ dysfunction; PRISM, pediatric risk of mortality; BMI, body mass index.
A moderate positive correlation was found between PPV and dIVC (r = 0.475, p < 0.01), while there were strong negative correlations of CVP with PPV and dIVC (r = –0.628, p < 0.001 and r = –0.760, p < 0.001, respectively). However, when groups were classified according to CVP and the relationship between CVP, PPV and dIVC was evaluated, there was a moderate negative correlation between CVP and dIVC in the group with CVP < 8 mmHg (r = −0.489, p< 0.01)
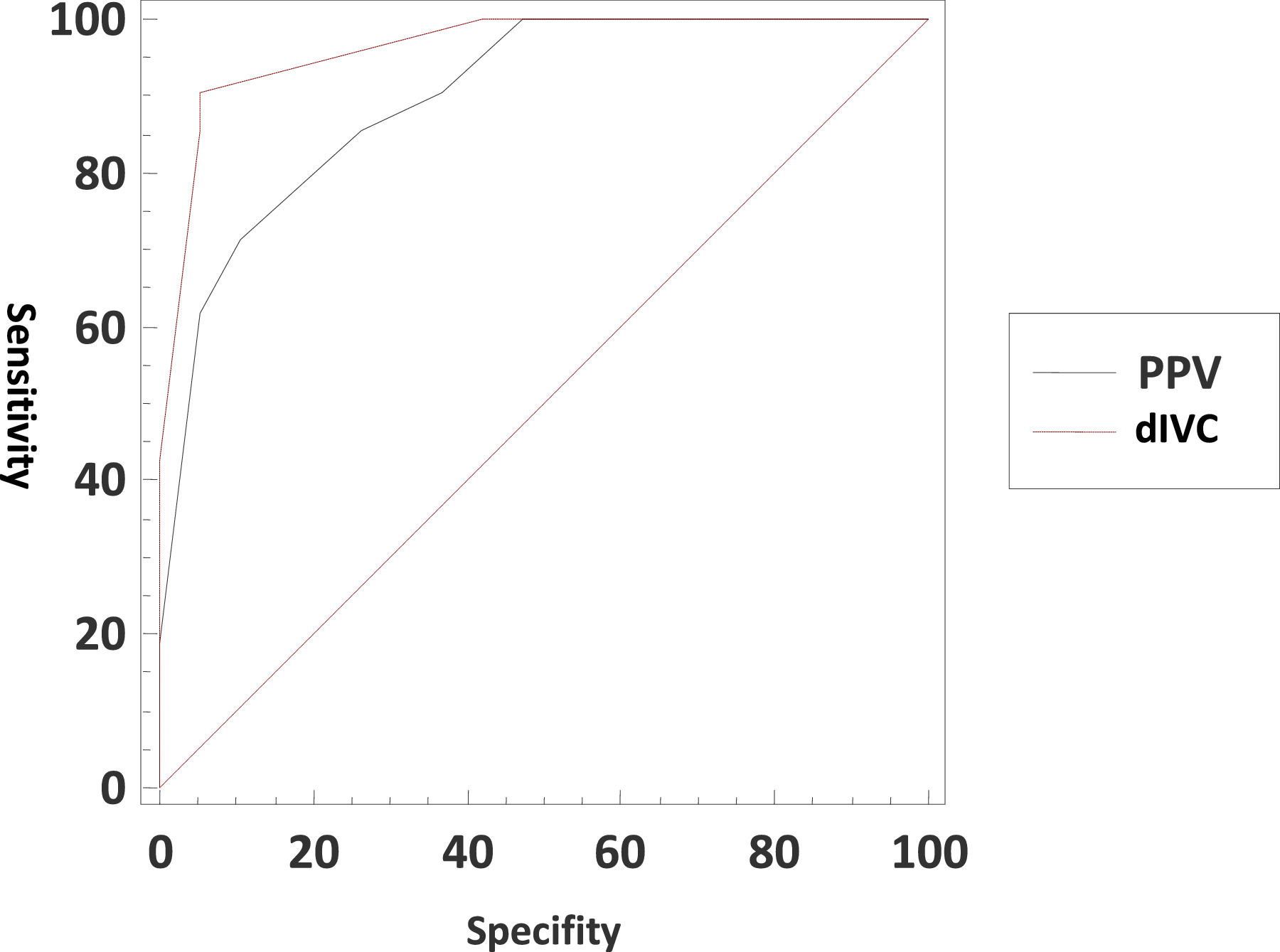
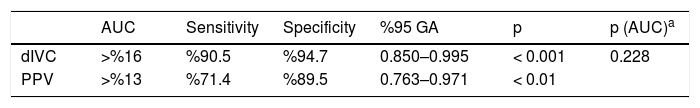
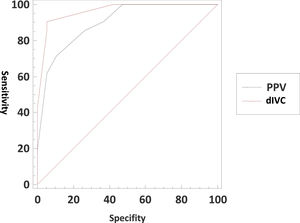
In terms of predicting hypovolemia, the predictive power for dIVC was >16%, and that for PPV was >13% (Table 2). There was no statistically significant difference in predictive power between the two parameters (Fig. 1).
ROC analysis of dIVC and PPV associated with hypovolemia.
| AUC | Sensitivity | Specificity | %95 GA | p | p (AUC)a | |
|---|---|---|---|---|---|---|
| dIVC | >%16 | %90.5 | %94.7 | 0.850–0.995 | < 0.001 | 0.228 |
| PPV | >%13 | %71.4 | %89.5 | 0.763–0.971 | < 0.01 |
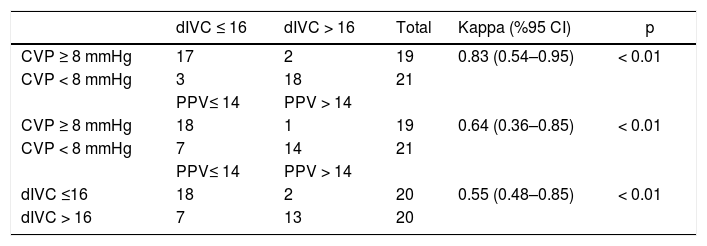
The agreement of dIVC and PPV with CVP was also evaluated. The agreement between CVP and dIVC was almost perfect (K = 0.83, 95% CI = 0.54–0.95), with 90.5% sensitivity and 94.7% specificity for detecting hypovolemia. The agreement between CVP and PPV was also substantial (K = 0.64, 95% CI = 0.36–0.85). The agreement between dIVC and PPV was fair (K = 0.55, 95% CI = 0.48–0.85) The analysis is presented in detail in Table 3.
DiscussionRapid evaluation of intravascular volume status and appropriate fluid resuscitation is very important in critically ill children. Measuring CVP may not give a clear estimate of intravascular fluid volume because, as an invasive method, it is affected by pressure changes in mechanically ventilated patients.4,9 Numerous approaches have been used to predict fluid change in the venous system, such as measuring the vena cava collapsibility index or the dIVC, as dynamic parameters that can be used to predict intravascular fluid volume in children and adults instead of CVP (which is a static parameter).9,14,15
Ng et al. found no significant relationship between VCI and CVP in mechanically ventilated pediatric patients.9 However, the dIVC is reportedly more specifically associated with intravascular fluid status in patients undergoing mechanical ventilator therapy.16,17 In the present study, there were initially 21 patients in the hypovolemic group based on CVP values. Evaluation of the relationship between CVP and dIVC revealed a strong negative correlation. However, when CVP values were divided into subgroups and the relationship between CVP, PPV and dIVC was evaluated, the authors found a moderate negative correlation between CVP and dIVC in the group with CVP 〈 8 mmHg. Rathore et al. found no correlation between CVP and PPV values in the fluid responsive group before the fluid bolus, as well as a moderate negative correlation, was found in the fluid responsiveness group before the fluid bolus. After fluid bolus, they showed a moderate negative relationship in both groups.18 For dIVC, the predictive power was 〉 16%, with 90.5% sensitivity and 94.7% specificity. Based on the dIVC values, 20 patients were included in the hypovolemic group. The authors found a strong correlation between CVP and dIVC. Barbier et al. reported that the dIVC showed a predictive power for hypovolemia of 18% in septic shock patients undergoing mechanical ventilation.16 They reported no statistically significant relationship between CVP and dIVC, similar to Mazlan et al.5
The PPV is another dynamic method for evaluating intravascular volume status and the response to fluid therapy. Measuring the PPV allows for dynamic and continuous monitoring of the interaction of the heart and lungs.19,20 Michard et al. reported a predictive power of the PPV for hypovolemia of > 13%, with a sensitivity of 94% and specificity of 96%.21 Similar to the literature, the predictive power of PPV in the present study was > 14%, with 71.4% sensitivity and 89.5% specificity. Mahjoub et al. performed a multicenter study involving 311 patients from 26 intensive care units and evaluated fluid responsiveness in 79 patients over a 24-hour period. PPV was evaluated in 15 patients who had arterial lines, and only 5 patients were reported as fluid-responsive.22 DeBacker et al. showed that PPV may not be sufficient for determining fluid responsiveness in the presence of arrhythmia or spontaneous respiration, or in cases where the tidal volume is < 8 mL/kg or the heart rate/respiratory rate is < 3.6.23,24 A small number of adult studies evaluated the effectiveness of dIVC and PPV for assessing intravascular volume.25-27 In the present study, initially, there was a strong negative correlation between CVP and PPV, similar to the results for dIVC. Although the hypovolemic group included 21 people based on CVP values, the authors classified 15 people as hypovolemic according to their PPV values and found a strong correlation between CVP and PPV.
Although all three parameters were correlated, the present study had some limitations. First, it was a single-center study including a small number of cases, and intrathoracic pressure values varied due to differences in the pressure applied to achieve a tidal volume > 8 mL/kg in each patient. The authors evaluated the PPV values of patients by classifying them as hypovolemic (fluid responsive) and non-hypovolemic (fluid non-responsive) according to only CVP values without any fluid bolus administration. Because it was not possible to routinely perform PPV in every pediatric intensive care unit in Turkey, and the authors wanted to evaluate its relationship with CVP. Moreover, the effect of intrathoracic pressure changes caused by differences in the response between the lungs was not consistent. dIVC and PPV are dynamic parameters for estimating intravascular volume in critically ill children, and their effectiveness and validity have been proven. dIVC exhibits greater sensitivity and specificity than PPV with respect to evaluating intravascular volume, and can also be performed non-invasively at the bedside. To validate the authors’ findings, studies including more cases are needed.
FundingThe study was supported by an Erciyes University BAP grant awarded to the Scientific Research Project Coordinator; project code TSA-2018-8279.