To assess the finger-feeding technique when compared with the cup feeding method during the early stage of preterm infant feeding transition regarding milk loss, milk ingestion period, and complications.
MethodsExperimental, randomized, prospective study including 53 preterm infants with gestation age<37 weeks, clinically stable, and with a score of >28 points in the Oral Feeding Readiness Assessment Scale. The preterm babies were randomized to be included in the control group, which underwent the feeding transition using a cup or in the experimental group, which used the finger-feeding technique. The analysis of data was performed using Student's t-test to evaluate differences between mean values of the appointed variables, and Fischer's test for categorical variables; the asymmetric variables were assessed by the Kruskal–Wallis ANOVA test.
ResultsWhen compared with the control group, the experimental group showed lower milk loss, longer milk ingestion time, and a lower frequency of complications during feeding. The significance level was set at 5%, with a confidence interval of 90%.
ConclusionThe finger-feeding technique was shown to be a better feeding transition method regarding efficacy when compared with cup feeding method, due to lower milk loss and fewer complication episodes.
Avaliar a técnica sonda-dedo em comparação ao copo no início da transição alimentar do prematuro quanto à perda de leite ofertado, tempo de ingestão e complicações.
MétodosEstudo experimental, randomizado, não cego, prospectivo com 53 prematuros de idade gestacional <37 semanas, clinicamente estáveis e com escore >28 pontos na Avaliação da Prontidão para início da alimentação por via oral. Os prematuros foram randomizados para o Grupo Controle que realizou a transição alimentar com o copo e para o Grupo Experimental que utilizou a técnica sonda-dedo. Na análise dos dados, foram aplicados o teste t de Student para avaliar a diferença de médias e o teste exato de Fisher para as variáveis categóricas, enquanto para as variáveis assimétricas foi aplicado a Anova de Kruskal-Wallis.
ResultadosO grupo experimental apresentou em relação ao grupo controle, diferença significativa quanto a menor perda de leite, maior tempo de dieta e menor frequência de complicações. O nível de significância foi de 5% e poder de teste mínimo de 90%.
ConclusãoA técnica sonda-dedo mostrou-se um método alternativo de transição alimentar superior em sua eficiência quanto a menor perda de leite e menor incidência de complicações.
Preterm newborn face a difficult reality, which is that of adapting to extrauterine life.1–3
Breastmilk is the best food for preterm newborns, and it is always indicated, as it contains specific nutrients that will contribute to their maturation, representing an important factor in the protection against infections, leading to a better digestibility and absorption of these nutrients and promoting better brain development.4,5
However, in a neonatal intensive care unit (NICU), the preterm population cannot always be fed directly at the mother's breast, either due to clinical instability or the mother's absence.6,7
Furthermore, it is worth noting that preterm newborns have inadequate oral functions due to neurological immaturity, abnormal muscle tone, lack of muscle activity integration, and alterations in oral reflex coordination, leading to less active, irregular, and diminished strength reflexes and difficulty maintaining alertness. All these factors lead to the initial need to feed the preterm newborn through an alternative feeding route, as is the case of gastric tube feeding.8–10
The way the milk is offered to preterm infants is an important variable to consider. The advantages and disadvantages of the methods are discussed in terms of physiological stability and impact on exclusive breastfeeding.11–13
Several forms of feeding are used, such as cup, suction from a syringe with the gloved finger, translactation, finger-feeding, paladai, and bottle, among others; scientific justification is necessary for all methods, but for the cup and the bottle, which have been widely studied.12–16
The use of techniques to mature the sensorimotor-oral system has been explored, so that the preterm newborn can undergo a safer and shorter transition to oral feeding.17
The finger-feeding method is a technique in which milk is supplied by suction to preterm infants through a gastric tube connected to a syringe and attached to the gloved small finger with adhesive tape. Although it is a widely used technique in several neonatal services, studies describing the technique, its indications. use, benefits, advantages, and disadvantages are still scarce.14,18–20
Therefore, it is necessary to enhance technologies that aim to improve the suction pattern and, consequently, the preterm infant's capacity of oral feeding, primarily directed to breastfeeding. The cup-feeding method has been indicated by the World Health Organization as the method of transition and/or oral feeding complementation for preterm infants, as it does not cause the nipple confusion phenomenon and does not influence the preterm infant's suction function.20,21
It should be noted that, in clinical practice and in the NICU routine, mothers are not always present, which is the reality of many health services. Due to maternal absence, the preterm infant is fed for long periods using the cup, without performing the suction function. As a result, this condition discourages maternal breastfeeding, because feeding preterm infant exclusively through the cup induces a modification in his/her oral behavior.22 This change in sucking behavior is evident mainly in the difficulty in opening the mouth and the anteroposterior movement of the preterm infant's tongue. When the mother comes to the NICU to breastfeed the child, a change in the sucking behavior at the mother's breast is observed, delaying and impairing the breastfeeding process.
The authors highlight the search for scientific evidence regarding the techniques used as alternative methods to the cup for feeding of preterm infants, with emphasis on cases of maternal absence. Thus, it is emphasized that the suction function should be stimulated through training, as physiologically and safely as possible, similarly to the suction actions performed in the mother's womb. Therefore, the aim of the present study was to evaluate the effectiveness of the finger-feeding technique in preterm infants in comparison with the cup-feeding method at the beginning of the feeding transition from the gastric to the oral route, regarding the loss of milk offered, time of milk ingestion, and presence of complications.
MethodsThis was an experimental, randomized, controlled, non-blinded, prospective, and longitudinal study.
The study population was selected among the 168 preterm infants admitted to the NICU of Hospital de Clínicas in the city Curitiba, state of Paraná, Brazil, from June 2012 to March 2013. Of the 93 neonates that comprised the target population, 53 were eligible for study, selected by probabilistic sampling technique, with block randomization.
The sample was calculated considering the main outcomes of the study measured as proportions, considering effect size of 30%, type I error of 5%, and type II error of 10%, with 25–30 cases being estimated per group.
For randomization, the authors a sequence of block letters of equal size, placed into brown envelopes, which were drawn by the nurses responsible for the NICU, and the assessed interventions were distributed, block by block, until the process of allocation of the study participants was completed for the control group (CG), identified by the letter A, and for the experimental group (EG), identified by the letter B. The researchers did not participate in this process. There was a subdivision regarding the gestational age ranges in both groups, aiming to maintain sample homogeneity.
The following were considered as inclusion criteria: gestational age <36 weeks and six days, determined by obstetric ultrasound performed up to 12 weeks gestation or by chronology, determined by the New Ballard Method; not receiving oral milk until inclusion in the study; a score>28 points in the readiness for oral feeding assessment, which consists in a speech therapy-audiological assessment consisting of items with a variation in performance, with scores ranging from 0 to 2, totaling a sum ranging from 0 to 3623; and the signing of the informed consent form by parents/tutors. The exclusion criteria included: grades 3 and 4 periventricular hemorrhage; clinical instability at the time or during the study, such as the presence of necrotizing enterocolitis, sepsis, bronchopulmonary dysplasia, and other respiratory or hemodynamic clinical instability; Apgar score<5 at the 5th minute; and presence of genetic syndromes, neurological disorders, or congenital malformation of the head and neck or of central nervous system.
Training for the finger-feeding technique was performed by the main study researcher and later offered to the NICU health team of Hospital de Clínicas regarding the handling of the utensils used in the two study techniques, i.e., the cup and finger-feeding, and educational material was made available.
The incubator or crib was identified with an image related to the feeding transition method performed by the nursing team, to minimize the interruption of the study protocol. The evaluations at the beginning of the feeding transition were filmed and the variables assessed were:
- -
Loss of the offered milk: using a gauze pad unit positioned below the chin of the neonate and weighed in a precision digital scale with a sensitivity of 0.1g, the milk was offered by the caregiver on duty and the feeding and gauze weighing were supervised by the nursing team before and after the neonate was fed.
- -
Time of feeding: the time of the feeding offered by the nursing team was observed during the filming.
- -
Presence of complications during the oral feeding: these complications were oxygen saturation, cyanosis, respiratory effort, and gagging. The observation of these signs of stress was performed by the nursing team.
The videos collected from both groups were analyzed by experienced professionals, who had been working in the NICU for over five years.
Use of the finger-feeding techniqueThe finger-feeding technique was used in a manner similar to that described by Fujinaga et al. for the feeding transition; first, the tip of the catheter was cut and fixated with adhesive tape to the inner side of the gloved small finger. The other end of the catheter was connected to a syringe without the plunger, attached laterally to the individual apron worn by the caregiver at the level of the neonate's head, with raw milk milked from the mother or from the human milk bank.20 The milk would slide through the tube as the sucking pattern was adjusted by the newborn and not by gravity, at which point the pulp of the small finger was facing the hard palate.
Use of the cup-feeding techniqueThe cup-feeding technique was carried out by the nursing team according to the service routine. The technique consisted in offering the milk in a disposable, 50-milliliter plastic cup. The neonate was kept in a seated or semi-seated position, with head and body aligned. The milk was placed on the edge of the cup, which was positioned on the neonate's lower lip, with the edges touching the labial commissures, where the neonate performed tongue anteriorization movements, sucking the milk from the cup.13,15,21
This study was approved by the Committee of Ethics in Research in Human Beings of Hospital das Clínicas, under CAAE No. 01934912.6.0000.0096.
The data were entered in a spreadsheet and the difference between the continuous variables was evaluated using Student's t-test, Mann–Whitney test, and ANOVA for repeated measures, with a minimum significance level of 5%, using Statistic-Statsoft™ (StatSoft, Inc., Electronic Statistics Textbook, USA).
ResultsThe control group comprised 27 newborns fed through the cup-feeding technique, 13 of whom had 32–34 weeks of gestational age (GA; 24.5%) and 14 had 34–36 weeks of GA (26.4%). The experimental group, fed using the finger-feeding technique, comprised a total of 26 newborns, 12 with 32–34 weeks of GA (22.6%) and 14 with 34–36 weeks of GA (26.4%).
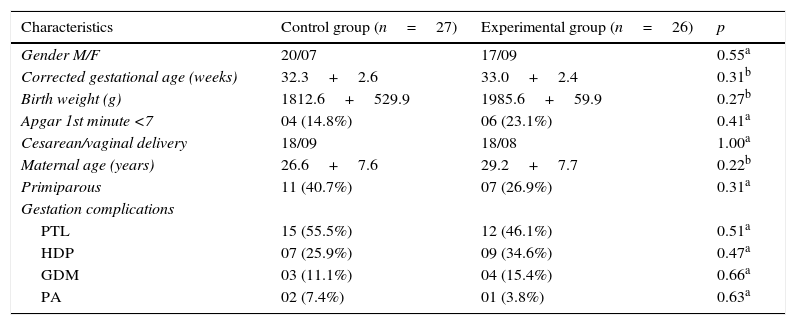
The control and experimental groups were homogeneous regarding birth weight, gestational age, and gender. There were also no differences regarding maternal age, type of delivery, frequency of maternal obstetric complications, and Apgar score at the 1st minute (Table 1).
Characteristics of the control and experimental groups (n=53).
| Characteristics | Control group (n=27) | Experimental group (n=26) | p |
|---|---|---|---|
| Gender M/F | 20/07 | 17/09 | 0.55a |
| Corrected gestational age (weeks) | 32.3+2.6 | 33.0+2.4 | 0.31b |
| Birth weight (g) | 1812.6+529.9 | 1985.6+59.9 | 0.27b |
| Apgar 1st minute <7 | 04 (14.8%) | 06 (23.1%) | 0.41a |
| Cesarean/vaginal delivery | 18/09 | 18/08 | 1.00a |
| Maternal age (years) | 26.6+7.6 | 29.2+7.7 | 0.22b |
| Primiparous | 11 (40.7%) | 07 (26.9%) | 0.31a |
| Gestation complications | |||
| PTL | 15 (55.5%) | 12 (46.1%) | 0.51a |
| HDP | 07 (25.9%) | 09 (34.6%) | 0.47a |
| GDM | 03 (11.1%) | 04 (15.4%) | 0.66a |
| PA | 02 (7.4%) | 01 (3.8%) | 0.63a |
PTL, preterm labor; HDP, hypertensive disease of pregnancy; GDM, gestational diabetes mellitus; PA, premature amniorrhexis.
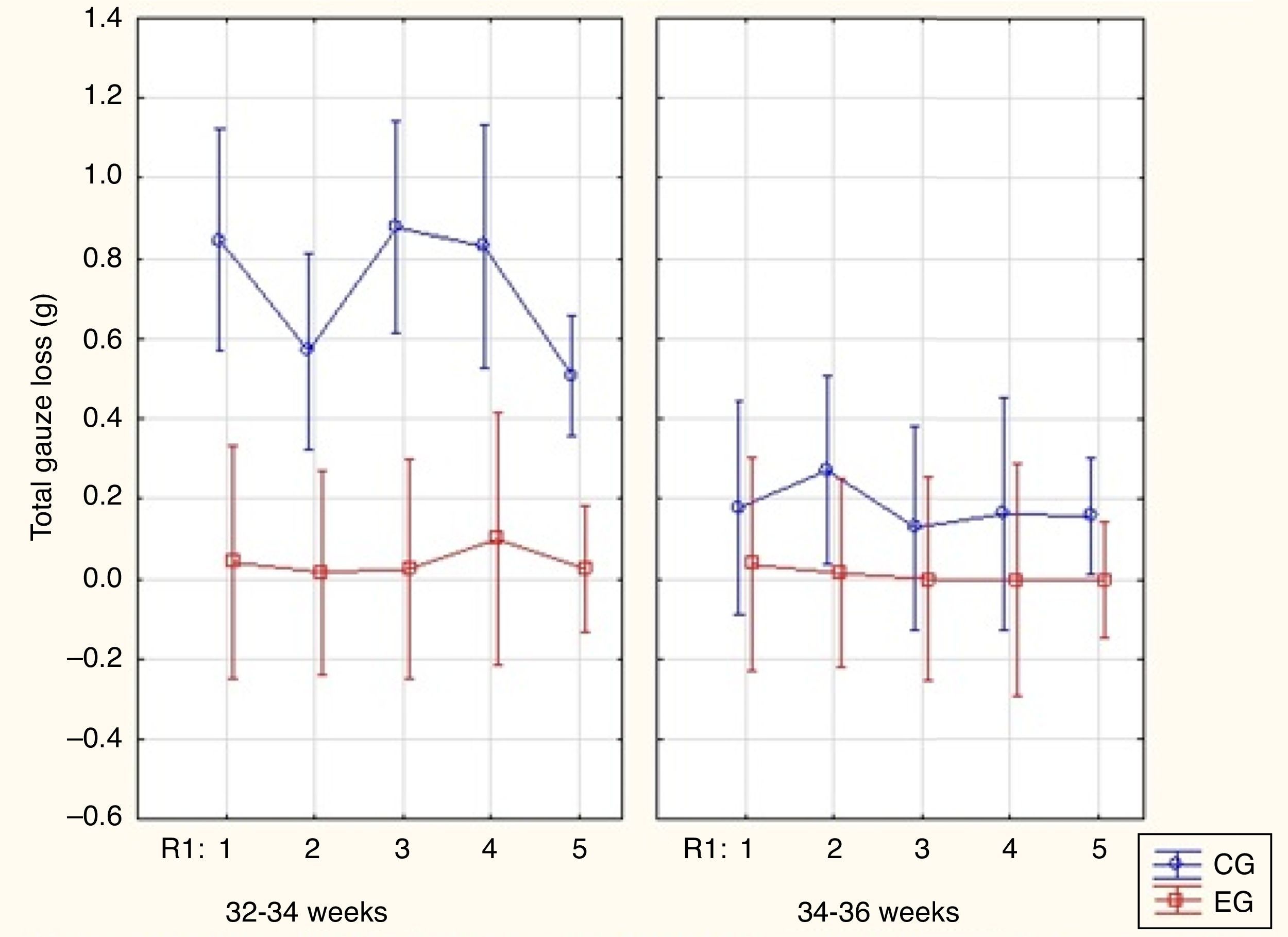
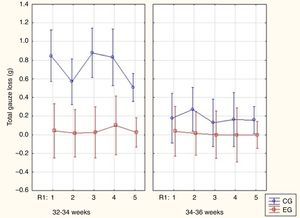
The control group in both GA ranges showed significantly higher values for milk loss, as measured by total gauze weighting, than the experimental group. This milk loss was higher in the control group among infants with 32–34 weeks of GA (Fig. 1).
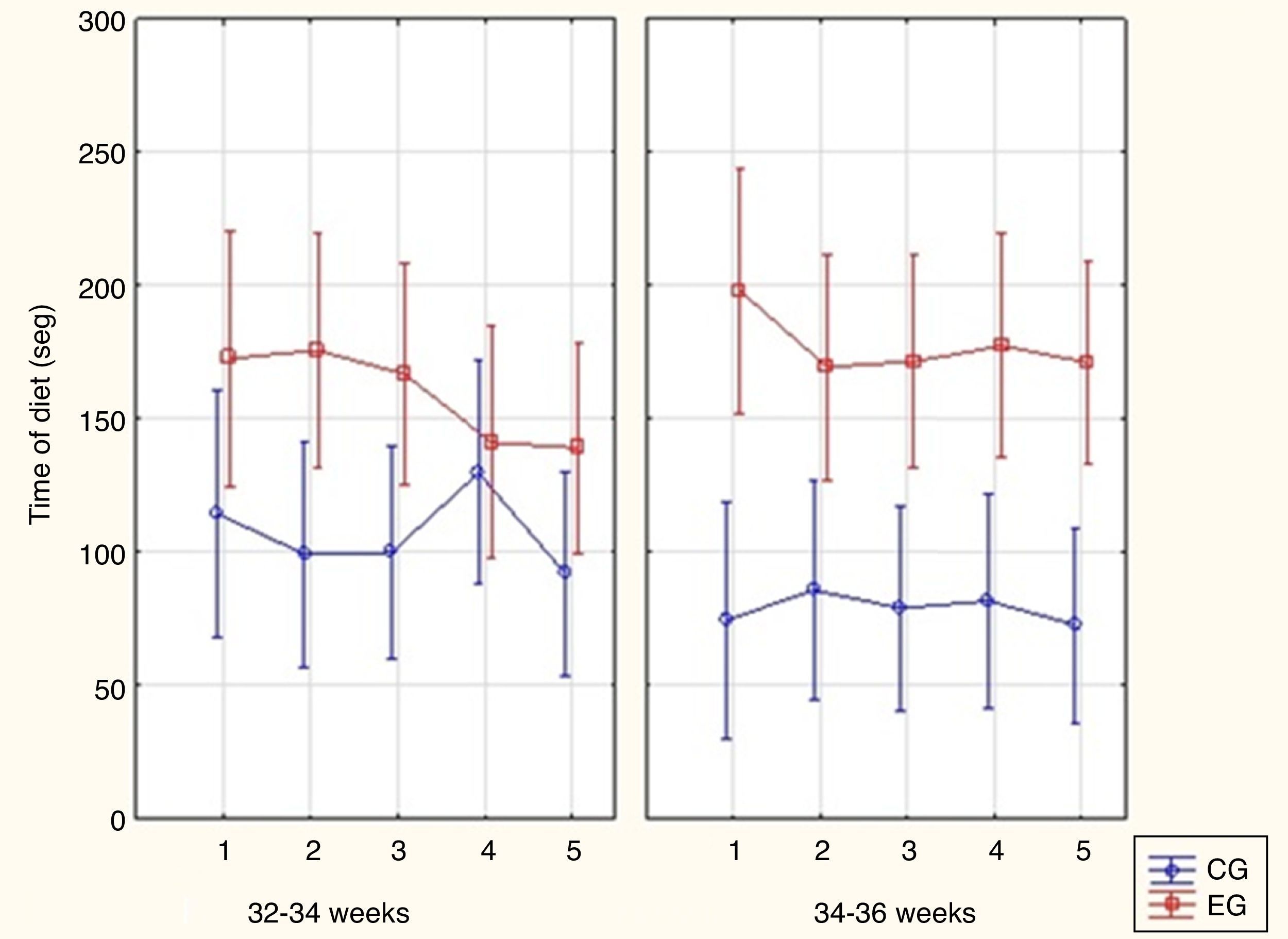
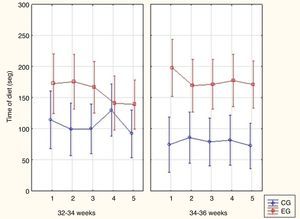
The time of feeding in the experimental group was longer than the time of feeding in the control group (Fig. 2).
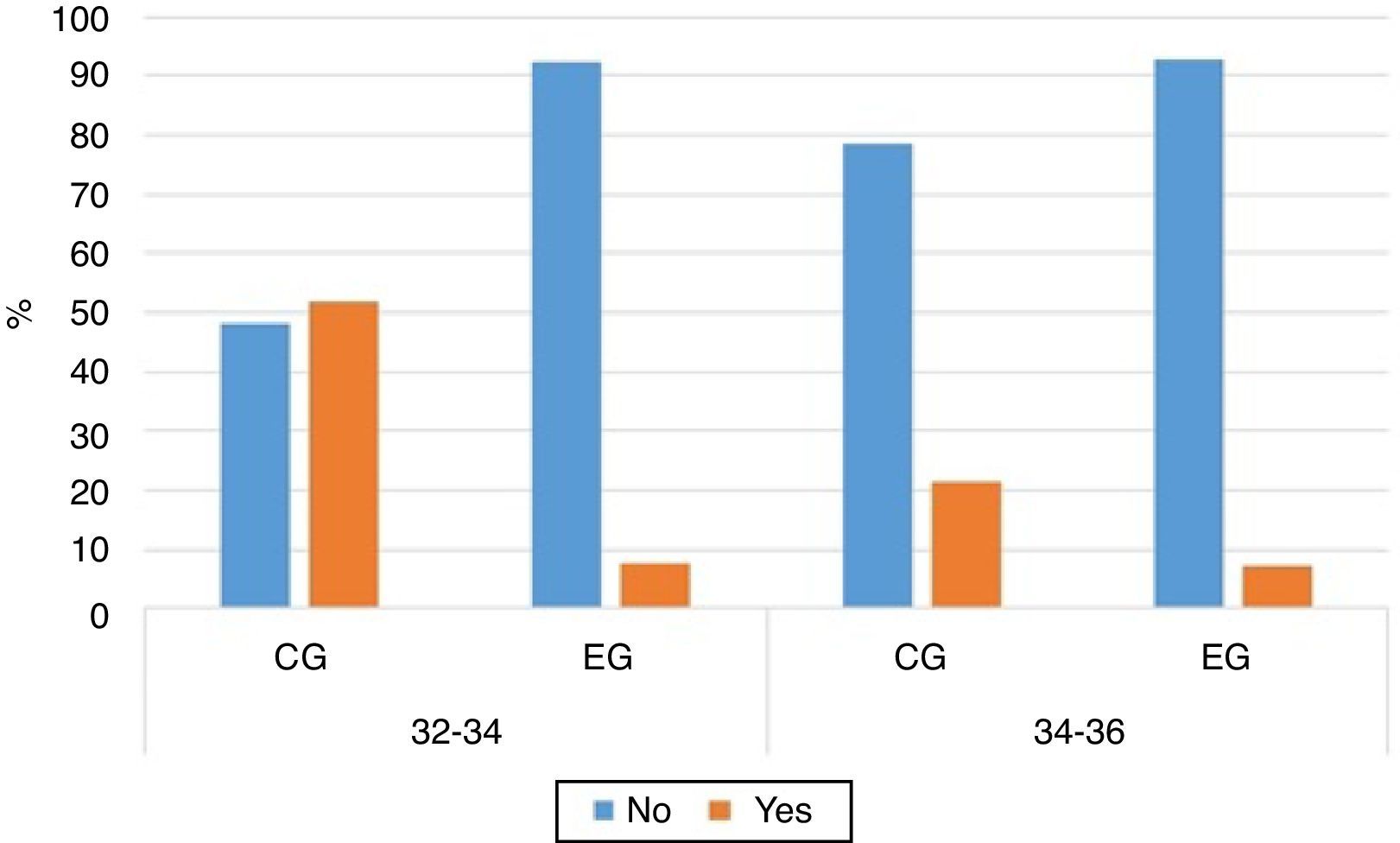
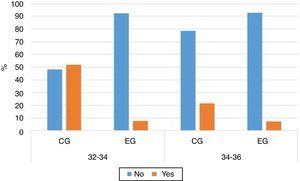
Complications occurred significantly more often among neonates with 32–34 weeks of GA in the control group (Fig. 3). However, no significant differences were observed regarding complications in the control and experimental groups in the GA range of 34+1/36+6 weeks.
Regarding weight gain, a similarity was observed between the assessed groups. In the control group, the median weight difference between the 1st and the last weight assessment was 145.0g, ranging from −50g to 850.0g, while in the experimental group, the median was 85.0g, ranging from −140g to 1060g (p=0.34).
DiscussionThe feeding transition from the gastric to the oral route is a great challenge, not only for the preterm infant, but also for the healthcare team, as it is their responsibility to assess the best feeding transition method for each newborn, considering it is a period that requires attention regarding safety and efficiency in diet administration.
The finger-feeding technique has emerged as a transition alternative, widely used in the routine of several services as a form of suction training and/or complementary feeding, when the mother is absent at the time of feeding. It is also an alternative to artificial nipples and bottles in the hospital environment, in situations where cup-feeding has not been successfully implemented.13–15,21
The cup, a utensil used in the feeding transition period, had its applicability assessed in comparison to the finger-feeding technique regarding the administration procedures and its use, because it is the method recommended by the World Health Organization (WHO) and used in the NICU of HC-UFPR. It was not the objective of this study to challenge the benefits of cup-feeding in the transition period, which has been widely studied and demonstrated,12,13,15,21 but to evaluate the applicability of both methods in a population of preterm infants with different ranges of corrected GA.
The previous training aimed at teaching all study collaborators in order to avoid the inappropriate use of the methods or that lack of experience could lead to complications or interfere with the results found, considering the lack of knowledge or inadequate use of alternative techniques in oral feeding in preterm infants can result in risk situations.17,23,24
During the data collection period, there were no changes in the nursing team or in the measurement equipment.
This study was carried out during the feeding transition period of preterm infants, and data were assessed from the first to the fifth days, because it is a critical period for the implementation of the oral diet, as it requires greater attention regarding the effectiveness of the preterm infant's undergoing feeding transition. Thus, the need for further studies assessing the applicability of the finger-feeding technique in other variables and in the follow-up of the feeding transition to the oral route is reinforced.
The subdivision of GA was necessary, since neurological system immaturity directly interferes with the suction results. In infants with younger GA, sucking may be inefficient, resulting in greater energy expenditure and greater risks due to the lack of swallowing-breathing coordination, which may lead to greater chances of complications. Moreover, it should be noted that, without this subdivision, the sample would not be homogeneous regarding coordination maturity of the suction-swallowing-breathing functions, as preterm infants with GA higher than 34 weeks are already able to feed more safely and efficiently.2,14,16,23
In both GA ranges, the control group showed significantly higher values of milk loss when compared with the experimental group, with a higher loss in the corrected GA range of 32–34 weeks. This superiority regarding feeding acceptance, with lower milk loss observed in the experimental group, is in agreement with studies that described a greater loss of milk with the use of the cup-feeding method.13,17,21
Other studies observed that the finger-feeding technique also increased the amount of milk ingested by the newborn and a more efficient use of the oral diet when compared to the cup.13,17
The loss of milk and, consequently, incomplete ingestion of the total prescribed volume is a situation which, in addition to leading to weight loss, may influence the clinical status of preterm newborns.
The finger-feeding technique was shown to require more time and have a higher cost, both in the organization of the material used and in the milk supply when compared with the cup-feeding. Nonetheless, it provides the newborn with oral stimuli that will favor suction training, alertness maintenance, and coordination of suction/deglutition/breathing. The longer duration of the diet by the finger-feeding technique was due to the fact that milk was offered to the newborn only when he/she sucked the gloved finger, without the possibility of gravity flowing. Therefore, it is believed that feeding occurred more physiologically, respecting the time of the preterm newborn regarding the coordination of the suction-swallowing-breathing functions, as well as resting. Thus, it is believed that the benefits provided when using the finger-feeding technique for the premature newborn in the feeding transition, especially in the gestational age range below 34 weeks, compensate the longer time it takes to use the method.16,20,22
Regarding the complications, it was observed that they were statistically higher in the group that used the cup in the range of 32–34 weeks of GA. In the group of 34+1/36+6 weeks of GA, there was no significant difference between the groups regarding the presence of complications during the use of each technique. This difference is justified by the fact that preterm infants in the 34+1/36+6 weeks of GA have higher neurological maturity, achieving a better maintenance of alertness and sucking, swallowing, and breathing coordination during the oral diet.
One of the limitations of this study is the lack of control regarding evacuation frequency or occurrence of diarrhea as possible complications of the techniques used.
Additionally, no significant difference was observed in relation to the groups regarding exclusive breastfeeding rates at hospital discharge. The authors believe there is no difference, because both groups received encouragement and support to breastfeed, such as early stimulation of milking, guidelines, and encouragement to practice the kangaroo method and maternal breastfeeding, as it is a routine in the NICU of HC-UFPR.
Moreover, it should be noted that the aim of this study was to demonstrate the safety of the finger-feeding technique as a method of transition from the gastric to the oral route, and not as a feeding method. This is because the aim is to always provide assistance that can prioritize the mother's presence in the NICU, aligning the techniques to encourage breastfeeding with maternal desires.
Further studies still need to be performed to assess the effects of the finger-feeding technique on the prevalence of post-discharge breastfeeding, assessing its long-term impacts.
Finally, it is noteworthy that although the literature is scarce regarding the description, indication, and use of the finger-feeding technique, it is believed the latter is a type of feeding transition that benefits the preterm infant, especially in the corrected GA range of 32–34 weeks, as it allows suction training and the provision of safe and effective oral milk supply when breastfeeding is not possible.13–17
The results shown here reinforce the benefits of this technique and provide scientific evidence on the evaluation of feeding technology in preterm neonates, which should certainly have an impact on the development of a healthier population and, thus, contribute to a more stable society from the physical, physiological, and emotional standpoints.
The finger-feeding technique was shown to be a superior alternative method at the start of the dietary transition regarding its efficiency, when compared with the cup feeding method, due to the lower milk loss and incidence of complications, mainly in the range of 32–34 weeks of GA. However, the duration of the diet supply using the finger-feeding method was significantly longer than that of the cup feeding method.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Moreira CM, Cavalcante-Silva RP, Fujinaga CI, Marson F. Comparison of the finger-feeding versus cup feeding methods in the transition from gastric to oral feeding in preterm infants. J Pediatr (Rio J). 2017;93:585–91.
Study conducted at Universidade Federal do Paraná (UFPR), Curitiba, PR, Brazil.