This study proposed a version of the Children's Sleep Habits Questionnaire for infants under 12 months (CSHQ-I).
MethodsThe sample was comprised of 299 infants, aged between 2 weeks and 12 months.
ResultsExploratory factor analysis revealed four subscales: Bedtime Resistance, Sleep Anxiety, Positive Sleep Habits, and Daytime Sleepiness. The CSHQ-I total scale presented good test-retest reliability and internal consistency. The CSHQ-I also showed good concurrent validity, with significant associations found between the CSHQ-I total scale and subscales and a measure of infant sleep-wake behaviors.
ConclusionsThe present study suggested the CSHQ-I as a reliable instrument to assess sleep problems in infants during the first year of life.
Este estudo propôs uma versão do Questionário de Hábitos de Sono das Crianças para bebés com menos de 12 meses (CSHQ-I).
MétodosAmostra composta de 299 bebés, com idades entre duas semanas e 12 meses.
ResultadosA análise fatorial exploratória revelou quatros subescalas: Resistência em ir para a Cama, Ansiedade do Sono, Hábitos de Sono Positivos e Sonolência Diurna. A escala completa do CSHQ-I apresentou boa confiabilidade teste-reteste e consistência interna. O CSHQ-I também mostrou boa validade concorrente, com associações significativas encontradas entre a escala completa e subescalas do CSHQ-I e uma medida de comportamentos de sono-vigília dos bebés.
ConclusõesO presente estudo sugeriu o CSHQ-I como um instrumento confiável para avaliar os problemas de sono em bebés durante o primeiro ano de vida.
Infant sleep problems are one of the most prevalent concerns of parents and clinicians, and 15% to 35% of Western children present a sleep problem during the first years.1–3 The most common problems include frequent night wakings and resistance to initiate sleep.4–6 Co-sleeping/bed-sharing and lack of parental agreement regarding infant sleep management are also reported by parents as sleep problems.5 Moreover, studies suggested that sleep problems in early childhood tend to persist throughout life.1,5,7
The Children's Sleep Habits Questionnaire (CSHQ) was designed to identify sleep problems based on the International Classification of Sleep Disorders (ICSD-1).8 The CSHQ psychometric characteristics were analyzed in preschool- and school-aged children, showing acceptable/good psychometric characteristics in several countries,8–12 including Portugal.13 Eight subscales were proposed: Bedtime Resistance, Sleep-onset Delay, Sleep Duration, Sleep Anxiety, Night Wakings, Parasomnias, Sleep-Disordered Breathing, and Daytime Sleepiness.8 The CSHQ was also suggested as a useful tool to assess sleep problems in children aged from 2 to 5.5 years, with the same eight subscales.14
The CSHQ has been used in several studies to assess children's and infants’ sleep problems.15–20 In a study with 4-month-old infants (n=184), a factor analysis of the CHSQ found two subscales.18 The first subscale contained items related with resisting sleep, and was termed Sleep Resist; the second subscale, labeled as Sleep Anxiety, included items related with anxiety about being alone. Although this study analyzed the factor structure of this instrument, to the best of the authors’ knowledge the CSHQ psychometric characteristics were not fully explored in infants under 1 year of age and there is no validated version of the CSHQ for infants.
Other measures have been used to assess infant sleep problems. The Infant Sleep Questionnaire (ISQ)21 and the Brief Infant Sleep Questionnaire (BISQ)22 are some of the validated instruments. However, these instruments do not base infant sleep problems in a standardized classification system of sleep disorders.
A version of the CSHQ for infants will allow clinicians to identify sleep problems at an early age, based in a standardized classification system of sleep disorders, and allow researchers to conduct longitudinal studies on infant sleep problems development. This study proposed a version of the CSHQ for infants (CSHQ-I), based on the CSHQ version for preschool- and school-aged children. The reliability of the items of the CSHQ-I was also analyzed in infants aged 0–3 months, 3–6 months, and 6–12 months.
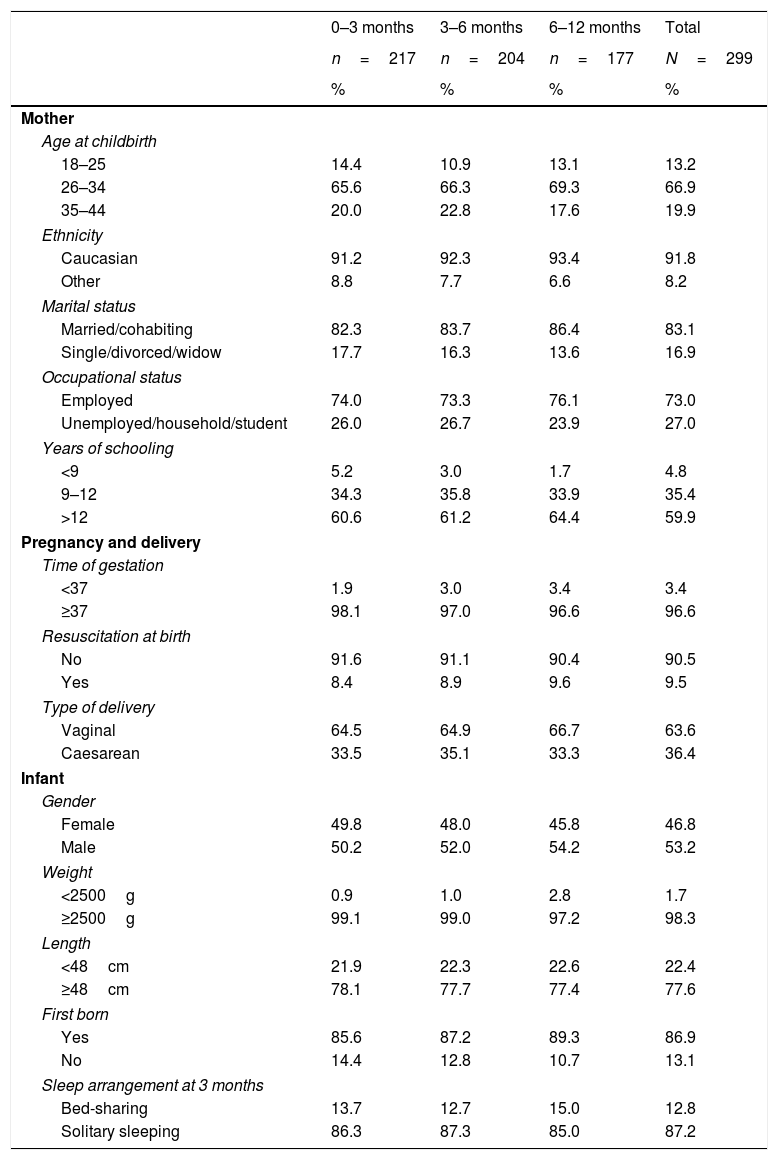
MethodsParticipantsThe sample was comprised of 299 infants aged between 2 weeks and 12 months whose mothers completed the CSHQ.8 Participants took part in a larger longitudinal study. Sample characteristics are presented at Table 1.
Socio-demographic characteristics.
| 0–3 months | 3–6 months | 6–12 months | Total | |
|---|---|---|---|---|
| n=217 | n=204 | n=177 | N=299 | |
| % | % | % | % | |
| Mother | ||||
| Age at childbirth | ||||
| 18–25 | 14.4 | 10.9 | 13.1 | 13.2 |
| 26–34 | 65.6 | 66.3 | 69.3 | 66.9 |
| 35–44 | 20.0 | 22.8 | 17.6 | 19.9 |
| Ethnicity | ||||
| Caucasian | 91.2 | 92.3 | 93.4 | 91.8 |
| Other | 8.8 | 7.7 | 6.6 | 8.2 |
| Marital status | ||||
| Married/cohabiting | 82.3 | 83.7 | 86.4 | 83.1 |
| Single/divorced/widow | 17.7 | 16.3 | 13.6 | 16.9 |
| Occupational status | ||||
| Employed | 74.0 | 73.3 | 76.1 | 73.0 |
| Unemployed/household/student | 26.0 | 26.7 | 23.9 | 27.0 |
| Years of schooling | ||||
| <9 | 5.2 | 3.0 | 1.7 | 4.8 |
| 9–12 | 34.3 | 35.8 | 33.9 | 35.4 |
| >12 | 60.6 | 61.2 | 64.4 | 59.9 |
| Pregnancy and delivery | ||||
| Time of gestation | ||||
| <37 | 1.9 | 3.0 | 3.4 | 3.4 |
| ≥37 | 98.1 | 97.0 | 96.6 | 96.6 |
| Resuscitation at birth | ||||
| No | 91.6 | 91.1 | 90.4 | 90.5 |
| Yes | 8.4 | 8.9 | 9.6 | 9.5 |
| Type of delivery | ||||
| Vaginal | 64.5 | 64.9 | 66.7 | 63.6 |
| Caesarean | 33.5 | 35.1 | 33.3 | 36.4 |
| Infant | ||||
| Gender | ||||
| Female | 49.8 | 48.0 | 45.8 | 46.8 |
| Male | 50.2 | 52.0 | 54.2 | 53.2 |
| Weight | ||||
| <2500g | 0.9 | 1.0 | 2.8 | 1.7 |
| ≥2500g | 99.1 | 99.0 | 97.2 | 98.3 |
| Length | ||||
| <48cm | 21.9 | 22.3 | 22.6 | 22.4 |
| ≥48cm | 78.1 | 77.7 | 77.4 | 77.6 |
| First born | ||||
| Yes | 85.6 | 87.2 | 89.3 | 86.9 |
| No | 14.4 | 12.8 | 10.7 | 13.1 |
| Sleep arrangement at 3 months | ||||
| Bed-sharing | 13.7 | 12.7 | 15.0 | 12.8 |
| Solitary sleeping | 86.3 | 87.3 | 85.0 | 87.2 |
From the 299 mothers that completed the CSHQ at least once when their child was aged between 2 weeks and 12 months, 217 completed the questionnaire when the infant was aged between 2 weeks and 3 months (2–12 weeks, M=5.08, SD=3.58), 204 when the infant was between 3 and 6 months (13–25 weeks, M=14.78, SD=2.49), and 177 when the infant was between 6 and 12 months (26–52 weeks, M=28.82, SD=4.86). The CSHQ was completed in two time-points by 103 mothers (34.4%), and by 98 mothers (32.78%) in three time-points.
No associations were observed between the infants whose mothers completed the CSHQ in the three time-points and the infants whose mothers completed the CSHQ only at one or two time-points regarding socio-demographic characteristics, except for gestational age (χ2[1]=5.15, p=0.023). The group that completed the CSHQ in three time-points presented a higher rate of full-term infants (gestational age≥37 weeks).
ProceduresThis study received previous approval from the Ethical Commissions of all the institutions involved. At the third trimester of pregnancy, 583 women were contacted at two public hospitals in the Northern Portugal, informed about the purposes and procedures of the study, and invited to participate. Women who were not able to read or write Portuguese, multiple births, and with gestational complications were excluded from the study (7.7%). Those who agreed to participate (90.5%) signed an informed consent form.
The CSHQ was sent by email or post to the mothers when their infants were aged 2 weeks, 3 months, 6 months, and 12 months. From the 487 mothers who agreed to participate and signed the informed consent, 299 (61.4%) completed the CSHQ.
The authors of the CSHQ were contacted and after to their permission, the scale was translated into European Portuguese by two independent Portuguese native and English fluent-speaking researchers. The two researchers discussed the translation and another Portuguese native and English fluent-speaking researcher performed a back-translation. The three researchers discussed the back-translation and consensus was reached through discussion.
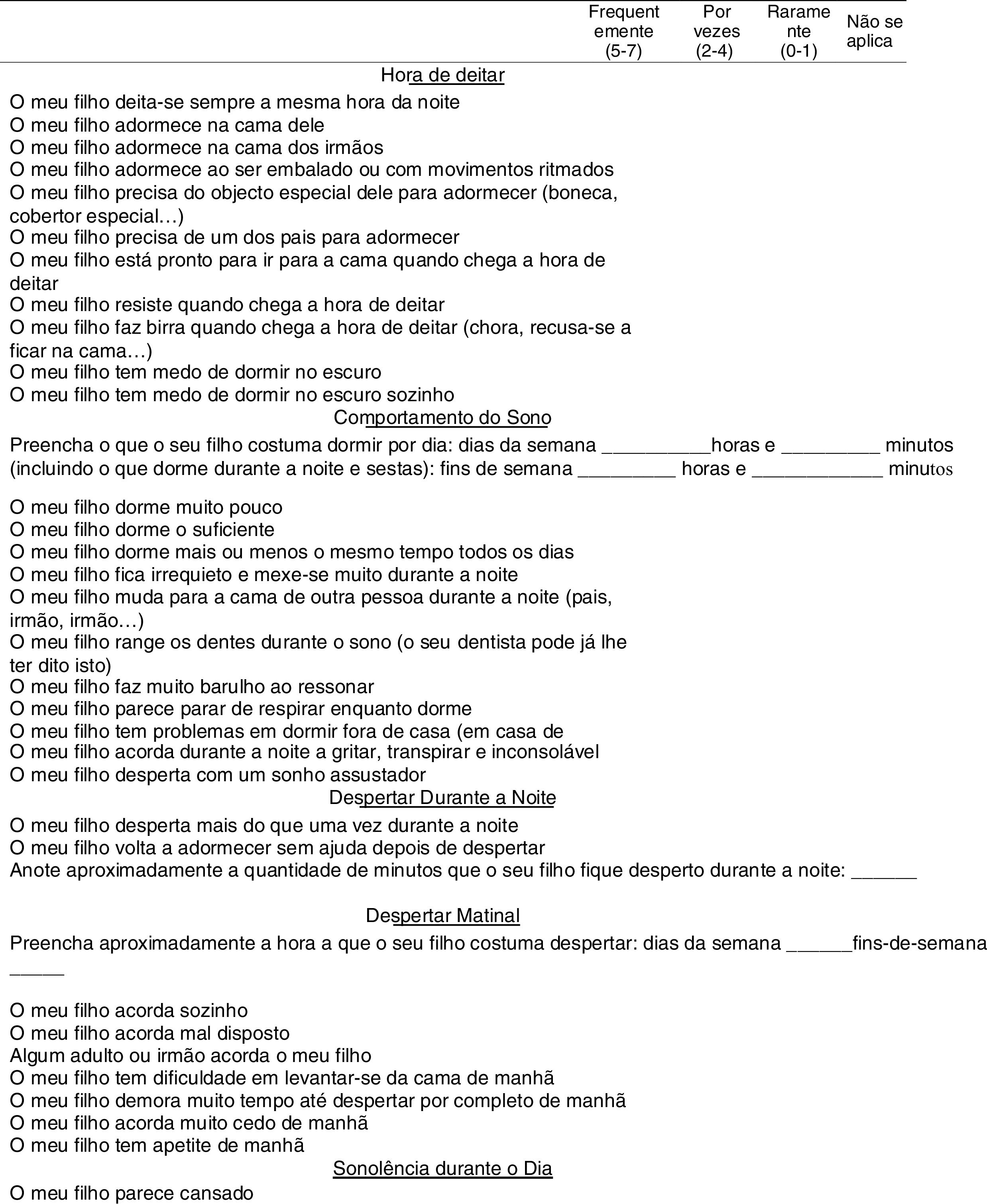
Sleep habits were recorded according to their frequency in a four-point Likert scale: usually (for behaviors occurring five to seven times in a week), sometimes (for behaviors occurring two to four times a week), rarely (for behaviors occurring zero to one time a week), and not applicable (for behaviors that do not apply to infant's age). Following the authors’ instructions, ten items were reverse scored to sum a total score indicative of more sleep problems and to avoid social desirability.
MeasuresThe CSHQThe CSHQ8 is a retrospective questionnaire where parents report their children's sleep habits and behaviors in a typical week, enclosing 48 items scored in a three-point Likert scale: usually, sometimes, and rarely. Higher scores in the CSHQ indicate more sleep problems. Parents also indicate children's evening bedtime, morning wake-up time, and total sleep duration.
CSHQ concurrent validityTo assess the concurrent validity of the CSHQ-I, the Infant Sleep Chronogram23 was used. The Infant Sleep Chronogram was designed for parents to record infant sleep-wake behaviors over a 24-hour period, in a timeline comprised of 30-minute periods from 8 a.m. one day to 8 a.m. the next day. “Daytime” was defined as 8 a.m. to 8 p.m., and “nighttime,” as 8 p.m. to 8 a.m. Based on the mothers’ records, the following variables were coded for the 24-hour period, day, and night: sleep hours, awake hours, awakenings, latency to sleep, and longest sleep period. 24-hour period sleep, awake hours, and awakenings were coded by the sum of the day and night, while the longest sleep period during the 24-hour period was coded using the longest sleep period in the whole day. Latency to sleep was coded by the average number of hours the infant took to fall asleep for each sleep period during the 24-hour period, both day and night. The Infant Sleep Chronogram presented an acceptable internal consistency.23
Data analysisAnalyses were performed using SPSS (IBM SPSS Statistics for Windows, Version 23.0. NY, USA). To examine the CSHQ-I factor structure, exploratory factor analysis (principal axis factoring analysis with orthogonal rotation [varimax]) was performed. Following recommendations, items with a factor loading <0.30 were removed.24 To analyze test-retest reliability, Pearson's correlations were performed between the total scale and subscales 0–3 months and 3–6 months and between 3–6 months and 6–12 months. This analysis was performed in the sample that completed the CSHQ-I in the three time-points. To assess the CSHQ-I (total scale and subscales) internal consistency, analyses of Cronbach's alpha coefficient, item-subscale correlation, and mean item correlation were performed. Following recommendations, good internal consistency was considered when the Cronbach's alpha was >0.70, the item-subscale correlation was >0.30, and the mean inter-item correlation was >0.15.24 To examine the CSHQ-I concurrent validity, Pearson's correlations between the CSHQ-I (total scale and subscales) and the Infant Sleep Chronogram were performed. These analyses were performed in the sample that completed the CSHQ at least one time. A random selection was performed to ensure the inclusion of participants in only one assessment and group equivalence.
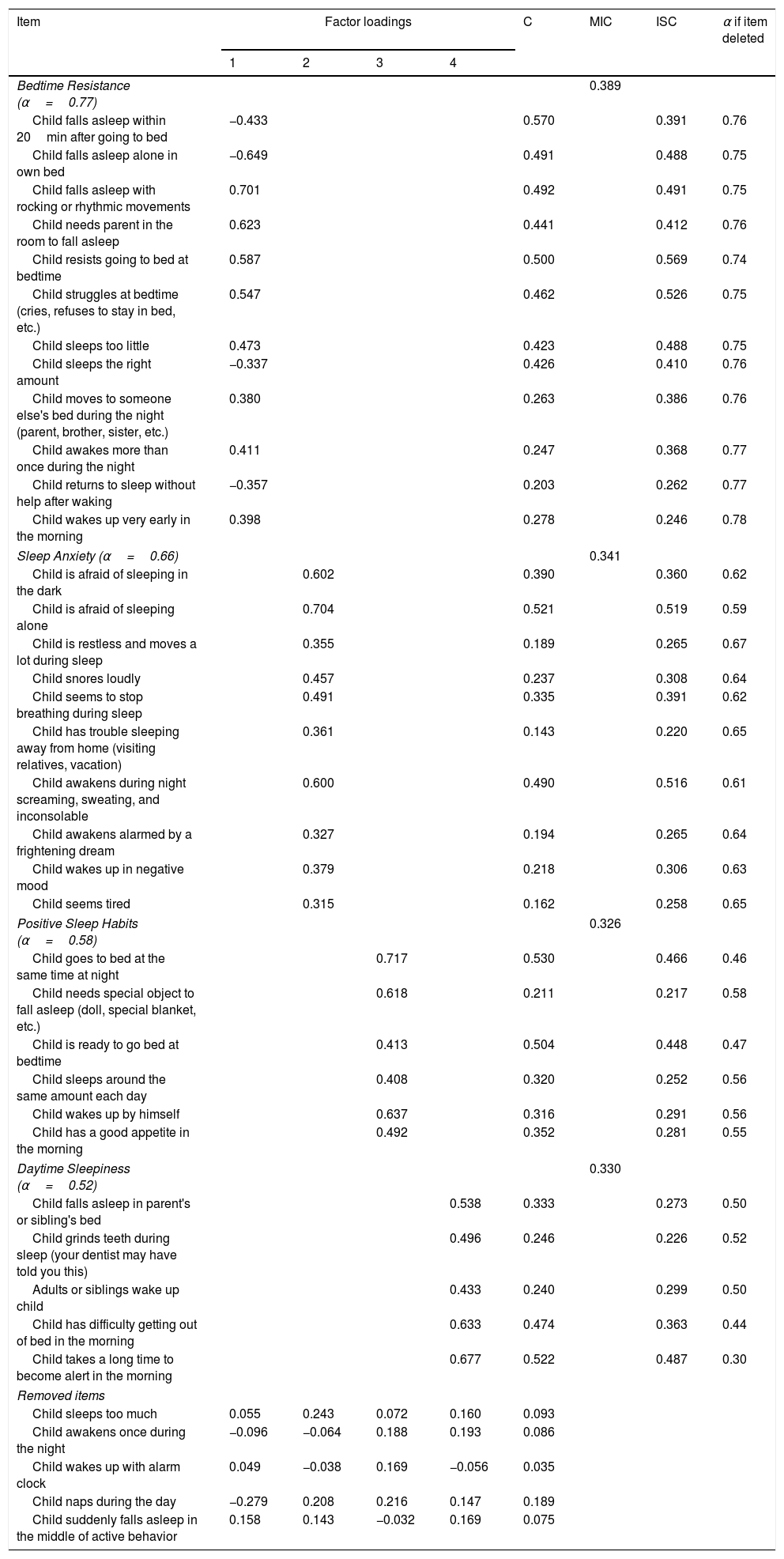
ResultsFactor analysis was performed and, after removing items with factor loadings <0.30, 33 items remained. Bartlett's test of sphericity revealed significant correlations and indicated data adequacy for principal component analyses (χ2[528]=2588.23, p<0.001). The Kaiser–Meyer–Olkin for measuring sample adequacy was 0.71. Four factors were generated, accounting for 35.3% of the total variance. The first factor contributed with 10.5% of the total variance and contained loadings for 12 items measuring Bedtime Resistance; the second factor contributed with 10.5% of the total variance and contained loadings for ten items measuring Sleep Anxiety; the third factor contributed with 8.2% of the total variance and contained loadings for six items measuring Positive Sleep Habits; and the fourth factor contributed with 6.4% of the total variance and contained loadings for five items measuring Daytime Sleepiness (Table 2 and Fig. 1).
CSHQ-I factor analysis – factor loadings, communalities, mean item correlation, item-subscale correlation, and alpha if item was deleted.
| Item | Factor loadings | C | MIC | ISC | α if item deleted | |||
|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||||
| Bedtime Resistance (α=0.77) | 0.389 | |||||||
| Child falls asleep within 20min after going to bed | −0.433 | 0.570 | 0.391 | 0.76 | ||||
| Child falls asleep alone in own bed | −0.649 | 0.491 | 0.488 | 0.75 | ||||
| Child falls asleep with rocking or rhythmic movements | 0.701 | 0.492 | 0.491 | 0.75 | ||||
| Child needs parent in the room to fall asleep | 0.623 | 0.441 | 0.412 | 0.76 | ||||
| Child resists going to bed at bedtime | 0.587 | 0.500 | 0.569 | 0.74 | ||||
| Child struggles at bedtime (cries, refuses to stay in bed, etc.) | 0.547 | 0.462 | 0.526 | 0.75 | ||||
| Child sleeps too little | 0.473 | 0.423 | 0.488 | 0.75 | ||||
| Child sleeps the right amount | −0.337 | 0.426 | 0.410 | 0.76 | ||||
| Child moves to someone else's bed during the night (parent, brother, sister, etc.) | 0.380 | 0.263 | 0.386 | 0.76 | ||||
| Child awakes more than once during the night | 0.411 | 0.247 | 0.368 | 0.77 | ||||
| Child returns to sleep without help after waking | −0.357 | 0.203 | 0.262 | 0.77 | ||||
| Child wakes up very early in the morning | 0.398 | 0.278 | 0.246 | 0.78 | ||||
| Sleep Anxiety (α=0.66) | 0.341 | |||||||
| Child is afraid of sleeping in the dark | 0.602 | 0.390 | 0.360 | 0.62 | ||||
| Child is afraid of sleeping alone | 0.704 | 0.521 | 0.519 | 0.59 | ||||
| Child is restless and moves a lot during sleep | 0.355 | 0.189 | 0.265 | 0.67 | ||||
| Child snores loudly | 0.457 | 0.237 | 0.308 | 0.64 | ||||
| Child seems to stop breathing during sleep | 0.491 | 0.335 | 0.391 | 0.62 | ||||
| Child has trouble sleeping away from home (visiting relatives, vacation) | 0.361 | 0.143 | 0.220 | 0.65 | ||||
| Child awakens during night screaming, sweating, and inconsolable | 0.600 | 0.490 | 0.516 | 0.61 | ||||
| Child awakens alarmed by a frightening dream | 0.327 | 0.194 | 0.265 | 0.64 | ||||
| Child wakes up in negative mood | 0.379 | 0.218 | 0.306 | 0.63 | ||||
| Child seems tired | 0.315 | 0.162 | 0.258 | 0.65 | ||||
| Positive Sleep Habits (α=0.58) | 0.326 | |||||||
| Child goes to bed at the same time at night | 0.717 | 0.530 | 0.466 | 0.46 | ||||
| Child needs special object to fall asleep (doll, special blanket, etc.) | 0.618 | 0.211 | 0.217 | 0.58 | ||||
| Child is ready to go bed at bedtime | 0.413 | 0.504 | 0.448 | 0.47 | ||||
| Child sleeps around the same amount each day | 0.408 | 0.320 | 0.252 | 0.56 | ||||
| Child wakes up by himself | 0.637 | 0.316 | 0.291 | 0.56 | ||||
| Child has a good appetite in the morning | 0.492 | 0.352 | 0.281 | 0.55 | ||||
| Daytime Sleepiness (α=0.52) | 0.330 | |||||||
| Child falls asleep in parent's or sibling's bed | 0.538 | 0.333 | 0.273 | 0.50 | ||||
| Child grinds teeth during sleep (your dentist may have told you this) | 0.496 | 0.246 | 0.226 | 0.52 | ||||
| Adults or siblings wake up child | 0.433 | 0.240 | 0.299 | 0.50 | ||||
| Child has difficulty getting out of bed in the morning | 0.633 | 0.474 | 0.363 | 0.44 | ||||
| Child takes a long time to become alert in the morning | 0.677 | 0.522 | 0.487 | 0.30 | ||||
| Removed items | ||||||||
| Child sleeps too much | 0.055 | 0.243 | 0.072 | 0.160 | 0.093 | |||
| Child awakens once during the night | −0.096 | −0.064 | 0.188 | 0.193 | 0.086 | |||
| Child wakes up with alarm clock | 0.049 | −0.038 | 0.169 | −0.056 | 0.035 | |||
| Child naps during the day | −0.279 | 0.208 | 0.216 | 0.147 | 0.189 | |||
| Child suddenly falls asleep in the middle of active behavior | 0.158 | 0.143 | −0.032 | 0.169 | 0.075 | |||
The CSHQ-I total scale scores were positively correlated between 0–3 months and 3–6 months (r=0.641, p<0.001), and between 3–6 months and 6–12 months (r=0.732, p<0.001). The subscales Bedtime Resistance, Sleep Anxiety, and Positive Sleep Habits scores were also positively correlated between 0–3 months and 3–6 months (r range=0.482–0.558, all p<0.001) and between 3–6 months and 6–12 months (r range=0.430–0.735, all p<0.001). The subscale Daytime Sleepiness scores were positively correlated between 3–6 months and 6–12 months (r=0.229, p=0.023), but not between 0–3 months and 3–6 months (r=0.084, p=0.410).
The CSHQ-I internal consistencyThe CSHQ-I total scale presented a Cronbach's alpha of 0.78. The Cronbach's alphas for the subscales were: Bedtime Resistance (α=0.77), Sleep Anxiety (α=0.66), Positive Sleep Habits (α=0.58), and Daytime Sleepiness (α=0.52). Over half of the items (60.6%) presented an item-subscale correlation >0.30, and the mean item correlation of all subscales was >0.15 (Table 2).
The CSHQ-I intercorrelationsAll subscales scores were significantly correlated with the CSHQ-I total scale score: Bedtime Resistance, Sleep Anxiety, and Daytime Sleepiness were positively correlated with the total scale (r=0.890, p<0.001; r=0.619, p<0.001; and r=0.210, p<0.001, respectively), while Positive Sleep Habits was negatively correlated with the total scale, (r=−0.540, p<0.001). Almost all subscales were significantly correlated: Bedtime Resistance was positively correlated with Sleep Anxiety, (r=0.437, p<0.001), and negatively correlated with Positive Sleep Habits, (r=−0.242, p<0.001); and Sleep Anxiety was positively correlated with Daytime Sleepiness, (r=0.252, p<0.001). No correlations were observed between Bedtime Resistance and Daytime Sleepiness, between Sleep Anxiety and Positive Sleep Habits, and between Positive Sleep Habits and Daytime Sleepiness.
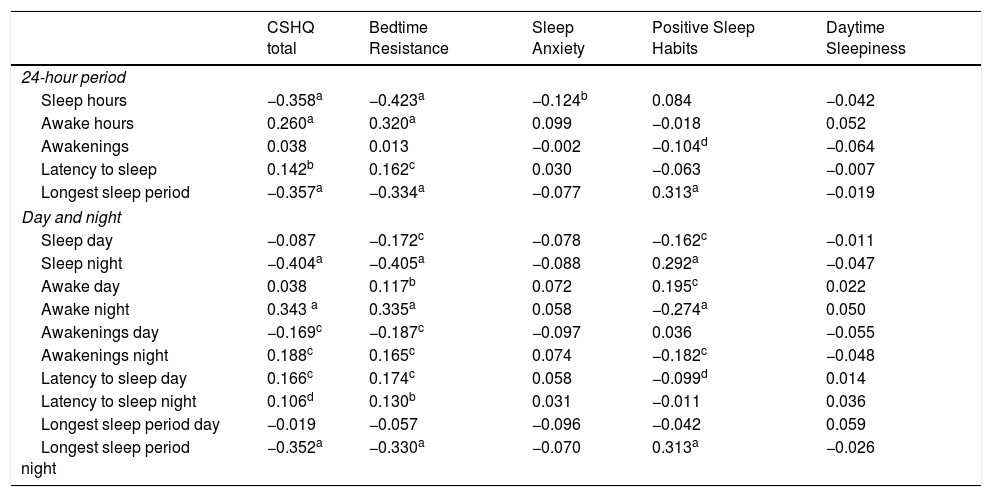
The CSHQ-I concurrent validityThe CSHQ-I (total scale and subscales) and the Infant Sleep Chronogram were assessed for correlation (Table 3).
CSHQ-I concurrent validity – correlations with the Infant Sleep Chronogram.
| CSHQ total | Bedtime Resistance | Sleep Anxiety | Positive Sleep Habits | Daytime Sleepiness | |
|---|---|---|---|---|---|
| 24-hour period | |||||
| Sleep hours | −0.358a | −0.423a | −0.124b | 0.084 | −0.042 |
| Awake hours | 0.260a | 0.320a | 0.099 | −0.018 | 0.052 |
| Awakenings | 0.038 | 0.013 | −0.002 | −0.104d | −0.064 |
| Latency to sleep | 0.142b | 0.162c | 0.030 | −0.063 | −0.007 |
| Longest sleep period | −0.357a | −0.334a | −0.077 | 0.313a | −0.019 |
| Day and night | |||||
| Sleep day | −0.087 | −0.172c | −0.078 | −0.162c | −0.011 |
| Sleep night | −0.404a | −0.405a | −0.088 | 0.292a | −0.047 |
| Awake day | 0.038 | 0.117b | 0.072 | 0.195c | 0.022 |
| Awake night | 0.343 a | 0.335a | 0.058 | −0.274a | 0.050 |
| Awakenings day | −0.169c | −0.187c | −0.097 | 0.036 | −0.055 |
| Awakenings night | 0.188c | 0.165c | 0.074 | −0.182c | −0.048 |
| Latency to sleep day | 0.166c | 0.174c | 0.058 | −0.099d | 0.014 |
| Latency to sleep night | 0.106d | 0.130b | 0.031 | −0.011 | 0.036 |
| Longest sleep period day | −0.019 | −0.057 | −0.096 | −0.042 | 0.059 |
| Longest sleep period night | −0.352a | −0.330a | −0.070 | 0.313a | −0.026 |
The CSHQ-I total scale was negatively correlated with sleep hours during the 24-hour period and during the night, longest sleep period during the 24-hour period and during the night, and awakenings during the day; it was positively correlated with awake hours during the 24-hour period and during the night, latency to sleep during the 24-hour period and during the day, and awakenings during the night. Moreover, it was marginally correlated with latency to sleep during the night. The Bedtime Resistance subscale was negatively correlated with sleep hours during the 24-hour period, during the day, and during the night; longest sleep period during the 24-hour period and during the night; and awakenings during the day. It was positively correlated with awake hours during the 24-hour period, during the day, and during the night; latency to sleep during the 24-hour period, during the day, and during the night; and awakenings during the night. The Sleep Anxiety subscale was negatively correlated with sleep hours during the 24-hour period. Positive Sleep Habits subscale was negatively correlated with sleep hours during the day, awake hours during the night, awakenings during the night; it was positively correlated with sleep hours during the night, awake hours during the day, longest sleep period during the 24-hour period and during the night. Furthermore, it was marginally correlated with awakenings during the 24-hour period, and latency to sleep during the day.
Internal consistency of CSHQ-I for 0–3 months, 3–6 months, and 6–12 monthsIn infants aged 6–12 months, the CSHQ-I total scale presented a Cronbach's alpha of 0.82. The Cronbach's alphas for subscales were: Bedtime Resistance (α=0.79), Sleep Anxiety (α=0.74), Positive Sleep Habits (α=0.45), and Daytime Sleepiness (α=0.41). The mean scores for infants aged 6–12 months were: total scale (M=13.08, SD=7.62), Bedtime Resistance (M=6.77, SD=4.76), Sleep Anxiety (M=1.66, SD=2.32), Positive Sleep Habits (M=8.85, SD=2.11), and Daytime Sleepiness (M=0.44, SD=0.88). In infants aged 3–6 months, the CSHQ-I total scale presented a Cronbach's alpha of 0.78. Two items (“Child falls asleep in parent's or sibling's bed” and “Child grinds teeth during sleep [your dentist may have told you this]”) were removed as they presented no variance in the response, and 31 items remained. The Cronbach's alphas for the subscales were: Bedtime Resistance (α=0.77), Sleep Anxiety (α=0.65), Positive Sleep Habits (α=0.40), and Daytime Sleepiness (α=0.54). The mean scores for infants aged 3–6 months were: total scale (M=13.43, SD=7.04), Bedtime Resistance (M=7.00, SD=4.76), Sleep Anxiety (M=1.52, SD=2.01), Positive Sleep Habits (M=8.27, SD=2.08), and Daytime Sleepiness (M=0.24, SD=0.67). In infants aged 0–3 months, the CSHQ-I total scale presented a Cronbach's alpha of 0.72. The Cronbach's alphas for the subscales were: Bedtime Resistance (α=0.68), Sleep Anxiety (α=.57), Positive Sleep Habits (α=0.61), and Daytime Sleepiness (α=0.46). The mean scores for infants aged 0–3 months were: total scale (M=15.77, SD=6.25), Bedtime Resistance (M=7.64, SD=4.12), Sleep Anxiety (M=1.27, SD=1.74), Positive Sleep Habits (M=6.62, SD=2.57), and Daytime Sleepiness (M=0.35, SD=0.78).
DiscussionThis study proposed the adaptation of the CSHQ for infants aged up to 12 months. Results showed that, generally, the CSHQ-I is a reliable measure to assess sleep problems in infants in this age. Four subscales were proposed, contrary to the CSHQ version for preschool- and school-aged children, where eight factors emerged from a conceptual grouping of items.8 In the CSHQ-I, Bedtime Resistance, Sleep Anxiety, and Daytime Sleepiness subscales were maintained and a new subscale, Positive Sleep Habits, was proposed.
Compared with the CSHQ version for preschool- and school-aged children,8 the Bedtime Resistance subscale maintained four of the six items and added the subscales Sleep Onset Delay and Night Wakings, and items of the subscale Sleep Duration. This subscale appears to cover the most prevalent problems presented from infancy to preschool age: bedtime resistance and frequent night wakings.4,6 These sleep problems are considered in the diagnostic category of Behavioral Insomnia of Childhood (BIC) proposed in the ICSD-2, which is characterized by difficulties in the initiation and maintenance of sleep,25 and the items of the CSHQ-I appear to cover the two types of BIC.25 While the item “Child falls asleep with rocking or rhythmic movements” could be included in the sleep-onset association type, the item “Child resists going to bed at bedtime” could be encompassed in the limit-setting type.
Compared with the CSHQ version for preschool- and school-aged children, the Sleep Anxiety subscale maintained three of the four items and included items from the subscales Parasomnias, Sleep-Disordered Breathing, and Daytime Sleepiness. Despite maintaining the majority of the items, this subscale also included the previous subscales Sleep-Disordered Breathing and Parasomnias, which are not proposed as separate subscales in the CSHQ-I. Moreover, three items of the Parasomnias subscale were removed in the CSHQ-I. This difference may be due to the age range of the infants, as Parasomnias and Sleep-Disordered Breathing are more common in preschool- and school-aged children.26 However, some symptoms of these problems appear to be already present during the first year of age.
The Positive Sleep Habits subscale included items from the subscales Bedtime Resistance, Sleep Duration, and Daytime Sleepiness, as well as three items that were removed from the CSHQ version for preschool- and school-aged children. This new subscale includes items related with bedtime and morning waking habits.
The Daytime Sleepiness subscale maintained three from the eight items and included one item from the Bedtime Resistance and one item from the Parasomnias subscales. The differences between the CSHQ version for preschool- and school-aged children and the CSHQ-I in the Daytime Sleepiness subscale may be due to the age differences. Daytime Sleepiness subscale items present mainly the daytime consequences resulting from sleep disorders.8 Although in the first year infants achieve the developmental task of concentrating their sleep during the night, they still maintain sleep hours during the day,24 and some of the items of Daytime Sleepiness subscale of the CSHQ version for preschool- and school aged children appear to not be applicable to infants.
The Bedtime Resistance and Sleep Anxiety subscales also presented similarities with the two factors presented in a study with infants.18 The Bedtime Resistance subscale maintained eight items from Resist Sleep and Sleep Anxiety subscale maintained four items from Sleep Anxiety.18 Two subscales (Positive Sleep Habits and Daytime Sleepiness) were added in the CSHQ-I.
The CSHQ-I total scale and subscales showed good test-retest reliability. Acceptable test-retest reliability was also showed in the CSHQ version for preschool- and school-aged children.8 The CSHQ-I total scale presented good internal consistency, with a Cronbach's alpha >0.70; over half of the items presenting an item-subscale correlation >0.30, and a mean-item >0.15.24 The Cronbach's alpha of the CSHQ-I is similar to the Portuguese, Indian, and Chinese,9,10,13 and higher than the American and German versions for preschool- and school-aged children.11,12 Cronbach's alpha of the CSHQ-I subscales ranged from 0.52 (Daytime Sleepiness) to 0.77 (Bedtime Resistance). Three subscales presented an internal consistency below the recommended 0.70.24 The subscales Positive Sleep Habits and Daytime Sleepiness presented the lowest internal consistency. That could be explained by the lower number of items and the lower variance presented by these two subscales. This result suggests that both these subscales appear to not be accurate to assess sleep problems in a community sample. This is consistent with a previous study that showed higher internal consistency in clinical samples,8 which could indicate that the CSHQ is more accurate in the assessment of clinical samples.
The CSHQ-I also showed good concurrent validity, with significant associations found with the Infant Sleep Chronogram. However, the subscale Daytime Sleepiness was not significantly correlated and the subscale Sleep Anxiety showed only one significant correlation. This result may suggest that these subscales are not as reliable as the other subscales to measure sleep problems in this age. Good concurrent validity was also observed in the Indian version of the CSHQ for preschool- and school-aged children.8 Infant Sleep Chronogram refers to infant sleep-wake behavior in the previous 24h, while the CSHQ-I refers to sleep habits in the previous week and all the characteristics of sleep-wake behavior occurring within a week could not be gathered with the Infant Sleep Chronogram. As both Infant Sleep Chronogram and CSHQ-I were based in parents’ reports, it would be important to analyze concurrent validity of the CSHQ-I with a more objective measure (e.g., actigraphy) in future research.
Given that infant sleep-wake behavior presents different developmental changes during the first months of life,23 the reliability of the items of the CSHQ-I was also analyzed in infants aged 0–3 months, 3–6 months, and 6–12 months. A good internal consistency was found for the three age ranges in the CSHQ-I total scale. However, most of the subscales for the three ages presented an internal consistency below the recommended 0.70,24 suggesting that these subscales should be used with caution. Two items were found not to be suitable for infants aged 0–3 and 3–6 months, suggesting these items should be removed when applying the CSHQ-I in infants under 6 months.
Further studies are warranted in order to assess CSHQ-I psychometric properties in comparison with a more objective measure or with sleep problems definitions.
This study presents some limitations. The voluntary nature of participation might have biased the results. Significant differences were found between the mothers that completed the CSHQ in the three time-points and those who completed the CSHQ at only one or two time-points on gestational age. The sample also presented homogeneity, considering the low rate of preterm infants, non-first-time infants, and infants with low birth weight and length.
This study provides the psychometric characteristics of the CSHQ-I, suggesting this instrument appears to be useful for clinicians to assess sleep problems and to detect potential specific sleep difficulties in infants under 12 months. This study also provides preliminary guidelines for how to use this instrument in infants. However, some of the subscales appear to not be accurate in assessing sleep problems in a community sample and caution should be taken when using them.
FundingThis research was supported by FEDER Funds through the Programa Operacional Factores de Competitividade – COMPETE and by National Funds through FCT – Fundação para a Ciência e a Tecnologia under the project: PTDC/SAU/SAP/116738/2010 and SFRH/BD/113005/2015 grant.
This study was conducted at Psychology Research Centre (UID/PSI/01662/2013), University of Minho, and supported by the Portuguese Foundation for Science and Technology and the Portuguese Ministry of Education and Science through national funds and co-financed by FEDER through COMPETE2020 under the PT2020 Partnership Agreement (POCI-01-0145-FEDER-007653).
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Dias CC, Figueiredo B, Pinto TM. Children's Sleep Habits Questionnaire – Infant Version. J Pediatr (Rio J). 2018;94:146–154.