To assess bone mineral density (BMD) in children with idiopathic nephrotic syndrome (NS) and normal glomerular filtration rate (GFR).
MethodsCross-sectional case–control study carried out on 50 children: 25 cases of NS (16 steroid-sensitive [SSNS] and nine steroid-resistant [SRNS] under follow up in the pediatric nephrology unit of Menoufia University Hospital, which is tertiary care center, were compared to 25 healthy controls with matched age and sex. All of the participants were subjected to complete history taking, thorough clinical examination, laboratory investigations (serum creatinine, blood urea nitrogen [BUN], phosphorus [P], total and ionized calcium [Ca], parathyroid hormone [PTH], and alkaline phosphatase [ALP]). Bone mineral density was measured at the lumbar spinal region (L2–L4) in patients group using dual-energy X-ray absorptiometry (DXA).
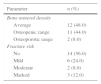
ResultsTotal and ionized Ca were significantly lower while, serum P, ALP, and PTH were higher in SSNS and SRNS cases than the controls. Osteopenia was documented by DXA scan in 11 patients (44%) and osteoporosis in two patients (8%). Fracture risk was mild in six (24%), moderate in two (8%), and marked in three (12%) of patients.
ConclusionBone mineralization was negatively affected by steroid treatment in children with NS.
Avaliar a densidade mineral óssea (DMO) em crianças com síndrome nefrótica idiopática (SNI) e com taxa de filtração glomerular (TFG) normal.
MétodosO estudo transversal de caso-controle foi realizado com 50 crianças: 25 casos de SNI [16 sensíveis a esteroides (SNSE) e nove resistentes a esteroides (SNRE) com acompanhamento na unidade de nefrologia pediátrica do hospital da Menoufia University, centro de cuidados terciário] foram comparados com 25 controles saudáveis do grupo de controle com idade e sexo equivalentes. Todos os participantes foram submetidos a anamnese completa, exame clínico completo, exames laboratoriais [creatinina sérica, nitrogênio ureico no sangue (BUN), fósforo (P), cálcio (Ca) total e ionizado, paratormônio (PTH) e fosfatase alcalina (ALP)]. A densidade mineral óssea foi mensurada na região da coluna lombar (L2-L4) no grupo de pacientes usando a absorciometria por raio-X de dupla energia (DXA).
ResultadosOs níveis de cálcio total e ionizado eram significativamente menores, ao passo que o fósforo sérico, a FA e o PTH eram maiores em casos de SNSE e SNRE que nos controles. A osteopenia foi documentada pelo exame DXA em 11 pacientes (44%) e a osteoporose, em dois pacientes (8%). O risco de fratura era leve em seis (24%), moderado em dois (8%) e acentuado em três (12%) dos pacientes.
ConclusãoA mineralização dos ossos foi afetada negativamente pelo tratamento com esteroides em crianças com SN.
Childhood nephrotic syndrome (NS) is defined by nephrotic-range proteinuria, generalized edema, hypoalbuminuria, and hyperlipidemia with normal renal function.1 Idiopathic nephrotic syndrome (INS) is the most frequent renal disease in children.2 Childhood NS typically follows a relapsing-remitting course, often requiring recurrent courses of glucocorticoids (GC), but with low systemic inflammation during remission.3
Bone mass deposition begins during fetal life and continues during infancy and adolescence, stabilizing at the beginning of adulthood.4 During childhood and adolescence, skeletal modeling results in sex- and maturation-specific increases in bone density. Metabolic bone disease (MBD) is characterized by changes in skeletal mineralization due to poor bone mineral content (BMC).5 Children may be especially vulnerable to the effects of GC on bone formation and peak bone mass.6
Prednisone is the first-line treatment for INS to induce remission, to prevent relapses and to avoid side effects of the disease.7 Prolonged administration of prednisone interferes with growth and bone mineralization, and has deleterious effect on basic cellular mechanisms that are important in the development and maintenance of bone strength.7,8 Steroids are known to cause osteoporosis and affect BMC and bone mineral density (BMD) in children.9 Glucocorticoids have a suppressive effect on osteoblastogenesis in the bone marrow and promote the apoptosis of osteoblasts and osteocytes, thus leading to decreased bone formation.10 There is some evidence to suggest that GC may increase bone resorption by extending the lifespan of pre-existing osteoclasts.11 Glucocorticoids may also promote calcium loss through the kidneys and gut, and this negative calcium balance can itself lead to increased bone remodeling and osteoclastic activity due to secondary hyperparathyroidism.12
Children with INS are at risk for MBD, accompanied by important alterations of mineral and bone metabolism.13
Therefore, it was hypothesized that patients with NS would have BMD deficits when compared to their peers. This study was designed to determine BMD in children with INS and normal glomerular filtration rate (GFR).
MethodsThis study was carried out on 50 children after approval of the Ethical Committee of Faculty of Medicine, Menoufia University, and a written consent was obtained from the guardians of patients and controls. Children were divided into two groups:
Group IIncluded 25 children aged 1–15 years who fulfill the clinical criteria for INS (heavy proteinuria>40mg/m2/h, hypoalbuminemia<2.5g/L, hypercholesterolemia>250mg/dL, and edema) with normal renal function (normal glomerular filtration by Schwartz formula).14 Patients with secondary NS, with other conditions unrelated to NS that could affect bone health, and patients who received prior medication for osteoporosis or vitamin D preparations before or during the study were excluded.
All of the children with INS were treated according to the standard protocol.14 The initial therapy consisted of daily prednisone 60mg/m2/day (80mg daily max) for four weeks, followed by 40mg/m2/day given every other day as a single daily dose for at least four weeks. The alternate-day dose was then slowly tapered and discontinued over the next one to two months. Relapses (proteinuria>40mg/h/m2 for three consecutive days after having been in remission) were treated with 60mg/m2/day in a single morning dose until the child entered remission (proteinuria<4mg/m2/h for three consecutive days). Dietary advice was given families to provide their children a diet rich in calcium, adequate caloric intake, adequate protein (1g/kg/d), with no added salt to limit fluid overload. The prednisone dose was then changed to alternate-day dosing as noted with initial therapy, and gradually tapered over four to eight weeks. Patients with INS were classified into three groups depending on their response to GC therapy: [i] steroid-dependent NS: two consecutive relapses during corticosteroid therapy or within 14 days after cessation of therapy (SDNS: 14 patients); [ii] steroid-resistant NS: failure to achieve remission following four weeks of prednisone 60mg/m2 followed by three methylprednisolone pulses (SRNS: nine patients); [iii] infrequent relapsers: less than four times in a 12-month period (IFR: two patients).14
Group IITwenty-five apparently healthy children of matched age and sex were enrolled as a control group. They were chosen from the outpatient pediatric clinic, complaining from acute transient illnesses.
All patients and controls were subjected to complete history taking, including type of treatment, its duration, and dates and number of relapses. The cumulative doses of prednisone that each patient received during therapy were calculated from their medical charts. Thorough clinical examination including height, weight, and body mass index (BMI) were recorded and plotted on World Health Organization standard deviation curves. Laboratory investigations included serum creatinine, blood urea nitrogen (BUN, phosphorous (P), calcium (total and ionized; Ca), parathyroid hormone (PTH), and alkaline phosphatase (ALP) were estimated.
BMD was measured at the lumbar spinal region (L2–L4) in patients group using dual-energy X-ray absorptiometry (DXA) (Challenger Envision osteodensitometer, DMS, England). BMD was classified according to Bakr15 on the basis of BMD Z-score. Scores were calculated from the following equation: Z-score=(BMD [g/cm3] of the patient — BMD predicted for age and sex/SD for BMD [age, sex, and height matched]). A patient was considered osteopenic if the Z-score was <–1.0. If the Z-score was ≤–2.5, the patient was classified as having severe osteopenia (osteoporosis). Chance of osteoporotic fracture <10%, 10–19%, and >20% were considered low, medium, and high risk of fracture, respectively.16
Statistical analysisThe results were analyzed statistically using SPSS software (version 17; SPSS Inc., Chicago, IL, USA). Statistical analysis was performed using one-way ANOVA (F test) with post hoc test, Student's t-test, and chi-squared test. Correlations were determined by Pearson correlation and linear regression analysis. Continuous variables were presented as mean±standard deviation, while for categorical variables, numbers (%) were used. Significance was considered at p-value <0.05.
ResultsDemographic and anthropometric characteristics of the participants with steroid-sensitive nephrotic syndrome (SSNS), steroid-resistant nephrotic syndrome (SRNS), and the control groups are summarized in Table 1. Weight and BMI Z-scores were significantly higher in the SSNS and SRNS patients than the controls, with no significant difference between them regarding the height Z-scores. In terms of serum markers of bone turnover, serum Ca (total and ionized) were significantly lower, while serum phosphorus and alkaline phosphatase were significantly higher in both SSNS and SRNS patients vs. the controls. Bone aches were found in eight patients (32%).
Demographic and clinical data of the studied groups.
| Parameter/group | SSNS | SRNS | Control | F test | Post hoc test |
|---|---|---|---|---|---|
| Number types | 16 | 9 | 25 | ||
| 14 SDNS | |||||
| 2 IFRNS | |||||
| Zero FRNS | |||||
| Age (years): | 7.62±2.78 | 7.78±4.49 | 8.04±3.37 | 0.076 | F1=0.160 |
| x¯±SD | F2=0.26 | ||||
| F3=0.420 | |||||
| Sex:n(%) | |||||
| Male | 13 (81.3) | 2 (22.2) | 13 (52.0) | x2=0.32 | |
| Female | 3 (18.7) | 7 (77.8) | 12 (48.0) | ||
| Weight (Z-score): | 1.23±1.57 | 1.42±1.01 | −0.24±1.32 | 8.09a | F1=0.478 |
| x¯±SD | F2=4.785a | ||||
| F3=4.453a | |||||
| Height (Z-score): | −0.54±1.35 | −0.52±1.05 | −0.31±1.15 | 0.206 | F1=0.063 |
| x¯±SD | F2=0.829 | ||||
| F3=0.615 | |||||
| BMI (Z-score): | 0.76±0.83 | 0.90±0.92 | −0.34±1.45 | 5.189a | F1=0.369 |
| x¯±SD | F2=3.838a | ||||
| F3=3.557a | |||||
| Serum creatinine (0.3–1.5mg/dL): | 0.59±0.13 | 0.60±0.14 | 0.56±0.18 | 0.512 | F1=0.297 |
| x¯±SD | F2=1.097 | ||||
| F3=1.223 | |||||
| BUN (7–22mg/dL): | 19.94±4.46 | 20.00±3.35 | 11.56±3.44 | 2.163 | F1=0.057 |
| x¯±SD | F2=2.572 | ||||
| F3=2.179 | |||||
| Total calcium (8.8–10.8mg/dL): | 9.24±0.87 | 9.37±0.74 | 10.18±0.52 | 10.69a | F1=0.130 |
| x¯±SD | F2=5.940a | ||||
| F3=4.810a | |||||
| Ionized calcium (4.4–5.4mg/dL): | 1.23±0.06 | 1.21±0.06 | 5.02±0.31 | 89.53a | F1=0.328 |
| x¯±SD | F2=75.617a | ||||
| F3=62.629a | |||||
| Serum phosphorus (4.5–5.5mg/dL): | 5.01±0.63 | 4.84±0.32 | 4.62±0.64 | 5.01b | F1=0.961 |
| x¯±SD | F2=4.314b | ||||
| F3=2.523 | |||||
| Alkaline phosphatase (<300U/L): | 156.81±51.91 | 171.89±105.39 | 68.00±29.89 | 18.76a | F1=0.913 |
| x¯±SD | F2=7.182a | ||||
| F3=6.894a | |||||
| PTH (9–52pg/mL): | 44.06±27.69 | 48.78±25.31 | 28.48±12.96 | 4.78b | F1=0.781 |
| x¯±SD | F2=3.434b | ||||
| F3=3.667b |
SSNS, steroid-sensitive nephrotic syndrome; SRNS, steroid-resistant nephrotic syndrome; F, one way ANOVA test; χ2, chi-squared test; x¯±SD, mean±standard deviation; PTH, parathyroid hormone; BMI, body mass index; BUN, blood urea nitrogen; F1, difference between SSNS and SRNS; F2, difference between SSNS and control; F3, difference between SRNS and control.
No significant statistical differences were found between SSNS and SRNS patients regarding the drugs received and DXA measurements (Table 2). Seventy-two percent of SSNS patients received immunosuppressive drugs, as follows: 48% were cyclosporine therapy, 4% on Mycophenolate Mofetil, 8% on cyclophosphamide, and 12% on mixed immunosuppressive therapy.
Drug received and DXA scan among patient groups.
| Parameter/group | SSNS | SRNS | Student's t-test | p-Value |
|---|---|---|---|---|
| Drugs received | ||||
| Steroid duration (years) | 2.55±2.49 | 2.56±1.62 | 0.02 | 0.49 |
| Cumulative steroid dose(mg/m2) | 17,300.94±17,221.76 | 11,570.00±6,776.68 | 0.95 | 0.35 |
| Immunosuppressive drugs | No (%) | No (%) | ||
| Yes | 9 (56%) | 9 (100%) | ||
| No | 7 (44%) | 0 (0%) | ||
| DXA scan | ||||
| BMD | 0.61±0.10 | 0.56±0.24 | 0.81 | 0.42 |
| Z-score | −1.11±1.08 | −1.00±0.86 | 0.27 | 0.79 |
SSNS, steroid-sensitive nephrotic syndrome; SRNS, steroid-resistant nephrotic syndrome; BMD, bone mineral density; DXA, dual-energy X-ray absorptiometry.
Bone mineral density (BMD) and fracture risk between nephrotic syndrome participants are given in Table 3. Osteopenia was documented by DXA scan in 11 patients (44%) (seven SDNS, four SRNS), and osteoporosis in two patients (8%) (two SDNS). Fracture risk was mild in six patients (24%) (one IFRNS, two SDNS, three SRNS), moderate in two (8%) (one SDNS, one SRNS), and marked in three (12%) (two SDNS, one SRNS).
A significant statistical correlation was observed between BMD Z-scores and age of patients (r=0.43; p<0.05), weight Z-score (r=0.56; p<0.001), height Z-score (r=0.57; p<0.05), BMI (r=0.34; p<0.05), duration (r=−0.46; p<0.05), and cumulative dose of GC therapy(r=−0.88; p<0.001). Linear regression analyses in Table 4 show that the steroid cumulative dose was the only significant independent risk factor.
Un-standardized and standardized linear regression coefficients for correlations between Z-score and some studied parameters.
| Parameter | Un-standardized coefficients B | Standardized coefficients B | p-Value |
|---|---|---|---|
| Age (years) | 0.06 | 0.19 | >0.05 |
| BMI | 0.103 | 0.268 | >0.05 |
| Steroid duration (years) | 0.05 | 0.11 | >0.05 |
| Cumulative steroid dose (mg/m2) | 0.12 | 0.23 | <0.05a |
BMI, body mass index.
Although GCs are the treatment of choice for children with idiopathic NS, obesity and bone mineralization side effects should be considered.7 In this study, the analyses clearly showed an impact of GCs on body weight and BMI in nephrotic syndrome participants. Not surprisingly, the SSNS and SDNS patients had significantly higher weight and BMI Z-scores than the controls, but with insignificant statistical difference between SSNS and SDNS. Similar results were reported by Lestari et al.17 and Ribeiro et al.7 in their analyses of obesity in SSNS and SDNS. The use of high-dose and long-term steroids leads to increased food intake and inhibited energy expenditure through stimulation of neuropeptide-Y and inhibited release of corticotrophin hormone. The process triggers an anabolic process and leads to obesity.14 Hypocalcemia in patients with NS reported in this study was in line with Koşan et al.18 GCs cause hypocalcemia by decreased Ca adsorption from gut and kidneys.7
However, some studies have reported normal serum calcium levels in children with NS due to increased PTH.19
There were significant elevated levels of serum P, ALP, and PTH in patients with NS vs. controls. These results are in accordance with Pańczyk-Tomaszewska et al.19 and Esmaeeili et al.20 Koşan et al.18 suggested that GCs indirectly affect bone by reduced intestinal calcium absorption and increased urinary calcium losses. Hyperparathyroidism reported in this study was likely due to hypocalcemia induced by GCs; high levels of PTH are known to induce reabsorption of Ca from bone, as mentioned by Aceto et al.21 Bone-specific ALP, which is one of the isoenzymes, is produced by osteoblasts and is a good marker of bone formation22; it was higher in the patients than in healthy children. Its increase during GCs therapy in children with NS was also found by Koşan et al.18 This elevation may be related to increased bone turnover and improvement of massive proteinuria.
This study has reported adverse effect of GCs on the BMD; GC therapy was associated with decreased BMD Z-score, osteoporosis, and an increased risk of fracture in nephrotic syndrome children, with insignificant statistical difference between SSNS and SRNS. Indeed, linear correlation between the cumulative dose of GCs and BMD was recorded. These results were in agreement with those reported by Pańczyk-Tomaszewska et al.,19 who concluded that children with NS treated with corticosteroids are at risk of bone mass loss. Also, Aceto et al.21 showed that GCs reduced BMD Z-score in SSNS, and that BMD Z-score significantly correlates with the total dosage of prednisone.
Canalis23 elucidated that corticosteroids suppress the differentiation of osteoblastic cells and enhance the apoptosis of mature osteoblasts, which result in a decrease of bone formation and loss of BMD. It has also been reported that steroid therapy can cause osteoporosis or exacerbate a pre-existing osteoporotic condition, leading to pathologic fractures.24 Basiratnia et al.25 concluded that bone loss can occur in some steroid-dependent nephrotic patients, especially those with a higher cumulative dose of steroid; higher cumulative doses were associated with more steroid consumption and consequently more bone loss.
It was concluded that osteopenia assessed by DXA was frequent in children with NS, especially those administered higher doses of steroids (SDNS or SRNS). Bone mineralization was negatively affected by steroid treatment in children with NS. The present study had some limitations, such as the small number of patients and short duration available for the study. Therefore, the authors recommend further studies with a larger sample size and longer duration. Regular BMD evaluation should be performed on NS children, and an appropriate therapeutic approach should be planned.
Conflicts of interestThe authors declare no conflicts of interest.
The authors would like to thank Prof. Mohamed Hamed Bahbah, Head and Creator of the pediatric nephrology unit, Menoufia University, Egypt.
Please cite this article as: El-Mashad GM, El-Hawy MA, El-Hefnawy SM, Mohamed SM. Bone mineral density in children with idiopathic nephrotic syndrome. J Pediatr (Rio J). 2017;93:142–7.