To systematically review the evidence about the impact of nutritional status in critically-ill pediatric patients on the following outcomes during hospitalization in pediatric intensive care units: length of hospital stay, need for mechanical ventilation, and mortality.
Data sourceThe search was carried out in the following databases: Lilacs (Latin American and Caribbean Health Sciences), MEDLINE (National Library of Medicine United States) and Embase (Elsevier Database). No filters were selected.
ResultsA total of seven relevant articles about the subject were included. The publication period was between 1982 and 2012. All articles assessed the nutritional status of patients on admission at pediatric intensive care units and correlated it to at least one assessed outcome. A methodological quality questionnaire created by the authors was applied, which was based on some references and the researchers’ experience. All included studies met the quality criteria, but only four met all the items.
ConclusionThe studies included in this review suggest that nutritional depletion is associated with worse outcomes in pediatric intensive care units. However, studies are scarce and those existing show no methodological homogeneity, especially regarding nutritional status assessment and classification methods. Contemporary and well-designed studies are needed in order to properly assess the association between children's nutritional status and its impact on outcomes of these patients.
Revisar, de forma sistemática, as evidências acerca do impacto do estado nutricional de pacientes pediátricos críticos sobre os seguintes desfechos durante a internação em Unidades de Terapia Intensiva Pediátrica: Tempo de internação, necessidade de ventilação mecânica e mortalidade.
Fonte de dadosA busca foi realizada nas seguintes bases de dados: Lilacs (Literatura Latino-Americana e do Caribe em Ciências da Saúde), Medline(National Library of Medicine Estados Unidos), e Embase (Elsevier Base de Dados). Não houve seleção de filtros.
ResultadosForam incluídos sete artigos relevantes sobre o tema. O período de publicação variou entre 1982 e 2012. Todos avaliam o estado nutricional de pacientes no momento da internação em Terapia Intensiva Pediátrica e relacionam com pelo menos um desfecho estudado. Foi aplicado um questionário de qualidade metodológica criado pelos autores. Ele foi baseado em algumas referências e experiência dos pesquisadores. Todos os estudos incluídos alcançaram os critérios de qualidade, porém apenas quatro, atenderam à todos os itens.
ConclusãoOs estudos incluídos nesta revisão sugerem que a depleção do estado nutricional está relacionado com piores desfechos em Terapia Intensiva Pediátrica. Porém os estudos são escassos, e os existentes, não tem uniformidade metodológica, em especial nos métodos de avaliação e classificação do estado nutricional. São necessários estudos atuais e bem delineados com o objetivo de avaliar adequadamente esta relação entre o estado nutricional de crianças e sua repercussão nos desfechos destes pacientes.
Critically-ill pediatric patients can have a number of organic alterations, leading to a state of metabolic stress. Therefore, in many cases, the nutritional needs of these patients can be increased.1 The inadequate supply of nutrients can result in worsened nutritional state leading to malnutrition, which has been associated in several studies with increased mortality and hospitalization time, as well as a higher number of organ dysfunctions and complications.2,3 The analysis of the cumulative protein calorie deficit in children admitted to a pediatric intensive care unit (PICU) in the Netherlands showed a significant association between this deficit and reduced Z-score for weight and arm circumference.4
There are many barriers to adequate nutritional supply in the PICU, which contributes to nutritional status deterioration. Among them, the most often mentioned in the literature are: gastrointestinal disorders, pause for procedures, and fluid restriction; however, to what extent these barriers can be preventable is a matter of debate.5,6
This group of critically-ill patients is extremely vulnerable. Their nutritional status at admission and its possible deterioration during hospitalization can be a predictor of worse outcomes.7–9
This study aimed to systematically review the evidence about the impact of nutritional status in critically-ill pediatric patients on the following outcomes during PICU hospitalization: length of hospital stay, need for mechanical ventilation (MV), and mortality.
MethodsData sourceA research protocol was developed, in which the authors defined the aim, keywords, search strategies, database definition, inclusion and exclusion criteria, and methodology to be used by the reviewers. The search was carried out in the following databases: Lilacs, Medline and Embase. No filters were selected.
DescriptorsThe descriptors used for the search were: Nutritional Status (Estado Nutricional) and Intensive Care Units Pediatric (Unidade de Terapia Intensiva Pediátrica). The combination of descriptors for the Lilacs and MEDLINE databases was: “Nutritional Status” AND “Intensive Care Units Pediatric” For the Embase database, the following combination was used: “Nutritional Status” AND ((Intensive Care Units AND Pediatric) OR (Intensive Care Units AND Child*)).
Inclusion criteriaOriginal studies conducted in patients aged between 1 month and 18 years, admitted to a PICU, that assessed the association between nutritional status of these patients and at least one of the following outcomes: mortality, hospital length of stay, and need for and/or time of MV.
Exclusion criteriaStudies conducted in a neonatal intensive care unit, articles without full text, review articles, letters to the editor, case reports, and studies that did not address the issue by not performing nutritional assessment and associating it to at least one outcome of interest were excluded.
Study selectionThe search was performed by one investigator using the predefined keywords. The initial selection was performed by two blinded researchers, in compliance with the inclusion and exclusion criteria described in the study protocol.
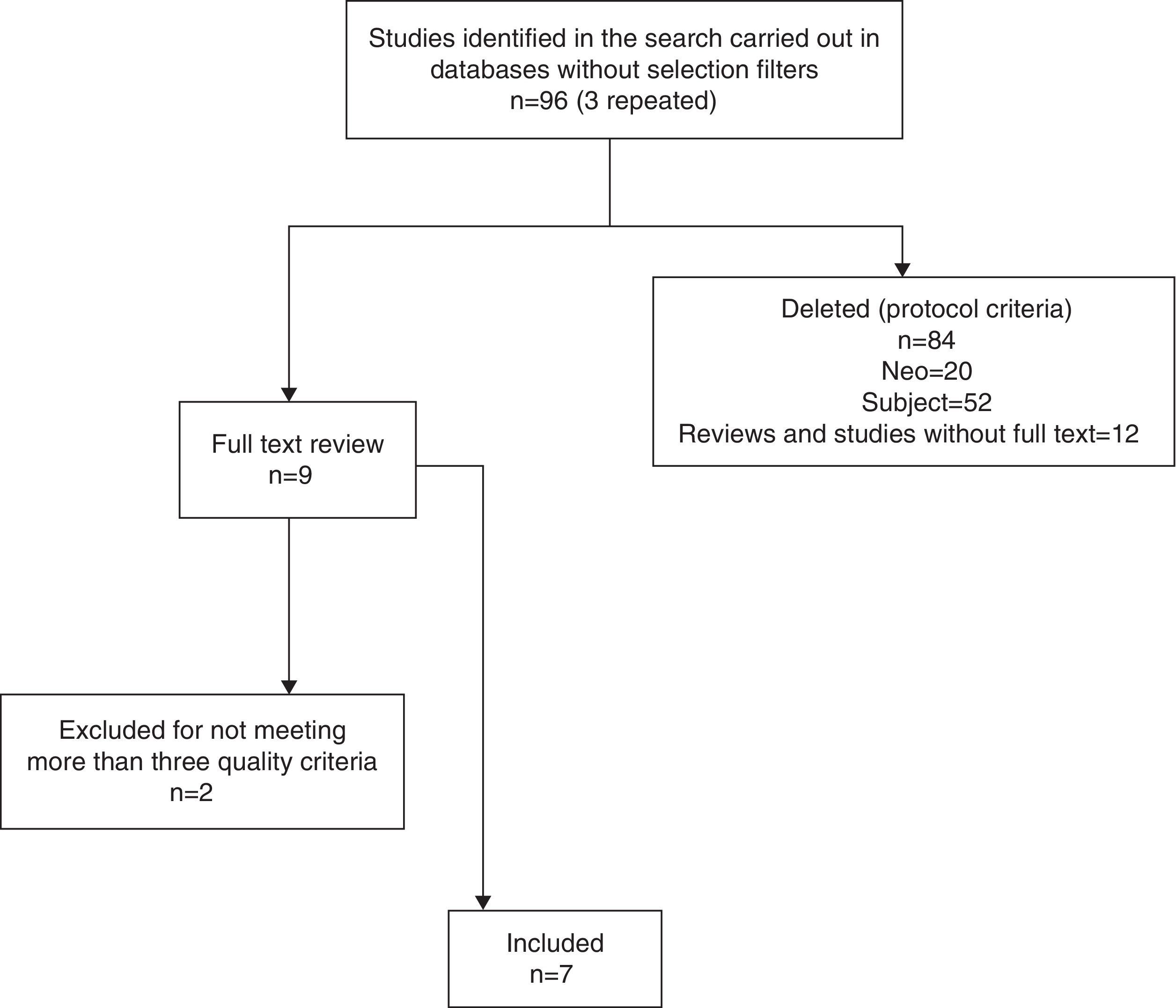
Firstly, articles were screened by reading the title and abstract. When the title and the abstract did not offer enough clarification, the authors searched for the full article. The disagreements were resolved by consensus, together with a third researcher. After that, the full text of all articles included was obtained and the quality protocol created by the authors was applied. Fig. 1 shows the steps of studies selection until the final inclusion.
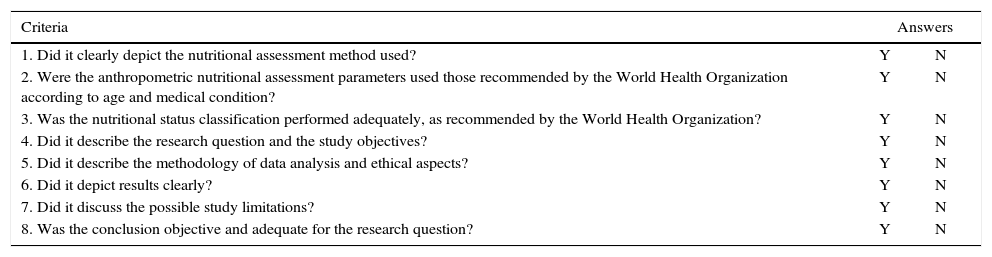
Study quality assessmentAfter the studies were selected and their full texts were obtained, the methodological quality questionnaire was applied, which was created based on two references and the researchers’ experience.10,11 To contemplate the technical issues, the authors considered the recommendations on nutritional status assessment and classification of the World Health Organization (WHO), according to the year of study publication. The questions used in the quality protocol are shown in Table 1.
Quality criteria.
| Criteria | Answers | |
|---|---|---|
| 1. Did it clearly depict the nutritional assessment method used? | Y | N |
| 2. Were the anthropometric nutritional assessment parameters used those recommended by the World Health Organization according to age and medical condition? | Y | N |
| 3. Was the nutritional status classification performed adequately, as recommended by the World Health Organization? | Y | N |
| 4. Did it describe the research question and the study objectives? | Y | N |
| 5. Did it describe the methodology of data analysis and ethical aspects? | Y | N |
| 6. Did it depict results clearly? | Y | N |
| 7. Did it discuss the possible study limitations? | Y | N |
| 8. Was the conclusion objective and adequate for the research question? | Y | N |
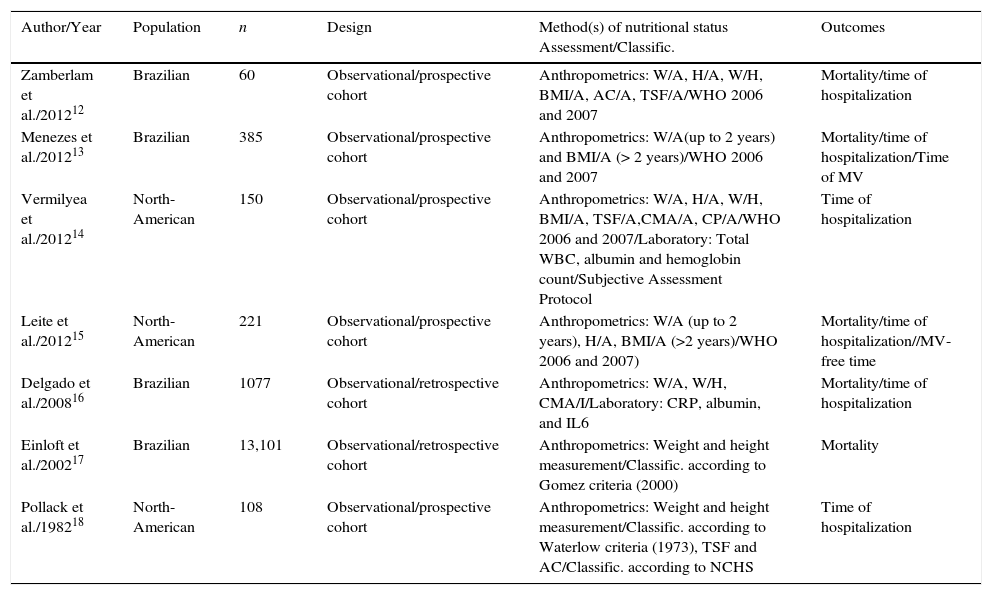
Seven relevant articles on the topic were included. The publication period ranged from 1982 to 2012. All studies assessed the nutritional status of patients on admission at the PICU and correlated it to at least one assessed outcome. Three studies assessed groups of patients in the PICU with specific health conditions (ketoacidosis, hyper- and hypoglycemia, and liver transplant), while the others assessed nutritional profile as a primary or secondary objective and correlated it to the outcomes.
All included studies met the quality criteria, but only four met all items. Nonetheless, those that did not meet up to three items were included, as the authors believed they contributed as evidence for the discussions about the studied subject. Table 2 shows a summary of the included studies.12–18
Summary of included studies.
| Author/Year | Population | n | Design | Method(s) of nutritional status Assessment/Classific. | Outcomes |
|---|---|---|---|---|---|
| Zamberlam et al./201212 | Brazilian | 60 | Observational/prospective cohort | Anthropometrics: W/A, H/A, W/H, BMI/A, AC/A, TSF/A/WHO 2006 and 2007 | Mortality/time of hospitalization |
| Menezes et al./201213 | Brazilian | 385 | Observational/prospective cohort | Anthropometrics: W/A(up to 2 years) and BMI/A (> 2 years)/WHO 2006 and 2007 | Mortality/time of hospitalization/Time of MV |
| Vermilyea et al./201214 | North-American | 150 | Observational/prospective cohort | Anthropometrics: W/A, H/A, W/H, BMI/A, TSF/A,CMA/A, CP/A/WHO 2006 and 2007/Laboratory: Total WBC, albumin and hemoglobin count/Subjective Assessment Protocol | Time of hospitalization |
| Leite et al./201215 | North-American | 221 | Observational/prospective cohort | Anthropometrics: W/A (up to 2 years), H/A, BMI/A (>2 years)/WHO 2006 and 2007) | Mortality/time of hospitalization//MV-free time |
| Delgado et al./200816 | Brazilian | 1077 | Observational/retrospective cohort | Anthropometrics: W/A, W/H, CMA/I/Laboratory: CRP, albumin, and IL6 | Mortality/time of hospitalization |
| Einloft et al./200217 | Brazilian | 13,101 | Observational/retrospective cohort | Anthropometrics: Weight and height measurement/Classific. according to Gomez criteria (2000) | Mortality |
| Pollack et al./198218 | North-American | 108 | Observational/prospective cohort | Anthropometrics: Weight and height measurement/Classific. according to Waterlow criteria (1973), TSF and AC/Classific. according to NCHS | Time of hospitalization |
n, number of patients; WHO, World Health Organization; W/A, weight for age; H/A, height for age; W/H, weight for height; BMI/A, body mass index for age; AC, arm circumference; TSF, tricipital skinfold; CP, cephalic perimeter; CMA, circumference muscular arm; CRP, C-reactive protein; IL6, interleukin 6; NCHS, National Center for Health Statistics; Classific., classification.
One of the great difficulties in the nutritional assessment of critically-ill patients is choosing the best method, as there is no evidence to guide the decision. The difficulties are found in different types of assessment, whether due to the patient's clinical condition, the hemodynamic alterations, body composition modification or even the lack of staff awareness on the importance of appropriately performing data measurement. These aspects make it difficult to standardize the assessment and quality of studies carried out with these patients.19
Weight and height are the measurements most often used and, based on these, the following indices can be obtained: W/A, H/A, W/H, and body mass index (BMI)/A. In 2006, the WHO released new growth charts developed from samples from six countries, among them Brazil. The Z-score and percentile curves were created. These curves include the evaluation of children aged 0–5 years.20 Subsequently, due to the need to create new recommendation standards for children older than 5 years, the WHO reassessed the data from the National Center for Health Statistics (NCHS, 1977), unifying it with the 2006 survey data, thus publishing new curves for children aged 5–19 years, also in Z-scores and percentiles.21 These curves are recommended for worldwide use in the age ranges, regardless of race or ethnicity.22
The assessment through skinfolds, circumferences, or by electrical bioimpedance may be good anthropometric indicators for children, providing data on the reserves of fat and lean mass. However, this practice is yet to be established for use in PICUs.23–25
Laboratory parameters can also be used to complement the nutritional assessment and/or monitor the effectiveness of the established nutritional therapy. In general, the parameters most often used are serum protein levels and immunological assessment. However, in critically-ill patients, it is more complex to use them, due to the organic alterations caused by the disease.26
Analyzing the studies included in this systematic review, the authors confirmed the abovementioned difficulties. It was observed that there was no homogeneity in the choice of methods and parameters used to assess nutritional status, even in studies with very similar objectives. Most of them mention as limitation the difficulty of measuring anthropometric data in this population. Weight and height measurement was performed in all studies. Regarding other less common assessment methods, as mentioned before, only two studies used laboratory assessment of nutritional status and three performed the measurement of skinfolds and circumferences.
Mechanical ventilationRespiratory dysfunction is often considered the most prevalent organ dysfunction as cause of patient admission in epidemiological studies carried out in the PICU.8,27,28 The evolution of these patients can be unfavorable, leading to respiratory failure and need for MV. The nutritional status alteration can lead to protein catabolism, with fat-free mass depletion, which reduces respiratory muscle strength, maximum voluntary ventilation, and vital capacity, and also affects the lungs and the immune function, increasing the risk of respiratory infections.9,29 Studies indicate that this nutritional status alteration and depletion often occur during hospitalization in the PICU, with a multifactorial cause.2–4,6
In addition to the influence of nutritional status on the need for MV, studies show that this depletion can also be associated with the difficulty in MV weaning, as well as its chronic use.30–32 In a study in adults with chronic pulmonary disease using VM at home, Hitzl et al. compared the assessment of nutritional status through electrical bioimpedance (BIA) with BMI, concluding that the fat-free mass values obtained by BIA were predictive of survival in these patients.32 Similar findings were reported by Martinez et al., who assessed body composition by BIA in children using VM at home and concluded that these children had a high prevalence of malnutrition and important fat-free mass depletion.33
Among the studies selected for this review, two used MV as one of the assessed outcomes, focusing on ventilation-free time and prolonged ventilation. Menezes et al. found a high prevalence of malnutrition in their sample, indicating this variable as one that showed a significant association with MV time>5 days (p=0.02).13 Leite et al. evaluated patients admitted to the PICU who had blood glucose alterations, using MV-free time as one of the secondary outcomes. It was verified that malnourished patients with hypoglycemia remained MV-free for a shorter period of time (p<0.01).15 An agreement between the findings of these studies can be observed, as both indicate that nutritional status influences MV time.
PICU length of stayThe length of stay of a patient in the PICU may reflect disease severity, quality of care, and unit procedures, and it also has an important impact on hospital costs.34,35 The authors emphasize that this outcome variable, together with mortality, is one of the most critical studied in pediatric patients. It was used in six of the seven selected studies in the present sample.
One of the authors that compared the nutritional status with hospital length of stay is Pollack, in a study carried out in 1982; this was the only outcome variable used in the research. This is the oldest study included in this review, but it is a reference often mentioned by researchers interested in the subject. Nearly half of its sample (47%) was malnourished and showed depletion of fat tissue, as well as of fat-free mass. However, that study failed to demonstrate a significantly longer length of stay when compared with patients with normal weight.18
Aiming to assess the association of malnutrition and inflammatory response with outcomes in critically-ill pediatric patients, Delgado et al. found no significant difference in length of stay among severely malnourished, moderately malnourished, eutrophic patients.16 Vermilyea et al. conducted a study to validate an overall subjective evaluation method for critically-ill pediatric patients. They compared the tool with anthropometric and laboratory evaluation, subsequently correlating them with the outcomes. Their findings corroborate the studies by Pollack and Delgado, demonstrating no significant association between nutritional status assessment performed with the three tools and patients’ length of stay, thus raising the discussion about inconsistencies in the existing data that associate malnutrition with length of stay.14
Zamberlam et al. studied a population of patients submitted to liver transplant, evaluating the nutritional status and associating it with outcomes. Regarding the length of stay of these patients, they observed that those with muscle depletion remained longer at the PICU. Leite et al. assessed a population of patients with abnormal glucose levels and found that hypoglycemia, when combined with malnutrition, was associated with increased hospitalization (p<0.01).15 Menezes et al. also observed that malnutrition is a risk factor for prolonged hospitalization (p=0.04), making it clear in the statistical methodology that this result was obtained at the univariate analysis, whereas the multivariate analysis showed no significant association. Differently from what was observed in the previously discussed outcome variable, the abovementioned studies have no homogeneity regarding their findings and conclusions.
MortalityDeath is the main and most feared primary outcome; its risk is the main reason for hospitalization in a PICU. The previously discussed outcomes may be the complications that precede death. The mortality risk assessment of patients admitted to the PICU can be measured through prognostic scores, which are widely used in almost all studies evaluating the association between nutritional status and mortality in this group of patients. The most commonly used scores are the Pediatric Risk of Mortality (PRISM, 1988), Pediatric Index of Mortality (PIM, 1997), and Pediatric Logistic Organ Dysfunction (PELOD, 1999). In the present sample, all studies that used mortality as outcome included a severity score, mostly one of the abovementioned scores.
Only two studies of those selected for the review did not use this outcome; the study of Vermilyea only assessed patient severity risk through PIM2 and PRISM scores. Similarly to length of stay, mortality showed to be a variable with inconsistent evidence of association with the nutritional status, as three of the five studies that were included found no significant association between these variables.12,13,16 Despite this finding, all studies discuss this result, pointing out other studies that found an association and emphasizing the importance of nutritional status assessment and its possible association with worse outcomes.
The two studies that found an association between nutritional status and mortality were those by Einloft et al., and Leite et al. The first described high mortality among malnourished patients (p<0.001), indicating malnutrition as a determining factor for this outcome.17 In the second study, mortality was the third outcome with a significant association in hypoglycemic patients, when this complication was associated with malnutrition (p<0.05).15
Search strategy and limitationsThe present search was quite comprehensive and initially included studies of several populations. However, after reviewing, applying the inclusion and exclusion criteria, and performing the quality assessment, only studies in Brazilian and North-American populations remained. The authors consider that this aspect limits a more consistent conclusion about the assessed research question.
ConclusionThis systematic review of literature evidences that studies with appropriate methodology associating nutritional status and outcomes in critically-ill pediatric patients are scarce. All selected studies suggest that malnutrition is associated with worse outcomes or discuss it, but they are not homogeneous. The methodology, particularly nutritional status assessment and classification, varies between authors. Thus, the evidence required to confirm this association was not found. It is of utmost importance that new studies be performed with adequate and homogeneous assessment methodology to clarify this research question and guide the conduct of the professionals involved in the follow-up of these patients.
Conflicts of interestThe authors declare no conflicts of interest.
To CAPES (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior), for the Master's Degree Scholarship.
Please cite this article as: Costa CA, Tonial CT, Garcia PC. Association between nutritional status and outcomes in critically-ill pediatric patients – a systematic review. J Pediatr (Rio J). 2016;92:223–9.