The aim was to adapt an instrument that evaluates the relationship between young individuals and health professionals to the Brazilian population, which will be called the Escala de Avaliação de Vínculo entre Jovens e Profissionais de Saúde (Youth Connectedness to Provider scale).
MethodThe questionnaire known as the Youth Connectedness to Provider scale consists of seven Likert-like questions. The translation, back-translation, evaluation by ten specialists, and pre-test with 43 adolescents and young adults aged between 10 and 24 years were performed to assess the clarity and reliability of meanings. The content validity index was calculated for each question. Subsequently, the clinical validation was performed with 83 patients aged 10–24 years old and Cronbach's alpha coefficient was calculated.
ResultsA content validity index >0.8 (considered satisfactory) was obtained for all items analyzed by experts and adolescents. At the clinical validation, it showed a high internal consistency (Cronbach’s alpha=0.76). The questions showed a good correlation, except for the question about judgment (Spearman’s rho=0.03–0.19).
ConclusionsThe scale adaptation showed an adequate agreement rate at the translation evaluation and a good reliability index in the questions. This instrument provides information on strengths and topics that require more attention from professionals to improve the relationship with their patients; it can be a valuable parameter in assessing the medical consultation quality.
Connectedness is defined as the patient’s degree of perception of having a close, important, and deep relationship with their physician and other health professionals. Several aspects are involved in these relationships: empathy; recognizing the patient as a person with autonomy; and the establishment of trust and affection between patients and professionals.1–3 These feelings must be mutual, where both the patient and the professional receive and reciprocate.4 Establishing a connection and a trust relationship can guarantee greater effectiveness of health actions.1 When referring to the adolescent population, which has its own specificities and vulnerabilities, establishing a good bond can influence the patient’s willingness to talk about confidential information and to follow the health professional’s recommendations.5 The importance of connectedness in the doctor-patient relationship is undeniable; however, there is little discussion about this topic and its parameters, and few studies on how it can be evaluated, especially in the context of medical consultations.4 Therefore, it is important to broaden the discussions about connectedness, especially in relation to adolescent patients, so that doctors can better understand what skills they should develop.
The aim of this study was to adapt the Youth Connectedness to Provider scale5,6 to the Brazilian population aged between 10 and 24 years old, which will be called the Escala de Avaliação de Vínculo entre Jovens e Profissionais de Saúde.
MethodsThe questionnaire known as the Youth Connectedness to Provider scale (Supplementary Appendix 1) is a Likert-type scale (i.e., with answers that measure step-by-step levels rather than just “yes” or “no” answers). It consists of seven simple questions that address the young person's perception of the consultation.5 Five answer options are offered for each question and each one gets an increasing score of 1 point (Not at all), 2 (A little), 3 (Somewhat), 4 (Quite a bit), up to 5 points (Very much). The fifth question is about feeling judged (How much do you feel that this doctor was judging you?), and it is the only question for which the answer score is reversed.5,6
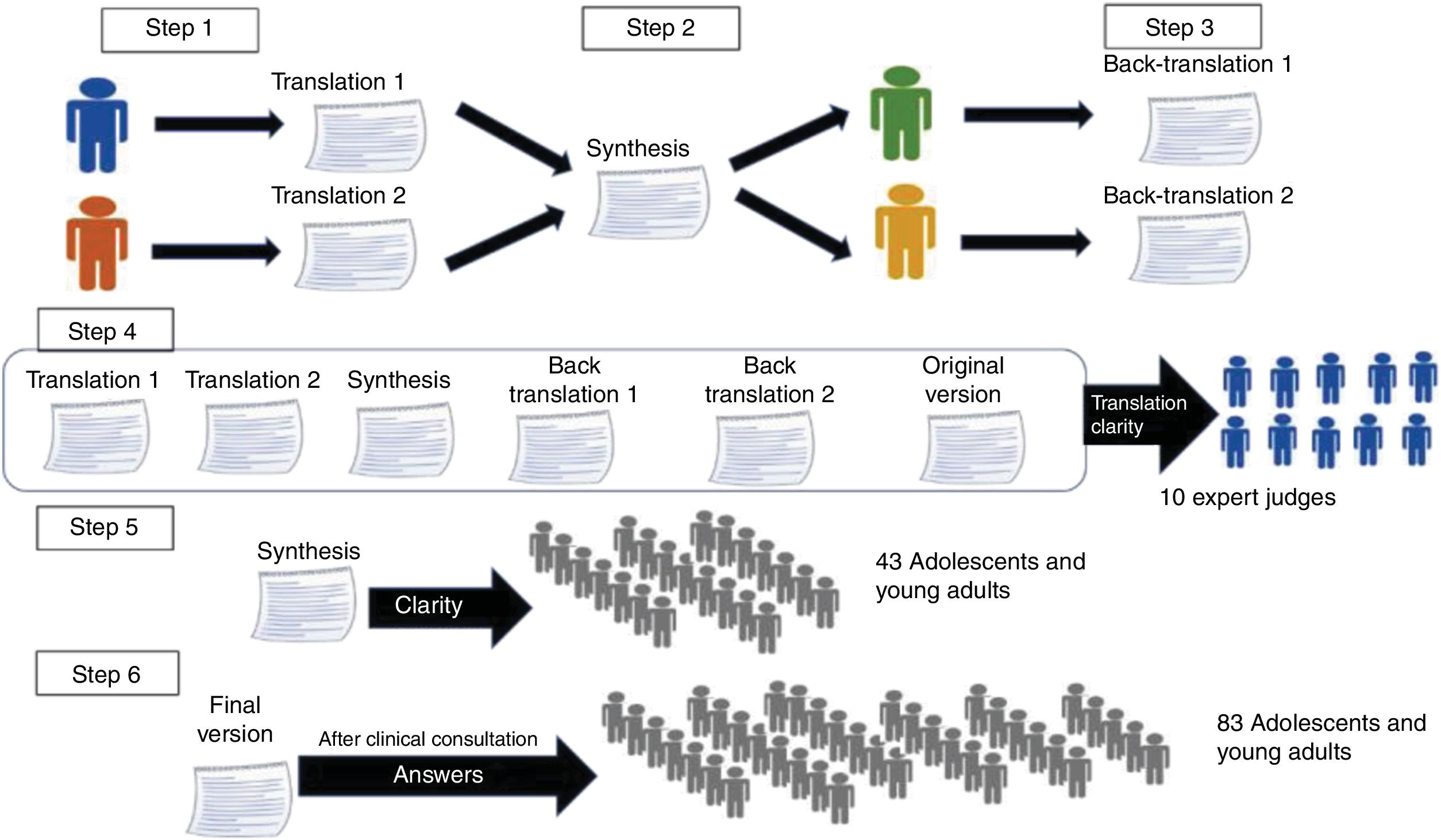
The following steps were performed for its adaptation to the Portuguese language: initial translation, synthesis, back-translation, review, evaluation by a committee of judges specialized in the field, and finally, a pretest,7 as shown in Fig. 1.
To maintain the scientific rigor of the instruments used, it is necessary that translations follow standardized protocols in order to maintain their quality.8 To perform the adaptation, the main determinations described by Beaton et al. were followed, according to the procedures described below (Fig. 1).7
Step 1: translations to PortugueseTranslations of the original questionnaire (Supplementary Appendix 1) into Portuguese were performed by two Brazilian individuals specialized in the English language.
Step 2: synthesisAfter the translations to Portuguese, a synthesis of the two versions was performed, adjusting the content to one closer to the original, corresponding to the final version of the questionnaire.
Step 3: back-translationsThe final Portuguese version was back-translated by two American individuals fluent in the Portuguese language. Subsequently, necessary adjustments were made to the final version.
Step 4: judges’ evaluationsA total of ten physicians that treat adolescents and young adults who were fluent in English evaluated all versions of the questionnaire (original, translated, synthesis, and back-translations) and answered two questions:
- 1)
How much do you agree that the versions have the same meaning?
- 2)
How much do you believe the following questions are clear?
For the second question the physicians were offered a space for them to write suggestions for changes. Both questions were answered using Likert- options, with a score ranging from 1 to 5.
The content validity index (CVI) was calculated, obtained by adding the number of responses equal to 4 or 5 divided by the total number of responses, and a value of 0.8 was considered an acceptable agreement rate.8
Step 5: pre-testThe fifth step was the assessment by the target audience, in which adolescents and young adults assessed the understanding of the question. A convenience sample of patients from the Adolescent Medicine Outpatient Clinic of a university hospital, relatives, and friends of the authors aged 10–24 years were invited to answer this question for each item of the questionnaire: “How clear is this question for you?”
The test was applied in person after a brief explanation of what the instrument was about. The assessment followed the same Likert-type scale from 1 to 5. Therefore, the final version of the questionnaire was evaluated by 43 participants aged 10–24 years (mean=16.5 years; SD±3.6; 65% females). The CVI was also calculated for the opinion of the target audience, considering 0.8 as an acceptable agreement rate.
Step 6: clinical validation – validity and reliability testAfter finishing the adaptation, the clinical validation was performed with the validity and reliability test. For this purpose, 83 patients aged 10–24 years (mean=15.9 years; SD±3.9, 63% females) answered the final questionnaire after a clinical consultation at a Health Center.
The North-American questionnaire was developed to assess the connectedness between adolescent and young adult patients with both medical and non-medical health professionals.5,6 The validation process for the Brazilian version included clinical consultations with physicians and nurses. When the care referred to a nursing consultation, the word “professional” was used instead of “doctor” in the questionnaire questions.
This project was approved by the local Research Ethics Committee and all participants signed the informed assent and/or consent.
Statistical analysisStatistical evaluation calculations were performed using SPSS software (IBM SPSS Statistics for Windows, Version 21.0. NY, USA).To assess the scale reliability, Cronbach's alpha coefficient was used, which ranges from 0 to 1; the closer to 1, the greater the consistency between items on the scale. A value ≥0.7 indicates high reliability; between 0.5 and <0.7, moderate reliability; >0.2 to <0.5, fair reliability, and ≤0.2, low reliability.9,10 The correlations between the scale questions were evaluated by Pearson's tests when there was a normal distribution and Spearman's tests when the distribution was not normal, considering p<0.05 as significant.
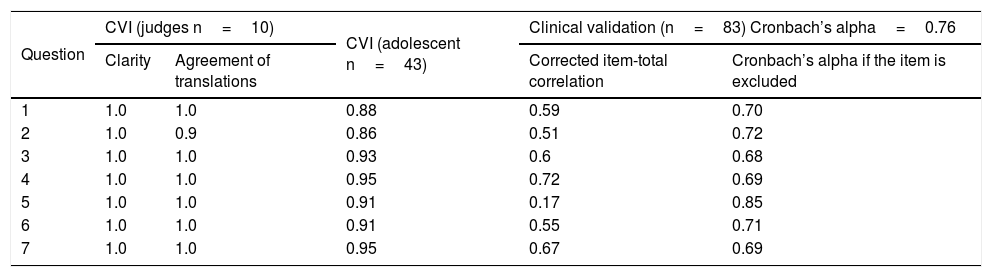
ResultsAfter all the steps, the final version of the translated questionnaire was defined (Supplementary Appendix 2). The judges evaluated the clarity and agreement of the translations and the CVI found was higher than 0.8 for all questions (Table 1). The questionnaire response options were evaluated and the CVI was 0.8.
Results of the analysis of judges and target audience showing the content validity index (CVI), Cronbach’s alpha coefficient, and correlation of the clinical validation of the Youth Connectedness to Provider scale (Escala de Avaliação de Vínculo entre Jovens e Profissionais de Saúde).
| Question | CVI (judges n=10) | CVI (adolescent n=43) | Clinical validation (n=83) Cronbach’s alpha=0.76 | ||
|---|---|---|---|---|---|
| Clarity | Agreement of translations | Corrected item-total correlation | Cronbach’s alpha if the item is excluded | ||
| 1 | 1.0 | 1.0 | 0.88 | 0.59 | 0.70 |
| 2 | 1.0 | 0.9 | 0.86 | 0.51 | 0.72 |
| 3 | 1.0 | 1.0 | 0.93 | 0.6 | 0.68 |
| 4 | 1.0 | 1.0 | 0.95 | 0.72 | 0.69 |
| 5 | 1.0 | 1.0 | 0.91 | 0.17 | 0.85 |
| 6 | 1.0 | 1.0 | 0.91 | 0.55 | 0.71 |
| 7 | 1.0 | 1.0 | 0.95 | 0.67 | 0.69 |
The target audience (adolescents and young adults) evaluated the clarity of all questions and the CVI found, but it persisted with values >0.8 (Table 1).
The scale showed a high internal consistency (Cronbach's alpha=0.76). The questions showed a good correlation among them, with the exception of the question about judgment, which showed a low correlation with the other questions (Spearman’s rho=0.03–0.19).When analyzing the answers, it was observed that most items had a normal distribution among the response options, except for item 5, which evaluated judgment, showing an asymmetrical distribution, in which 66% of participants chose the “not at all” answer option, i.e., they absolutely did not feel they were being judged by the professional who treated them.
DiscussionIn this study, the authors performed the translation and validation of the Youth Connectedness to Provider scale, which aims to measure the quality of the relationship between adolescents and young adults and health professionals. The scale, which was proposed and validated by Harris et al., can be used to assess the relationship between adolescent and young adult patients during a consultation with clinicians and other health professionals.5,6 The presence of connectedness between the patient and health professionals is associated with better outcomes, such as improved participation in medical decision-making, adherence to treatment, and a decrease in risk behaviors.4
Phillips et al., in a qualitative study with young individuals undergoing cancer treatment, showed that a good relationship ensures that patients feel comfortable discussing their needs with the professional, as well as helping to reduce anxiety and concerns during and after the treatment.11
The way adolescents are embraced by a service can guarantee the construction of a relationship between professionals and patients. Training of health professionals on how to promote and maintain this relationship is scarce and seldom discussed. This is even worse regarding relationships with adolescents. This lack of training can contribute to the difficulties in providing the psychosocial support that these patients need.
The Youth Connectedness to Provider scale (called the Escala de Avaliação de Vínculo entre Jovens e Profissionais de Saúde in Portuguese) provides information about strengths and areas that require more attention by physicians to improve the relationship with their patients. Phillips-Salimi et al., aiming to conceptualize “connectedness,” translated here as “bond,” identified seven necessary attributes: intimacy, sense of belonging, caring, empathy, respect, trust, and reciprocity.4 When analyzing these concepts, the Youth Connectedness to Provider scale can assess:
- -
Caring (How much do you feel that this doctor cares about you?);
- -
Intimacy (How much do you feel that this doctor is someone you can talk to if you had a problem?);
- -
Empathy (How much do you feel that this doctor listens to what you have to say?);
- -
Respect (How much do you feel that this doctor respects you as a person?);
- -
Reciprocity (How much do you feel that this doctor was judging you?);
- -
Trust (How much do you trust that this doctor will keep what you tell him/her confidential (private)? How much do you believe that what this doctor tells you is true?)
Although the scale does not have a specific item for the sense of belonging, this feeling is reinforced throughout the patient's follow-up when a good relationship is built. The validated instrument has the advantage of being short and easy to apply and, consequently, it can be used as a tool in the continuous evaluation of health services.
Potential applications include the assessment of connectedness in outpatient care, quality of care assessment in primary care, and in secondary and tertiary services. Moreover, the instrument can be used in research when the doctor-patient relationship is a bias or a variable, e.g., in research aimed at evaluating the effectiveness of interventions.6,12
In the proposed translation, it was observed that the answer options, evaluated by the judges regarding the meaning of the translation, was the item with the lowest CVI, although it was within an acceptable value. Despite the difficulty of finding a more reliable translation for some of the words due to the natural barriers between the two languages, it is understood that the most important feature is the step-by-step alternatives, and this has been preserved in the adaptation options.
Question 5, which was about feeling judged by the doctor, was the item with the lowest CVI in the target audience. It was also the question with the lowest reliability index. In the work by Haris et al., who created the scale, this question was also the one that showed the lowest correlation with the others.5 This questionnaire item is the only one that has a reversed score for its answer options. The use of reversed items in questionnaires is controversial; however, their use may help to decrease the response bias, as it interrupts the process of answering automatically.13 Despite the low correlation of this question with the rest of the questionnaire, assessing the presence of judgment at the consultation is important, as moral issues and unconscious biases of professionals interfere with empathy and reciprocity during care, compromising the physician-patient relationship.
This study is limited by the fact that the clinical validation of the questionnaire was performed in a convenience sample from a primary Health Center and it needs to be tested in services with different levels of care.
The authors herein present the adaptation of the Youth Connectedness to Provider scale to the Portuguese language. The adaptation was well evaluated by the judges and the target audience, with a good understanding of the questions, an adequate agreement rate in the translation evaluation, and a good reliability index in the questions. The use of this instrument can be a valuable parameter to help physicians and health professionals identify behaviors that require attention to decrease communication barriers and improve the quality of medical consultation.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Pavan GN, Roselli LF, D’Souza LL. Adaptation of the Youth Connectedness to Provider scale to assess the relationship between health professionals and adolescent and young adult patients. J Pediatr (Rio J). 2020;97:61–5.