To describe the epidemiology and clinical features of acute pancreatitis and recurrent acute pancreatitis in children.
MethodsObservational and retrospective study with an analytical component. Patients were classified into two groups: Acute pancreatitis and recurrent pancreatitis. The relationship with each parameter obtained was analyzed using the chi-squared test, Student's t-test, or the Mann–Whitney U test.
ResultsThere were 130 patients with acute pancreatitis; recurrent pancreatitis was diagnosed in 23.8% of the cases. The most frequent causes were anatomical (29.6%), pharmacological (19.2%), and biliary (14.6%), although in 29.2% etiology was not identified. Fasting lasted 3.5±3.8 days and parenteral nutrition was indicated in 26.9% of the cases for 10.8±11.3 days. A statistical association with anatomical (p=0.02) and pharmacological causes (p=0.01) was found in the recurrent pancreatitis group; no other differences between acute pancreatitis and recurrent pancreatitis groups were observed. The mortality rate was 3.1%, it was not attributable to acute pancreatitis in any cases.
ConclusionAcute pancreatitis is associated with a high frequency of acute recurrent pancreatitis. Severity and complications did not show statistically significant differences in this investigation. Anatomical etiologies were the most relevant cause in this cohort. Fasting time and parenteral nutrition use were relevant. Genetics testing is required in this population.
Descrever a epidemiologia e as características clínicas da pancreatite aguda e da pancreatite aguda recorrente em crianças.
MétodosEstudo observacional e retrospectivo com um componente analítico. Os pacientes foram classificados em dois grupos: pancreatite aguda e pancreatite recorrente. A relação com cada parâmetro obtido foi analisada com o teste de qui-quadrado, teste t de Student ou teste U de Mann–Whitney.
ResultadosForam analisados 130 pacientes com pancreatite aguda; pancreatite recorrente foi diagnosticada em 23,8% dos casos. As causas mais frequentes foram anatômicas (29,6%), farmacológicas (19,2%) e biliares (14,6%), embora em 29,2% a etiologia não tenha sido identificada. O jejum durou 3,5±3,8 dias e a nutrição parenteral foi indicada em 26,9% dos casos por 10,8±11,3 dias. Uma associação estatística com causas anatômicas (p=0,02) e farmacológicas (p=0,01) foi encontrada no grupo com pancreatite recorrente; não foram observadas outras diferenças entre os grupos pancreatite aguda e pancreatite recorrente. A taxa de mortalidade foi de 3,1% e nenhum caso foi atribuível à pancreatite aguda.
ConclusãoA pancreatite aguda está associada à alta frequência de pancreatite aguda recorrente. A gravidade e as complicações não apresentaram diferenças estatísticas nesta investigação. Etiologias anatômicas foram a causa mais relevante nesta coorte. O tempo de jejum e o uso de nutrição parenteral foram relevantes. Testes genéticos são necessários em nossas populações.
Acute pancreatitis (AP) in children is an increasingly recognized clinical entity1; in parallel, an increase in its incidence at all ages in the last two decades has been reported.2,3 Recently, the definitions of AP, acute recurrent pancreatitis (ARP), and chronic pancreatitis in children have been developed by consensus to promote the standardization and unification of the diagnostic criteria in clinical investigations and thereby improve the level of knowledge on these entities.4
Currently, it is known that the socioeconomic burden of AP and ARP is significant given the presence of symptoms like pain and the costs to the health system5,6; as a consequence, the knowledge about these entities in children has increased in recent years. Epidemiological, clinical, and etiological data associated with these entities have been explored in recent investigations. Pant et al.,6 in a multicentric American study, showed that ARP-related hospitalizations had an increased requirement for intensive care unit treatment compared with an index episode of AP and recently Kumar et al.5 provided an extensive analysis of ARP in a multinational cross-sectional study; their important data concluded that at least one gene mutation in pancreatitis-related genes was found in 48% of patients with ARP.
In the present authors’ region, Sánchez-Ramírez et al.7 performed a study in Mexican children with AP and ARP, demonstrating an ARP incidence of 34.5%; in the same investigation, biliary stones and a family history of pancreatitis were the most commons causes found. No others studies that included Latin-American children were found. The objective of this study was to obtain better knowledge on the epidemiology and clinical aspects of patients diagnosed with AP and ARP in a pediatric reference hospital in Colombia.
Materials and methodsA cross-sectional, retrospective study was performed. A review of all medical registries with International Disease Classification-10 diagnoses related to AP was performed between January 2010 and December 2015 in a Colombian pediatric institution; there is no IDC-10 definition for ARP, thus the cases were taken based on AP codes and then selected according ARP definitions.
Subjects under 18 years of age were included. AP was defined as requiring two of the following: (a) abdominal pain compatible with AP, (b) serum amylase and/or lipase values ≥3 times upper limits of normal, (c) imaging findings of AP. ARP was defined as: ≥2 distinct episodes of AP with intervening return to baseline according to the definitions provided by INSPPIRE (International Study Group of Pediatric Pancreatitis: in Search for a Cure).4 Demographic and clinical variables, as well as laboratory parameters, etiology, comorbidities, type of images and interpretations, treatment strategies, and outcomes were recorded based on clinical charts. The analysis of the nutritional status was performed using the tool Anthro for personal computers (version 3.2.2, January 2011, World Health Organization (WHO))8 and was interpreted according to the parameters of the WHO.9
Variables obtained from laboratory exams taken within the first 24h of the onset of symptoms were included. In the case of serum amylase and lipase, the follow-up value of each was recorded, and the diagnostic images of each patient were reviewed. The radiological report recorded in the medical history was used to describe parameters compatible with AP: pancreatic edema, pancreatic or peripancreatic necrosis, peripancreatic inflammation, single or multiple collections, pancreatic hemorrhage, pancreatic abscess, and pseudocyst. Findings associated with alterations of the biliary tract or other abdominal abnormalities were also considered.
In regard to treatment, fasting, fasting time, and use and duration of enteral and parenteral nutrition were assessed. The length of stay at the hospital and the admission and length of stay in the pediatric intensive care unit (PICU) were included as variables. Cases with prolonged stays and admission to the PICU not related to AP or ARP were excluded. The stay in the PICU or in the intermediate care unit was considered as a single variable.
Severity and complications were classified according to the Atlanta criteria,10 in which an episode is defined as severe if there is evidence of organ failure (systemic arterial pressure of <P5 for age or vasopressors requirement, PaO2<60mm Hg, acute renal failure, or gastrointestinal bleeding) or local complications (pseudocyst, necrosis, abscess, need to perform pancreatic surgery, or death).
Statistical analysis was performed using Microsoft Excel (Microsoft Corporation, versión 2014, WA, USA) and IBM SPSS Statistics (IBM SPSS Statistics for Windows, version 22.0, NY, USA) and a descriptive analysis of all cases is presented below. Quantitative variables are reported in terms of mean and standard deviation (SD) or median and interquartile range (IQR), according to their distribution. Nominal variables are expressed as absolute and relative frequencies. In addition, the descriptive analysis of each variable was done independently for AP and ARP groups, and their results were compared using the chi-squared test and the Fisher's exact test for categorical variables, and Student's t-test or the Mann–Whitney U-test for quantitative variables. Results were interpreted based on a level of statistical significance of 0.05. This research was approved by the institutional ethics committee.
ResultsOf the 366 records reviewed, 236 cases were excluded because of incomplete medicals records or other diagnoses besides AP or ARP; thus, only 130 (35.5%) met the INSPPIRE criteria for AP and ARP diagnosis. From this group, 81 patients (62.3%) were female. The mean age was 11.4±3.8 years and three patients (2.3%) were younger than 2 years at the time of diagnosis. In total, 31 (23.8%) children were diagnosed with ARP.
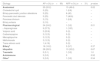
The most common clinical findings were abdominal pain, found in 119 patients (91.5%); nausea or vomiting, in 93 (71.5%); hyporexia, in 66 (50.8%); fever, in 18 (13.8%); oliguria, in nine (6.9%); jaundice, in eight (6.2%), and respiratory distress, found in one case (0.8%). On physical examination, pain on palpation of the epigastrium was observed in 93 cases (71.5%), gastrointestinal motility was increased in six (4.6%), signs of peritoneal irritation were seen in four (3.1%), abdominal masses were found in two (1.5%), and ascites, in one (1.5%). Comorbidities were observed in 31.5% of the patients, the most important being leukemia (11.5%) and epilepsy (5.4%) (Table 1).
Associated comorbidities.
| Comorbidities | AP n (%) (n=99) | ARP n (%) (n=31) | p-value |
|---|---|---|---|
| Leukemiasa | 10 (10.1%) | 5 (16.1%) | 0.35 |
| Epilepsy | 5 (5.1%) | 2 (6.5%) | 0.76 |
| Systemic lupus erythematosus | 3 (3.0%) | 1 (3.2%) | 1.00 |
| Diabetes mellitus type 1 | 1 (1%) | 2 (6.5%) | 0.14 |
| Lymphomas | 2 (2.0%) | 1 (3.2%) | 0.56 |
| Immune thrombocytopenic purpura | 2 (2%) | 0 | 1.00 |
| Otherb | 5 (5.1%) | 2 (6.5%) | 0.76 |
AP: acute pancreatitis; ARP: acute recurrent pancreatitis.
Regarding the pancreatic enzymes amylase and lipase, in 90% and 89.5% of the cases, respectively, they were three times higher than the upper limit. In the cases with abnormal pancreatic enzymes, the diagnosis was made with symptoms and radiology criteria. In total, 76 cases (58.4%) had amylase and lipase studies performed simultaneously at the beginning of the clinical picture; of them, 65 showed an increase of both enzymes according to the limit defined for diagnosis. For amylase, the mean between the first and second samples was 3.5±3.1 days, and for lipase, 5.7±6.5 days. Because of the broad lapse of time in which follow-up values of the enzymes were obtained, no statistical association was explored. Immunological studies were performed in 18 (13.8%) patients; the following laboratory parameters were taken: antinuclear antibodies, extractable nuclear antigen antibodies, levels of complements, and anti-neutrophil cytoplasmic antibodies; however, each patient had different sets of immunological assays. No medical histories of genetic or metabolic causes were found. No genetics or metabolic assays were performed in this group.
The most frequently used imaging test carried out was total abdominal ultrasonography (in 111 cases) followed by contrast-enhanced tomography (59 cases), magnetic resonance cholangiopancreatography (in 48 cases), and endoscopic retrograde cholangiography (in 17 cases). Fasting was considered as part of the treatment in 108 cases (83.1%), with a median duration of two days (IQR 1–4). Enteral feeding with jejunal probe was not used, while in 35 patients (26.9%) parenteral nutrition was used for a median of eight days (IQR 3–12).
In conclusion, 38 patients (29.2%) met at least one criterion for severe AP. The complications documented were acute renal failure in 11 (8.5%), hypotension or vasoactive requirement in 12 (9.2%), PaO2<60mmHg in seven (5.4%), gastrointestinal hemorrhage in six (4.6%), pancreatic pseudocyst in six (4.6%), and pancreatic necrosis in five (3.8%). The mortality rate was 3.1% (causes were abdominal catastrophe after closed trauma, liver laceration secondary to laparoscopic correction of pancreaticobiliary malunion, and two cases due to sepsis), it was not attributable to acute pancreatitis in any of the cases.
Comparative analysis of AP and ARP casesNinety-nine (76.2%) cases were classified in AP group and 31 (23.8%) cases were included in ARP group. No differences were found in relation to sex (p=0.771) and age (p=0.439) distribution between AP and ARP cases. Overweight or obesity was found in 30% and 35% of cases with ARP and AP, respectively, and 46% of AP and 70% of ARP cases were eutrophic. No association between ARP and nutritional status was found (p=0.35). Furthermore, no statistical differences regarding symptoms and clinical findings were obtained. Regarding comorbidities, no relationship between them and ARP was documented (Table 1).
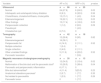
On the other hand, a statistically significant association between ARP and pharmacological and anatomical etiologies was found (Table 2 for the etiologies of AP and ARP). However, no statistical differences were found in relation to enzyme levels, nor was an association observed with lipid profiles or local complications found in the images. The summary of the findings in the diagnostic images is presented in Table 3.
Etiology.
| Etiology | AP n (%) (n=99) | ARP n (%) (n=31) | p-value |
|---|---|---|---|
| Anatomical | 20 (20.2) | 15 (48.4) | 0.02 |
| Choledochal cyst | 5 (25) | 1 (6.6) | – |
| Biliary-pancreatic junction alterations | 5 (25) | 6 (40) | – |
| Pancreatic duct stenosis | 5 (25) | 7 (46.6) | – |
| Pancreas divisum | 3 (15) | 1 (6.6) | – |
| Biliary ectasia | 2 (10) | – | – |
| Pharmacological | 24 (24.2) | 1 (3.2) | 0.01 |
| l-Asparaginase | 9 (37.5) | 1 (100) | – |
| Valproic acid | 5 (20.8) | 0 (0) | – |
| Carbamazepine | 3 (12.5) | 0 (0) | – |
| Mercaptopurine | 3 (12.5) | 0 (0) | – |
| Methotrexate | 3 (12.5) | 0 (0) | – |
| Trans retinoic-acid | 1 (4.16) | 0 (0) | – |
| Biliarya | 16 (16.2) | 3 (9.7) | 0.37 |
| Idiopathic | 28 (28.3) | 10 (32.2) | 0.67 |
| Traumatic | 5 (5.1) | 1 (3.2) | 1.0 |
| Autoimmune | 3 (3.0) | 0 | 0.52 |
| Otherb | 3 (3.0) | 1 (3.2) | 0.54 |
AP, acute pancreatitis; ARP, acute recurrent pancreatitis.
Findings in diagnostic images.
| Variable | AP n (%) | ARP n (%) | p-value |
|---|---|---|---|
| Ultrasound | n=86 | n=25 | |
| Normal | 24 (27.9) | 6 (24.0) | 0.05 |
| Intrahepatic and extrahepatic biliary dilatation | 8 (9.3) | 8 (32.0) | 0.56 |
| Cholelithiasis, choledocholithiasis, cholecystitis | 13 (15.1) | 1 (4.0) | 0.04 |
| Edema/enlargement | 19 (22.1) | 3 (12.0) | 0.03 |
| Other findings | 15 (17.4) | 4 (16.0) | 0.03 |
| Peripancreatic collection | 1 (1.2) | 2 (8.0) | 0.09 |
| Pseudocyst | 1 (4.0) | ||
| Choledochal cyst | 6 (7.0) | 0 | |
| Tomography | n=42 | n=18 | |
| Normal | 12 (28.6) | 9 (50) | 0.82 |
| Edema/enlargement | 16 (38.1) | 0 | |
| Peripancreatic fat | 6 (14.3) | 2 (11.1) | 0.52 |
| Multiple collection | 1 (2.4) | 0 | |
| Single collection | 2 (4.8) | 2 (11.1) | |
| Other unrelated findings | 5 (11.9) | 4 (22.2) | 0.52 |
| Pancreatic laceration | 0 | 1 (5.6) | |
| Magnetic resonance cholangiopancreatography | n=35 | n=13 | |
| Normal | 12 (34.3) | 2 (15.4) | 0.02 |
| Malformation of the bile duct and the pancreatic ducta | 10 (28.5) | 5 (38.4) | 0.04 |
| Pancreatic and peripancreatic inflammation | 6 (17.1) | 0 | |
| Bile duct abnormalitiesb | 4 (11.4) | 3(23.0) | 0.23 |
| Anatomical alterations pancreasc | 2 (5.7) | 1 (7.7) | 0.35 |
| Not related to pancreatitis | 1 (2.9) | 1 (7.7) | 0.26 |
| Pancreatic tumor | 0 | 1 (7.7) | |
AP, acute pancreatitis; ARP, acute recurrent pancreatitis.
Fasting time was higher in AP (p=0.01) cases, as well as the duration of parenteral nutrition (p=0.043). No evidence was found regarding the association with fasting as a therapy nor the requirement of parenteral nutrition. Finally, there were four deaths (3.1%), but none of them were attributable to AP or ARP. Table 4 summarizes the treatment and outcome findings in each group.
Treatment and clinical outcomes.
| Variable | AP | ARP | p-value |
|---|---|---|---|
| Fasting time (days) | 3 (IQR 2–5) (n=79) | 2 (IQR 1–2.5) (n=29) | 0.01 |
| Parenteral nutrition time (days) | 9 (IQR 5.5–15.3) (n=30) | 3 (IQR 1.5–8) (n=5) | 0.043 |
| Hospital stay (days) | 9 (IQR 6–13.5) (n=85) | 10 (IQR 6.5–17.7) (n=26) | 0.44 |
| Admission to the PICU n (%) | 34 (36.2) | 14 (48.3) | 0.24 |
| Stay at the PICU (days) | 5 (IQR 3–10) (n=34) | 6.5 (IQR 3.8 –10.3) (n=29) | 0.37 |
AP, acute pancreatitis; ARP, acute recurrent pancreatitis.
This study contains information, previously unavailable in Colombia, describing AP and ARP. No similar investigations have been published in this country. Previously, only Sánchez-Ramírez et al.,7 in a cohort with 55 patients, described ARP in Latin-American children; their group had similar proportions with idiopathic etiology: 33.3% in AP and 36.8% in ARP vs. 28.3% and 32.2% in the present study; however, their study differs in the other more prevalent causes.
Pharmacological etiology was an important cause in AP, which is similar to findings from other cohorts.11,12 Bai et al.13 showed in their investigation that valproic acid, l-asparaginase, and 6-mercaptopurine were among the most frequent causes, as was found in this cohort; this is related with the most important comorbidities: leukemias and epilepsy, which coincide in both studies. Comorbidities were not associated with ARP. The authors’ hospital is an important reference center for childhood cancer and epilepsy management, and this could be related with some of the findings.
Regarding ARP in children, its frequency in this study coincides with the range reported in similar research,1 showing that an important percentage of AP is related with an ARP episode. Regarding ARP etiologies, the anatomical causes represent most important factor in this cohort, which is concordant with the most recent and largest study about ARP,5 in which similar anatomical etiologies were described by the authors.
The number of records (366) reviewed on which this study is based was considerably larger, perhaps because of the general initial intention of discarding AP in the patients. Abdominal pain and emesis, symptoms more frequently found in conjunction with other series.13,14 A judicious differential diagnosis is important to treat children with AP in a timely manner instead of treating other diseases unnecessarily.15 The symptoms were similar in the presentation of AP and ARP, and no significant differences were established. Thus, their initial diagnosis remains clinically supported by serum pancreatic enzymes (with wide variations) and imaging studies.
With respect to amylasemia, reports indicate that it increases between 40% and 60%,14,16 unlike what happened in this case series, where an increase in 90% of the cases was observed, which could be explained by the difference in the age of the patients, because both amylase and lipase expression increase after birth, with amylase expression increasing at a slower rate.17 No differences between enzyme levels and lipid profiles in the two forms of pancreatitis were found.
Diagnostic images were primarily used for identifying anatomical alterations and complications. Likewise, a striking lack of standardization was seen when interpreting patterns and using severity scales such as the CT scoring index or the Atlanta classification, which leads to diverse results, in the review of the images in the radiological records in present study there were not a unique standard to interpreted it but we are working in to evaluate the CT scores and their utility in pediatric patients.18
Therefore, the management scheme of children with AP and ARP remains conservative, and primarily medical. Nutrition deserves special attention. In this cohort, fasting continued to prevail, while early enteral nutrition with advanced probe was non-existent, which is consistent with reports showing a frequency of use of only 3% in children.19
In addition, the frequency of parenteral nutrition is similar to what has been reported in other studies,7 where a significant number of patients received this therapeutic alternative as treatment, but this preference is not clear in the retrospective review. Nutritional limitations and requirements must be established to prevent complications, shorten hospitalization periods, and reduce costs. Recently, a new consensus about nutritional management in pediatric pancreatitis20 was published; however, its recommendations were not applied in the present cohort.
Scales for predicting AP severity in children have not been validated among the different populations studied,21 nor the need for routine transfer to the PICU. In this case series, the behavior of the entities evaluated was the same: no differences in severity, local complications, and admission to the PICU were found. Mortality was low and there were no cases in which AP was the primary cause of death.
This study has several limitations. Its retrospective design did not allow follow-up of patients and the data were taken from each clinical record. As there was not a protocol for the evaluation of patients with ARP at the end of this study in the hospital, the same tests (immunological, viral, genetics) were not performed in all patients. Other authors have showed genetic causes,5,22 especially the cystic fibrosis transmembrane conductance regulator and others: cationic trypsinogen, pancreatic secretory trypsin inhibitor, chymotrypsin C, and carboxypeptidase 1 (CPA1); however, no genetics studies were made in this population, so far, and no studies on the Colombian population have been performed to identify mutations associated with ARP5; their frequency and usefulness should be assessed in this subgroup of children; the cost for the health system of the genetic studies could be a limitation in Colombia.
AP in children is associated with high frequency of ARP, and clinical manifestations are similar in both entities. Severity and complications did not have statistical differences in this investigation. Anatomical etiologies were the most relevant cause in this cohort of ARP, and imaging studies were fundamental in the approach. It is necessary to evaluate the use of parenteral nutritional, and to consider using naso-jejunal nutrition as an alternative according to each patient. The use of consensus in the approach of ARP will permit standardization in the evaluation of this group of patients, and genetic tests are required in these populations.
This research was conducted in a national reference center, so its results may be applicable to the general population in Colombia, but multicentric studies are necessary to confirm this hypothesis.
FundingUniversidad Nacional de Colombia. National call for projects to strengthen research, creation, and innovation at Universidad Nacional de Colombia, 2016-2018.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Fonseca Sepúlveda EV, Guerrero-Lozano R. Acute pancreatitis and recurrent acute pancreatitis: an exploration of clinical and etiologic factors and outcomes. J Pediatr (Rio J). 2019;95:713–9.
Study conducted at Universidad Nacional de Colombia, Bogota, Colombia.