To assess the accuracy of stridor in comparison to endoscopic examination for diagnosis of pediatric post-intubation subglottic stenosis.
MethodChildren who required endotracheal intubation for >24h were included in this prospective cohort study. Children were monitored daily and underwent flexible fiberoptic laryngoscopy after extubation. Those with moderate-to-severe abnormalities underwent another examination 7–10 days later. If lesions persisted or symptoms developed, laryngoscopy under general anesthesia was performed. Patients were assessed daily for stridor after extubation.
ResultsA total of 187 children were included. The incidence of post-extubation stridor was 44.38%. Stridor had a sensitivity of 77.78% (95% confidence interval [95% CI]: 51.9–92.6) and specificity of 59.18% (95% CI: 51.3–66.6) in detecting subglottic stenosis. The positive predictive value was 16.87% (95% CI: 9.8–27.1), and the negative predictive value was 96.15% (95% CI: 89.9–98.8). Stridor persisting longer than 72h or starting more than 72h post-extubation had a sensitivity of 66.67% (95% CI: 41.2–85.6), specificity of 89.1% (95% CI: 83.1–93.2), positive predictive value of 40.0% (95% CI: 23.2–59.3), and negative predictive value of 96.07% (95% CI: 91.3–98.4). The area under the receiver operating characteristic (ROC) curve was 0.78 (95% CI: 0.65–0.91).
ConclusionsAbsence of stridor was appropriate to rule out post-intubation subglottic stenosis. The specificity of this criterion improved when stridor persisted longer than 72h or started more than 72h post-extubation. Thus, endoscopy under general anesthesia can be used to confirm subglottic stenosis only in patients who develop or persist with stridor for more than 72h following extubation.
Analisar a precisão do estridor em comparação com o exame endoscópico no diagnóstico de estenose subglótica pós-intubação em crianças.
MétodoForam incluídas neste estudo de coorte prospectivo crianças que necessitaram de intubação endotraqueal por mais de 24 horas. Elas foram monitoradas diariamente e submetidas à nasofibrolaringoscopia flexível após a extubação. As crianças com anomalias moderadas foram submetidas a outro exame sete a 10 dias depois. Caso as lesões persistissem ou os sintomas evoluíssem, a laringoscopia era realizada com anestesia geral. Os pacientes foram avaliados diariamente quanto ao estridor após a extubação.
ResultadosParticiparam 187 crianças. A incidência de estridor após a intubação foi de 44,38%. O estridor apresentou uma sensibilidade de 77,78% (intervalo de confiança de 95% [IC]: 51,9-92,6) e especificidade de 59,18% (IC: 51,3-66,6) na detecção de SGS. O valor preditivo positivo foi de 16,87% (IC: 9,8-27,1) e o valor preditivo negativo (VPN) foi de 96,15% (IC: 89,9-98,8). O estridor que persistiu por mais de 72 horas ou que começou 72 horas após a extubação teve uma sensibilidade de 66,67% (IC: 41,2-85,6), especificidade de 89,1% (IC: 83,1-93,2), valor preditivo positivo de 40,0% (IC: 23,2-59,3) e valor preditivo negativo de 96,07% (IC: 91,3-98,4). A área sob a curva de característica de operação do receptor (ROC) foi de 0,78 (IC: 0,65-0,91).
ConclusõesA ausência de estridor foi adequada para descartar a estenose subglótica pós-intubação. A especificidade desse critério melhorou quando o estridor perdurou por mais de 72 horas ou começou mais de 72 horas após a extubação. Assim, a endoscopia com anestesia geral pode ser utilizada para confirmar a estenose subglótica somente em pacientes que desenvolveram ou continuaram com estridor por mais de 72 horas após a extubação.
Post-intubation subglottic stenosis (SGS) in children is one of the most challenging diseases for otolaryngologists. The majority of authors consider airway endoscopy to be the optimal modality for diagnosis and evaluation. However, there is no consensus on which technique is best or which patient characteristics indicate a need for this diagnostic approach after extubation. Furthermore, the procedure is not risk-free, and not all centers have the required equipment or appropriately trained and experienced professionals.1–7
The assessment of stridor as a marker of post-intubation laryngeal lesions is largely accepted in clinical practice, mainly because it is easy to perform and has no restrictions.8 However, the validity and reliability of stridor for this purpose have been questioned. Given the lack of studies in pediatric patients comparing this clinical approach to other methods for diagnosis of post-intubation SGS, especially the gold-standard endoscopic technique, these concerns are justified.9–14
This study aimed to determine the accuracy of stridor, in comparison with airway endoscopy, to predict post-intubation SGS in pediatric patients.
MethodsPatients who required endotracheal intubation in the pediatric intensive care unit (PICU) of this hospital were selected for the study. The inclusion criteria were age between 28 days and 4 years and duration of intubation >24h. The exclusion criteria were history of stridor or dysphonia, previous intubation, presence or history of tracheostomy, craniofacial malformations, and terminal illness, as identified by the PICU medical staff.
When patients who met the inclusion criteria completed 24h of endotracheal intubation, the study investigators were notified by the PICU team. After obtaining consent from parents or legal guardians, an interview was conducted to collect data on pregnancy, comorbidities, and previous hospitalizations. Information on diagnosis and intubation procedure, such as number of attempts and endotracheal tube characteristics (size, cuffed vs. uncuffed) were obtained from PICU staff.
During their PICU stay, children were monitored daily by the investigators. At some point, during the first 8h after extubation, patients underwent flexible fiberoptic laryngoscopy (FFL). Examinations were performed at bedside in the PICU, without sedation, by one of four investigators (LVE, CSN, DM, CS). All FFL examinations were recorded digitally. The videos were then evaluated by a researcher (GK) blinded to clinical data, and cases were classified into two groups, according to previously published data.7 Patients with evidence of moderate-to-severe lesions on FFL underwent a second examination 7–10 days after extubation and were followed up by the otolaryngology team. In case of persistent lesions, patients underwent examination under general anesthesia, and those with SGS were classified according to criteria proposed by Myer and Cotton.15 Patients who developed laryngeal symptoms also underwent examination under general anesthesia, regardless of their initial classification.
All extubated children were followed daily by the investigators until hospital discharge. Development of stridor was verified by daily review of progress notes written by the PICU staff, as well as by questioning staff members directly. The PICU staff is composed entirely of specialist pediatric intensivists.
For the purposes of this study, stridor was defined as a high-pitched breath sound. Stridor was classified as present or absent.
Thirty days after discharge, all patients were re-examined at the outpatient pediatric laryngology clinic. Once-monthly telephone follow-up was continued for 6 months thereafter.
Statistical analyses were carried out in SPSS (Statistical Package for the Social Sciences for Windows, version 18.0., Chicago, USA). Quantitative variables were described as mean±standard deviation or median (interquartile range), with minimum and maximum values, as appropriate. For dichotomous variables, the chi-squared test or Fisher's exact test was used for comparisons, as indicated. For comparisons of continuous variables, Student's t-test (for symmetrically distributed variables) or the nonparametric Wilcoxon–Mann–Whitney test (for asymmetrically distributed data) was used. Multivariate analysis was performed using Poisson regression with robust variance.
The performance of the stridor-based assessment for diagnosis of SGS was evaluated by comparison to direct laryngoscopy, which is considered the gold standard. Two analyses were performed. First, the presence or absence of stridor was compared to direct laryngoscopy findings. Second, patients were dichotomized between those without stridor or with stridor only in the first 72h post-extubation (negative test) and those with stridor lasting longer than 72h post-extubation or stridor developing after this period (positive test). These groups were classified as “negative” or “positive” for “72-h stridor.” From these data, it was possible to obtain the receiving operator characteristic (ROC) curve, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV), with their respective 95% confidence intervals (95% CIs).
The study was approved by the hospital's research ethics committee under protocol No. 05-266.
ResultsA total of 234 patients were eligible for enrollment from November 2005 to August 2012; consent was obtained for 226. Of these, three underwent tracheostomy for prolonged mechanical ventilation, 25 died before extubation, and 11 died after initial FFL. All were considered losses (19.5%). The final sample thus comprised 187 patients who completed the study. Among these patients, 111 (59.4%) were male. The median age was 2.7 months (range, 0.9–59.5 months).
The primary diagnosis leading to intubation was acute bronchiolitis in 118 patients (63.1%), other respiratory problems (asthma, pneumonia, and respiratory distress) in 36 (19.3%), meningitis in 11 (5.9%), and other causes in 22 patients (11.8%).
The incidence of SGS was 9.62% (95% CI: 5.9–15.1), diagnosed by direct laryngoscopy. Of the 18 patients with SGS, three (16.66%) showed grade 4 SGS and underwent tracheotomy followed by open reconstructive airway surgery; seven (38.9%) had grade 3 SGS, of whom three (42.8%) required open surgery, three (42.8%) underwent balloon dilatation, and one (14.3%) underwent tracheotomy and subsequently died of sepsis; five (27.7%) had grade 2 SGS, of whom two (40%) underwent balloon dilatation, two (40%) underwent open reconstructive airway surgery, and one (20%) underwent endoscopic laser resection of the stenotic segment; and three (16.66%) had grade 1 SGS, of whom one (33%) underwent balloon dilation, one (33%) underwent tube dilation, and one (33%) did not require treatment. All patients were symptomatic at the time of their respective procedures. Clinical data for the groups (classified after revision FFL as SGS or no-SGS) are shown in Table 1.
Patient characteristics after final endoscopic exam.
| Stenosis | ||||
|---|---|---|---|---|
| Total | No, n (%) | Yes, n (%) | p-Value | |
| Sex | ||||
| Male | 111 (59.4) | 103 (60.9) | 8 (44.4) | 0.175 |
| Previous hospitalization | ||||
| Yes | 76 (40.9) | 71 (42.3) | 5 (27.8) | 0.235 |
| Diagnosis | ||||
| Bronchiolitis | 118 (63.1) | 106 (62.7) | 12 (66.7) | 0.322 |
| Other respiratorya | 36 (19.3) | 31 (18.3) | 5 (27.8) | |
| Meningitis | 11 (5.9) | 10 (5.9) | 1 (5.6) | |
| Other | 22 (11.8) | 22 (13.0) | 0 (0.0) | |
| Neuropathy | ||||
| Yes | 29 (15.6) | 26 (15.5) | 3 (16.7) | 0.895 |
| Median (interquartile range) [min–max]b | ||||
| Age (months) | 2.7 (1.5–6.7) [0.9–95.0] | 2.7 (1.6–6.5) [0.9–95.0] | 3.9 (1.4–12.1) [1.0–58.7] | 0.683 |
| Weight at intubation (g) | 5,500 (3,925–7500) [334–22,000] | 5420.0 (3831.3–7475.0) [334–22,000] | 6350.0 (4431.3–9113.8) [2110–12,000) | 0.274 |
| Days intubated | 7.0 (5.0–9.8) [1–33] | 7.0 (5.0–9.0) [1–31] | 8.0 (5.0–15.3) [3–33] | 0.118 |
| Mean (SD)c | ||||
| Gestational age (weeks) | 37.2 (3.1) | 37.1 (3.2) | 37.9 (2.3) | 0.295 |
| Intubation and mechanical ventilation | ||||
| Route | ||||
| Nasotracheal | 1 (0.5) | 1 (0.6) | 0 (0.0) | 0.999 |
| Orotracheal | 186 (99.5) | 168 (99.4) | 18 (100.0) | |
| Cuffed tube | ||||
| Yes | 43 (23.2) | 35 (21.0) | 8 (44.4) | 0.025d |
| No. of attempts | ||||
| 0–4 | 173 (96.1) | 156 (95.7) | 17 (100.0) | 0.383 |
| ≥5 | 7 (3.9) | 7 (4.3) | 0 (0.0) | |
| No. of reintubations | ||||
| 0 | 133 (71.5) | 125 (74.4) | 8 (44.4) | 0.033d |
| 1 | 43 (23.1) | 35 (20.8) | 8 (44.4) | |
| 2 | 8 (4.3) | 6 (3.6) | 2 (11.1) | |
| 4 | 2 (1.1) | 2 (1.2) | 0 (0.0) | |
SD, standard deviation.
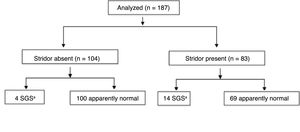
Of the 187 patients included in the study, 83 developed stridor during follow-up; therefore, the overall incidence of stridor in the sample was 44.38% (95% CI: 37.1–51.8). Of these, 49 (26.2% of the overall sample) had stridor for no longer than 72h post-extubation. Twenty-six children (13.9% of the overall sample) had stridor with onset in the first 72h post-extubation and continuing after this period, and four (2.1% of the overall sample) developed stridor ≥72h after extubation (72-h stridor positive). Long-term follow-up could not be performed in four patients (2.1%); however, none of these patients exhibited stridor for more than 3 days, and none was diagnosed with SGS. When we analyzed those patients who exhibited stridor only in the first 72h post-extubation, the incidence of post-extubation stridor was 26.2% (95% CI: 20.00–32.63).
Of the 18 patients who developed SGS, four (2.1% of 187) did not exhibit stridor and only one did not experience any signs or symptoms of upper airway obstruction during follow-up. Of the 169 patients without stenosis, 104 (55.6% of 187) did not develop stridor. Thus, stridor showed a sensitivity of 77.78% (95% CI: 51.9–92.6) and a specificity of 59.18% (95% CI: 51.3–66.6) for detection of SGS in this sample. The probability of SGS diagnosis in patients with stridor (positive predictive value, PPV) was 16.86% (95% CI: 9.8–27.1), and the probability of absence of SGS in the absence of stridor (negative predictive value, NPV) was 96.15% (95% CI: 89.9–98.7). The area under the ROC curve was 0.69 (95% CI: 0.57–0.81).
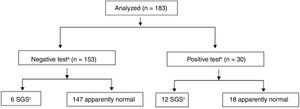
A similar analysis, taking into account duration and timing of stridor (defined as a positive test when stridor was present for >72h or developed >72h post-extubation) was performed. This analysis yielded a sensitivity of 66.67% (95% CI: 41.1–85.6), specificity of 89.1% (95% CI: 83.1–93.2), PPV of 40.0% (95% CI: 23.2–59.3), and NPV of 96.1% (95% CI: 91.3–98.4) for stridor as a diagnostic tool for SGS. The area under the ROC curve was 0.78 (95% CI: 0.65–0.91).
The distribution of patients according to development of stridor and timing of stridor (positive or negative at 72h) is shown in Figs. 1 and 2, respectively.
Flow chart of the analysis, stratified by presence or absence of stridor at 72h. Four patients were lost to follow-up.
SGS, subglottic stenosis.
a No stridor or stridor only in the first 72h post-extubation.
b Stridor lasting >72h post-extubation or developing after this period.
c Diagnosis confirmed through laryngoscopy under general anesthesia.
Bedside FFL, performed without sedation in the post-extubation period in a PICU setting, is useful, safe, and accurate for the evaluation of laryngeal lesions caused by intubation (including those in the subglottic region).6,7,16 According to Manica et al., this modality has 93.7% sensitivity and an NPV of 98.8% when used as a screening method for SGS in this setting.7
In this study, FFL was performed in all patients, regardless of symptoms, whereas direct laryngoscopy under general anesthesia was reserved for patients whose lesions persisted on follow-up examination or those who developed laryngeal symptoms during follow-up. All diagnoses of SGS were confirmed and classified by direct laryngoscopy. This probably accounts for the relatively high incidence of post-intubation SGS in this sample (9.3%) as compared with other studies.10,17–20
The incidence of post-extubation stridor in this population was 43.81%, which is quite high in comparison with other studies. However, incidence rates reported in the literature have varied widely, from 1% to 37%, which is explained by marked heterogeneity among studies in several aspects, including design, population, evaluation, follow-up period, and, particularly, the definitions applied.21–25
Other factors may also explain the higher incidence of stridor in the present study's population. First, patients were evaluated for stridor until hospital discharge, not only immediately after extubation. For calculation of incidence, the presence of stridor was considered independent of severity or treatment need. The young age of the studied population was also a risk factor for post-extubation stridor, and may have accounted at least partly for its high incidence.21,22,26–28 If only those patients who developed stridor in the first 72h after extubation are considered, the incidence decreases to 26.1%. Furthermore, the 95% CI of the incidence overlaps with the majority of previously published studies. Finally, studies that compared stridor to endoscopic diagnosis of laryngeal lesions caused by intubation are rare and have reported conflicting results.9–13
Two prior prospective studies conducted in the neonatal period used flexible bronchoscopy to evaluate the occurrence of airway lesions due to intubation and evaluate its association with stridor. Both reported divergent results. Fan et al. showed that stridor had high specificity, low sensitivity, and an NPV of 67% for detection of moderate or severe acute laryngeal lesions.9 Sherman et al. found high sensitivity and specificity of stridor in detecting moderate or severe SGS, and concluded that lesions associated with significant airway obstruction would rarely remain undiagnosed if only neonates with stridor were evaluated.10 It is worth noting that both studies evaluated patients for stridor at only one time point, i.e., immediately after extubation, and were restricted to neonatal samples.
Cordeiro et al., in a prospective study of 215 patients in a mixed pediatric and neonatal intensive care unit, evaluated the performance of a respiratory distress score (which included stridor among its variables) to detect airway lesions diagnosed by endoscopy immediately after extubation. Higher scores had 73.3% sensitivity and 58.6% specificity for detection of moderate or severe lesions. In patients with lower scores, the likelihood of absence of such lesions was 80.4%. Thus, the score had satisfactory performance for predicting absence of moderate or severe lesions in patients with mild distress.12
In the current study, analysis of the presence of stridor was found to be useful in establishing the likelihood of SGS among patients who did not develop stridor during the follow-up period, as demonstrated by the NPV of 96.15%. The specificity of only 54% can be justified by the fact that different types of laryngeal lesions may cause stridor. Moreover, transient vocal fold lesions (e.g., edema or granulation tissue) and acute alterations of vocal fold mobility are common causes of stridor in this period.29
The results of the present study are further explained by the timing of stridor occurrence during follow-up. Most patients who developed SGS showed persistent stridor, i.e., were positive for stridor at 72h. By considering only these patients as having a positive test, the specificity increased significantly to 89.1%. Furthermore, in this population, two out of every five children who experienced stridor onset or persistence >72h after extubation were ultimately diagnosed with SGS. As in previous studies, SGS could essentially be ruled out in patients who did not exhibit stridor and in those whose stridor resolved within 72h of extubation.
The results show that SGS due to intubation can still be diagnosed if airway endoscopy is restricted to patients who exhibit stridor during the post-extubation period. When considering the high specificity of persistent or late-onset stridor (lasting or beginning >72h post-extubation) for SGS, it seems relevant that these patients should undergo airway endoscopy under general anesthesia. Moreover, the area under the ROC curve in the second analysis shows that stridor can be considered an accurate marker of post-intubation SGS in the pediatric population.
Direct laryngoscopy under general anesthesia is considered the gold standard for visualization of the subglottic region; however, in this study, its use was restricted to specific patients. FFL was used for screening purposes because the objective was to evaluate all children endoscopically, irrespective of their symptoms, in a less invasive manner. In addition, FFL provides adequate visualization of the subglottis in the vast majority of patients. Furthermore, the follow-up period of at least 6 months decreased the likelihood of missed SGS diagnoses in this sample.
One of the limitations of this study was the use of a clinical marker (i.e., stridor) that is subject to interobserver variability. However, some authors have reported satisfactory agreement between clinical scores and stridor measurement, and excellent interobserver reliability, with kappa reaching 0.93 in a study conducted by Klassen and Rowe.30
In conclusion, absence of stridor proved to be adequate to rule out the diagnosis of post-intubation SGS in pediatric patients. Improved specificity was found when stridor persisted for >72h after extubation or when onset was >72h post-extubation. Given these findings, it seems appropriate to restrict airway endoscopy under general anesthesia for confirmation of SGS only in those patients who have stridor 72h following extubation.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Schweiger C, Eneas LV, Manica D, Netto CS, Carvalho PR, Piva JP, et al. Accuracy of stridor-based diagnosis of post-intubation subglottic stenosis in pediatric patients. J Pediatr (Rio J). 2020;96:39–45.
This study was performed in the Hospital de Clínicas de Porto Alegre, Unidade de Terapia Intensiva Pediátrica, Porto Alegre, RS, Brazil.