To verify whether early intervention focused on the family improves the cognitive, motor, and language development of children born preterm and/or at social risk in the first 3 years of life.
Source of dataMeta-analysis of clinical trials published between 2008 and 2018, in the following databases: CINAHL, MEDLINE – PubMed, MEDLINE – BVS, LILACS – BVS, IBECS – BVS, PEDro and Cochrane Reviews. Experimental studies on early interventions focused on the family, whose target groups were children born preterm and/or at social risk, with assessment of cognitive and/or motor and/or language development up to 3 years were included. The studies were rated using the PEDro Scale.
Data synthesisTwelve studies were included from a total of 3378 articles. Early intervention focused on the family contributed to the development of the cognitive (Standardized Mean Difference – SMD=0.48, 95% CI: 0.34–0.61) and motor (SMD=0.76, 95% CI: 0.55–0.96) domains of preterm infants. Regarding cognitive development, performance improvement was observed at 12, 24 and 36 months, while in the motor domain, the effect was observed only at 12 months in preterm infants. There was no benefit of the intervention in the cognitive, motor, and language outcomes of children with the social risk factor associated to biological risk.
ConclusionEarly intervention focused on the family has a positive effect on the cognition of preterm infants. The effect on motor development was lower, possibly due to the emphasis on interventions in family–child interaction. The effect of interventions on the development of children at social risk and on the language domain was inconclusive, due to the scarcity of studies in the area.
Verificar se a intervenção precoce com foco na família melhora o desenvolvimento cognitivo, motor e a linguagem de crianças nascidas prematuras e/ou em risco social nos primeiros três anos de vida.
Fontes de dadosMetanálise de ensaios clínicos publicados entre 2008 a 2018, nas bases de dados CINAHL, Medline – Pubmed, Medline – BVS, Lilacs – BVS, IBECS – BVS, PEDro e Cochrane/Reviews. Foram incluídos estudos experimentais de intervenção precoce com foco na família cujo público-alvo eram prematuros e/ou crianças em risco social com avaliação do desenvolvimento cognitivo e/ou motor e/ou linguagem até os três anos. Os artigos foram pontuados pela Escala PEDro.
Síntese dos dadosDo total de 3378 artigos, 12 estudos foram incluídos. A intervenção precoce com foco na família contribuiu para o desenvolvimento dos domínios cognição (DMP=0,48; 95% IC: 0,34–0,61) e motor (DMP=0,76; 95% IC: 0,55–0,96) de prematuros. Na cognição, a melhora do desempenho foi observada aos 12, 24 e 36 meses, enquanto no domínio motor, o efeito foi observado apenas aos 12 meses nos prematuros. Não houve benefício da intervenção nos desfechos cognitivo, motor e linguagem de crianças com fator de risco social associado ao biológico.
ConclusãoIntervenção com foco na família tem efeito positivo sobre a cognição de crianças prematuras. O efeito no desenvolvimento motor foi menor, possivelmente devido à ênfase das intervenções na interação família-criança. O efeito das intervenções sobre o desenvolvimento de crianças em risco social e no domínio da linguagem foram inconclusivos, devido à escassez de estudos na área.
Early childhood is a critical period for brain maturation, being crucial for cognitive, socio emotional, and physical development. It is at this stage that neural circuits are formed or strengthened through interactions with the environment.1–3 Estimates indicate that in low- and middle-income countries, more than 200 million (43%) of children up to 5 years of age fail to reach their development potential due to exposure to biological, psychosocial, and environmental risks, such as inadequate stimulation in the home environment.4,5 In preschool, children exposed to these factors may show a higher frequency of emotional difficulties, agitated behavior, deficiencies in executive functions and self-control, learning disabilities, Attention Deficit Hyperactivity Disorder (ADHD), and mental health problems.2,6,7
In low- and middle-income countries, social and biological risks, represented by prematurity, often occur concomitantly.8,9 Prematurity is associated with increased neonatal morbidity that generates risk for sensory and attention deficits, learning disabilities, ADHD and autism symptoms, motor or global developmental delay, and Cerebral Palsy (CP), which limits social participation and reduces the quality of life of these children.10–15
Investments in early childhood can reduce the effects of social and biological risks and bring benefits throughout life. Early intervention refers to preventive programs implemented shortly after birth and up to 3 years of age8 and consists of multidisciplinary clinical-therapeutic services provided to children at risk and their families for the purpose of promoting child health and well-being, stimulating emerging skills, minimizing development delays, reducing existing disabilities, preventing loss of functionality, contributing to the structuring of the mother–baby bond and the reception of these children by the family, and promoting adaptive parenting and overall family functioning.16,17
Early intervention focused on the family aims to support family dynamics in the domestic environment.18 This type of approach has been recommended due to the possibility of influencing the care and stimuli offered daily by the family and, consequently, having a positive impact on the child's development.18–22 Its main components are psychosocial support and parental education.23 Psychosocial support to parents is aimed at reducing stress, anxiety, and depressive symptoms, as well as increasing maternal self-efficacy, sensitivity, and the mother's ability to respond in interactions with her child, which has a positive effect on the child's environment and contributes to improving the developmental outcome.23 Parental education aims to increase the parents’ capacity, knowledge, and ability to care for their baby.23
Although it seems intuitive that improving the parent–child relationship results in gains for the baby's development, the effectiveness of early intervention focused on the family programs has yet to be fully established. The planning of scientific evidence-based interventions allows the prioritization of problems, the estimation of risks and benefits of the intervention, and the monitoring and evaluation of the results.24 The synthesis of scientific evidence generated by systematic reviews and meta-analyses, together with the experience of health professionals and patient preferences, can also support decision-making in clinical practice.25 In this sense, the purpose of this meta-analysis was to evaluate and synthesize the evidence available in the literature about the effects of early intervention focused on the family programs on the cognitive, motor, and language development of preterm children and/or those at social risk in the first 3 years of life.
MethodsThe protocol for this review was registered in PROSPERO: the International Prospective Register of Systematic Reviews (CRD 42018082059) (available at http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018082059). The review followed the recommendations of the Cochrane Library26 and Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).27 Two independent authors carried out the literature search in the CINAHL, MEDLINE – PubMed, MEDLINE – BVS, LILACS – BVS, IBECS – BVS, PEDro, and Cochrane Review databases for studies published in the last 10 years (January 2008–August 2018), in three languages (Portuguese, English, and Spanish).A search was also carried out in the reference sections of the studies found in the databases. Three search strategies were used, using previously chosen terms after consulting the Health Sciences Descriptors (DeCS), including the following terms: (1) Infant or Infant, Premature or Premature or Infant, Newborn and Child Development or Language Development or Child Language or Psychomotor Performance or Motor Skills or Cognition and Early Intervention (Education) or Early Intervention; (2) Infant or Infant, Premature or Premature or Infant, Newborn and Developmental Disabilities or Delay Development and Early Intervention (Education) or Early Intervention; (3) Infant or Infant, Premature or Premature or Infant, Newborn and Motor Skills Disorders or Cognition Disorders or Movement Disorders or Language and Early Intervention (Education) or Early Intervention.
Selection criteriaThe following were included: (1) Experimental studies, such as randomized, quasi-experimental, and single-case experimental trials; (2) Studies whose target audiences were premature children with gestational age<37 weeks, without neuromotor abnormalities or congenital abnormalities, and/or children at social risk; (3) Studies on early intervention focused on the family programs that included at least one of the following two main components: psychosocial support to parents, which could be psychological counseling or social support and/or parental education, which could include information on child development, demonstrations of child behavior with discussion, or parental involvement in parent–baby interaction activities, with feedback from the professional; (4) Early intervention focused on the family programs, performed during home visits and/or during the outpatient consultation, before and/or after hospital discharge, with individual and/or group care; (5) Those in which motor and/or language and/or cognition development were evaluated up to the third year of life through standardized tests. Systematic reviews and/or meta-analyses, longitudinal, cross-sectional, case reports, cohort, and case-control studies were excluded. All studies were evaluated by the PEDro scale of the Physiotherapy Evidence Database,28 excluding those with a score≤5.
Validity and bias risk assessmentEligibility and quality evaluation of the studies were conducted by two independent evaluators, who initially analyzed titles and abstracts to obtain potentially relevant studies. Those that met the eligibility criteria of this review were read in full and scored according to the PEDro scale criteria28 to assess the methodological quality.
The PEDro scale28 is based on the Delphi list and has 11 items, and the item “specification of inclusion criteria” is not scored, whereas the other items of the scale are: subject inclusion criteria; random allocation; allocation concealment; similarity of the groups in the initial phase; masking of the subjects, the therapist, and the evaluator; measurement of at least one key result; analysis of intention to treat; results of the statistical comparison between groups and reporting of measures of variability; and accuracy of at least one outcome. Each item receives one point when it meets the response criteria, for a total of ten points. In the present study, aiming to select studies with greater methodological accuracy, a cutoff score>5 was used.
The risk of bias analysis of the included studies was performed by two reviewers, according to the Cochrane Handbook for Systematic Reviews of Intervention, taking into account the generation of a randomization sequence, allocation concealment, masking, incomplete data, and other sources of bias. Each item was classified as “low risk of bias”, “high risk of bias” or “unknown risk of bias”.29
Data analysisA table with the following variables was created to analyze the data: study identification (title and authors), year of publication, country where the study was performed, sample size and characteristics, children's age, early intervention characteristics (description of the intervention, age at the intervention, individual- or group-based, carried out at the hospital or at home, before or after hospital discharge, and number of sessions), outcomes, evaluation tools, results/conclusions and PEDro scores.28
To obtain the analysis of the combined estimate of the intervention effects, post-intervention scores were extracted and analyzed using the fixed-effect model. In the case of statistically significant heterogeneity (I2>40%), a random effects model was applied. The pooled data from all outcomes were recorded as the Standardized Mean Difference (SMD) and their respective 95% Confidence Intervals (95% CI). The analyses were performed using the Comprehensive Meta-Analysis software30 (version 3.0; Biostat – Englewood, New Jersey, USA). The critical value to reject the null hypothesis was set at a level of 0.05 (two-tailed).
ResultsFlowchart of the review studiesThe electronic search identified 3378 studies in the different databases, whose titles and/or abstracts were analyzed. Of these, 3345 were excluded and the 33 potentially eligible studies had their texts analyzed. Based on the reading of the full texts, 13 studies were selected and scored using the PEDro scale.28 Of these, three were excluded because they showed scores≤5, and therefore, ten were selected. During the manual search of the references of the 10 studies selected from the database, another 10 were found, but only two studies were related to the topic and received scores>5 according to the PEDro scale. Therefore, 12 studies were included in the qualitative analysis and 10 studies were included in the quantitative analysis (meta-analysis). Fig. 1 depicts the review flowchart (adapted from PRISMA).
Characteristics of the included studiesThe 12 studies selected for the review included 2559 participants (intervention=1305 and control=1254) and investigated seven intervention modalities to promote better child development; they had guidelines for parents and parental education as a common component. All clinical trials compared the intervention to the control group, which received the usual care consisting of standard service care without the intervention, including referral to an early intervention/physical therapy service if the health team considered it necessary20,21,31–33; clinical care, massage guided by a physical therapist, and follow-up after discharge34,35; usual care with child-centered interventions and visits to the neonatal clinic36; usual care that included the kangaroo mother care position and method37; home visits based on the World Health Organization (WHO) curriculum5,38 and in only one study, the standard care was not specified.39 The characteristics of the intervention and the control follow-up in the reviewed studies are summarized in Table 1.
Characteristics of intervention programs and procedures performed in the control group of the included studies.
| Author/year | Description of intervention | Intervention component | Intervention type | Place of intervention | N° of sessions and age at the intervention | Control | |||
|---|---|---|---|---|---|---|---|---|---|
| Parental education | Support to parents | Individual | Group | Hospital outpatient clinic | Home | ||||
| Spittle et al.31 (2018) | VIBeS Plus – two components: (1) strategies to promote enriched environment, positive play, general developmental milestones, feeding, sleep, and well-being of parents, (2) specific content that was targeted to the baby and family based on goals and/or concerns identified by the parents. | Yes | Yes | Yes | – | – | Yes | N° of sessions: 9 sessions after discharge. Age: first 12 months | Control and intervention group received standardized care: included access to a child health nurse and early intervention service, if it was considered appropriate by the child's health team. |
| Van Hus et al.32 (2016) | IBAIP – offer support to the child's regulatory competence and multiple development functions through child-parent interaction. Based on the synchronous-active model of the neonate's behavioral organization, guided by the Infant Behavioral Assessment, a systematic observation tool for the recording and interpretation of the baby's communication behaviors. | Yes | – | Yes | – | Yes | Yes | N° of sessions: 7 to 9 sessions (1 before hospital discharge and 6 to 8 sessions during home visits). Age: first 6 months | Usual care: including referral to regular pediatric physical therapy if deemed necessary by the pediatrician. |
| Chang et al.39 (2015) | Development Media International, London, UK-demonstration using films depicting the behaviors that the intervention should stimulate, followed by discussion and demonstration of the viewed activities. The mothers practiced the activities with their children and were encouraged to perform them at home. | Yes | – | – | Yes | Yes | – | N° of sessions: 5 outpatient sessions performed after discharge. Ages: 3, 6, 9, 12, and 18 months | Usual care: not specified by the study |
| Wu et al.36 (2014) | It consisted of two intervention groups in the same program, which was differentiated only regarding location: one was performed at the hospital and the other at home. Intervention centered on the child-parent dyad and clinical consultations. Prior to hospital discharge, the intervention was guided by principles of the synchronous-active Theory and family-centered care. After discharge, the theory of biosocial systems was used. | Yes | Yes | Yes | – | Yes | Yes | N° of sessions: 13 sessions (5 sessions before discharge and 8 sessions after discharge). Ages: 36, 38, and 40 weeks before discharge and 1 week after discharge, 1, 2, 4, 6, 9 and 12 months of age after discharge. | Usual developmental care, which consisted of intra-hospital interventions centered on the child and consultation at the neonatal clinic |
| Wallanderet al.5 (2014) | Partners for Learning –which encompasses the areas of cognition, fine and gross motor, social, self-help and language skills. Parents were trained to perform activities that were adequate to the child's development and practiced them in the presence of the professional, who gave feedback. Parents received cards describing activities and were encouraged to apply activities during the routine care of the child until the next home visit. | Yes | – | Yes | – | – | Yes | N° of sessions: 72. Age: first 3 years. | Home visits: WHO curriculum (2014) which addressed, for instance, breast feeding, nutrition, hygiene and vaccination. |
| Bann et al.38 (2016) | Partners for Learning – same characteristics mentioned in the study by Wallander et al.5 (2014). | Yes | – | Yes | – | – | Yes | N° of sessions: 72 sessions. Age: first 3 years | Same characteristics as the study by Wallander et al.5 (2014) |
| Spittle et al.21 (2010) | VIBeS Plus – same characteristics mentioned in the study by Spittle et al.31 (2018) | Yes | Yes | Yes | – | – | Yes | N° of sessions: 9 Sessions after discharge. Age: first 12 months | Same characteristics as the study by Spittle et al.31 (2018) |
| Koldewijn et al.33 (2010) | IBAIP – same characteristics mentioned in the study by Van Hus et al.32 (2016) | Yes | – | Yes | – | Yes | Yes | N° of sessions: 7 to 9 sessions (1 before discharge and 6 to 8 sessions at home). Age: first 6 months | Same characteristics as the study by Van Hus et al.32 (2016) |
| Nordhov et al.34 (2010) | Mother–Infant Transaction Program – modified version: it addressed aspects such as the child's reflexes, self-regulation, signs of distress and the child's predominant states and adjustment to the home environment, parent–child interactions, how to guide and stimulate the child, and discussion and evaluation of the intervention program. | Yes | – | Yes | – | Yes | Yes | N° of sessions: 11 sessions (7 sessions before discharge and 4 home visits). Ages: 3, 15, 30, and 90 days after discharge | Usual care for discharge: clinical examination, infant massage training performed by physical therapist. Both groups had access to follow-up after discharge |
| Koldewijn et al.20 (2009) | IBAIP – same characteristics mentioned in the study by Van Hus et al.32 (2016). | Yes | – | Yes | – | Yes | Yes | N° of sessions: 7 to 9 sessions (1 before discharge and 6 to 8 sessions at home). Age: first 6 months | Same characteristics as the study by Van Hus et al.32 (2016) |
| Peters et al.37 (2009) | NIDCAP – Characterized by observation of baby's behavior. Encourages parental led involvement guided by the baby and requires parents to respond to individual infant behaviors, be more flexible in caring and modify the environment in accordance with observed behaviors. | Yes | – | Yes | – | Yes | – | N° of sessions: 7 sessions (carried out in the ICU). Age: not informed | Usual care that included positioning, kangaroo method, but without intervention and behavioral observation |
| Kaaresen et al.35 (2008) | Mother–Infant Transaction Program-modified version – the same characteristics mentioned in the study by Nordhov et al.34 (2010) | Yes | – | Yes | – | Yes | Yes | N° of sessions: 11 sessions (7 sessions before discharge and 4 home visits). Ages: 3, 15, 30 and 90 days after discharge | The same characteristics mentioned in the study by Nordhov et al.34 (2010) |
VIBeS Plus, Victorian Infant Brain Studies; IBAIP, Infant Behavioral Assessment and Intervention Program; NIDCAP, Newborn Individualized Developmental Care and Assessment Program; Bayley II, The Bayley Scales of Infant Development, 2nd Edition; Bayley III, The Bayley Scales of Infant Development, 3rd Edition.
The overall characteristics and outcomes of the studies are summarized in Table 2. Most of the selected studies were carried out in high-income countries: the Netherlands (three), Norway (two), Australia (two) and Canada (one). The other studies are from low- and middle-income countries: India, Pakistan, and Zambia together had two studies published, and Taiwan, Jamaica, Antigua, and Saint Lucia published one study each. Most of them – 9 of the 12 included – reported positive effects of cognition intervention. Regarding the motor outcome, 5 of the 11 studies that evaluated this outcome found positive effects. However, in the four studies that evaluated language, no effects of the intervention were observed.
General characteristics and outcomes of included studies.
| Author/year | Participants | Country of origin of the sample | Intervention/evaluation tool/age at evaluation | Positive effect of the intervention on development | Additional information on the effect | ||
|---|---|---|---|---|---|---|---|
| Cognition | Motor | Language | |||||
| Spittle et al.31 (2018) | PMT GA<30 weeks classified as high or low social risk. n=120 (intervention group n=61, control group n=59). | Australia | VIBeS Plus/Bayley III; Age: 24 months | Yes | No effect | No effect | Higher mean cognitive score in the intervention group (101.8; SD=11.0) of the children at social risk when compared to the control group (92.2; SD=12.5); p=0.006 at 24 months of age |
| Van Hus et al.32 (2016) | PMT GA<32 weeks and/or BW<1500g; n=176 (intervention group n=86, control group n=90). | The Netherlands | IBAIP/Bayley II; Ages: 6, 12, and 24 months | Yes | Yes | Not evaluated | Positive longitudinal effect of intervention on motor development (SD=0.4; p=0.006), but not on cognition (p=0.063). Children with bronchopulmonary dysplasia had a significant longitudinal effect on cognitive (SD=0.7 p=0.019) and motor outcomes (SD=0.9, p=0.026). |
| Chang et al.39 (2015) | Children at social risk (born full-term): n=501 (intervention group n=251, control group n=250). | Jamaica, Antigua, and Santa Lucia (Caribbean) | Development Media International, London, United Kingdom/Griffith Mental Development Scales and MacArthur-Bates Short Form of the Communicative Development Inventory (CDI). Age: 19.7 months. | Yes | No effect | No effect | Significant effect on cognition (3.09 points, 95% CI: 1.31–4.87, effect size=0.3), but not on language or motor development. |
| Wu et al.36 (2014) | PMT GA<37 wks. and BW <1500g: n=178 (outpatient intervention group n=57, home intervention group n=63, control group n=58). | Taiwan | Synchronous-active theory and family-centered care/Bayley III.Age at assessment: 24 months. | Yes | Yes | No effect | Outpatient intervention group had a higher cognition score compared to the control group (difference=4.4, 95% CI: 0.8 to −7.9) and a lower rate of motor development delay (OR=0.29, 95% CI: 0.08–0.99). |
| Wallander et al.5 (2014) | Children at socioeconomic disadvantage (preterm and full term) n=407 (intervention group n=204, control group n=203). | Rural areas of India, Pakistan, and Zambia | Partners for Learning/Bayley II. Age at evaluation: 12, 24 and 36 months. | Yes | Yes | Note valuated | Considering the interaction between age and intervention, the children in the intervention group showed a better trajectory in the development of cognition in the three evaluations (12, 24, and 36 months). At 36 months, the children in the intervention group showed a significantly higher motor score compared to the control group. |
| Bann et al.38 (2016) | Children at socioeconomic disadvantage (preterm and full term) n=293 (intervention group n=146, control group n=147). | Rural areas of India, Pakistan, and Zambia | Partners for Learning/Bayley II. Age at evaluation: 12, 24 and 36 months | Yes | Not evaluated | Not evaluated | In the economically disadvantaged children, the intervention group showed a higher mental score than the control group at 36 months of age (p=0.001). |
| Spittle et al.21 (2010) | PMT GA<30 wks.: n=120 (intervention group n=61, control group n=59). | Australia | VIBeS Plus/Bayley III. Age at evaluation: 24 months. | No effect | No effect | No effect | There was no statistically significant difference regarding the cognition, language, and motor scores (p=0.20, p=0.67, p=0.66, respectively). |
| Koldewijn et al.33 (2010) | PMT GA<32 weeks and/or BW<1500g: n=176 (intervention group n=86, control group n=90). | The Netherlands | IBAIP/Bayley II. Age at evaluation: 24 months | Yes | Yes | Not evaluated | After adjustment for perinatal variables, there was an effect of 6.4 (standard error=2.4) on the motor development index favorable to the intervention children. After the post hoc analysis, there was better mental development after the intervention in the subgroups of children with bronchopulmonary dysplasia associated with social and biological risk factors. |
| Nordhov et al.34 (2010) | PMT BW<2000g n=146 (intervention group n=72, control group n=74). | Norway | Mother–Infant Transaction Program-modified version/Bayley II. Age at evaluation: 3 years. | No effect | No effect | Not evaluated | At 3 years of age, in the analysis after adjustment for maternal education, no significant difference was found between the intervention and control groups regarding the mental development index score of 4.5 points (95% CI: −0.3 to 9.3) |
| Koldewijn et al.20 (2009) | PMT GA<32 weeks and/or BW<1500g, n=176 (intervention group n=86, control group, n=90). | The Netherlands | IBAIP/Bayley II. Age at evaluation: 6 months | Yes | Yes | Not evaluated | After analysis with a multivariate regression model, the mean MDI score was 106 (SD=2.12) for the intervention group and 99 (SD=2.18) for the control group (p=0.02). In the motor score, the mean PDI score was 98 (SD=1.63) in the intervention group and 92 (SD=1.66) in the control group (p=0.008). |
| Peters et al.37 (2009) | PMT GA≤32 weeks, BW between 500 and 1250g; n=120 (intervention group=60, control group=60). | Canada | NIDCAP/Bayley II. Age at evaluation: 18 months. | Yes | No effect | Not evaluated | Lower frequency of cognition delay (intervention: 10%, control: 30%; OR=0.25; 95% CI: 0.08–0.82, p=0.017). |
| Kaaresen et al.35 (2008) | PMT BW<2000g: n=146 (intervention group n=72, control group n=74). | Norway | Mother–Infant Transaction Program-modified version/Bayley II. Age at evaluation: 24 months. | No effect | No effect | Not evaluated | Mental development index: Difference between the means of the intervention and control groups equal to 0.7 (95% CI: −4.3 to 6.0) (p=0.74).Motor development index: Difference between the means of the intervention and control groups equal to 1.2 (95% CI: −4.3 to 6.8) (p=0.66). |
PMT, prematurity; BW, birth weight; GA, gestational age; VIBeS Plus, Victorian Infant Brain Studies; IBAIP, Infant Behavioral Assessment and Intervention Program; MDI, Mental Developmental Index; PDI, Psychomotor Developmental Index; NIDCAP, Newborn Individualized Developmental Care and Assessment Program; Bayley II, Bayley Scales of Infant Development, 2nd Edition; Bayley III, Bayley Scales of Infant Development, 3rd Edition.
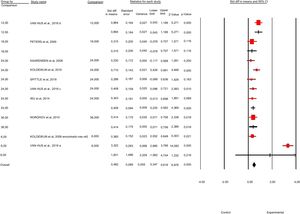
All studies were randomized clinical trials, with PEDro scale scores ranging from 6 to 8 points (mean of 6 points) (Supplementary Material 1 presents the score details). Regarding the risk of bias (Fig. 2), the absence of subject allocation concealment was observed for the intervention and the control groups in six studies, absence of masking of the participants and of the professional who performed the clinical trial intervention was observed in all studies, as well as differences in the sample characteristics in the intervention and control groups at baseline in two studies.
ParticipantsMost reviewed studies had a target audience of preterm children, with three evaluating children born with gestational age<32 weeks and/or weighing less than 1500grams (g)20,32,33; one evaluating children born with age gestational age<32 weeks and/or birth weight between 500g and 1250g37; and one whose sample had a gestational age<30 weeks.21 The other studies that assessed preterm infants had as inclusion criteria only birth weight<2000g34,35 and one had participants with birth weight<1500g.36 All studies that assessed preterm infants had exclusion criteria for congenital abnormalities. The other studies (four) assessed children considered to be at socioeconomic risk, but only one study exclusively assessed social risk, excluding preterm children.39 In the others, children with and without neonatal asphyxia were included, both at-term and preterm infants, excluding preterm infants with birth weight<1500g5,38 and one study assessed premature infants with gestational age<30 weeks, who were classified as having high or low social risk.31
Assessment of cognitive, motor and language developmentThe cognitive outcome was assessed in all of the reviewed studies, whereas 11 studies assessed the motor development, but only four studies included language assessment. The Bayley Scales of Infant Development 2nd Edition (Bayley II) was the test used for outcome evaluation in most studies (eight studies).5,20,32–35,37,38 The other studies used the Bayley Scales of Infant Development 3rd Edition (Bayley III) (three studies)21,31,36 and the Griffith Mental Development Scales and the MacArthur-Bates Short Form of the Communicative Development Inventory (CDI) (one study).39
The age at the evaluation of child development varied greatly, and in one-third of the studies the evaluation was performed at 24 months (four studies). In the others, the evaluations were performed from 12 to 36 months of age (one study); at 12, 24 and 36 months (two studies); at 18 months (one study); and at 6 months (one study). In three studies, a longitudinal evaluation was performed for a longer period, in two studies up to five and a half years and in one study up to 8 years, but as the focus of the meta-analysis was interventions in the first 3 years of life, only the results related to this age group were considered.
Characteristics of the early intervention focused on the family programsTable 1 shows the characteristics of early interventions focused on the family. In most studies, the interventions were individual, with a number of sessions ranging from 5 to 13, mostly performed after hospital discharge and during the child's first 12 months of life20,21,31–36 and all interventions involved components of guidelines for parents and parental education to stimulate child development, mainly through the synchronous-active theory.20,32–37 Although the purpose of this review was to address interventions focused on the family in most studies, the family was restricted to the involvement of mothers and fathers, with the exception of the study by Chang et al.,39 in which early intervention involved only the mothers.
The Infant Behavioral Assessment and Intervention Program (IBAIP) was investigated in three studies,20,32,33 the Mother–Infant Transaction Program-modified version in two,34,35 one study used the Newborn Individualized Developmental Care and Assessment Program (NIDCAP),37 two studies used the Victorian Infant Brain Studies (VIBeS Plus)21,31 and two studies had their interventions based on the Partners for Learning curriculum.5,38 The other two addressed educational guidelines for parents through film viewing, discussions and support to parents.36,39
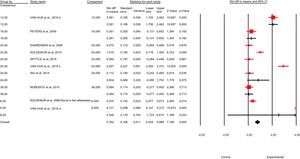
Effects of early intervention focused on the family on cognitionThe effects of the early intervention focused on the family on the cognition of preterm children were evaluated in eight clinical trials.20,21,32–37 The interventions and respective assessment tools used in the studies were: IBAIP and Bayley II20,32,33; Mother–Infant Transaction Program – modified version and Bayley II34,35; VIBeS Plus team and Bayley III21 and NIDCAP and Bayley II.37 In one of the studies,36 two groups underwent the same early intervention focused on the family, one at home and the other at the outpatient clinic, using the Bayley III evaluation tool. All the interventions showed previously mentioned characteristics, based mainly on the synchronous-active theory.20,32–37 The control groups received the usual service care, but without the early intervention focused on the family.
The analysis of the intervention effects on the cognition of preterm infants was performed by grouping data from the eight studies (n=1238 participants; intervention=643, control=595). In the overall result, children receiving an early intervention focused on the family had a standardized mean of cognitive scores of 0.48 (95% CI: 0.34–0.61, p-value<0.001, I2=39%), higher than the children who received the usual service care. In two studies, the intervention effects on cognition were evaluated at 6 months of age20,32 and there was no significant change in cognition (SMD=1.83, 95% CI: −1.08 to 4.74, p=0.21, I2=39%).
In the study in which the evaluation was performed at 12 months, 32 children who received the intervention showed a standardized mean of 0.86 (95% CI: 0.54–1.18, p<0.001, I2=39%) higher than the control group. In the study with evaluation at 18 months,37 there was no significant change in cognition (SMD=0.31, 95% CI: −0.07 to 0.7, p=0.11, I2=39%).In five studies the evaluation was carried out at 24 months31–33,35,36 and the children who received the intervention showed a standardized mean of cognitive scores of 0.4 (95% CI: 0.22–0.59; p<0.001; I2=39%), higher than the children in the control group. In a single study,34 the evaluation was performed at 36 months and there was an increase in the standardized mean of cognitive scores of 0.41 (95% CI: 0.22–0.59, p=0.018, I2=39%) in the children from the intervention compared to the control group (Fig. 3).
Of the four studies that evaluated cognition in the sample of children considered to be at social and/or biological risk, two studies performed home interventions based on the Partners for Learning curriculum5,38 and the effect was evaluated by the Bayley II scale. In another study, the intervention was performed by the VIBeS Plus team and the tool was the Bayley III scale.31
In the fourth clinical trial,39 the intervention consisted of showing short films by health education consultants (Development Media International, London, United Kingdom), followed by discussion groups about the films and practical activities with children, with the mothers being encouraged to perform these activities at home with their children.
The cognitive outcome was evaluated using the Griffith Mental Development Scales and the MacArthur-Bates Short Form of the CDI. Regarding the characteristics of the interventions, all had a component that presented guidelines for parents for the development of the children, which were performed after hospital discharge, with variations related to the other characteristics.
The analysis of the intervention effects on the cognition of children at social and/or biological risk was performed by pooling data from two studies5,31 (n=527 participants; intervention=265, control=262). It was not possible to include the study by Bann et al.,38 because they did not have the necessary data for the meta-analysis. Although the initial proposal was to consider only children at social risk, this was not possible, since only one study was identified39 with this type of sample. Therefore, the meta-analysis was performed with the two studies that included children at social and biological (prematurity) risk: Wallander et al.,5 who included preterm and at-term children with high social risk, and Spittle et al.,31 whose sample of preterm infants was classified as high or low social risk.
In the overall result, the intervention focused on the family did not promote a significant change in cognition (SMD=0.79, 95% CI: −0.31 to 0.46, p=0.69, I2=1%) when compared to children from the control group. In the two studies that assessed cognition of children at high social risk (SMD=0.38, 95% CI: −0.32 to 1.08, p=0.29, I2=1%), there was no significant difference in the cognition scores. In the study whose sample had low social risk (SMD=−0.05, 95% CI: −0.52 to 0.41, p=0.82, I2=1%) there was also no significant difference in cognition (For the plot, see Supplementary Material 2).
Effects of early intervention focused on the family on motor developmentThe eight studies that evaluated cognition in preterm infants also evaluated the motor outcome, thus the characteristics of the studies are the same as those reported for the cognition outcome.
The effects of the intervention on the motor outcome in the preterm population were analyzed by pooling the data from the eight studies (n=1238 participants; intervention=643, control=595).20,21,32–37 In the overall result, children who received early intervention focused on the family had a standardized mean of motor development scores of 0.76 (95% CI: 0.55–0.96; p<0.001; I2=88%), higher than the children who received routine care at the service. Similarly to cognition, in two studies the motor outcome was evaluated at 6 months (SMD=2.54, 95% CI: −1.72 to 6.81, p=0.24, I2=88%) and there was no significant change. In only one study, the evaluation was performed at 12 months, and the children in the intervention group had a standardized mean of motor development scores of 2.08 (95% CI: 1.7–2.46; p<0.001; I2=88%), higher than the children in the control group. One study evaluated the motor outcome at 18 months (SMD=0.26, 95% CI: −0.13 to 0.65, p=0.19, I2=88%), five studies at 24 months (SMD=0.83, 95% CI: −0.08 to 1.75, p=0.07, I2=88%) and one study at 36 months of age (SMD=0.06, 95% CI: −0.27 to 0.4, p=0.71, I2=88%), showing no significant change in the motor domain at these age ranges (Fig. 4).
In three of the four previously described studies regarding the cognitive outcome, motor development evaluation was also performed in children at social and/or biological risk.5,31,39 The analysis of the effects of intervention on motor development was performed by pooling data from two studies (n=527 participants: intervention=265 and control=262).5,31 The study by Chang et al.39 was excluded and the studies by Wallander et al.5 and Spittle et al.31 were included in the analysis, as previously justified in the cognition outcome. In the overall result, there was no significant difference regarding the motor development of children at social and/or biological risk who received the intervention (SMD=0.12, 95% CI: −0.05 to 0.29, p=0.18, I2=0%), when compared to controls. In the two studies focused on the motor development of children at high social risk (SMD=0.16, 95% CI: −0.03 to 0.35, p=0.1, I2=0%), there was no significant difference between the control and intervention groups, nor in the study that included children at low risk (SMD=−0.1; 95% CI: −0.57 to 0.36; p=0.65; I2=0%) (Supplementary Material 3 presents the plot).
Effects of early intervention focused on the family on languageTwo studies evaluated the effects of the intervention on the language of preterm infants. One of the studies is related to the intervention developed by the VIBeS Plus team, whose language evaluation was performed using the Bayley III scale.21 In the other study,36 two groups underwent the same intervention focused on the family, with a difference related only to the intervention location – at home or at the outpatient clinic – and the evaluation tool was also Bayley III. Regarding the characteristics of the interventions, all had guidelines for the parents’ component on the children's development, and most were performed individually, with the number of sessions varying from 9 to 13 during the first 12 months of the child's life, which occurred after hospital discharge. The control group received the service's routine care, but without the intervention.
The analysis of the intervention effects on the language of the preterm population was performed by pooling data from the two studies (n=298 participants: intervention=181 and control=117).21,36 The analyzed studies did not show any significant difference in the children's language when comparing those who received the intervention (SMD=0.02, 95% CI: −0.23 to 0.27, p=0.87, I2=0) when compared to those who received the usual service care. (Supplementary Material 4 presents the plot).
Among the population at social and/or biological risk, in the study in which short films created by Development Media International were exhibited,39 the language was evaluated, on average, at 19 months of age, using the language subscale of the Griffith Mental Development Scales and the MacArthur-Bates Short Form of the CDI. In the study by Spittle et al.,31 language was evaluated at 2 years of age using the Bayley III scale. Both studies showed no significant effects on language. It was not possible to carry out meta-analysis, since Chang et al.39 excluded preterm infants from the sample and Spittle et al.31 investigated preterm infants and therefore, the samples were considered heterogeneous for meta-analysis.
DiscussionThis review aimed to verify the effects of early intervention focused on the family on cognition, motor development, and language of children born preterm and/or at social risk in the first 3 years of life. Twelve studies were included, most with moderate quality,5,20,21,31–33,36,38,39 which were mainly conducted in high-income countries.20,21,31–35,37 The samples consisted mainly of children born prematurely20,21,31–37 and the only domain evaluated in all studies was the cognitive domain, with language being evaluated in only four studies.21,31,36,39 The programs based on the synchronous-active theory were the most frequently used.20,32–37
In the overall result, early intervention focused on the family contributed to the development of cognition in preterm infants when compared to the usual care. This result is similar to that of the meta-analysis performed by Vanderveen et al.,22 which aimed to evaluate interventions involving parents in the development of preterm infants. Similar results regarding cognition were also found in a meta-analysis carried out by Spittle et al.,18 which observed improvement in the cognitive outcome in the group of children who received intervention in the first 3 years of life compared to controls, although the intervention was not exclusively focused on the family. Considering the age group, there was a positive effect of intervention on the cognitive domain at 12, 24 and 36 months of age, but not at 6 and 18 months of age. Vanderveen et al.22 also found positive effects of the intervention on the cognitive development of preterm infants at ages 12, 24 and 36 months, but not at 6 months.
The effect of early intervention focused on the family on the cognition of preterm children, evident at different ages, is possibly associated with the types of analyzed intervention programs, which, for the most part, were based on the principles of the synchronous-active theory.20,32–37 According to this theory, to maintain the organization of behavior and adaptively respond to the environment, the baby depends on the interaction between five basic subsystems (autonomic, motor, state-organizational, attention and interaction, and self-regulation).40
Neonatal behavior is expressed through signs associated with each subsystem, which can be recognized by the parents, thus identifying the baby's individual needs, respecting the rhythm of development and the adequate time for stimulation, manipulation, and interaction.40 Based on this theory, most of the programs analyzed were aimed at improving reciprocity in parent/baby relations, promoting the baby's self-regulation and better parental understanding of the child's needs. Better understanding of the baby's communication signs favors the provision of positive physical and emotional experiences for the child, leading to better neurodevelopment responses, including the cognitive outcome in the preterm infant sample.
Similarly, in the overall result, early intervention focused on the family compared to the usual care improved the motor development of children born prematurely; however, when the analysis was performed at different ages, the effect was observed only at 12 months of age. Similar results were observed in the meta-analysis by Spittle et al.,18 although they did not specifically address interventions focused on the family, and by Vanderveen et al.,22 who found a positive effect on the motor outcome only at 12 months.
The interventions analyzed in the present study, which promoted greater benefits in motor development, were those based mainly on the synchronous-active theory. Although most of the programs analyzed are not specifically focused on motor development, the early intervention elements based on the synchronous-active theory help to explain the overall positive effect of an early intervention on the motor outcome in the preterm infant sample.
When the social risk was added to the biological risk, no positive effect of the intervention was observed on motor development and cognition, even when children with high vs. low social risk were compared. It should be noted that the meta-analysis was performed by grouping data from only two studies with moderate methodological quality5,31; therefore, the result should be interpreted with caution. There is evidence that more intensive and long-term programs, such as Early Head Start,41 carried out in the United States with more than 3000 children from low-income families in the first 3 years of life, have a positive impact on cognitive development. It is possible that the number of sessions31 and the intensity5 of the interventions were not sufficient to affect the motor and cognitive development of children with associated social and biological risks.
Regarding the language outcome, it was observed that early intervention compared to usual care was not effective in improving the language of preterm children and/or those at social risk. However, language was evaluated only in four more recent studies, using the Bayley III scale21,31,36 and the MacArthur-Bates Short Form of the CDI.39
The Bayley II scale was applied to the other eight studies, which consists of mental and psychomotor scales, with no isolated score for language. With the availability of specific scales for language evaluation, it is important to include this domain in clinical trials, so it will be possible to analyze the impact of interventions on children's language, contributing to the creation of more efficient programs.
The interventions included in this meta-analysis were heterogeneous regarding their duration, number of sessions and methods used. However, most cases included parental education on how to deal with and stimulate their children in the different areas, based mainly on the synchronous-active theory,20,32–37 performed individually, mainly in the first 12 months of life and during a small number of sessions.20,21,31–37
Wallander et al.42 verified that children from low- and middle-income countries exposed to social and biological risk factors who received higher doses of early intervention involving their parents in the first 3 years of life had better outcomes in cognition and motor development. In the study by Wallander et al.,42 the intervention was based on the Partners for Learning curriculum and consisted of home visits held twice a month until the child was 3 years old (72 sessions). A greater intervention benefit was observed for children who received at least 91% of the scheduled home visits held twice a month. The authors understand the difficulty of implementing long-term programs, especially in low- and middle-income countries. However, efforts to promote more intervention focused on the family programs that are consistent with the reality of these countries may result in greater benefits for children's development in populations exposed to multiple risk factors.
Due to sample heterogeneity and lack of some data, it was not possible to perform a specific meta-analysis of the studies with children exposed only to social risk. Additionally, the few studies found are of moderate methodological quality. Moreover, the scarcity of studies on early intervention focused on the family with high methodological quality also indicates the inherent difficulties of performing this type of research in low- and middle-income countries.
This review has some limitations. Seven different early intervention focused on the family approaches were combined: IBAIP, NIDCAP, VIBeS Plus, the intervention based on the Partners for Learning curriculum, the Mother–Infant Transaction Program – modified version and two studies with interventions based on educational guidelines for parents. Although these interventions have some characteristics in common, each of them addressed specific components of parental involvement.
The combination of data from relatively heterogeneous programs to provide estimates of the overall effect of the intervention may not have disclosed the potential of each approach. However, the scarcity of studies with acceptable methodological quality justifies this choice of analysis until further studies are developed that address standardized interventions with clearly defined characteristics.
Another limitation is that all included clinical trials had moderate methodological quality and risk of bias, especially regarding allocation concealment and masking of the participants and the professional, which is often difficult or impossible to do in this type of intervention. Similarly, in several trials, some children in the control groups were referred for early intervention or physical therapy, an ethical recommendation, but which also included biases that could not be controlled.
ConclusionThe results show that early intervention focused on the family programs have a positive effect on the cognition of preterm infants, especially when the programs are based on the synchronous-active theory. The effects on the motor domain were not as consistent, possibly due to the theoretical reference used in the analyzed interventions. Studies from low- and middle-income countries were poorly represented, making the results poorly conclusive regarding the effects of programs on the development of children at social risk. The same can be said about the effects of interventions on the language domain.
Considering the need for evidence to guide public policies and clinical practice, this meta-analysis showed positive effects of early intervention focused on the family programs on child development, especially on the cognitive abilities of preterm infants and it identified gaps in the literature that need be filled, aiming to better understand the effectiveness of this type of intervention.
FundingThe present study was carried out with the support of Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Brazil – Funding Code 001, Conselho Nacional de Pesquisa (CNPQ), Grand Challenges Canada and Fundação Maria Cecília Souto Vidigal.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Ferreira RC, Alves CR, Guimarães MA, Menezes KK, Magalhães LC. Effects of early interventions focused on the family in the development of children born preterm and/or at social risk: a meta-analysis. J Pediatr (Rio J). 2020;96:20–38.
Study conducted at Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil.