To analyze the factors associated with neonatal mortality related to health services accessibility and use.
MethodsCase–control study of live births in 2008 in small- and medium-sized municipalities in the North, Northeast, and Vale do Jequitinhonha regions, Brazil. A probabilistic sample stratified by region, population size, and information adequacy was generated for the choice of municipalities. Of these, all municipalities with 20,000 inhabitants or less were included in the study (36 municipalities), whereas the remainder were selected according to the probability method proportional to population size, totaling 20 cities with 20,001–50,000 inhabitants and 19 municipalities with 50,001–200,000 inhabitants. All deaths of live births in these cities were included. Controls were randomly sampled, considered as four times the number of cases. The sample size comprised 412 cases and 1772 controls. Hierarchical multiple logistic regression was used for data analysis.
ResultsThe risk factors for neonatal death were socioeconomic class D and E (OR=1.28), history of child death (OR=1.74), high-risk pregnancy (OR=4.03), peregrination in antepartum (OR=1.46), lack of prenatal care (OR=2.81), absence of professional for the monitoring of labor (OR=3.34), excessive time waiting for delivery (OR=1.97), borderline preterm birth (OR=4.09) and malformation (OR=13.66).
ConclusionThese results suggest multiple causes of neonatal mortality, as well as the need to improve access to good quality maternal-child health care services in the assessed places of study.
Analisar fatores associados à mortalidade neonatal referentes ao acesso e à utilização dos serviços de saúde.
MétodosEstudo caso-controle de nascidos vivos em 2008 nos municípios de pequeno e médio porte nas regiões Norte, Nordeste e Vale do Jequitinhonha do Brasil. Uma amostra probabilística e estratificada por região, tamanho da população e adequação da informação foi gerada para escolha das cidades. Foram selecionados municípios com até 200.000 habitantes. Desses, todos os municípios com até 20.000 habitantes foram incluídos no estudo (36 municípios), os demais foram selecionados de acordo com o método de probabilidade proporcional ao tamanho populacional, totalizando 20 cidades com 20.001 a 50.000 habitantes e 19 municípios com 50.001 a 200.000 habitantes. Foram incluídos todos os óbitos de nascidos vivos nessas cidades, nesse período. Os controles foram amostrados aleatoriamente quatro vezes mais o número de casos. A amostra foi de 412 casos e 1772 controles. Foi utilizada regressão logística múltipla hierarquizada para análise dos dados.
ResultadosOs fatores de risco para o óbito neonatal foram classe socioeconômica D e E (OR=1,28), história de óbito infantil (OR=1,74), gestação de risco (OR=4,03), peregrinação para o parto (OR=1,46), não realização de pré-natal (OR=2,81), ausência de profissional para o acompanhamento do trabalho de parto (OR=3,34), tempo de espera para o atendimento ao parto (OR=1,97), malformação (OR=13,66) e prematuridade moderada/limítrofe (OR=4,09).
ConclusãoTais resultados sugerem a multicausalidade da mortalidade neonatal e apontam para necessidade de melhoria ao acesso de serviços voltados à atenção materno-infantil, de qualidade, nos locais do estudo.
The infant mortality coefficient, which is most impacted by the neonatal component, is considered a sensitive indicator to quality of life, development level, and access to health services of a given population.1
Despite the decrease in neonatal mortality, in the last decade Brazil has shown a disparity of this indicator in the different regions of the country. In 2014, both neonatal mortality rates (NMR) in the North and Northeast regions were 10.3/1000 live births (LB), whereas in the South region it was 7.6/1000 LB, in the Southeast 8.1/1000 LB, and in Brazil 8.9/1000 LB, showing the socioeconomic disparities between the different regions of the country, in which only the North and Northeast regions persist with two digits to the left of the decimal point, according to the most recent available data.2 Only in 2014, the North and Northeast regions had NMR compatible with that of the Southeast region in 2005 (10.2/1000NV), but still higher than the coefficient of the South, which in 2005 was 9.4/1000 LB.2
In addition to showing the highest neonatal mortality rates in the country, the North, Northeast, and Vale do Jequitinhonha regions have an excess of underreporting in national health systems. It was identified that 30% of municipalities had less than 80% coverage from the Mortality Information System (Sistema de Informação da Mortalidade [SIM]), most of them located in the Northeast and North regions of the country. The smaller municipalities, those with up to 200,000 inhabitants, showed worse-quality information on vital data.3 The small and medium-sized municipalities of the North, Northeast, and Vale do Jequitinhonha regions have different characteristics when compared to the larger cities located in these same regions.
In most cases, the smaller municipalities show worse socioeconomic conditions and, mainly, difficulty in access to health care services, which contributes to infant mortality. Thus, the present study aimed to analyze the association of neonatal mortality with variables of health service access and use in the North, Northeast, and Vale do Jequitinhonha regions, in 2008.
It has as a differential feature the analysis of data obtained from populations of smaller Brazilian municipalities, which are hard to study with high statistical power, due to their reduced population sizes. It has an assured representativeness, since it is not based only on the official statistics, which are hindered by underreporting.
MethodsThis is a case–control study with a live-birth population from the year 2008, born to mothers residing in the North, Northeast, and Vale do Jequitinhonha regions.
Based on an evaluation of the coverage of the Information System on Live Births and Mortality (Sistema de Informação sobre Mortalidade e Sistema de Nascidos Vivos [SINASC]) between 2007 and 2009 in the municipalities belonging to the Amazônia Legal and the Northeast regions, Andrade and Szwarcwald4 chose the criteria for the classification of municipalities with up to 200,000 inhabitants of the aforementioned regions according with the adequacy of the information system. Municipalities with up to 200,000 inhabitants were categorized based on the assessment of indicators related to vital statistics (mortality and birth). This evaluation classified these indicators as “satisfactory,” “unsatisfactory,” and “deficient” in each municipality and from that point onwards, the following categorization was attained: “Consolidated vital information” (all indicators classified as adequate), “Vital information undergoing consolidation (at least one indicator that is not satisfactory, but none deficient), and “Unconsolidated vital information” (at least one indicator classified as deficient). The random sampling system selected municipalities from each state, ensuring the representativeness of these different categorizations.
Thus, a probabilistic and stratified sample by region, population size, and adequacy of information was generated for municipality selection. All municipalities with up to 20,000 inhabitants were included in the study (36 municipalities); the other municipalities were selected according to the probability method proportional to the population size, totaling 20 cities with 20,001 up to 50,000 inhabitants and 19 municipalities with 50,001 up to 200,000 inhabitants.
All live births that died within 27 days after birth from January 1 to December 31, 2008, whose mothers lived in these chosen municipalities, were considered cases. The controls were children aged less than 1-year, born in 2008 in the same place of the cases, randomly chosen from the complete lists of live births of each sampled municipality, together with all live births found that were not registered in any information system.
Cases and controls were selected from SIM, SINASC, and by active search in different places, such as notary offices, cemeteries, and traditional midwives, among others. Between 2010 and 2011, trained and supervised interviewers, guided by a previously structured script, collected data at home through interviews with those responsible for the selected children, constituting the data source. This study selected 1951 controls and 530 cases (3.6 controls per case). After the removal of the individuals with loss of information in some variables of interest, there were 1772 controls and 412 cases.
The variables of interest were those that could somehow influence the access and use of health services. After these variables were listed, a descriptive analysis was performed, excluding those with 10% or more of absence of information (prenatal site, locomotion to the prenatal site, time until reaching the prenatal unit, prenatal examinations, weighing, blood pressure measurement, uterine height measurement, auscultation of the fetal heartbeat, previous guidance in the maternity for the delivery, moment of rupture of the amniotic sac, Apgar score, and birth weight).
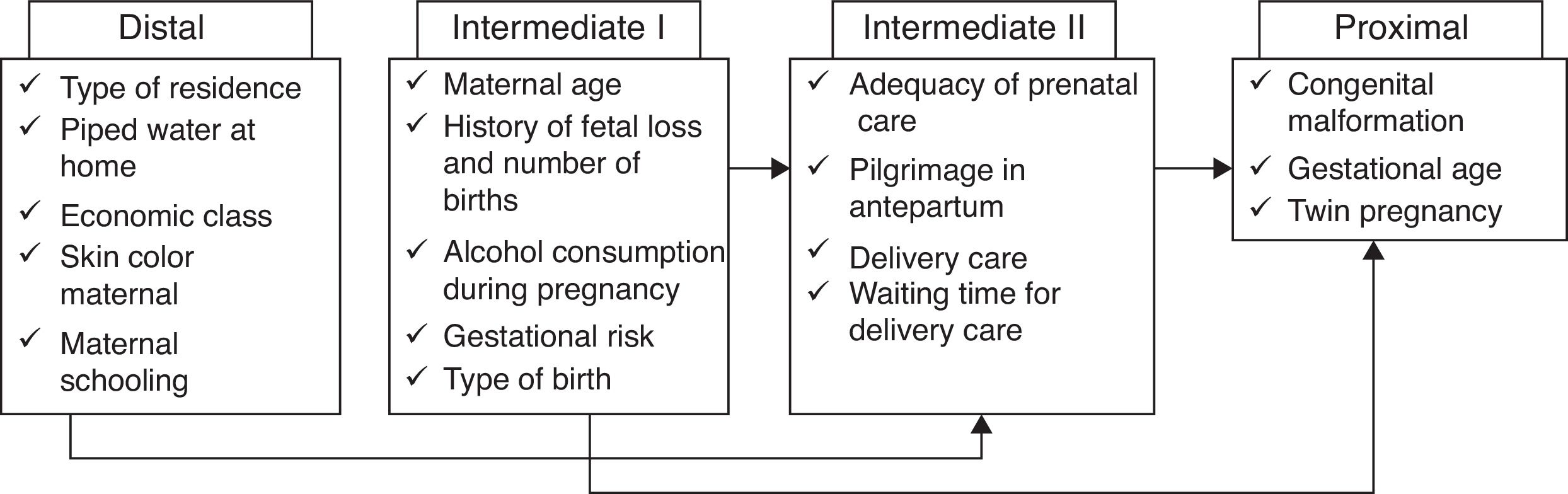
Subsequently, a bivariate logistic regression analysis was performed and variables that showed p-value≥20% were excluded: basic sanitation, baby's gender, and smoking during pregnancy. Conversely, the variables that showed p-value<20% were organized in a hierarchical theoretical model (Fig. 1) according to the adapted proposal by Lima, Carvalho, and Vasconcelos.5 In the hierarchical logistic regression, the proposal of Victora6 was used, according to which the variables are introduced by level of proximity to the outcome, starting with those at the distal level. To maintain the variables at each hierarchical level, the p-value criterion was defined as less than 5%. Variables of a certain level that lost significance with the inclusion of variables from the next level remained in the model.
Variables inserted at each level during the hierarchical modeling for neonatal death. Adapted from Lima et al.5
The models of each level were compared by the Akaike information criterion (AIC). The software programs SPSS (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0, NY, USA) and R version 3.3.0 were used for statistical analysis of the data.
Neonatal mortality was considered in case of death of live births between 0 and 27 days of life, subdivided into early neonatal, when the death occurs until the sixth day of life and late neonatal, when the death occurs from the seventh day of life onwards. To guarantee the independence of the events, only the first twin was selected and the others were excluded.
The Brazilian Association of Market Research Institutes (Associação Brasileira de Institutos de Pesquisa de Mercado [ABIPEME]) score is a proxy of the measured socioeconomic level based on family consumption, considering the best socioeconomic level as “A” and worst, as “E.”
Gestational risk was defined when the mother had at least one of these morbidities: HIV seropositivity and/or syphilis, Rh negative, chronic arterial disease, threatened preterm birth, seizure, obstetric hospitalization, use of medication for hypertension, or use of medication for diabetes.
The classification of prematurity was defined according to Marcondes, Vaz, and Ramos,7 being considered extreme with less than 31 weeks of gestational age, moderate between 31 and 34 weeks, borderline from 35 to 36 weeks, and full-term from 37 weeks onward. Moderate and borderline prematurity were aggregated to avoid categories with small numbers.
The Kotelchuck8 criterion was used for prenatal adequacy, which is considered adequate when the pregnant woman has at least 80% of the expected consultations in relation to the gestational age of prenatal care onset and the child's birth. The Kotelchuck criterion was adapted considering the number of consultations expected by the Brazilian Ministry of Health (six consultations). Pilgrimage in antepartum until reaching a hospital facility was considered when the pregnant woman sought more than one health unit before the child was born.
The present study was submitted and approved in October 2013 by the Research Ethics Committee of the ENSP (Escola Nacional de Saúde Pública Sérgio Arouca), with a consolidated opinion, number 434,401.
ResultsThe population of the current study consisted of 412 cases and 1772 controls. Considering only the early neonatal period, there were 319 deaths, or more than two-thirds of all deaths.
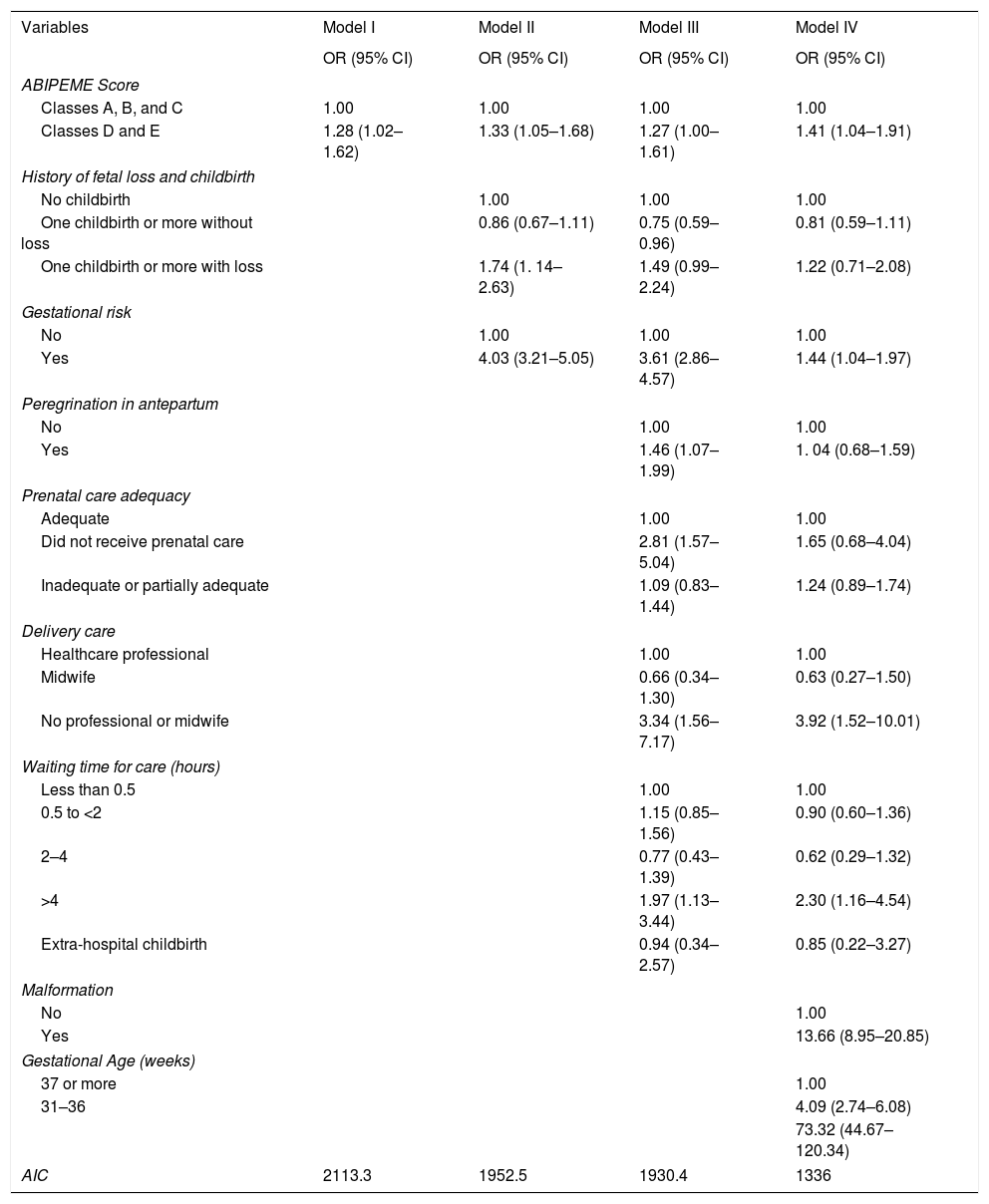
As shown in Fig. 1, the five variables at the distal level were initially introduced simultaneously and only the ABIPEME score showed a p-value<5%, remaining in the hierarchical logistic regression. Subsequently, the variables were included in the intermediate level I, with only history of gestational loss and gestational risk remaining (p-value<5%). After that, the variables in the next levels were included one at a time, and the same procedure was adopted, with the variables shown in Table 1 remaining in the model.
Factors associated with neonatal death by hierarchical logistic regression. North, Northeast, and Vale do Jequitinhonha, Brazil, 2008. (Cases=412, Controls=1772).
| Variables | Model I | Model II | Model III | Model IV |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| ABIPEME Score | ||||
| Classes A, B, and C | 1.00 | 1.00 | 1.00 | 1.00 |
| Classes D and E | 1.28 (1.02–1.62) | 1.33 (1.05–1.68) | 1.27 (1.00–1.61) | 1.41 (1.04–1.91) |
| History of fetal loss and childbirth | ||||
| No childbirth | 1.00 | 1.00 | 1.00 | |
| One childbirth or more without loss | 0.86 (0.67–1.11) | 0.75 (0.59–0.96) | 0.81 (0.59–1.11) | |
| One childbirth or more with loss | 1.74 (1. 14–2.63) | 1.49 (0.99–2.24) | 1.22 (0.71–2.08) | |
| Gestational risk | ||||
| No | 1.00 | 1.00 | 1.00 | |
| Yes | 4.03 (3.21–5.05) | 3.61 (2.86–4.57) | 1.44 (1.04–1.97) | |
| Peregrination in antepartum | ||||
| No | 1.00 | 1.00 | ||
| Yes | 1.46 (1.07–1.99) | 1. 04 (0.68–1.59) | ||
| Prenatal care adequacy | ||||
| Adequate | 1.00 | 1.00 | ||
| Did not receive prenatal care | 2.81 (1.57–5.04) | 1.65 (0.68–4.04) | ||
| Inadequate or partially adequate | 1.09 (0.83–1.44) | 1.24 (0.89–1.74) | ||
| Delivery care | ||||
| Healthcare professional | 1.00 | 1.00 | ||
| Midwife | 0.66 (0.34–1.30) | 0.63 (0.27–1.50) | ||
| No professional or midwife | 3.34 (1.56–7.17) | 3.92 (1.52–10.01) | ||
| Waiting time for care (hours) | ||||
| Less than 0.5 | 1.00 | 1.00 | ||
| 0.5 to <2 | 1.15 (0.85–1.56) | 0.90 (0.60–1.36) | ||
| 2–4 | 0.77 (0.43–1.39) | 0.62 (0.29–1.32) | ||
| >4 | 1.97 (1.13–3.44) | 2.30 (1.16–4.54) | ||
| Extra-hospital childbirth | 0.94 (0.34–2.57) | 0.85 (0.22–3.27) | ||
| Malformation | ||||
| No | 1.00 | |||
| Yes | 13.66 (8.95–20.85) | |||
| Gestational Age (weeks) | ||||
| 37 or more | 1.00 | |||
| 31–36 | 4.09 (2.74–6.08) | |||
| 73.32 (44.67–120.34) | ||||
| AIC | 2113.3 | 1952.5 | 1930.4 | 1336 |
ABIPEME, Brazilian Association of Market Research Institutes (Associação Brasileira de Institutos de Pesquisa de Mercado); AIC, Akaike information criterion.
The socioeconomic level was important for neonatal death in all models.
The risk of death in newborns was higher when the mother had a history of previous fetal loss, which lost its significance with the introduction of variables of the next level. High-risk pregnancy showed a greater chance of neonatal death, even when adjusted for all other variables.
In model III, pilgrimage in antepartum while seeking for health services before delivery indicated an increased risk of death, as did the adequacy of prenatal care. The absence of prenatal care appears as a risk factor for neonatal death, and its effect probably becomes indirect in model IV. The absence of a health professional in childbirth care has a direct effect even in model IV, increasing the risk of death by almost four-fold. Babies born to mothers who waited more than four hours for pre-delivery care had more than double the risk of death compared to mothers who waited less than half an hour (model IV).
Congenital malformation showed a strong association with the outcome. Prematurity showed a great increase in the risk of neonatal death, 4-fold higher among moderate and borderline preterm infants when compared to full-term infants, and 73-fold higher among extremely preterm infants, despite its imprecision due to the wide range of the confidence interval.
When using the Akaike criterion, it is observed that the inclusion of the variables at each level of the model improves the adjustment, with model IV being the most complete explanation of neonatal death in this population.
DiscussionThe great advantage of the hierarchical analysis is to allow the analysis of the influence of the distal variables, stressing their importance and strength of association even with the inclusion of variables from other levels, which are more proximal and usually are strongly associated with the outcome. Additionally, it is possible to observe the effect of each variable along the different levels of hierarchy in the theoretical model.
Socioeconomic level, an important marker of life conditions, was part of the model of neonatal death explanation. Other studies also found an association between neonatal death and socioeconomic variables.9–11
A national survey from 2000 to 2007 found that the geographical access to the maternity hospital had a significant association with income and, even when controlled for other variables, it showed an influence on infant mortality.12
Maternal age and maternal skin color did not remain in the hierarchical multiple logistic regression, unlike the results of some previous studies.10,13 These same variables did not show statistical significance in the study of a national cohort.14
Maternal schooling did not appear as a variable associated with infant death; in contrast, another study found an association between this variable and neonatal death.14 The baby's gender did not show any association with neonatal death, even in the bivariate analysis, in contrast to two studies that found male gender as a risk factor for death in newborns.13,14
In the current study, the hierarchical analysis identified pilgrimage in antepartum as a variable associated with neonatal mortality, consistent with a national cohort of live births.14
Maternal history of previous losses and inadequate prenatal care were considered risk factors in the current study, in agreement with other studies.13–15 The variable prenatal adequacy was associated with neonatal death in a study, showing a gradient, and the category “Inadequate” had greater risk.14 Other studies showed the lack of and inadequacy of prenatal care as risk factors for neonatal and early neonatal mortality.13,16
The variable waiting time longer than four hours for delivery appeared as a risk factor for neonatal death, even after inclusion of variables at the proximal level; such evidence points to the importance of having access to a timely delivery. Lansky et al.14 consider the parturient woman an emergency case and thus, she must receive immediate care at the health service.
Similarly, when the delivery was not accompanied by a health professional or midwife, there was an increase in the risk of neonatal death, including in model IV, demonstrating the importance for the parturient woman to have access to the health professional who will monitor the labor.
The variables most often associated with neonatal death were congenital malformation and prematurity. These malformations are more likely to be the most severe types, considering the risk of mortality. A Brazilian cohort showed a greater risk of neonatal death among those newborns with congenital malformation.14 Another cohort identified prematurity as the main cause of neonatal death.17
It is noteworthy that even moderate and borderline preterm infants, who mostly have a good chance of survival when treated by trained professionals, showed an almost four-fold higher risk of death when compared to those born at term. The chance of survival of a preterm infant is associated with the place of birth and with the quality of care provided.18 High-income countries have increased the chances of extremely preterm infants’ survival, while low-income ones have difficulty increasing the chance of survival of moderately preterm infants.18 Investments in prenatal care and delivery improve the outcome of preterm infants.18 The neonatal death profile caused mainly by prematurity, found in the current study, follows the tendency of high- and middle-income countries. Prematurity has been the leading cause of neonatal death worldwide.18
Lansky et al.14 warn that 23% of the deaths in their study were avoidable, mainly caused by asphyxiation and borderline prematurity, which points to the need not only for improved access to care, but also for good-quality care, which can prevent asphyxiation during birth and assist newborns with borderline prematurity, who are mostly viable.
Considering studies selected for comparison with the current one, which are mostly studies carried out in capitals or larger municipalities, many similarities were found, since social inequality impairs access to health care services, regardless of the location. However, it should be emphasized that even in similar situations of poverty, the context can make access to health care services even more difficult, when one considers, for instance, the geography where the riverine populations live in the North region, as well as the difficulty of allocating doctors in the North and Northeast regions. Such situations can influence the increase in magnitude of the odds ratios in the current study when compared to others, as demonstrated in prematurity. The study is different from others because it points out the absence of the health professional in childbirth care as a factor associated with neonatal mortality, demonstrating the poor-quality health services offered to the populations of the assessed municipalities.
Some limitations need to be considered in the present study, such as the possibility of memory bias, since the data were collected two to three years after the outcome, and some information could be better remembered by the cases, generating a differential bias. Additionally, there was greater loss of information among cases when compared to their controls, possibly causing distortions in the measurement of odds ratios, with no trend prediction. This loss also occurred because data collection was performed at least two years after the birth or death; in case of lack of controls, it was still possible to replace them. However, this could not be applied to the cases that were not retrieved; although they were accounted for, not much information was available. In spite of the excluded individuals due to missing data, no contradictory results were found considering the current scientific evidence.
Another limitation of this study is that the data are not recent; however, the inequality situation between the regions of Brazil remains a current issue, as demonstrated by the recent neonatal mortality coefficients. Moreover, the smaller municipalities, located in the countryside of the states, mainly in the North and Northeast regions, continue to show difficulties in the organization of health services, in the hiring of professionals, mainly physicians, and in the provision of more complex services.
The results found herein confirm that the factors that affect or represent access to and the use of health services are still determinant for neonatal death, at least in the assessed regions.
It is necessary to achieve the basic aspects of health care, such as adequate and good-quality prenatal care, guaranteed access to a maternity hospital before delivery, timely care of the parturient woman, and guaranteed professional care for the mother and the baby at the time of delivery.
Public health policy in Brazil needs to guarantee investments in the organization of health services and in the improvement and development of the health care structures and professionals in these services, including the increase in the number of beds in the intensive care units and neonatal intensive care units for appropriate care of preterm infants who are born in the smaller municipalities, considering the significant risk of death for borderline and moderate preterm infants, probably due to the inadequacy of the attention provided to the required care. It is important to study, design, and implement health care networks in regions that encompass small and medium-sized municipalities regarding the basic health needs at birth.
The marked risk factors for this study were prematurity and malformation. These aspects demonstrate that Brazil has a neonatal death profile similar to that of developed countries, but in addition, it raises the need for detailed studies to better understand deaths in premature infants and those with malformation who were, however, viable.
Public policies that facilitate access to good-quality services in the smaller municipalities of the North, Northeast, and Vale do Jequitinhonha regions and that can improve the quality of care to premature infants need to be encouraged and implemented, so that Brazil may reach the neonatal mortality coefficients found in the higher-income countries.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Batista CB, de Carvalho ML, Vasconcelos AG. Access to and use of health services as factors associated with neonatal mortality in the North, Northeast, and Vale do Jequitinhonha regions, Brazil. J Pediatr (Rio J). 2018;94:293–9.
The current study was performed in partnership with the maternal-child area team of Escola Nacional de Saúde Pública Sergio Arouca (ENSP), Fundação Oswaldo Cruz (Fiocruz), Rio de Janeiro, RJ, Brazil.