To study the evidence on the role of water and fluid intake in the prevention and treatment of functional intestinal constipation in children and adolescents.
Source of dataA search was carried out in the Medline database (between 1966 and 2016) for all published articles containing the following words: constipation, water, and fluids, published in Portuguese, English, and Spanish. All original articles that assessed children and adolescents were selected by title and abstract. The references of these articles were also evaluated.
Synthesis of dataA total of 1040 articles were retrieved. Of these, 24 were selected for reading. The study included 11 articles that assessed children and adolescents. The articles were divided into two categories, those that evaluated water and fluid intake as a risk factor for intestinal constipation and those that evaluated their role in the treatment of intestinal constipation. Five articles were included in the first category. The criteria for assessing fluid intake and bowel rhythm were different in each study. Three studies demonstrated an association between low fluid intake and intestinal constipation. Regarding treatment, five articles with heterogeneous methodologies were found. None of them clearly identified the favorable role of fluid intake in the treatment of intestinal constipation.
ConclusionThere are few articles on the association between fluid intake and intestinal constipation. Epidemiological evidence indicates an association between lower fluid intake and intestinal constipation. Further clinical trials and epidemiological studies that consider the international recommendations for fluid intake by children and adolescents are required.
Estudar as evidências sobre o papel do consumo de água e líquidos na prevenção e no tratamento da constipação intestinal funcional em crianças e adolescentes.
Fontes de dadosFoi pesquisado na base de dados do Medline (entre 1966 e 2016) todos os artigos publicados com as seguintes palavras: constipação, água e líquidos, nos idiomas português, inglês e espanhol. Foram selecionados, pelo título e resumo, todos os artigos originais com crianças e adolescentes. As referências desses artigos também foram avaliadas.
Síntese de dadosForam encontrados 1040 artigos. Desses, 24 foram selecionados para leitura. Foram incluídos 11 artigos que estudaram crianças e adolescentes. Os artigos foram distribuídos em duas categorias, os que avaliaram o consumo de água e líquidos como fator de risco para constipação intestinal e os que avaliaram o seu papel na terapêutica da constipação intestinal. Cinco artigos se enquadraram na primeira categoria. Os critérios para avaliar consumo de líquidos e ritmo intestinal foram diferentes em cada estudo. Três estudos demonstraram relação entre baixo consumo de líquidos e constipação intestinal. Quanto ao tratamento, foram encontrados cinco artigos com metodologias heterogêneas. Em nenhum deles foi possível identificar com clareza o papel favorável do consumo de líquidos no tratamento da constipação intestinal.
ConclusãoExistem poucos artigos sobre a relação entre consumo de líquidos e constipação intestinal. Evidências epidemiológicas indicam associação entre menor consumo de líquidos com constipação intestinal. São necessários outros ensaios clínicos e estudos epidemiológicos que levem em consideração as recomendações internacionais para consumo de líquidos por crianças e adolescentes.
Intestinal constipation is a common clinical manifestation in the pediatric population, and over 90% of cases are classified as functional gastrointestinal disorders.1–3 As observed in other functional gastrointestinal disorders, childhood intestinal constipation results from the interaction of biological, dietary, and psychosocial factors that interfere with intestinal motility.4 The main factors related to diet are water and dietary fiber consumption.3–6
According to the guidelines, functional intestinal constipation treatment includes fecaloma clearing and maintenance therapy using laxatives to avoid fecal re-impaction, toilet training, and guidelines for increasing fiber and water intake.4,7–9 However, the guidelines of the European Society for Pediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN)/North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN), published in 2014, questions the efficacy of increased water intake in intestinal constipation therapy and suggests that, according to the evidence, an increase in fluid intake for the treatment of functional intestinal constipation should not be recommended.10 When analyzing the evidence supporting this position, it can be verified that this was based on only one clinical trial, published in 1998.11
Considering that increased water intake is part of the treatment of functional intestinal constipation in other guidelines7–9 and in clinical practice, this recent positioning motivated the development of the present study, which aimed to assess the evidence on the role of water and fluid intake in the prevention and treatment of functional intestinal constipation in children and adolescents.
MethodologyThe Medline database was used for the search. The period evaluated was January 1966 to November 2016. Research was carried out on articles that analyzed the role of water and/or fluid intake in the treatment and prevention of intestinal constipation in children and adolescents. As for the strategy, a broad search was made using the following pairs of words: “constipation” and “water”; “constipação” and “água”; “estreñimiento” and “agua”; “constipation” and “fluid”; “constipação” and “líquidos”; “estreñimiento” and “neto”, in English, Portuguese and Spanish. All original articles that included children and adolescents were selected by reading the title and abstracts. The search was not restricted to the exclusive evaluation of controlled and randomized clinical trials. No review articles, editorials, and comments were included in this selection.
Moreover, the reference list of the selected articles was assessed to obtain other non-indexed articles. The selected articles were analyzed by two authors for the final data extraction.
ResultsAt the beginning of the search, 1040 articles were retrieved. All articles that assessed the association between constipation and water intake or that used fluids as part of the therapy were selected. Thus, 26 articles11–36 were selected for reading. Of these, only the 11 articles11,22,24–30,32,36 that addressed children and adolescents were included in this review. After analysis, the articles were divided into two categories: those that assessed water and fluid intake as a possible risk factor for intestinal constipation and those that assessed their role in intestinal constipation treatment.
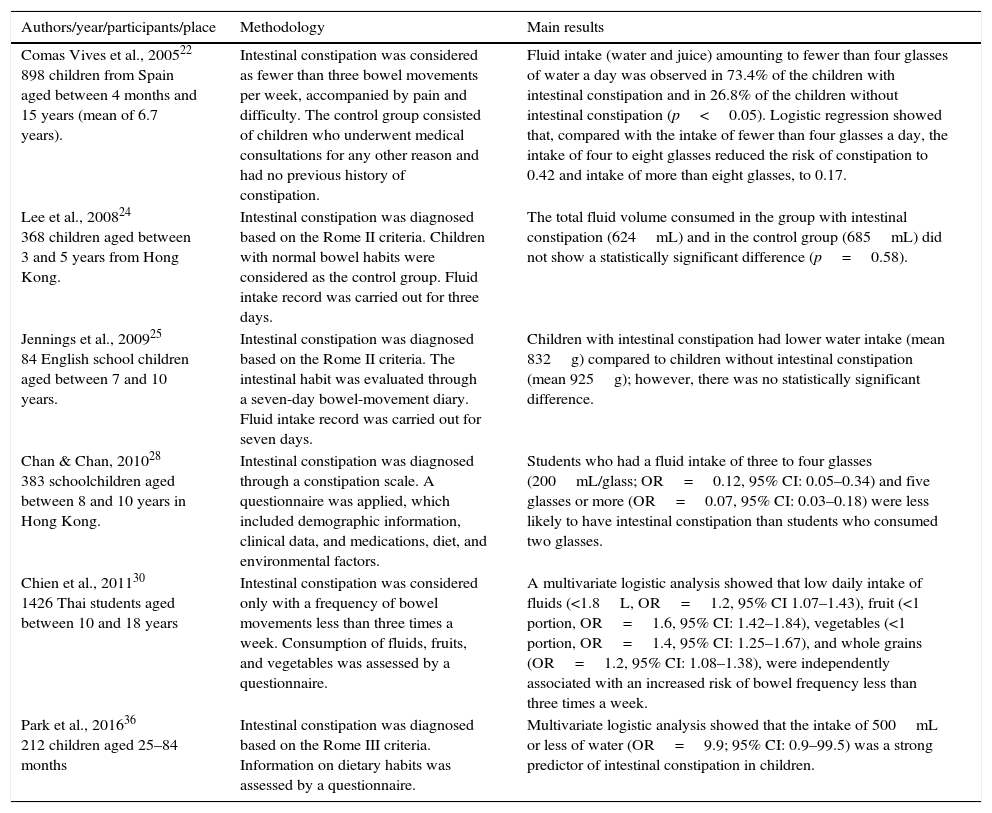
Of the retrieved articles, six evaluated water and/or fluid intake as a possible risk factor for intestinal constipation.22,24,25,28,30,36 These studies were carried out in Spain,22 Hong Kong,24,28 United Kingdom,25 Thailand,30 and Korea.36 The studied samples ranged from 84 to 1426 individuals. The criteria used to evaluate fluid intake and intestinal rhythm were different in each study. The main results are shown in Table 1. Four articles showed an association between low fluid intake and intestinal constipation.22,28,30,36 The other two studies found lower fluid intake in children with intestinal constipation; however, the difference was not statistically significant.24,25
Characteristics of studies in children that evaluated water or fluid intake as a risk factor for intestinal constipation.
| Authors/year/participants/place | Methodology | Main results |
|---|---|---|
| Comas Vives et al., 200522 898 children from Spain aged between 4 months and 15 years (mean of 6.7 years). | Intestinal constipation was considered as fewer than three bowel movements per week, accompanied by pain and difficulty. The control group consisted of children who underwent medical consultations for any other reason and had no previous history of constipation. | Fluid intake (water and juice) amounting to fewer than four glasses of water a day was observed in 73.4% of the children with intestinal constipation and in 26.8% of the children without intestinal constipation (p<0.05). Logistic regression showed that, compared with the intake of fewer than four glasses a day, the intake of four to eight glasses reduced the risk of constipation to 0.42 and intake of more than eight glasses, to 0.17. |
| Lee et al., 200824 368 children aged between 3 and 5 years from Hong Kong. | Intestinal constipation was diagnosed based on the Rome II criteria. Children with normal bowel habits were considered as the control group. Fluid intake record was carried out for three days. | The total fluid volume consumed in the group with intestinal constipation (624mL) and in the control group (685mL) did not show a statistically significant difference (p=0.58). |
| Jennings et al., 200925 84 English school children aged between 7 and 10 years. | Intestinal constipation was diagnosed based on the Rome II criteria. The intestinal habit was evaluated through a seven-day bowel-movement diary. Fluid intake record was carried out for seven days. | Children with intestinal constipation had lower water intake (mean 832g) compared to children without intestinal constipation (mean 925g); however, there was no statistically significant difference. |
| Chan & Chan, 201028 383 schoolchildren aged between 8 and 10 years in Hong Kong. | Intestinal constipation was diagnosed through a constipation scale. A questionnaire was applied, which included demographic information, clinical data, and medications, diet, and environmental factors. | Students who had a fluid intake of three to four glasses (200mL/glass; OR=0.12, 95% CI: 0.05–0.34) and five glasses or more (OR=0.07, 95% CI: 0.03–0.18) were less likely to have intestinal constipation than students who consumed two glasses. |
| Chien et al., 201130 1426 Thai students aged between 10 and 18 years | Intestinal constipation was considered only with a frequency of bowel movements less than three times a week. Consumption of fluids, fruits, and vegetables was assessed by a questionnaire. | A multivariate logistic analysis showed that low daily intake of fluids (<1.8L, OR=1.2, 95% CI 1.07–1.43), fruit (<1 portion, OR=1.6, 95% CI: 1.42–1.84), vegetables (<1 portion, OR=1.4, 95% CI: 1.25–1.67), and whole grains (OR=1.2, 95% CI: 1.08–1.38), were independently associated with an increased risk of bowel frequency less than three times a week. |
| Park et al., 201636 212 children aged 25–84 months | Intestinal constipation was diagnosed based on the Rome III criteria. Information on dietary habits was assessed by a questionnaire. | Multivariate logistic analysis showed that the intake of 500mL or less of water (OR=9.9; 95% CI: 0.9–99.5) was a strong predictor of intestinal constipation in children. |
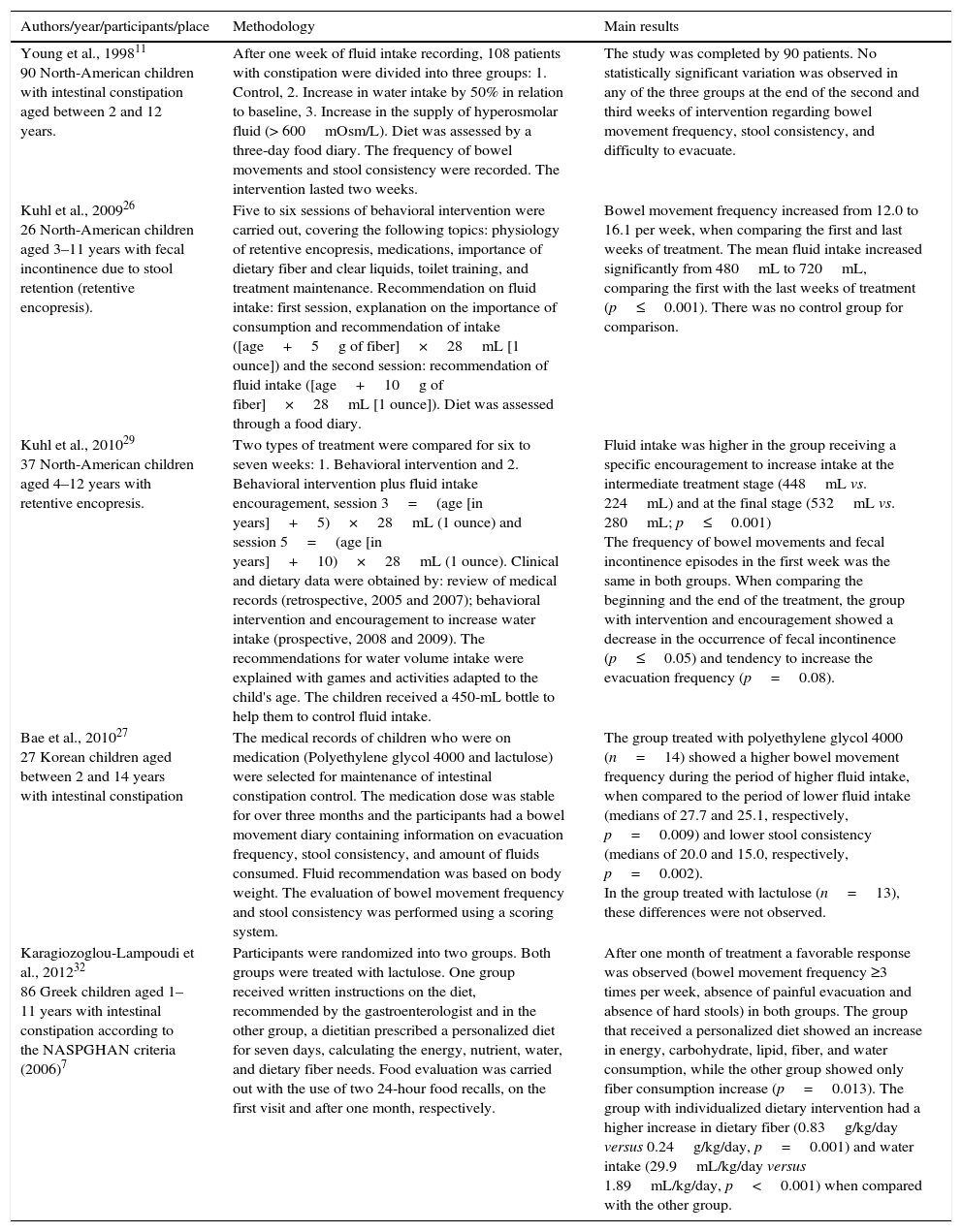
Fluid intake as treatment of intestinal constipation was assessed in five articles,11,26,27,29,32 with heterogeneous methodologies. The studies were conducted in the United States,11,26,29 Korea,27 and Greece.32 Of these, only one found a positive effect of higher fluid intake in the treatment of intestinal constipation; the positive effect was observed when the treatment included polyethylene glycol 4000.27 Two articles assessed the increase in fluid consumption after a behavioral intervention with29 and without26 fluid intake encouragement in children with retentive encopresis (fecal incontinence caused by retention). An increase in fluid intake was observed in both studies. Moreover, there was also an increase in evacuation frequency26 and a decrease in the occurrence of fecal incontinence.29 In the other articles, there was no statistically significant effect of increased fluid intake on the treatment of intestinal constipation (Table 2).11,32
Characteristics of the studies in children that evaluated the role of water intake in the treatment of intestinal constipation.
| Authors/year/participants/place | Methodology | Main results |
|---|---|---|
| Young et al., 199811 90 North-American children with intestinal constipation aged between 2 and 12 years. | After one week of fluid intake recording, 108 patients with constipation were divided into three groups: 1. Control, 2. Increase in water intake by 50% in relation to baseline, 3. Increase in the supply of hyperosmolar fluid (> 600mOsm/L). Diet was assessed by a three-day food diary. The frequency of bowel movements and stool consistency were recorded. The intervention lasted two weeks. | The study was completed by 90 patients. No statistically significant variation was observed in any of the three groups at the end of the second and third weeks of intervention regarding bowel movement frequency, stool consistency, and difficulty to evacuate. |
| Kuhl et al., 200926 26 North-American children aged 3–11 years with fecal incontinence due to stool retention (retentive encopresis). | Five to six sessions of behavioral intervention were carried out, covering the following topics: physiology of retentive encopresis, medications, importance of dietary fiber and clear liquids, toilet training, and treatment maintenance. Recommendation on fluid intake: first session, explanation on the importance of consumption and recommendation of intake ([age+5g of fiber]×28mL [1 ounce]) and the second session: recommendation of fluid intake ([age+10g of fiber]×28mL [1 ounce]). Diet was assessed through a food diary. | Bowel movement frequency increased from 12.0 to 16.1 per week, when comparing the first and last weeks of treatment. The mean fluid intake increased significantly from 480mL to 720mL, comparing the first with the last weeks of treatment (p≤0.001). There was no control group for comparison. |
| Kuhl et al., 201029 37 North-American children aged 4–12 years with retentive encopresis. | Two types of treatment were compared for six to seven weeks: 1. Behavioral intervention and 2. Behavioral intervention plus fluid intake encouragement, session 3=(age [in years]+5)×28mL (1 ounce) and session 5=(age [in years]+10)×28mL (1 ounce). Clinical and dietary data were obtained by: review of medical records (retrospective, 2005 and 2007); behavioral intervention and encouragement to increase water intake (prospective, 2008 and 2009). The recommendations for water volume intake were explained with games and activities adapted to the child's age. The children received a 450-mL bottle to help them to control fluid intake. | Fluid intake was higher in the group receiving a specific encouragement to increase intake at the intermediate treatment stage (448mL vs. 224mL) and at the final stage (532mL vs. 280mL; p≤0.001) The frequency of bowel movements and fecal incontinence episodes in the first week was the same in both groups. When comparing the beginning and the end of the treatment, the group with intervention and encouragement showed a decrease in the occurrence of fecal incontinence (p≤0.05) and tendency to increase the evacuation frequency (p=0.08). |
| Bae et al., 201027 27 Korean children aged between 2 and 14 years with intestinal constipation | The medical records of children who were on medication (Polyethylene glycol 4000 and lactulose) were selected for maintenance of intestinal constipation control. The medication dose was stable for over three months and the participants had a bowel movement diary containing information on evacuation frequency, stool consistency, and amount of fluids consumed. Fluid recommendation was based on body weight. The evaluation of bowel movement frequency and stool consistency was performed using a scoring system. | The group treated with polyethylene glycol 4000 (n=14) showed a higher bowel movement frequency during the period of higher fluid intake, when compared to the period of lower fluid intake (medians of 27.7 and 25.1, respectively, p=0.009) and lower stool consistency (medians of 20.0 and 15.0, respectively, p=0.002). In the group treated with lactulose (n=13), these differences were not observed. |
| Karagiozoglou-Lampoudi et al., 201232 86 Greek children aged 1–11 years with intestinal constipation according to the NASPGHAN criteria (2006)7 | Participants were randomized into two groups. Both groups were treated with lactulose. One group received written instructions on the diet, recommended by the gastroenterologist and in the other group, a dietitian prescribed a personalized diet for seven days, calculating the energy, nutrient, water, and dietary fiber needs. Food evaluation was carried out with the use of two 24-hour food recalls, on the first visit and after one month, respectively. | After one month of treatment a favorable response was observed (bowel movement frequency ≥3 times per week, absence of painful evacuation and absence of hard stools) in both groups. The group that received a personalized diet showed an increase in energy, carbohydrate, lipid, fiber, and water consumption, while the other group showed only fiber consumption increase (p=0.013). The group with individualized dietary intervention had a higher increase in dietary fiber (0.83g/kg/day versus 0.24g/kg/day, p=0.001) and water intake (29.9mL/kg/day versus 1.89mL/kg/day, p<0.001) when compared with the other group. |
NASPGHAN, North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition.
This review showed that few studies evaluated low fluid intake as a factor associated with intestinal constipation or the role of fluid intake in the treatment of constipation. Of the eleven articles retrieved, six22,24,25,28,30,36 analyzed the association between water and fluid intake and intestinal constipation and five, their role in the treatment of intestinal constipation.11,26,27,29,32
The association between intestinal constipation and lower fluid intake in samples from the general population indicate the possibility of a causal association between the two variables. Thus, in four22,28,30,36 of the six22,24,25,28,30,36 articles, a statistically significant association was found between low fluid intake and evidence of intestinal constipation. In the other two articles,24,25 fluid intake by children with intestinal constipation was lower; however, the difference was not statistically significant. These articles are heterogeneous and difficult to compare due to how the variables were quantified and to the methods used to study the association between variables.
In four articles,22,28,30,36 the odds ratio was analyzed to analyze the association between lower fluid intake and higher probability of intestinal constipation. In Thailand, fluid intake of less than 1800mL/day in individuals aged between 10 and 18 years was associated with an increase of 20% in the risk of fewer than three bowel movements a week.30 In Spanish children, regarding the intake of fewer than four glasses a day (800mL), a 2.5-fold probability of intestinal constipation was verified.
When fluid intake was four to eight glasses a day, the decrease was 5.8 times.22 In Hong Kong, an intake of up to two glasses a day (400mL) was considered as the cutoff. It was found that the consumption of 600–800mL a day and of more than 1000mL was associated with a decrease in the chance of intestinal constipation of eight to 14 times, respectively.28 In Korea, intake of less than 500mL/day between 25 and 84 months of age was associated with an increased risk of intestinal constipation.36 As shown in Table 1, different criteria were used to assess bowel habits, but all studies indicated a statistically significant association between lower water consumption and signs of intestinal constipation.
The strength of the associations expressed by the odds ratio showed great variability. The only two articles23,24 that did not disclose a statistically significant association between constipation and lower fluid consumption used the Rome II criteria37 for characterization of intestinal constipation. Based on these articles, it is possible to speculate that the Rome II criteria were very strict to characterize intestinal constipation in the samples that did not originate from specialized outpatient clinics. That is, the Rome II criteria can be considered more appropriate for patients with severe intestinal constipation treated at specialized services; however, it presents a lower positivity in studies carried out with samples from the general population.3 Although the fluid intake by children with intestinal constipation was lower, the statistical analysis showed no significance (Table 1). These two articles24,25 included fewer children than the others,22,28,30,36 which may have influenced the lack of association between water intake and intestinal constipation. Thus, based on the studies that expressed their results as odds ratios, despite the great variability in outcome characterization, all of them indicated an association between lower fluid intake and signs suggestive of intestinal constipation. When the same theme was analyzed in adults and the elderly, it was observed that the available information is also limited.
In adults, five of the six published articles showed an association between low fluid intake and intestinal constipation.14,23,31,33,34 In the elderly, six articles were retrieved,13,15,17,19,21,35 and five15,17,19,21,35 did not identify an association between fluid intake and intestinal constipation. Therefore, in both children and adults, the evidence indicates an association between lower fluid intake and intestinal constipation. From the experimental standpoint, it has been demonstrated that fluid restriction in rats leads to lower feed intake and less stool elimination. When controlling for the effect of decreased feed intake, it was confirmed that water intake restriction is associated with a reduction in fecal weight.38 In healthy human adults, it was observed that fluid deprivation decreases the frequency of bowel movements and fecal weight.14
These articles with samples from the general population did not consider whether the fluid intake of the assessed individuals was within the internationally recommended range. There are two recommendations for fluid intake, one for North America (Dietary References Intake)39 and another for Europe (European Community).40 In Brazil, it is suggested that the North American recommendations be followed.41
It should be noted that both recommendations consider not only the amount of water consumed as liquids (water, juice, and soft drinks), but also the water contained in food. The pediatric studies compiled in this review did not consider the water present in food, but only in the form of liquids. Thus, in the future, epidemiological studies should be planned to consider not only the volume and quality of consumed liquids, but also the estimation of water in food. These values should be compared to the existing recommendations for fluid intake by the pediatric population.
The NASPGHAN/ESPGHAN10 guideline says that, due to the lack of scientific evidence, increased fluid intake should not be part of the functional intestinal constipation therapeutic program. They only mention the article published in 1998 by Young et al.11 (Table 2). This randomized clinical trial compared two interventions with increased fluid intake in a group that did not receive this type of recommendation. The project brings a simple consideration: what would the placebo be in this study that could be used for it to be double-blind? Thus, this clinical trial involving 90 patients failed to observe any difference regarding clinical response to the three interventions related to higher fluid intake. The article does not report whether patients were treated simultaneously using other conducts that could mask the role of fluid intake in the evolution of intestinal constipation. The other four articles26,27,29,32 were not prospective clinical trials. The articles by Kuhl et al.26,29 evaluated the effect of a standardized guideline in the increase fluid intake as part of the treatment of retentive encopresis (fecal incontinence caused by retention). Apparently, the authors assumed that increased water intake is a measure that is part of intestinal constipation treatment. The first article showed that the patients had increased fluid intake and the frequency of evacuations at the end of the follow-up; however, since there was no control group, it was not possible to attribute the effect, or part of it, to the fluid intake increase.26 In the second article,29 a group was prospectively treated and compared with data from the medical files of other previously treated patients. It was verified that the intervention resulted in greater fluid intake; however, no improvement in clinical response was observed. These two studies, whose design was not specifically aimed at assessing the efficacy of increasing fluid intake in the treatment of constipation, did not offer evidence on the efficacy of fluids in controlling intestinal constipation associated with retentive encopresis.
Another article on this subject was a randomized clinical trial.32 It was performed to compare two types of treatment: (1) standardized diet and (2) personalized dietary intervention. It was observed that the group that received personalized dietary intervention had a higher increase in water intake than the group with a standardized diet. However, both groups showed similar improvement in evacuation frequency and difficulty, as well as in pain to evacuate. Both groups received lactulose during the observation period.32 The lactulose dose used in the study was not reported, nor whether it remained the same in both groups during the follow-up period. The most recent article retrieved in the literature search was carried out in Korea.36 The files of patients with constipation who had been stable for at least two months and had recorded fluid intake, stool consistency, and frequency of bowel movements were retrospectively evaluated. The article did not define what was considered higher and lower fluid intake. Moreover, the article did not specify how the consistency and frequency of evacuation scores were calculated based on the information in the medical records. The information on each patient was studied at two different moments. The results showed that there was an association between greater evacuation frequency and lower stool consistency with the use of polyethylene glycol 4000 in periods with higher fluid intake. However, due to its limitations, the clinical relevance of the observed differences may be considered debatable. Therefore, the analysis of these articles to evaluate the role of fluid intake in the treatment of intestinal constipation did not show any consistent results.
Regarding the role of water intake for constipation treatment in adults and the elderly, three studies were retrieved, one in adults18 and two in the elderly.12,16 In the study carried out in adults, it was observed that patients with constipation who consumed two liters of water had a statistically significant increase in the evacuation frequency and a decrease in the use of laxatives. In the elderly, an association was found between higher fluid and dietary fiber intake and intestinal constipation improvement,12 as well as less need for laxative use.16 However, in this situation, it is difficult to discriminate whether the positive effect was due to the higher fluid intake or to the higher dietary fiber intake, or even due to the synergistic effect of the two interventions.
Thus, based on the literature analysis, it was observed that few studies have assessed the association between water and/or fluid intake and intestinal constipation. Moreover, these studies are heterogeneous and difficult to compare. The results of studies with a sample of the general population suggest that a lower intake of water and/or fluids is associated with intestinal constipation. Regarding the role of water in the treatment of intestinal constipation, the few existing articles did not show an advantage of a greater fluid intake in the treatment. Conversely, studies with samples from the general population show a favorable effect of increasing water/fluid intake to improve intestinal habits. There is also evidence that normal children and adolescents do not meet daily fluid intake recommendations. In this context, it is considered that the adequate intake of liquids and dietary fiber is part of what are considered healthy eating habits. These may constitute a preventive measure and an initial therapy for cases of mild intestinal constipation. In contrast, more severe patients with fecaloma and fecal incontinence must undergo a treatment program that involves therapeutic measures for disimpaction and medication to ensure that the intestinal rhythm is normalized. For these patients, although there is no evidence, it is important to evaluate fluid intake. If necessary, an increase in fluid intake should be recommended, so that the patient reaches at least what is recommended worldwide.
Therefore, the authors conclude there are few articles that assessed the association between water and fluid intake and intestinal constipation in children and adolescents. The results suggest that a lower water intake is associated with a higher risk of intestinal constipation. Thus, it can be speculated, based on studies carried out with community samples, that a greater water intake may be beneficial for the prevention and treatment of mild intestinal constipation. Further studies are necessary to better understand the role of water and fluids in the etiology and treatment of intestinal constipation in children and adolescents.
Conflicts of interestThe authors declare no conflicts of interest.
Please cite this article as: Boilesen SN, Tahan S, Dias FC, Melli LC, Morais MB. Water and fluid intake in the prevention and treatment of functional constipation in children and adolescents: is there evidence? J Pediatr (Rio J). 2017;93:320–7.
This study was carried out at Universidade Federal de São Paulo (UNIFESP), Escola Paulista de Medicina (EPM), Disciplina de Gastroenterologia Pediátrica, São Paulo, SP, Brazil.