Narrative review evaluating the use of dietary supplements by children and adolescents.
Data sourceThe terms “dietary supplements”, “children” and “adolescents” were used in combination in the PubMed, MEDLINE, and SciELO databases, between 2000 and 2023, evaluating studies in humans, published in Portuguese, English, French and Spanish.
Data synthesisThe use of dietary supplements by children and adolescents has increased in recent decades. The most commonly used supplements are vitamins, minerals, trace elements, proteins, amino acids, melatonin, fatty acids, probiotics and energy drinks.
ConclusionDespite having specific indications, most of the time they are not prescribed by a healthcare professional. The reasons for use are varied. In children, the main reasons are protection against infections, stimulating growth, and poor food intake, with multivitamins and minerals being the most commonly used supplements. In adolescents, they are used to improve athletic performance and attain the “ideal body”, with proteins and amino acids being the most often used nutrients. As they are not regulated by health agencies and are sold without a prescription, their unsupervised use can lead to inadequate doses, with inefficiency or overdose risk. As for compounding formulations, or when available in preparations with multiple nutrients, the chance of errors increases. It is essential that pediatricians advise parents and patients about the indications, risks and benefits, prescribing them when necessary.
Dietary supplements are products used orally aimed at supplementing the diet of healthy individuals. They are also used to supplement the diet of individuals at increased risk for deficiency, or in morbid conditions that limit their bioavailability. They include macro and micronutrients, bioactive substances, enzymes, or probiotics, in isolated or combined form.1 They are sold without regulation.2 and are available in supermarkets and pharmacies as tablets, capsules, gums, powders, drinks and bars. They show great advertising appeal, and a variety of claimed benefits.1
The use of dietary supplements (DS) has increased in recent decades. More than 30 % of children in the United States use them regularly.3 Other countries, such as Australia and China, also have high consumption, with 22.6 % and 32.4 % of children, respectively, using supplements.4 In these studies, multivitamins and minerals were the most frequently used products (23.8 %), and the higher the family income and level of schooling, the greater their use.3 Regarding the use of vitamin supplements, a study carried out in Brazil with 7528 children from the five regions of the country showed a prevalence of 4.8 %.5
The main reasons for their use are to improve or maintain a healthy lifestyle, supplement the diet, reduce the risk of health problems, or increase immunity.6 However, to achieve a nutritional balance, parents should be encouraged to offer a varied diet to their children. There is no need for dietary supplements for healthy children with an adequate diet, in whom the excessive intake can even harm their health.7
The safety and effectiveness of dietary supplements are a growing concern for regulators and healthcare professionals, but there are few prospective, randomized clinical trials on the topic. There is also a lack of standardized guidelines for the use of dietary supplements.2 Most dietary supplements used by children are not oriented by a health professional, but rather by parents and family, friends, magazines and websites.6 Therefore, health professionals need to increase the parents' understanding of the safety and effectiveness of dietary supplements and promote quality infant nutrition.
This review article aims to analyze the caregivers’ perception of the use and reason for the popularity of dietary supplements and, then, address the importance (functions and benefits), adverse effects, and indications of the main dietary supplements used in the pediatric age group.
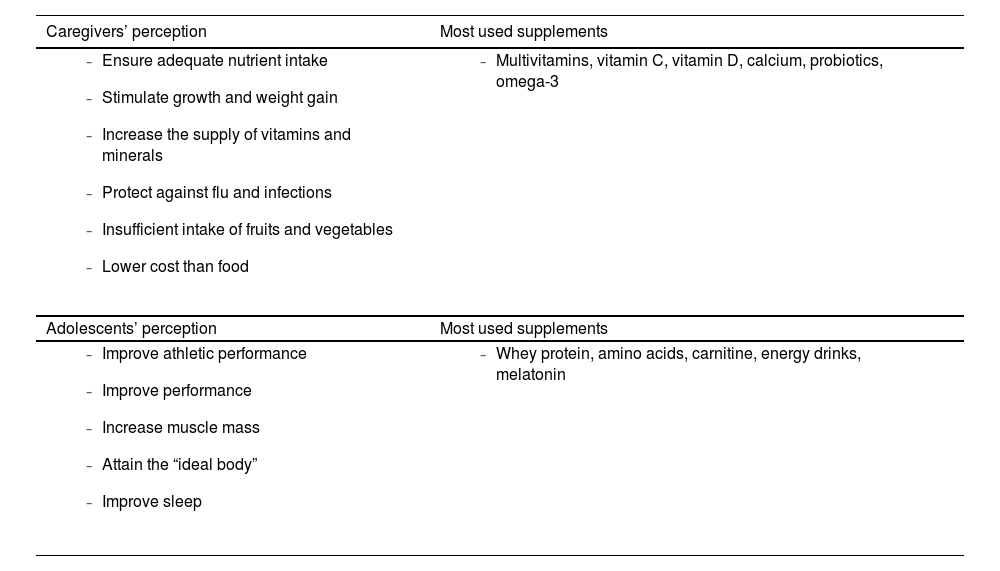
Food supplements: perception of useThe caregivers' perception of the use of dietary supplements varies. Some think that dietary supplements constitute a practical way to ensure nutrient intake. Others prefer that children get their nutrients from a healthy diet. There are also those who are concerned about the safety of DS because they are not regulated like medicines.
Research on the use of dietary supplements by North American children aged 1–10 years showed that 52 % of the parents offered some type of supplement to their children, especially: multivitamins, probiotics, minerals and omega-3. Only 43 % reported having consulted a health professional and the use was more frequent in families with higher income. The main reasons for their use were: snacking eating patterns and insufficient intake of fruits and vegetables.8 A study in China, evaluating children between 6 and 12 years old, showed that 20.4 % used dietary supplements. The most frequently used supplements were: calcium, vitamin C, and vitamin D. The reasons for supplementation were: improving immunity and stimulating growth. Around 37.5 % of the caregivers did not obtain medical advice to use DS.9 A Polish article investigating the use of dietary supplements by children between 3 and 12 years old showed that 54.8 % of caregivers offered them to their children. The main reasons were: improving immunity against flu and infections, protecting against adverse effects of antibiotics, and increasing the intake of vitamins and minerals.10
In adolescents, the perception of the use of dietary supplements is influenced by marketing that says these foods are functional, containing nutrients capable of improving athletic performance and even giving them the “ideal body”. Other sources of information are friends and gym acquaintances, as well as advertisements on social media by famous people. Few adolescents receive information from a nutritionist or doctor and often make excessive use of these products, believing they will have better results.11
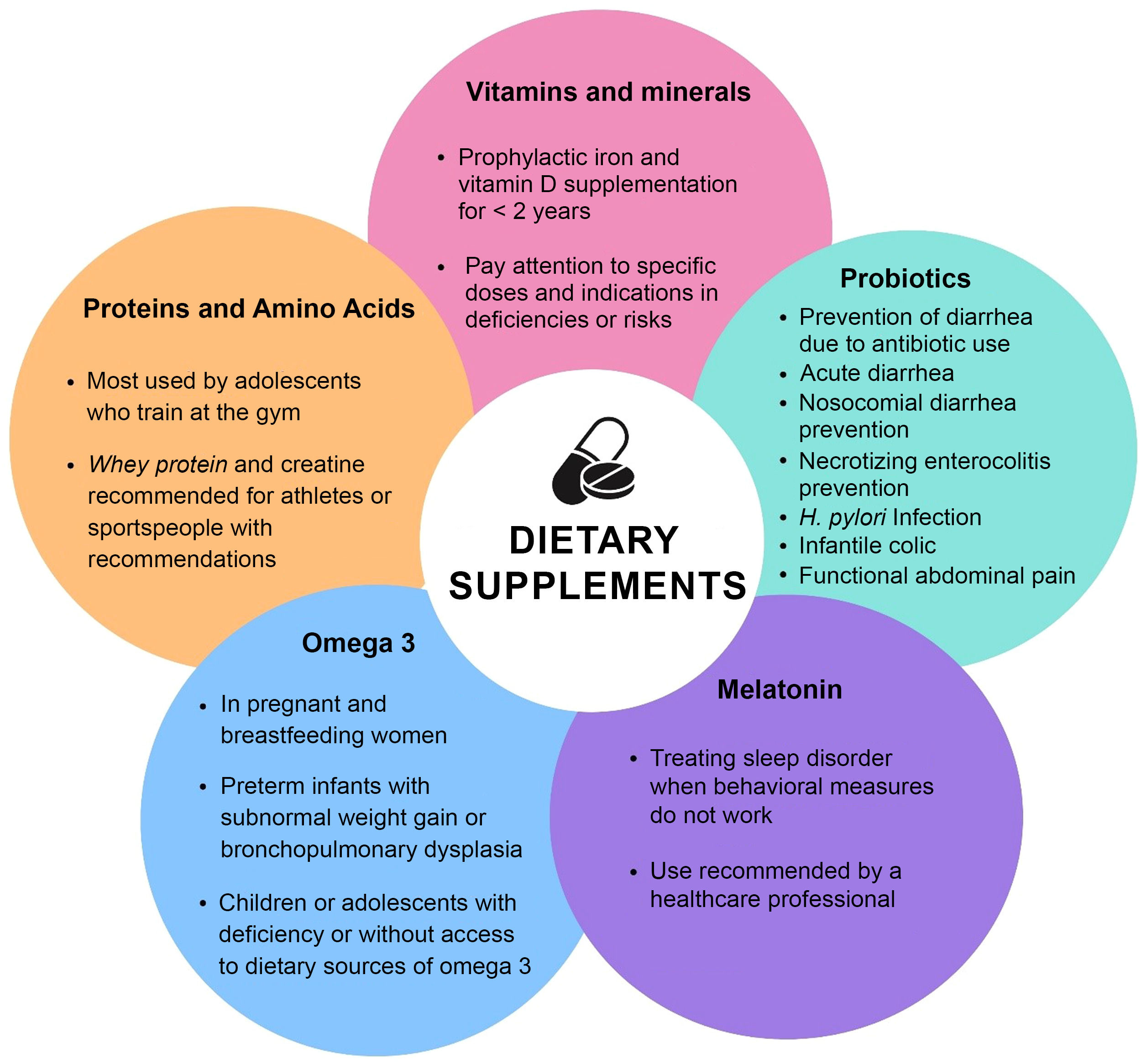
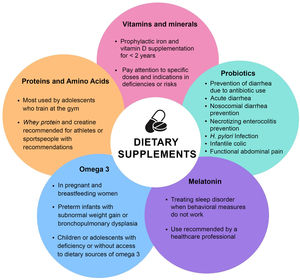
Table 1 summarizes the perception of caregivers and adolescents about the use of dietary supplements. figure 1 illustrates the main dietary supplements used by children and adolescents.
Dietary supplements in children and adolescents: perception and most used products.
The following topics will describe the main dietary supplements most frequently used by children and adolescents: proteins and amino acids, multivitamins, vitamin D, vitamin C, B complex vitamins, calcium, melatonin, iron, zinc, polyunsaturated fatty acids, probiotics, and breast milk fortifiers.
Proteins and amino acidsProteins and amino acids are the dietary supplements most frequently consumed by adolescents, especially those who train at the gym, with the aim of increasing muscle mass. However, the recommended approach is to consume good quality protein from food sources12, with the exception of adolescent athletes, or vegetarians who do not reach their protein target with their usual diet.12,13
Whey protein, the noblest protein fraction of milk, is used in several food products, from infant formulas (in compliance with legislation for foods intended for infants), to food supplements for children and adults, in proportions adequate for the recommended age ranges.
Whey protein is the protein supplement most frequently used by adolescents and adults who train at the gym.14 There are three types of whey protein: isolated, concentrated, and hydrolyzed. The concentrated product undergoes less processing, where not all the nutrients are removed from the whey, thus having a high caloric content and a protein concentration between 34 and 89 %. The isolated product undergoes more detailed filtration to eliminate or minimize fats and carbohydrates, containing approximately 90 % protein. The hydrolyzed product is the one that undergoes the hydrolysis process, during which rapidly absorbed oligopeptides are generated.15 Whey proteins are recognized as healthy ingredients due to the several advantages associated with their regular intake, including appetite control, exercise recovery, and promotion of satiety.
The indication and use of whey protein by adolescents who practice physical activity is at the discretion of the specific dietary prescription for training or sports. It is mainly used in muscle hypertrophy training when protein needs are not met with food. Although intake before and after the exercise is important, protein synthesis is highest in the period between 16 and 48 h after resistance exercise, a period considered a “window of opportunity”. Therefore, total intake throughout the day, especially after 24 h of physical activity, seems to be more effective for muscle recovery and protein synthesis.12,13 For adolescent athletes aiming to gain or maintain muscle mass, the recommendation and prescription of whey protein must be individualized according to the need and objective of the training.12,16,17 In adults, this recommendation varies from 1.3 to 1.7 g/kg/day.
Albumin is a protein of high biological value obtained from dehydrated egg whites, with slower absorption and lower leucine content when compared to whey protein. Its use has been overvalued by bodybuilders and adolescents who train at the gym, who consume up to 30 egg whites/day, an amount that exceeds the recommended daily needs for muscular hypertrophy and can cause kidney overload.11,18
Branched-chain amino acids (BCAAs) are used post-workout and associated with carbohydrate solutions to reduce fatigue and increase muscle mass. Although they are prescribed to reduce the risk of infections, evidence of these benefits is scarce.18
Creatine is a compound consisting of three amino acids (arginine, glycine and methionine). Its supplementation increases the muscle concentration of phosphocreatine, providing energy for high-intensity repetitive efforts and enhancing muscle explosion. It also buffers lactic acid produced during exercise, delaying muscle fatigue and painful sensations.19 It can be used in conditions that require hypertrophy or increased muscle strength with reduced fatigue, such as neuromuscular diseases and traumatic brain injury, and in competitive athletes.19,20 The dose indications are saturation phase (0.3 g/kg/day of creatine monohydrate, for 5 to 7 days), followed by the maintenance phase (3–5 g/day). It can be taken at any time of the day, regardless of whether it is taken pre- or post-workout.19,20
MultivitaminsThe abundance of vitamin supplements can make it difficult for patients to understand their use. Inadequate information increases the risk of attributing only beneficial effects to vitamin supplementation, neglecting adverse reactions, especially in relation to upper dose limits.21
Most multivitamins available on the market do not cover 100 % of the needs for all the micronutrients contained in them, and when there is a combination of more than one supplement, the risk of toxicity increases, due to the coexistence of the same components at different doses.21.22
The main source of vitamins must be a balanced diet, with supplementation being indicated in situations of compromised nutritional status, restrictive diets, pregnancy, risk of deficiencies, or diagnosis of deficiencies.21
Vitamin DVitamin D is a fat-soluble vitamin, also described as a prohormone produced in the skin after exposure to UVB rays and subsequent transformation into its active form by hydroxylation in the liver and kidneys. It can also be obtained orally by ingesting foods such as egg yolks, butter, fish, and fatty cheeses, or through dietary supplements.22
The main effect of vitamin D is in the prevention of rickets and osteomalacia. Some studies point to potential benefits in the prevention of type 2 diabetes mellitus, in the pathophysiology of type 1 diabetes mellitus, and in the prevention of autoimmune, infectious, and allergic diseases.22 The main causes for its deficiency are inadequate exposure to sunlight, insufficient intake or absorption, liver alterations, use of medications, and metabolism defects.
Excess vitamin D can cause hypercalcemia, hypercalciuria, or nephrocalcinosis. To prevent its toxicity, it is recommended to monitor serum levels of 25-hydroxyvitamin D in children who receive long-term supplementation equal to or above the maximum intake level.22
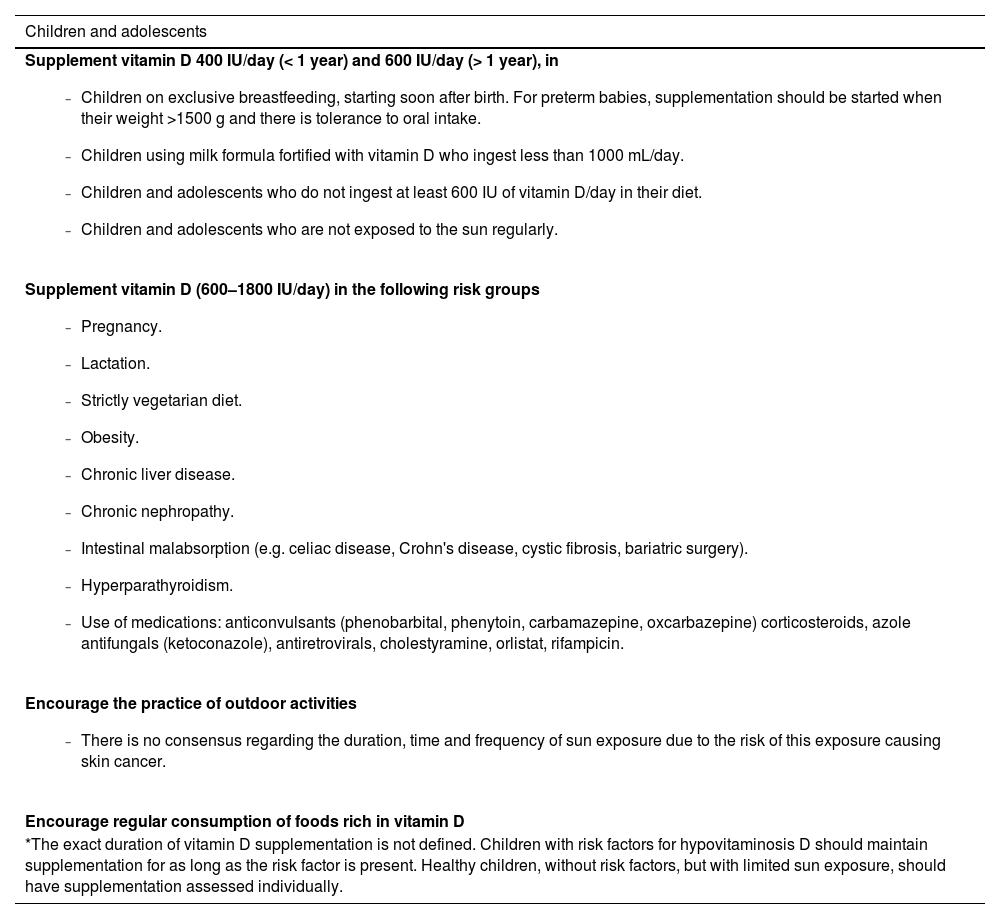
The Brazilian Society of Pediatrics recommends supplementation in the first two years of life. There is also a recommendation for supplementation in prematurity, protein-energy malnutrition, chronic renal failure, and chronic liver disease.22,23Table 2 shows the indications for prophylactic vitamin D supplementation.
Recommendations for preventing hypovitaminosis D in children and adolescents.21
Vitamin C is a water-soluble vitamin found most frequently in vegetables and citrus fruits. It is essential for collagen synthesis, in addition to acting as a cofactor for several enzymes, having an antioxidant effect and helping in iron absorption. Its deficiency is caused by a diet with restricted foods that are sources of this vitamin and the main symptoms of deficiency are: anorexia, irritability and joint pain. Scurvy, the most severe form of the deficiency, is a rare condition.21,22
The dietary requirements, 35 and 75 mg/day, are often met with the recommended daily consumption of fruits and vegetables. Vitamin C supplementation has not been shown to be beneficial in reducing symptoms of respiratory infections in children.24 There is no recommendation for routine supplementation in healthy children.
Complex B vitaminsThe vitamins in the B complex are water-soluble and act on energy metabolism. Their main source is food, especially milk, cheese, meat, liver and eggs. There is no indication for routine supplementation of B vitamins in healthy children unless there are dietary or absorptive restrictions that affect the intake of these vitamins. B complex vitamins are usually administered together, except in specific deficiencies, in which the dose is individualized.21,22
The main source of folic acid (vitamin B9) is green vegetables. It is an important supplement in pregnancy due to its role in the normal neural and physical development of the fetus. There is also evidence of a possible reduction in the risk of cardiovascular diseases, cancer, and psychiatric disorders.21,22 Indications for supplementation include patients with severe malnutrition, sickle-cell anemia, inborn errors of metabolism involving the folate pathways, pregnant women up to the 12th week of gestation, and use of medications that interfere with folate metabolism.21,22
Cyanocobalamin (vitamin B12) is essential for good neurological function, preventing endothelial damage and being a cofactor in several metabolic pathways. It is found naturally in animal products. To be absorbed in the terminal ileum, vitamin B12 must bind to the intrinsic factor produced by the gastric mucosa. Its deficiency can be caused by restrictive diets, after bariatric surgery, or absorption problems. Some medications can reduce vitamin B12 levels, such as proton-pump inhibitors, histamine receptor antagonists and metformin.21 Clinical manifestations of the deficiency are megaloblastic anemia, neuropathies, drowsiness, irritability, reduced visual acuity, paresthesia and hyperreflexia.21 Vitamin B12 supplementation should be carried out in individuals with dietary restrictions, short bowel syndrome with absence of terminal ileum, post-bariatric surgery, or conditions that affect its absorption. Breastfeeding mothers following a vegan or macrobiotic diet should receive vitamin B12 supplements.
MelatoninMelatonin is a hormone secreted mainly by the pineal gland. Its main functions are regulation of the circadian rhythm and wake/sleep cycle, antioxidant and anti-inflammatory action. Melatonin supplements have been used in children with sleep disorders such as attention deficit hyperactivity disorder, autism spectrum disorder, atopic dermatitis and neurodevelopmental disorders. However, there is no consensus on the indication, dose, duration of use, and long-term effects, including interference with puberty, menstrual cycle and increased prolactin secretion. Adverse reactions in children are dizziness, headache, agitation and nocturnal enuresis.
As it is considered a natural, low-cost, over-the-counter product that promises the improvement of sleep quality, there has been a considerable increase in its consumption in the last decade.25 Moreover, many supplements do not contain the amount of melatonin described on the label.26
The American Academy of Sleep Medicine recommends that behavioral strategies to improve sleep be considered before using melatonin and that its use should be guided by a health professional, using products that have a quality seal, such as the US Pharmacopeia (USP verified) in the United States. The initial dose should be the lowest possible, between 0.5 and 1 mg/day, with a maximum dose of 5 mg/day in adolescents.
CalciumCalcium is the most abundant mineral in the body and essential for bone composition. Its chronic deficiency causes rickets and osteomalacia. Dairy products are the main source of this nutrient because they have efficient absorption (30–40 %), due to the lactose content.27
Risk factors for calcium deficiency are preterm birth, inadequate dietary intake, systemic inflammation, and chronic use of medications (e.g. glucocorticoids). In these situations, bone health screening and calcium and vitamin D supplementation should be considered.28
Supplementation in healthy children with adequate calcium intake is not indicated, as its use does not significantly improve bone mineral density and does not reduce the risk of fractures. Adverse effects of supplementation are diarrhea or constipation, increased urinary excretion of calcium and phosphorus, and nephrocalcinosis.29
Therefore, supplementation with 500–1000 mg/day of calcium is recommended in children and adolescents receiving less than 300 mg of calcium in the diet.27 Special attention should be given to vegan children because to obtain the recommended intake of calcium in the diet they must consume a high amount of foods rich in calcium and low in phytate and oxalate (cruciferous vegetables, green leafy vegetables, soy, tofu).30
IronIron is an essential mineral for the formation of hemoglobin and the transport of oxygen. It is also found in almost all tissues, acting as a cofactor and regulating cell oxidative processes.31 Iron deficiency is the most common micronutrient disorder. Iron -deficiency anemia is among the eight most prevalent chronic diseases worldwide. In Brazil, it is estimated that 33 % of the children have anemia.32
Chronic anemia causes growth deceleration, pubertal delay, and cognitive impairment, increase the risk of infectious diseases and contributes to low humoral response to vaccines. Iron deficiency, even without anemia, can have negative metabolic effects.31
Newborn iron stores depend on the mother's iron status, gestational age, and birth weight. Due to this limited reserve and rapid growth, babies are considered a risk group, especially those with low birth weight and preterm infants.33
In inflammatory diseases, increased hepcidin production can cause reduced iron absorption and iron retention in macrophages, resulting in reduced levels of circulation. Therefore, regular monitoring of iron deficiency is necessary for these patients, in whom ferritin may be normal or high.33
Adolescents in the growth spurt phase, girls just after menarche, vegetarians and vegans also have an increased risk of developing iron deficiency. Vegetarian and vegan diets have lower iron bioavailability than those with heme iron from animal sources. Furthermore, the presence of phytates in cereals and legumes decreases iron absorption. Consuming rice or soy-based infant formula in adequate amounts or breastfeeding provides the necessary iron. In older children, iron should be monitored regularly. Foods rich in iron (soy, beans, whole grains, leafy vegetables) associated with fruits rich in vitamin C should be offered at each meal. Preparation methods, such as soaking and using yeast, interfere with iron absorption.30
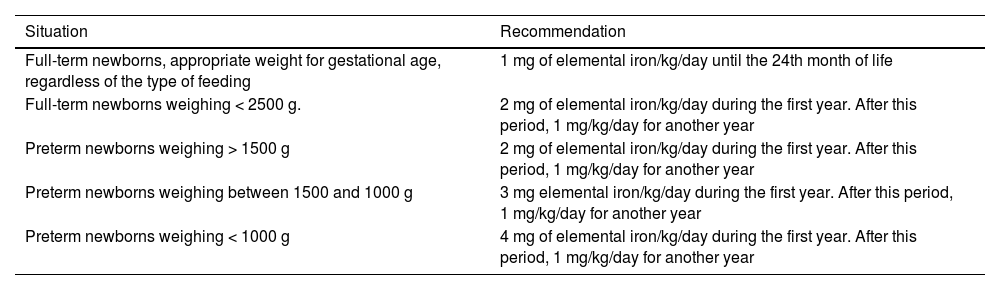
The indications for universal iron supplementation, according to the World Health Organization (WHO), are pregnant women and children aged between 6 and 24 months. Infants supplemented with iron have better motor and mental development and higher levels of anti-vaccine IgG.34 However, there are no clear benefits of this supplementation in healthy, full-term children in countries where the prevalence of anemia is low. Table 3 summarizes prophylactic iron supplementation in infants.33
Recommendations for prophylactic iron supplementation in infants.31
Zinc is an essential mineral for the body's basic physiological needs, such as normal growth and development, metabolism and maintenance of cell integrity and function.34 Diets rich in fiber and phytates reduce its absorption. The main causes of its deficiency are dietary errors and increased gastrointestinal losses.
Zinc deficiency is associated with anorexia, growth retardation, altered senses of taste and smell, and greater susceptibility to infections. Acrodermatitis enteropathica is characterized by diarrhea, alopecia and dermatitis around the eyes, nose, mouth and buttocks.30,34
Its role in supporting the immune response against viral infections has been extensively studied, particularly in children. However, there is little evidence that zinc supplementation reduces the incidence and morbidity of respiratory diseases, including in cases of COVID-19.35 One should be aware of the possibility of zinc supplementation inhibiting copper absorption and reducing HDL-cholesterol concentration. Furthermore, its use has been associated with episodes of vomiting.
In relation to vegetarian and vegan patients, similarly to iron, breastfed infants or those receiving an infant formula based on rice or soy protein, zinc intake is sufficient to meet the needs. Vegetarian and vegan children and adolescents, on the other hand, need to eat a variety of vegetables (kale, turnip, mustard, radish, rapeseed, watercress, horseradish) to meet their needs. However, the difficulties in following this diet explain the increased risk of deficiency, and tests to detect zinc levels need to be regularly performed.30
Some studies demonstrate that zinc supplementation improves growth, particularly in children aged 6 months to 12 years in places where the risk of zinc deficiency is relatively high.36 Zinc supplementation is recommended at a dose of 20 mg/day for 10 days for all children with diarrhea, regardless of the type. Infants aged six months or younger should receive 10 mg/day for 10 days. In low-income countries, studies document its effectiveness in reducing both the duration and severity of diarrhea, especially in malnourished children and persistent diarrhea.36 Another indication is the supplementation for preterm infants (0.5–1 mg/day) up to six months of corrected age, as this supplementation can increase weight gain and linear growth.37
Polyunsaturated fatty acidsPolyunsaturated fatty acids are classified into: omega-3, found in vegetable oils, wheat germ and fish; omega-6, from vegetable oils such as soy and corn; and omega-9, found in olive oil.38,39
Omega-3, when metabolized, gives rise to the long-chain polyunsaturated fatty acids DHA (docosahexaenoic acid) and EPA (eicosapentaenoic acid). DHA contributes to cognitive and visual development.38,39
The first thousand days of life (27th week of pregnancy to two years of age) is the time of greatest need for this nutrient, due to brain development. For this reason, DHA is recommended in the diet of pregnant and breastfeeding women. For children, adolescents and adults, the recommended intake of DHA can be achieved by consuming at least two weekly servings of marine fish rich in this nutrient.39
The Brazilian Association of Nutrology (ABRAN, Associação Brasileira de Nutrologia) advises that breastfed children should have breast milk as a source of omega-3 and from two to five years old, they should have access to food sources of this nutrient, reserving supplementation for cases of deficiency or absence of this nutrient in a food source.39
As for preterm infants receiving infant formulas, the latter already include DHA supplementation. In preterm infants with subnormal weight gain or bronchopulmonary dysplasia, supplementation with polyunsaturated fatty acids is recommended, at least until 52 weeks of corrected age.40
ProbioticsProbiotics are live microorganisms that, when administered in adequate quantities, provide health benefits to the host. Probiotic strains are identified according to their genus, species, subspecies and an alphanumeric name that identifies a specific strain.41,42
The effects of probiotics are specific and depend on the strain and dose used.42 In February 2023, the European Society of Gastroenterology, Hepatology and Nutrition (ESPGHAN) published a document on the use of probiotics and prebiotics for the management of gastrointestinal disorders in pediatrics. These indications include: acute diarrhea (Lacticaseibacillus rhamnosus, Saccharomyces boulardii, Limosilactobacillus reuteri), prevention of diarrhea associated with the use of antibiotics (S. boulardii or L. rhamnosus GG), prevention of nosocomial diarrhea (L. rhamnosus GG), prevention of necrotizing enterocolitis in preterm infants (L. rhamnosus GG, association of Bifidobacterium BB-02, B. lactis BB-12 and Streptococcus thermophilus TH-4), adjuvant treatment of Helicobacter pylori (S. boulardii) infection, infantile colic in breastfed children (L. reuteri DSM 17938, B. lactis BB-12) and in functional abdominal pain (L. rhamnosus, L. reuteri).42
There is no consensus on the supplementation of specific strains of probiotics in attention deficit hyperactivity disorder, obesity, hepatic steatosis, and depression in the pediatric age group.41-43
Breast milk fortifiersBreast milk fortifiers are dietary supplements added to breast milk to increase its nutritional value and provide additional nutrients to newborns born prematurely.
In preterm newborns, breast milk is insufficient to provide the necessary amount of calcium and phosphorus.44 On average, breast milk contains 30 mg of calcium, 15 mg of phosphorus, and 8 IU of vitamin D per 100 mL, while the needs of newborns on full enteral feeding are 140 to 160 mg/Kcal/day of calcium and 95 to 108 mg/Kcal/day of phosphorus (alkaline phosphatase- AP). Formulas for preterm infants contain, on average, 90 to 150 mg of calcium and 50 to 90 mg of phosphorus for every 100 mL.
When using breast milk for preterm infants, it must be fortified with calcium and phosphorus to prevent the development of metabolic bone disease of prematurity:
- -
FM85®: add 1 g for every 25 mL of breast milk.
- -
Aptamil FMS®: add 1 g for every 25 mL of breast milk.
- -
Enfamil HMF®: add 0.71 g for every 25 mL of breast milk.
Table 4 summarizes the recommendations for the use of pediatric dietary supplements in children with feeding difficulties.21,45
Despite having specific indications, dietary supplements are most frequently not prescribed by a healthcare professional. In children, the main reasons for its use are protection against infections, stimulating growth, and poor food intake, with multivitamins and minerals being the most commonly used supplements. In adolescents, supplements are used to improve athletic performance and attain the “ideal body”, with proteins and amino acids being the most often used nutrients. As they are not regulated by health agencies and are sold without a prescription, their unsupervised use can lead to an inefficiency or overdose risk. When compounded, or available in preparations with multiple nutrients, the chance of errors increases. It is essential that pediatricians advise parents and patients about their indications, risks, and benefits, prescribing them when necessary. Remember there is no need for healthy children to use dietary supplements.